Abstract
Scientific interest in optimizing outcomes after anterior cruciate ligament (ACL) reconstruction is ongoing, and some recent developments have focused on graft shape as one of the most important factors of anatomic graft placement. The double-bundle or fanlike structure of the native ACL seems to more closely restore normal function and control of rotational stability of the knee with implant-free or press-fit techniques, creating a favorable situation in terms of direct graft-tunnel healing. The ACL reconstruction technique presented in this article enables safe, reproducible, and anatomic fixation of the patellar tendon autograft, providing the biological and biomechanical benefits of direct bony integration of the ribbonlike bone–patellar tendon–bone graft. Because press-fit fixation represents a technically challenging surgical procedure, the goal of the described technique is to enable direct bone-to-bone healing by using secondary extracortical femoral and tibial fixation without the need for a true press-fit situation. Safe and anatomic femoral tunnel drilling is achieved with an outside-in technique (retrograde drilling), hence providing advantages in the routine clinical setting in terms of applicability and time effort. To reduce donor-site morbidity caused by bone block harvesting, refilling of the harvest sites with autologous material is performed.
Anterior cruciate ligament (ACL) reconstruction is one of the most frequently performed orthopaedic procedures. A plethora of techniques for performing ACL reconstruction are available today; most primary reconstructions are conducted using hamstring tendon, bone–patellar tendon–bone (BPTB), and quadriceps tendon autografts.1,2 With current trends toward individualized ACL reconstruction, the BPTB graft is experiencing a renaissance in primary ACL reconstruction because some studies and registry data show a lower revision rate, especially in younger patients; reduced graft elongation; and a higher return to the preinjury level of activity than with hamstring grafts.3
With the idea of improved graft-tunnel healing in mind, surgical techniques for implant-free ACL reconstruction have been published previously.4 Theoretically, optimal bone-to-bone healing is reached when bone blocks are fixed within tunnels in a press-fit technique. In addition, this creates a favorable situation for a potential revision operation.4 However, press-fit fixation of an ACL graft requires high-level surgical skills, and it remains technically challenging to achieve the same level of secure fixation as with screw or button fixation. Drilling of an anatomic femoral tunnel through the anteromedial portal in combination with reduced visibility at a high knee flexion angle when impacting the bone block has an increased risk of posterior-wall blowout fractures.5 Despite many interesting features, in combination, this results in a low applicability of press-fit techniques in clinical routine.
The arthroscopic ACL reconstruction technique presented in this article was developed to combine optimal graft-tunnel healing through press-fit bone-to-bone contact with the clinical practicability of reproducible tunnel sizing and secure fixation known from other contemporary ACL reconstruction techniques. In addition, safe and anatomic femoral tunnel drilling is achieved with an outside-in, retrograde drilling technique. To reduce potential donor-site morbidities created by bone block harvesting, the harvest sites are refilled with autologous material.
Technique
Patient Positioning
The patient is placed in the supine position, with the operative knee fixed in a thigh tourniquet and both legs hanging. It is important for the positioning to allow knee flexion to 120°.
Graft Harvest
With the knee at 90° of flexion, a 4-cm longitudinal, slightly medial skin incision is performed just over the patellar tendon, starting approximately 2 cm below the inferior pole of the patella (Video 1). Sharp preparation is performed to expose the paratenon, which is then incised and thoroughly separated from the patellar tendon. As a rough guideline, in larger patients, a central 10-mm tendon strip is created, whereas in smaller patients, a 9-mm tendon strip is harvested (Fig 1A).
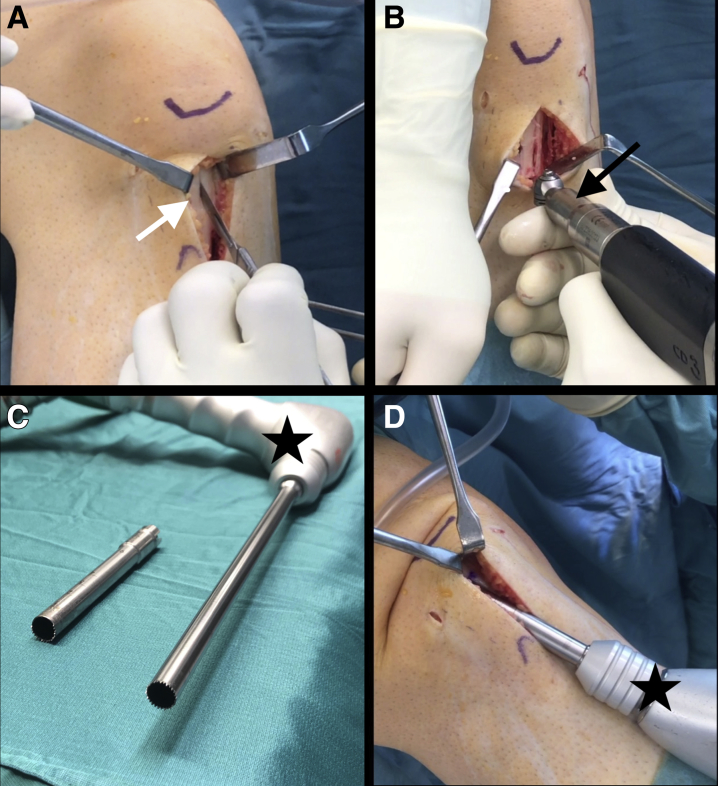
Fig 1.
