Abstract
We tend to study health inequalities as differentials in disease and death that exist within a population. But the most important cause of health inequality is social stratification, and social stratification only varies between populations. Here, I highlight a way forward in the study of health inequality that resolves this mismatch of analytical levels: we must study the fundamental causes as systems of exposure. Through this critical review of the literature, I argue that the explicit study of variation in social stratification is the next frontier in research on fundamental causes of health inequality.
Keywords: Fundamental cause theory, Social determinants, SES, Social stratification, Racial hierarchy, Systems thinking
Highlights
-
•
Research on Fundamental Cause Theory suffers from two major pitfalls.
-
•
The most important cause of health inequality is social stratification.
-
•
Scholars incorrectly assume social stratification is static.
-
•
Social stratification varies between populations, not within them.
-
•
Study of variation in social stratification will advance health inequality research.
Introduction
Health inequalities are differentials in disease and death that exist within a population. But the most important cause of health inequality is social stratification, and social stratification only varies between populations. Thus, as scholars of health inequality, we encounter a mismatch between the level of analysis we think about, and the level of analysis we must study to reveal the mutability of fundamental cause associations. Here, I highlight a way forward in the study of health inequality that resolves this dilemma. I argue that the explicit study of variation in social stratification is the next frontier in research on fundamental causes of health inequality.
The article proceeds in the following way. First, I consider Fundamental Cause Theory as the theoretical basis for the approach I advocate. I highlight two common pitfalls in the application of Fundamental Cause Theory that limit insight into the mutability of health inequalities. Second, I introduce the system of exposure concept. Then, I briefly review some key lessons from the past that inform my call to study systems of exposure. Next, I highlight four studies that succeed in using population-level comparison to reveal the influence of social stratification on health. Finally, I discuss the benefits of this approach for future research.
Fundamental Cause Theory
Since its introduction in 1995, Fundamental Cause Theory has grown into, arguably, the most developed theoretical model of how social inequality produces health inequality. Fundamental Cause Theory (FCT) is a theoretical attempt to resolve the puzzle of why social inequalities in health (e.g., the socioeconomic gradient in mortality) persist despite medical innovation and disease elimination (Link and Phelan 1995). According to FCT, it is social inequality in access to flexible social resources (in particular, wealth, income, education, and racial privilege) that drives population health inequalities. Individuals with high social status can deploy their resources to avoid disease, seek treatment, and adopt healthy behaviors. And while FCT has given us an excellent model for how social conditions map onto health, it has yet to deliver on its original mission to disrupt notions that health inequality is inevitable. Instead, FCT has been used by scholars to frame health inequalities with a new kind of inevitability – one based in the assumed stability of social stratification rather than biological determinism – but it is an inevitability, nonetheless.
Scholars of health inequality are seemingly stuck comparing subgroups and documenting disparities attributable to socioeconomic status (SES) or race or gender. Few of the many studies that apply FCT explore variation in the fundamental causes themselves (i.e., variation in racial hierarchy). Instead, the literature continues to confirm the existence of the fundamental cause associations. On one hand, it is great progress to show that fundamental cause associations exist and drive health inequalities. On the other hand, as the evidence accumulates documenting the health inequalities that result from socioeconomic inequality and racism and residential segregation, these fundamental cause associations can seem fixed and intractable. Thus, in its emphasis on the persistence of socioeconomic inequalities in health, research that applies FCT can perpetuate the assumption that social stratification is static.
Goal: study dynamics in fundamental cause associations
FCT has inspired an exciting area of research on the ways that social policy can intervene to disrupt the social production of health inequality. This research is focused on social policies that weaken fundamental cause associations by ensuring universal access to the social determinants of health regardless of an individual’s social resources, power, or privilege. For example, studies have shed light on the ways that school desegregation (Liu, Linkletter, Loucks, Glymour, & Buka, 2012), anti-immigrant laws (Torche & Sirois, 2019), unemployment insurance (Cylus, Glymour, & Avendano, 2014), and state policy regimes (Montez, Anna, Hayward, Woolf, & ChapmanBeckfield, 2019) can prevent or exacerbate social stratification from turning into health inequalities, even without any direct intervention on the system of social stratification itself.
But this focus on policies that disrupt the extent to which individuals can “buy” their way into good health is only one side of the equation. The associations between a fundamental cause and health inequalities can change in not one, but two main ways: either what a particular position within the stratification system means for health can change, or the patterning of the underlying stratification system itself can change. While research on the first type of change is advancing, there has been limited attention to the second type of change. The ways that the patterning of social stratification itself can change has been a more elusive area of study for health researchers.
Why has there been limited attention among health researchers to social policies and unplanned social changes that flatten systems of social hierarchy? I think there are two reasons for the neglect that have their basis in how we conceptualize fundamental causes. First is the tendency to accept the existence of fundamental causes, such as socioeconomic stratification, as natural. Second is the usual mismatch between our level of analysis in studying fundamental causes and the level at which stratification systems are defined. These common practices restrict the potential for studies to reveal the mutability of health inequalities. In this article, I propose reframing fundamental causes as systems of exposure in order to resolve these two common pitfalls in the application of FCT.
Pitfall 1: assuming social inequality is static
The study of fundamental causes has helped change thinking in the medical and public health communities away from biological determinism. Instead of searching for the roots of health disparities in genetics, proponents of FCT generally locate the roots of health disparities in social inequality. This is indeed progress that should be celebrated. Yet scholars have failed to use FCT to overcome the assumption that there is something immutable about disparities by gender, race, and social class in health. Perhaps this is because researchers merely transfer their assumptions about the basis for the fixed nature of inequalities in health from biology to social stratification. And among many health professionals, social stratification is assumed to be just as immutable as genetics.
Like draping a cloth over a table, health trends reveal the shape of even hidden systems of social stratification. Herein lies an opportunity. Population health data can be used to study shifts in otherwise elusive systems of social stratification. But this requires researchers to consider the ways that fundamental cause gradients are context-specific and dynamic. Alas, current theory and methods in epidemiology and medical sociology make it easy to accept that there is a “natural” order to social inequalities in health. This is evident in the way health disparities researchers make comparisons to a White reference group unquestioningly; and in the way that the persistence of Black-White or Native American-White disparities in health and life expectancy are taken as the way things are; and in the tendency to view any divergence from White advantages in health as a paradox (See Palloni & Morenoff, 2001 critique of the ‘Hispanic Mortality Paradox’) or puzzle (See Navarro’s 2019 critique of Case and Deaton’s ‘deaths of despair’ puzzle) or to ignore them completely (e.g., See Chen & Hawks, 1995 regarding stereotypes about Asian American and Pacific Islander health). Although the public health literature does show increasing comfort with the idea that race is a social construct, race is still conceptualized as a fixed individual-level trait. Health researchers lack models that reject notions of a natural social order and instead take the social construction of racial stratification, and other forms of stratification, as a starting point.
Racial identities, for example, are constantly being renegotiated and reformulated with consequences for population-level rules (de facto and de jure) of social exclusion. For instance, following World War II, political organizing and mobilization transformed racial stratification in the U.S. (Omi & Winant, 2014). Uprisings in the 1950s and 1960s challenged the Jim Crow-based system of white supremacy and succeed in achieving partial reforms (Omi & Winant, 2014). Health is surprisingly sensitive to even such subtle shifts in racial order. So while white supremacy continues in the U.S., there are both acute and gradual shifts in racial and ethnic stratification that have occurred in recent decades that have consequences for health inequality. For example, a change in ethnic stratification occurred during the postwar period with the absorption of hyphenated Whites into an undifferentiated White majority. But just as ethnic distinctions can lose their power to differentiate and exclude, ethnic distinctions can emerge as a new basis for social exclusion and, in turn, for health. The attacks of September 11, 2001, major immigration raids, and anti-immigrant laws are each examples of events that transform the links between ethnic hierarchy and health, or between immigration status and health. Thus, studies of these dynamics in systems that stratify and oppress can be very instructive for understanding the social production of health inequality. While less common, there is research is being done that avoids the pitfall of assuming social stratification is static. Later in this essay, I highlight four examples from the literature that explore the health consequences of a change in the patterning of a system of social stratification.