Graft harvest in right knee, with patient in supine position. The right leg is hanging with the thigh fixed in a tourniquet. (A) A central 9- to 10-mm strip is created from the patellar tendon (white arrow). (B) At the height of the tibial tuberosity, a 1-cm-wide calibrated oscillating saw blade is used to create the vertical bone cuts, and a smaller, 0.5-cm saw blade (black arrow) is used for the distal horizontal cut about 15 to 20 mm distal to the tendon insertion to create a bone block of sufficient length. (C) A hollow saw (Wolf) with a 9.5-mm diameter for creating the tibial tunnel is shown on the right (black star); a 9.4-mm (two-thirds toothed) hollow saw used to harvest the patellar bone block is shown on the left. (D) A cylindrical bone block, approximately 15 to 20 mm in length, is harvested from the patella, after insertion of the patellar tendon strip with the tibial bone block into the 9.4-mm trephine (black star).
The insertion of the patellar tendon at the tibial tuberosity is identified, and an approximately 20-mm bone block is harvested. For this purpose, a 1-cm-wide calibrated oscillating saw blade is used to create the vertical bone cuts in a slightly converging fashion, and a smaller, 0.5-cm saw blade is used for the distal horizontal cut so that the adjacent patellar tendon insertion is not harmed (Fig 1B). The bone block is then harvested by completing the proximal bone cut using a small chisel.
Two drill holes are made in the proximal and distal thirds of the bone block, respectively. A suture is passed through the distal hole. After dissection of the tendon strip from the Hoffa fat pad, the proximal incisions are completed to show and mark the insertion of the patellar tendon to the inferior pole of the patella with a skin marker. Now, the sutures are passed through a hollow saw with a guidewire so that the distal bone block and the central patellar tendon can be inserted into an oscillating trephine, with two-thirds toothing (Fig 1C). A cylindrical bone block, approximately 15 to 20 mm in length, is then harvested from the patella (Fig 1D). The surgeon can therefore choose from 2 different sizes (8.4 or 9.4 mm in diameter; Wolf, Tuttlingen, Germany) to roughly match the patient's height, choosing the 8.4-mm hollow saw in women or smaller patients. The bone block is separated proximally by elevating the trephine or using a small chisel.
Graft Preparation
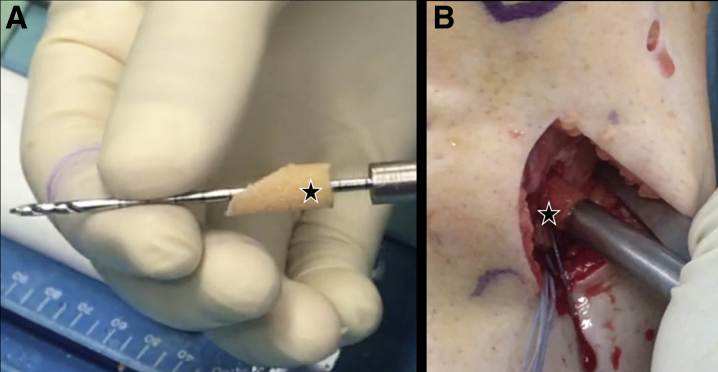
For femoral press-fit fixation, the cylindrical patellar bone block is shaped with a rongeur and rasp so that the tip just fits the entrance of a 9-mm tunnel (9.4-mm hollow saw) or an 8-mm tunnel (8.4-mm hollow saw) (Fig 2A). For further femoral backup fixation, a BTB TightRope device (Arthrex, Naples, FL) is brought through a 2-mm drill hole at the center of the proximal bone block (Figs 2B and 3). The insertion of the patellar tendon is marked for easier orientation when later impacting the bone block.
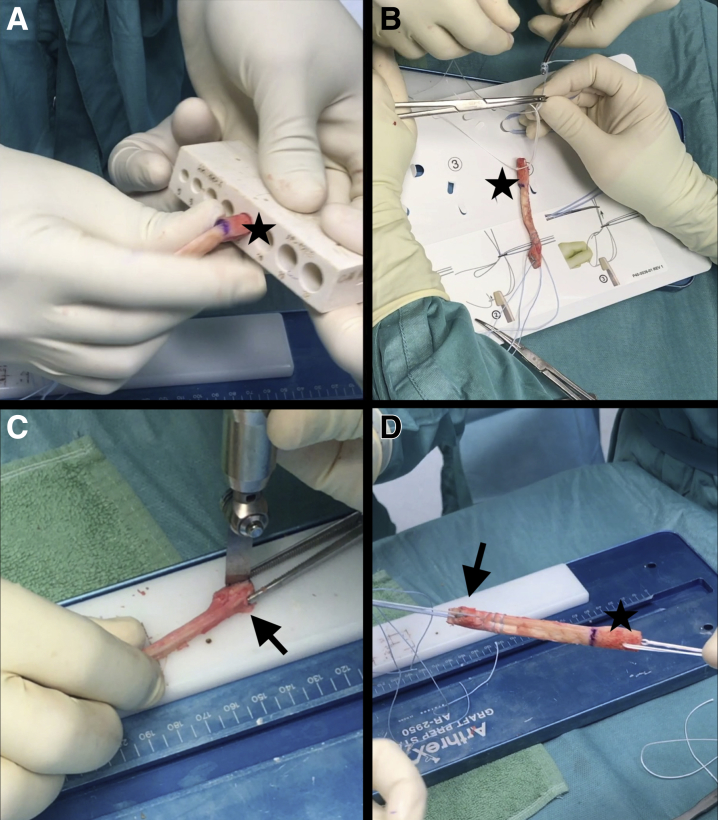
Fig 2.
External view of bone–patellar tendon–bone graft during preparation. (A) The cylindrical patellar bone block, 15 to 20 mm in length, is shaped with a rongeur and rasp so that the tip just fits the entrance of a 9-mm template (black star) (or an 8-mm template when the 8.4-mm trephine has been used). (B) For further femoral backup fixation, a BTB TightRope is brought through a 2-mm drill hole at the center of the proximal bone block (black star). (C) Narrowing of the free end of the distal bone block (from the tibial tuberosity) is performed with an oscillation saw (black arrow) so that a trapezoid bone block is shaped (Fig 3). (D) The total length of the graft is determined after placement of 2 No. 2 FiberWire threads within the distal ligament and the trapezoid bone block (black arrow). The cylindrical femoral bone block is shown with the BTB TightRope (black star) in place.
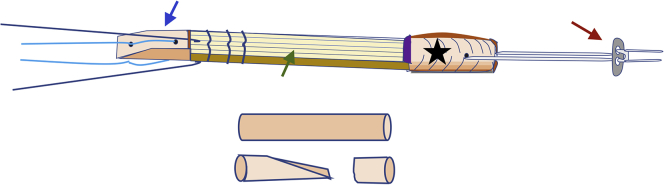
Fig 3.
To perform graft preparation, a BTB TightRope (red arrow) is brought through a 2-mm drill hole at the center of the proximal bone block (black star). A No. 2 FiberWire suture (light blue) is brought through each of two 2-mm drill holes in the distal bone block (blue arrow). A No. 2 FiberLoop (dark blue) is used to place a whipstitch through the distal part of the patellar tendon itself. One suture end is again brought through the graft so that tilting of the bone block is avoided when pulling on the sutures. The bone cylinder harvested from creating the tibial tunnel is prepared with a small oscillating saw blade to refill the harvest site at the distal patella (short bone cylinder) and the tibial tunnel in a press-fit fashion. Therefore, the cylinder is trapezoidal to enable tapping in the bone material in a press-fit manner, ensuring direct bone-to-bone healing of the graft in the tibial tunnel. The green arrow indicates the patellar tendon graft.
Now, the distal (tibial) bone block is prepared. After narrowing of the free end of the bone block with an oscillation saw (Fig 2C), a No. 2 FiberWire suture (Arthrex) is brought through each of two 2-mm drill holes. A No. 2 FiberLoop (Arthrex) is used to place a whipstitch through the distal part of the patellar tendon itself. By use of this technique, 2 independent suture strands are available for later fixation of the graft (Fig 3).
The total length of the graft and the femoral bone block is determined (Fig 2D). Then, the graft is placed into a surgical swab soaked with vancomycin.
Femoral Tunnel
After standard arthroscopic evaluation and removal of ACL remnants, the footprint is visualized through the anteromedial portal. At 90° of knee flexion, the femoral ACL guide is inserted into the anterolateral portal and placed at the anatomic ACL footprint to ideally cover the anteromedial- and posterolateral-bundle area (Fig 4A). A 2-cm skin incision is made on the lateral thigh, the lateral cortex is cleared with a rasp, and the drill sleeve is placed on the lateral femur. The intraosseous tunnel length can be seen on the marking of the drill sleeve. With a 9-mm FlipCutter (fold-out drill; Arthrex) (when the 9.4-mm hollow saw has been used) or 8-mm FlipCutter (when the 8.4-mm hollow saw has been used), an anatomic femoral socket is placed with an outside-in, retrograde drilling technique, matching the length of the bone block (Fig 4B). It is important to set the angle of the femoral drill guide to 115° to 120° so that a “killer angle” for later insertion of the bone block is avoided.