Pitfall 2: mismatched levels of analysis
Health inequalities are differentials in disease distribution among subgroups or between different social locations that exist within a population. Yet the most salient cause of health inequality is social stratification which only varies between populations. This mismatch of levels of analysis has confused efforts by researchers committed to understanding social inequalities in health. Our research suffers from “the streetlight effect” – an observational bias to look for things where there is light, not where we are most likely to find what we are looking for. This is why the study of fundamental causes has been limited up to this point. But an opening can be found in Rose’s (1985) call to study ubiquitous causes across populations and in a related call for systems thinking in health research (Diez Roux, 2007). Detecting variation in stratification systems is impossible with research designs that compare individuals, yet the individual-level is the most common level of analysis for studying the fundamental causes of health inequality. In order to advance research that reveals how health inequalities within a population are modifiable, we actually must look across populations.
Solution: reframe fundamental causes as systems of exposure
So how do we move beyond documenting the influence of fundamental causes to exploring their mutability? I propose we build on FCT to reframe fundamental causes as systems of exposure to the determinants of health that vary across populations. We can resolve the two common pitfalls in applications of FCT by recognizing a special case of fundamental causes that are actually ubiquitous causes: stratification systems. The patterning that stratification systems exhibit within a population can trick us into thinking that their influence on health can be studied by comparing subgroups within a population. Indeed, it is tempting to think of fundamental causes as we do any other risk factor or exposure: as a determinant of health risk that is either present or absent. But some fundamental causes, such as racism, are not merely exposures. Rather, they are systems of exposure – not everyone is exposed to the same disease agents, but everyone is included in the system that shapes exposure to the determinants of health.
Accordingly, my proposition is this: to the extent that a particular fundamental cause stratifies exposure to the determinants of health, we should think of it as a system of exposure, not an individual trait. Stratification systems are actually population-level attributes so they must be studied across populations or population moments– a glimpse of a population in a particular spatiotemporal context. This approach offers ways to address the constraints that come from an intense focus on fundamental causes without an equally intense focus on population-level analysis. It can be intimidating to theorize about social stratification systems. This is why I propose thinking instead about systems of exposure, a concept that emerges directly from the epidemiology and medical sociology literatures. It invites health scholars to acknowledge that stratification systems are dynamic and to think explicitly about temporal and geographic variation in stratification systems.
Origins: how the systems of exposure concept integrates insights from the past
In 1985, sociologist Stanley Lieberson introduced the idea of basic causes, which he distinguished from superficial causes. Lieberson cautioned, “it is rarely possible to distinguish between basic and superficial causes if the research is working exclusively with data for a single point in time” (Lieberson, 1985:186). House, Lepkowski, Kinney, Mero, Kessler, and Herzog (1994) picked up on Lieberson’s idea of basic causes in their paper on socioeconomic stratification in health and aging. House and colleagues called for “comparative and historical research on variation in social stratification” which is precisely what I advocate for in this essay (House et al., 1994:230). A year later, Link and Phelan (1995) introduced Fundamental Cause Theory to explain how individuals with higher SES can translate their social privilege into better health regardless of changes in the disease landscape.
Meanwhile, epidemiologist Geoffrey Rose (1985) published a now classic piece, “Sick Individuals, Sick Populations.” In the article, and further elaborated in his 1992 book (Rose, 1992), Rose describes the challenge of studying the influence of ubiquitous causes with our tendency for individual-level comparison. Rose (1985) argues that it is the “mass influences” which are ubiquitous in a population, as opposed to individual risk factors, that explain differences between population distributions of disease. He uses the example of a population distribution of hypertension in England and Kenya to point out that simply comparing two Englanders, one case and one control, and asking why one has hypertension and the other does not will not reveal why England has much more hypertension than Kenya. To see the effect of “England” on hypertension, we need to compare to a population distribution that does not share the uniform exposure to England.
Rose explains that the study of ubiquitous causes requires comparison at the scale at which the exposure varies (1992). For example, we cannot effectively study the effect of American culture on premature mortality by comparing one American who died prematurely to another who did not. Generally speaking, ubiquitous exposures that act on the population as a whole and which are uniformly distributed do not shape within-population health inequalities. Rather, they drive inequalities between populations. A good example of a uniformly-distributed ubiquitous cause can be found in electrification in the U.S. Electrification influences the health of all Americans, but it is no longer an important sources of health inequality because it is uniformly distributed (or close to it). Uniformly-distributed ubiquitous causes are the most difficult to detect because standard methods for causal inference leverage heterogeneity of exposure. Thus, to detect a fundamental cause that is ubiquitous, it must either be differentiated, or we must compare across populations. In 2004, Diez Roux re-issued Rose’s call for the comparison of different populations to investigate population-level attributes (Diez Roux 2004). My proposal to reframe fundamental causes as systems of exposure draws on these insights about the importance of population-level comparison.