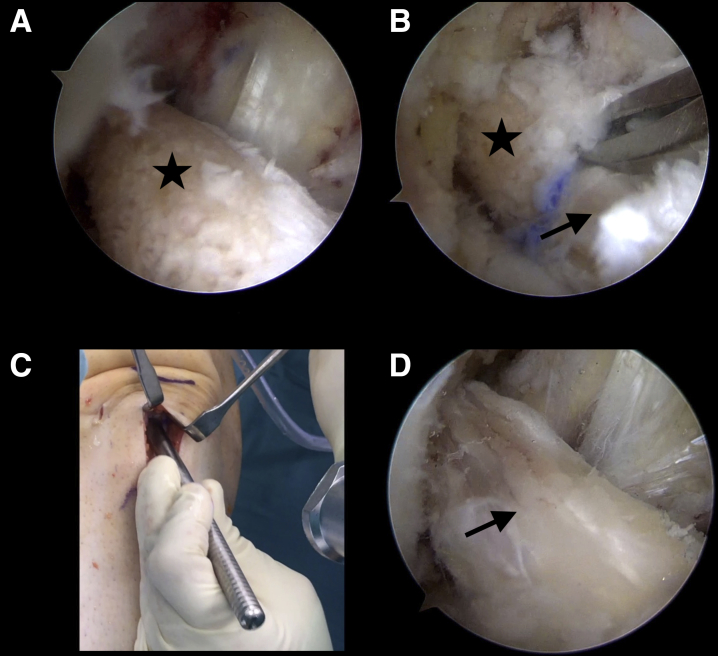
Fig 4.
Arthroscopic view of femoral tunnel drilling from anteromedial portal (A, B) and tibial tunnel creation from anterolateral portal (C, D). (A) At 90° of knee flexion (a right knee in this case), the femoral anterior cruciate ligament (ACL) guide is inserted into the anterolateral portal and placed at the anatomic ACL footprint on the lateral intercondylar wall to ideally cover the anteromedial- and posterolateral-bundle area (black star). (B) With a FlipCutter (fold-out drill), an anatomic femoral socket (black arrow) is placed with an outside-in, retrograde drilling technique. (C) A 2.5-mm guidewire is introduced at the center of the tibial ACL footprint with a 60° aimer or an adjustable aimer (Wolf, Tuttlingen, Germany) (red star). (D) The hollow saw (9.5-mm outer diameter) is used with a centering device. The cylindrical bone block from the tibial tunnel can then be removed, after cutting of the remnant ACL fibers with electrocautery (blue arrow). The red arrow indicates the fully toothed 9.5-mm trephine.
Now, a FiberStick (Arthrex) with a No. 0 FiberWire is introduced into the joint, and the thread is pulled through the lateral portal and secured with a clamp. The femoral tunnel is rechecked arthroscopically; rough edges are smoothed and bone debris is removed with a shaver.
Tibial Tunnel
The tibial tunnel is created using a special oscillating trephine with a 9.5-mm outer diameter (Richard Wolf, Knittlingen, Germany). A 2.5-mm guidewire is introduced on the center of the tibial ACL footprint, and the hollow saw is used with a centering device (Fig 4C). The tibial guide can be used with a fixed 55° targeting device or a standard aimer with adjustable angulation (Richard Wolf). Now, a cylindrical bone block is removed from the tibial tunnel (Fig 4D), which later can be used for refilling the tibial tunnel and the harvesting sites. Furthermore, the tibial tunnel length can easily be determined by the length of the bone cylinder. Again, any intra-articular edges are smoothed with a shaver.
Graft Insertion and Femoral Fixation
With a suture grasper, the shuttling suture is pulled out through the tibial tunnel. The BTB TightRope threads are pulled percutaneously through the joint and the lateral femoral cortex. Then, the graft is introduced into the tibial tunnel with correct angulation of the bone block so that cancellous bone remains anteriorly or the fanlike ACL footprint is best covered (Fig 5A). With further pulling on the TightRope leading sutures, the femoral bone block enters the joint and the TightRope button is pulled out of the lateral femoral cortex. It is important not to flip the button and shorten the adjustable strands of the BTB TightRope at this point; rather, the button should be completely shuttled to leave enough slack in the adjustable loop to angulate and guide the bone block into the femoral tunnel with a suture grasper (Kingfisher; Arthrex) or arthroscopic examination hook (Fig 5B).
Fig 5.
Graft insertion and fixation with arthroscopic view from anterolateral portal (A, (B, D) and external view of distal pole of patella (C). (A) The graft is introduced into the tibial tunnel with correct angulation of the bone block (black star) and advanced into the joint by pulling all 4 sutures coming from the BTB TightRope. (B) The bone block (black star) is guided into the femoral tunnel between the posterior cruciate ligament and lateral intercondylar wall with a suture grasper (Kingfisher). The bone-tendon transition is marked with a skin marker (black arrow). In this step, correct angulation in line with the femoral tunnel is crucial. The bone block can usually then be pulled into the socket without the need for an arthroscopic tappet. (C) The harvest site at the distal pole of the patella is refilled with bone material (Fig 3) using a tappet. An absorbable No. 0 Vicryl suture is then used to close the defect. (D) Final arthroscopic evaluation is performed, and proof of graft tension (black arrow) is confirmed.
At 110° of knee flexion, the bone block is placed on the entrance of the femoral tunnel, and after the correct orientation is ensured, the graft can be pulled into the femur. Because the femoral tunnel has a diameter of either 9 mm, with a bone block of 9.4 mm, or 8 mm, with a bone block of 8.4 mm, an arthroscopic impactor can be used to help tap the graft into the femoral socket, but pulling strongly on the TightRope is usually sufficient to seat the graft into the femoral socket with correct alignment.
Now, an arthroscopic slide is placed around the TightRope strands and down onto the lateral femoral cortex, and by pulling on the white strands of the BTB TightRope, the adjustable loop is shortened with the button slipping back onto the femur. Correct cortical placement of the button is determined by either endoscopic or fluoroscopic imaging.
Tibial Fixation
For graft tensioning, the distal sutures are pulled and the knee is cycled 10 times through its range of motion to remove any slack. By pulling the strands from the bone block at maximum manual force at 20° of knee flexion, the strands placed within the distal ligament are fixed tibially with a knotless bone anchor (SwiveLock, 4.75 mm; Arthrex).6
Bone material harvested from creating the tibial tunnel is now inversely shaped with an oscillating saw blade (Figs 3 and 6A) and tapped in a press-fit manner over the distal bone block of the graft into the tunnel to enable bone-to-bone healing (Fig 6B). The strands from the distal bone block are fixed with another knotless anchor for backup fixation of the bone block. After extracortical and press-fit bone-on-bone fixation within the tibial tunnel, final arthroscopic evaluation is performed and proof of graft tension is confirmed before the FiberWire threads are cut (Fig 5D).
Fig 6.
Refilling of tibial tunnel with external view of bone cylinder (stars) on 2-mm guidewire (A) and tibial tunnel at anteromedial tibial surface (B). The inversely shaped bone cylinder (harvested from creating the tibial tunnel with the 9.5-mm trephine) is placed on a 2-mm guidewire (A) and is then placed over the graft in the tibial tunnel and tapped into the tunnel with the use of a centering device or a tappet (B).
Closure
Remaining bone material harvested from the tibial tunnel is used to refill the defect of the distal patella and the tibial tuberosity by impacting with a tappet (Fig 6C). An absorbable suture (No. 0 Vicryl; Ethicon, Somerville, NJ) is used to close the superficial patellar tendon and the paratenon with a locking configuration and the knee flexed to 90°. Interrupted, absorbable subcutaneous suturing and routine skin closure follow.
Discussion
We have described an anatomic ACL reconstruction technique using patellar tendon autograft, which facilitates both graft-tunnel healing through direct bone-on-bone contact and clinical practicability through a secure fixation technique. Pearls and pitfalls are listed in Table 1.
Table 1.
Pearls and Pitfalls
| Surgical Step | Pearls | Pitfalls |
|---|---|---|
| Graft harvest | ||
| Tibial tuberosity | The surgeon should harvest a bone block that is no longer than 20 mm because it could exceed the total tunnel length. | If the distal bone block overhangs the tibial tunnel, a curved chisel can be used to create a socket within the tibia, allowing the bone block to seat flush with the tibial cortex. |
| Patella | The surgeon should avoid harvesting a superficial bone block from the distal patella when using the oscillating two-thirds toothed hollow saw. | The upper edge of the hollow saw can be pressed down to the level of the insertion of the patellar tendon during harvesting. |
| Femoral tunnel | ||
| Drilling | The surgeon should set the femoral FlipCutter guide to 115°-120° to avoid a killer angle of the femoral tunnel. This eases press-fit insertion of the bone block. | A suture grasper can be used to exactly align the bone block with the entrance of the femoral tunnel before the TightRope is pulled. |
| Socket length | The length of the socket should exceed the total length of the bone block by about 2 mm. | Because the femoral socket is oval, the bone block cannot be fully seated into the tunnel if the length exactly matches the length of the femoral bone block. |
| Tibial tunnel | The use of a 60° aimer ensures sufficient tibial tunnel length. | When the tibial tunnel is short, care must be taken so that the total graft length does not exceed the tunnel length, with the tibial bone block overhanging the tunnel entrance. |
| Graft preparation | The surgeon should place the drill hole centrally within the patellar bone block. | A drill hole placed too proximally might lead to breakage of the bone block when the BTB TightRope is pulled. |
| Graft insertion | When the 9.4-mm trephine is used for harvesting, dilating the tibial tunnel entrance to 10 mm (i.e. with a 10-mm drill tip) facilitates introducing the graft into the tibial tunnel. | It is essential to fully seat the bone block into the femoral socket before shortening the loop strands; otherwise, the bone block might become stuck at the tunnel entrance. |
| Graft fixation | Using a low medial portal (as in the anteromedial drilling technique) with a femoral tunnel at 115°-120° provides the possibility of using an interference screw for femoral fixation if a small and superficial bone block has been harvested. |
Graft Choice
Apart from an ongoing discussion about different graft-harvesting techniques, with advantages and disadvantages regarding donor-site morbidity, the graft structure (i.e. hamstring grafts with a round and tubular structure vs the flat and ribbonlike form of quadriceps tendon and patellar tendon grafts) is gaining importance.7 In patients aiming to return to pivoting sports, control of rotational instability of the knee is the key to a successful return to preinjury activity levels. Recent clinical and biomechanical results have shown that the (functional) double-bundle or fanlike shape of a graft tends to more closely restore normal ACL function.8 Owing to a lower revision rate, reduced graft elongation, and better return to the preinjury level of activity in earlier studies, the BPTB graft plays an important role especially in the young and active patient.3,9, 10, 11
Biological Benefits and Press-Fit Technique
We believe that direct bone-to-bone healing of an intact ligament insertion reduces the weakness of soft-tissue grafts (without bone blocks) of delayed or impaired graft-tunnel healing, which may cause graft insufficiency, elongation, or delayed ligamentization of the graft. Ideal bone-to-bone healing is achieved when bone blocks are fixed with press-fit techniques,12 additionally avoiding bony defects or potential tunnel widening.13 Surgical techniques for and clinical results of press-fit and implant-free ACL reconstruction have been previously published, and interest in biologically more advantageous ACL reconstruction clearly exists.4 Still, press-fit fixation of an ACL graft can be a challenging and time-consuming procedure, leading to low clinical acceptance. The described outside-in, retrograde drilling technique allows straightforward and reproducible tunnel placement. With secondary extracortical fixation on the femoral side and tibial side, this technique provides direct bone-on-bone healing without the need for a perfect press-fit fixation, which provides a great advantage in the setting of clinical routine in terms of applicability and time management.