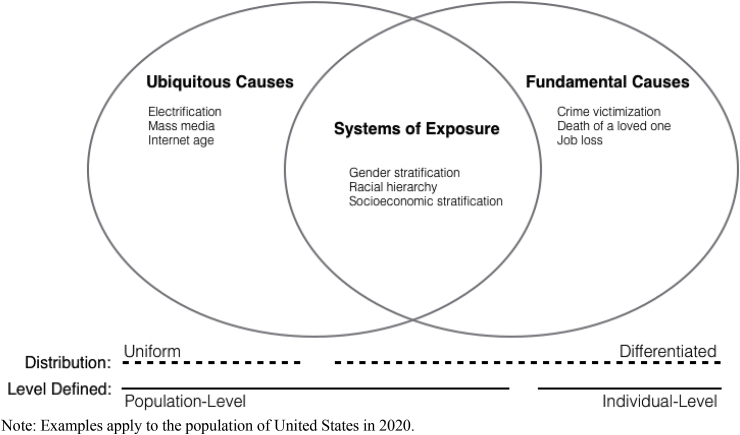
As I depict in Fig. 1, stratification systems sit at the intersection of ubiquitous causes and fundamental causes. While there is similarity in the motivation behind Rose’s conceptualization of ubiquitous causes and Link and Phelan’s fundamental causes, they are distinct concepts. According to Rose (1992), ubiquitous causes explain the incidence rate of disease in a population and they can be used to understand the basis for differences in disease incidence between populations. Link and Phelan’s fundamental causes explain the differential incidence of disease between population subgroups (Link and Phelan 1995). But what I want to emphasize is that there is a special case of fundamental causes which are inescapable and should be studied as systems of exposure, namely, stratification systems.
Fig. 1.
Where Systems of Exposure Fit Into Existing Theory
Note: Examples apply to the population of United States in 2020.
It may be helpful to clarify here what I mean by stratification. Massey defines stratification as “the unequal distribution of people across social categories that are characterized by differential access to scarce resources” (Massey, 2007:1). Stratification systems order social categories such that higher positions get more access to social resources and power, at the expense of the lower order positions. This results in social inequality. Stratification systems are defined at various social scales and they vary greatly across populations and over time.
Stratification systems are special because they can be conceptualized as both ubiquitous causes and fundamental causes. As such, they can help us uncover both causes of population incidence rates (which satisfies Rose, 1985) and causes of health inequality (which satisfies Link and Phelan 1995). We find systems of exposure in a population well-circumscribed in time and space. Local systems of racial hierarchy are systems of exposure. National systems of gender stratification are systems of exposure. The stratification of regions within the U.S. is a system of exposure. Ultimately, they are the systems that determine the patterning of social resources and power.
Stratification systems are distinct from other ubiquitous causes in that they do not have a uniform distribution across a population. Their differentiated patterning is precisely what is dynamic and, thus, extremely useful for health researchers if studied explicitly using systems thinking. The term “systems of exposure” reminds us we cannot study these exposures as we do individual-level risk factors. All of us hold positions in stratification systems. There is no absence of exposure.
Not all fundamental causes are systems of exposure that only vary between populations. In the landmark paper that introduced Fundamental Cause Theory, Link and Phelan list job loss, crime victimization, and death of a loved one, along with socioeconomic status as examples of fundamental causes (Link and Phelan 1995). But of these original examples, only socioeconomic status is a system of exposure. This is because a system of exposure is a type of fundamental cause that is inescapable at the individual level – it is ubiquitous. Job loss is not a ubiquitous cause because some individuals are exposed to job loss events and spells of unemployment, while others are not. While the social meaning of job loss certainly varies across populations, job loss is not easily conceptualized as a stratification system. Similarly, crime victimization and death of a loved one are not ubiquitous causes. These, in themselves, are not population-level attributes that can be compared across populations.