Bone Defects
One of the disadvantages of traditional BPTB and quadriceps tendon–bone grafts is caused by creating bony defects during graft harvesting, which might lead to kneeling pain.1 These donor-site morbidities have long been the reason for investigations concerning treatment strategies lacking satisfactory results.14 Our technique addresses the bony defects by refilling the removal sites with the bone collected during graft harvesting using hollow saws.
Limitations
Our technique represents a biologically favorable situation of direct bone-to-bone healing without the “interference” of fixation screws within the tunnels. Although this definitely leads to an unproblematic situation in possible revision surgery, it is unclear if there is clinical benefit to well-established screw fixation, therefore questioning the additional instrument costs and surgery time for optimal graft preparation.
Secondarily, BPTB graft harvesting might have higher donor-site morbidity.15 In our technique, we tried to accommodate for this problem by refilling the harvest sites with bone material. Still, all possible causes of anterior knee pain are not addressed by this, so donor-site morbidity could still be higher than with ACL reconstruction with hamstring tendon.
In conclusion, the presented ACL reconstruction technique enables safe, reproducible, and anatomic fixation of the BPTB autograft providing the biological and biomechanical benefits of bone-to-bone healing. In addition, donor-site morbidities, which constitute a disadvantage of traditional BPTB graft use, are addressed by refilling the harvest sites.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.O. receives personal fees from Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is in the supine position; a thigh tourniquet is used, allowing 120° of knee flexion. Anterior cruciate ligament (ACL) surgery is performed in a right knee in this patient. We perform a standard midline incision harvesting the central third of the patellar tendon. An approximately 20-mm-long bone block from the tibial tuberosity is harvested by use of small oscillating saw blades; it can be separated with a chisel. After removal of excess bone material, which can later be used to refill the harvest site, 2 drill holes are made, and a suture is passed through the bone block. The threads are pulled into the hollow saw (9.4 mm in this case) using a guidewire, and the graft is now introduced. With an oscillating trephine (Richard Wolf), a 15- to 20-mm cylindrical bone block is harvested from the distal patella and separated by elevation or with the use of an osteotome. The tibial bone block is prepared to narrow the free end. A No. 2 FiberLoop is used to place a whipstitch within the ligament portion of the graft; one end of the suture is passed to the other side of the graft using the straight FiberLoop needle. A second No. 2 FiberWire is placed within the tibial bone block, whereby 2 independent suture pairs are available for later graft fixation. The cylindrical patellar bone block is shaped with a rasp for femoral press-fit fixation so that the tip just fits the entrance of a 9-mm template (when the 9.4-mm hollow saw is used, as in this case). In the next step, a BTB TightRope is placed within a 2-mm drill hole in the center of the cylindrical bone block. The final graft construct is stored in a vancomycin-soaked surgical swab. After routine arthroscopic examination, the lateral notch is cleared of remnant fibers with a shaver and electrocautery, and the femoral drill guide is placed at the center of the ACL footprint. By an outside-in technique, with a FlipCutter, a 3.5-mm drill hole is created, and after correct positioning is ensured, a socket matching the length of the bone block (9 mm in this case) is drilled after the drill bit is unfolded and the FlipCutter is pulled back. Bone debris is cleared, a TigerStick (Arthrex) is introduced into the tunnel, and a TigerWire suture (Arthrex) is pulled out the lateral portal and secured with a clamp. We now proceed to create the tibial tunnel. With a 60° aimer (as used in this case) or, alternatively, a standard adjustable aimer, a 2.5-mm guidewire is placed in the center of the tibial ACL footprint. A centering device for the hollow saw is brought over the guidewire after changing the drill sleeve, and now, the 9.5-mm trephine can be used. After completion of the tibial tunnel, the bone cylinder is freed from soft tissue with electrocautery so that it can be easily pulled out of the tunnel. The harvested bone material can now be prepared to refill the harvest site at the distal patella and to fill the tibial tunnel at a later stage of the operation. This is again performed with the small oscillating saw blade used for harvesting. A short bone cylinder, matching the length of the harvest site at the distal patella, is prepared; the remainder will later be used to refill the tibial tunnel. After retrieval of the shuttling suture (TigerWire) through the tibial tunnel with a suture grasper, the graft can be inserted. Care must be taken not to shorten the white strands of the BTB TightRope at this stage; otherwise, the bone block might become stuck at the entrance of the femoral tunnel. The femoral (cylindrical) bone block must now be rotated and angulated in the direction of the femoral tunnel; it can then be pulled into the femoral socket. If the bone block becomes stuck, after correct alignment with the tunnel is ensured, an arthroscopic tappet may be used to engage the graft into the femur. Now, the BTB TightRope button is pulled back to the lateral femoral cortex by shortening the white strands. When doubt exists, an image intensifier can be used to ensure correct cortical positioning of the button. Final tibial, extracortical graft fixation is performed using 2 independent suture anchors (SwiveLock, 4.75 mm, bio-composite) for the 2 suture pairs. The tibial canal is then refilled, by a press-fit technique, with the bone harvested from tunnel creation to achieve direct bone-on-bone healing of the graft. The distal pole of the patella is exactly refilled with remaining bone material. A tappet is used for fixation. Final graft tension is evaluated arthroscopically, before standard closure of the patellar tendon is performed with the paratenon at 90° of knee flexion. Subcutis and skin closure is performed in a standard fashion.
References
- 1.Wipfler B., Donner S., Zechmann C.M., Springer J., Siebold R., Paessler H.H. Anterior cruciate ligament reconstruction using patellar tendon versus hamstring tendon: A prospective comparative study with 9-year follow-up. Arthroscopy. 2011;27:653–665. doi: 10.1016/j.arthro.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 2.Sheean A.J., Musahl V., Slone H.S. Quadriceps tendon autograft for arthroscopic knee ligament reconstruction: Use it now, use it often. Br J Sports Med. 2018;52:698–701. doi: 10.1136/bjsports-2017-098769. [DOI] [PubMed] [Google Scholar]
- 3.Gifstad T., Foss O.A., Engebretsen L. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: A registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014;42:2319–2328. doi: 10.1177/0363546514548164. [DOI] [PubMed] [Google Scholar]
- 4.Boszotta H. Arthroscopic anterior cruciate ligament reconstruction using a patellar tendon graft in press-fit technique: Surgical technique and follow-up. Arthroscopy. 1997;13:332–339. doi: 10.1016/s0749-8063(97)90030-x. [DOI] [PubMed] [Google Scholar]
- 5.Robin B.N., Jani S.S., Marvil S.C., Reid J.B., Schillhammer C.K., Lubowitz J.H. Advantages and disadvantages of transtibial, anteromedial portal, and outside-in femoral tunnel drilling in single-bundle anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2015;31:1412–1417. doi: 10.1016/j.arthro.2015.01.018. [DOI] [PubMed] [Google Scholar]
- 6.Lanzi J.T., Felix J., Tucker C.J. Comparison of the suture anchor and transosseous techniques for patellar tendon repair: A biomechanical study. Am J Sports Med. 2016;44:2076–2080. doi: 10.1177/0363546516643811. [DOI] [PubMed] [Google Scholar]
- 7.Śmigielski R., Zdanowicz U., Drwięga M., Ciszek B., Ciszkowska-Łysoń B., Siebold R. Ribbon like appearance of the midsubstance fibres of the anterior cruciate ligament close to its femoral insertion site: A cadaveric study including 111 knees. Knee Surg Sports Traumatol Arthrosc. 2015;23:3143–3150. doi: 10.1007/s00167-014-3146-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moulton S.G., Steineman B.D., Haut Donahue T.L., Fontboté C.A., Cram T.R., LaPrade R.F. Direct versus indirect ACL femoral attachment fibres and their implications on ACL graft placement. Knee Surg Sports Traumatol Arthrosc. 2017;25:165–171. doi: 10.1007/s00167-016-4188-9. [DOI] [PubMed] [Google Scholar]
- 9.Feller J.A., Webster K.E. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:564–573. doi: 10.1177/03635465030310041501. [DOI] [PubMed] [Google Scholar]
- 10.Webster K.E., Feller J.A., Hartnett N., Leigh W.B., Richmond A.K. Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: A 15-year follow-up of a randomized controlled trial. Am J Sports Med. 2016;44:83–90. doi: 10.1177/0363546515611886. [DOI] [PubMed] [Google Scholar]
- 11.Cristiani R., Sarakatsianos V., Engström B., Samuelsson K., Forssblad M., Stålman A. Increased knee laxity with hamstring tendon autograft compared to patellar tendon autograft: A cohort study of 5462 patients with primary anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:381–388. doi: 10.1007/s00167-018-5029-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boszotta H., Anderl W. Primary stability with tibial press-fit fixation of patellar ligament graft: An experimental study in ovine knees. Arthroscopy. 2001;17:963–970. doi: 10.1053/jars.2001.25955. [DOI] [PubMed] [Google Scholar]
- 13.Akoto R., Müller-Hübenthal J., Balke M. Press-fit fixation using autologous bone in the tibial canal causes less enlargement of bone tunnel diameter in ACL reconstruction—a CT scan analysis three months postoperatively. BMC Musculoskelet Disord. 2015;16:200. doi: 10.1186/s12891-015-0656-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walters B.L., Porter D.A., Hobart S.J. Effect of intraoperative platelet-rich plasma treatment on postoperative donor site knee pain in patellar tendon autograft anterior cruciate ligament reconstruction: A double-blind randomized controlled trial. Am J Sports Med. 2018;46:1827–1835. doi: 10.1177/0363546518769295. [DOI] [PubMed] [Google Scholar]
- 15.Mouarbes D, Menetrey J, Marot V, Courtot L, Berard E, Cavaignac E. Anterior cruciate ligament reconstruction: A systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone–patellar tendon–bone and hamstring-tendon autografts [published online February 21, 2019]. Am J Sports Med. doi:10.1177/0363546518825340. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is in the supine position; a thigh tourniquet is used, allowing 120° of knee flexion. Anterior cruciate ligament (ACL) surgery is performed in a right knee in this patient. We perform a standard midline incision harvesting the central third of the patellar tendon. An approximately 20-mm-long bone block from the tibial tuberosity is harvested by use of small oscillating saw blades; it can be separated with a chisel. After removal of excess bone material, which can later be used to refill the harvest site, 2 drill holes are made, and a suture is passed through the bone block. The threads are pulled into the hollow saw (9.4 mm in this case) using a guidewire, and the graft is now introduced. With an oscillating trephine (Richard Wolf), a 15- to 20-mm cylindrical bone block is harvested from the distal patella and separated by elevation or with the use of an osteotome. The tibial bone block is prepared to narrow the free end. A No. 2 FiberLoop is used to place a whipstitch within the ligament portion of the graft; one end of the suture is passed to the other side of the graft using the straight FiberLoop needle. A second No. 2 FiberWire is placed within the tibial bone block, whereby 2 independent suture pairs are available for later graft fixation. The cylindrical patellar bone block is shaped with a rasp for femoral press-fit fixation so that the tip just fits the entrance of a 9-mm template (when the 9.4-mm hollow saw is used, as in this case). In the next step, a BTB TightRope is placed within a 2-mm drill hole in the center of the cylindrical bone block. The final graft construct is stored in a vancomycin-soaked surgical swab. After routine arthroscopic examination, the lateral notch is cleared of remnant fibers with a shaver and electrocautery, and the femoral drill guide is placed at the center of the ACL footprint. By an outside-in technique, with a FlipCutter, a 3.5-mm drill hole is created, and after correct positioning is ensured, a socket matching the length of the bone block (9 mm in this case) is drilled after the drill bit is unfolded and the FlipCutter is pulled back. Bone debris is cleared, a TigerStick (Arthrex) is introduced into the tunnel, and a TigerWire suture (Arthrex) is pulled out the lateral portal and secured with a clamp. We now proceed to create the tibial tunnel. With a 60° aimer (as used in this case) or, alternatively, a standard adjustable aimer, a 2.5-mm guidewire is placed in the center of the tibial ACL footprint. A centering device for the hollow saw is brought over the guidewire after changing the drill sleeve, and now, the 9.5-mm trephine can be used. After completion of the tibial tunnel, the bone cylinder is freed from soft tissue with electrocautery so that it can be easily pulled out of the tunnel. The harvested bone material can now be prepared to refill the harvest site at the distal patella and to fill the tibial tunnel at a later stage of the operation. This is again performed with the small oscillating saw blade used for harvesting. A short bone cylinder, matching the length of the harvest site at the distal patella, is prepared; the remainder will later be used to refill the tibial tunnel. After retrieval of the shuttling suture (TigerWire) through the tibial tunnel with a suture grasper, the graft can be inserted. Care must be taken not to shorten the white strands of the BTB TightRope at this stage; otherwise, the bone block might become stuck at the entrance of the femoral tunnel. The femoral (cylindrical) bone block must now be rotated and angulated in the direction of the femoral tunnel; it can then be pulled into the femoral socket. If the bone block becomes stuck, after correct alignment with the tunnel is ensured, an arthroscopic tappet may be used to engage the graft into the femur. Now, the BTB TightRope button is pulled back to the lateral femoral cortex by shortening the white strands. When doubt exists, an image intensifier can be used to ensure correct cortical positioning of the button. Final tibial, extracortical graft fixation is performed using 2 independent suture anchors (SwiveLock, 4.75 mm, bio-composite) for the 2 suture pairs. The tibial canal is then refilled, by a press-fit technique, with the bone harvested from tunnel creation to achieve direct bone-on-bone healing of the graft. The distal pole of the patella is exactly refilled with remaining bone material. A tappet is used for fixation. Final graft tension is evaluated arthroscopically, before standard closure of the patellar tendon is performed with the paratenon at 90° of knee flexion. Subcutis and skin closure is performed in a standard fashion.