With this essay, I urge scholars to move away from studying ubiquitous, fundamental causes as if they were individual traits that carry the same consequences regardless of context. Instead, we should theorize these as variable systems that shape our exposure to the social determinants of health. Other scholars have issued similar calls to better theorize the influence of race in health inequality by focusing on intersectionality (Pearson, 2008) and by “conceptualizing racism based on how it operates in the period of interest to the study” (Ford & Airhihenbuwa, 2010:1392). For example, according to Ford and Airhihenbuwa’s Public Health Critical Race praxis, arguably the most developed application of Critical Race Theory to public health, “efforts to understand inequities in the 1950s should reflect how racialization operated then, while research on inequities in the 2000s should be based on contemporary characteristics” (Ford & Airhihenbuwa, 2010:1392). The work of Hatzenbueler on structural stigma also emphasizes the way stigma is context-specific in that it focuses on the “societal-level conditions, cultural norms, and institutional policies that constrain the opportunities, resources, and well-being of the stigmatized” (Hatzenbuehler, 2016:742). Instead of conceptualizing fundamental causes as stigmatizing characteristics, I advocate a relational approach that considers the relative locations of Whiteness or Blackness within a population’s system of racial hierarchy. Similar recommendations have been made before. For example, in his thoughtful 2008 essay, Pearson explains, “when thinking about differentials in health, race is best conceptualized not as an individual or even group characteristic, but as a relational one among groups located within a given social hierarchy” (Pearson, 2008:33). And drawing on Intersectionality Theory (Crenshaw, 1989), the systems-of-exposure approach emphasizes that an individual’s health is determined by their relative location within intersecting social hierarchies.
Fundamental causes as systems of exposure
Systems-of-exposure thinking is an extension of Fundamental Cause Theory. As such, the careful theorizing about pathways between SES or race and health that has been done as part of FCT applies here (See, for example, Clouston, Rubin, Phelan, & Link, 2016; Phelan, Link, & Parisa, 2010; Phelan & Link, 2015). FCT describes the way that flexible social resources can be converted into health via multiple mechanisms affecting multiple health outcomes. It is through the differentiated allocation of social resources that stratification systems influence disease susceptibility. One’s racial privilege or socioeconomic status are almost like coordinates that indicate their location in intersecting systems of differential exposure. For example, the system of racial hierarchy in the U.S. today, especially in the ways it intersects with class and gender privilege, differentiates access to stable housing, nutrition, and education. It also differentiates protection from toxic exposures and violence. Thus, a system of exposure is best conceptualized as a variable that differentiates exposure to the social determinants of health. The system-of-exposure framing makes it easier to study both ends of the spectrum of exposure (from socially advantaged to socially disadvantaged).
Those of us concerned with health equity should be especially concerned with differential exposure to the social determinants of health that is based in ascribed characteristics such as race, ethnicity, gender, sexual orientation, caste, the social class of our parents, height, disability status, and appearance – the properties that are involuntary; we do not choose them. We should also pay attention to the many ways ascribed characteristics can be further activated through their intersection with other kinds of stratification such as income inequality, educational inequality, nativity, legal status, and contact with the criminal justice system.
How: articulating systems of exposure
The system-of-exposure concept invokes systems thinking; this is on purpose. There has been growing interest in systems theory among health scholars (Diez Roux, 2007, 2008, 2015). General systems theory involves intentionally studying a system’s dynamics and evolution. Systems theory takes a holistic approach and does not reduce systems to simply the sum of their parts. In these ways, systems thinking is “a healthy antidote to the obfuscation that can result from too much simplification” (Diez Roux, 2015:101), but also a way to handle greater complexity.
By thinking of a fundamental cause such as structural racism as a system, we can more easily think of its properties: a) What is the system’s patterning (e.g., continuous, threshold, dichotomous, ordinal)? b) At what scale is the system defined (e.g., national, regional, state, local)? c) How is the system maintained or enforced? d) How do we theorize the system’s influence on susceptibility (e.g., cumulative, fixed, reversible, critical periods, dynamic over the life course)? This simple reframing of fundamental causes as systems of exposure urges us to theorize more clearly how we expect fundamental causes to vary, and then to conduct studies designed to detect that variation.
Scale
When we think about the scale at which to study a system of exposure, we should ask: 1) At what level is the system assigned meaning? 2) At what level can this meaning be transformed or disrupted? 3) At what level could we intervene? The scale can be any social unit large enough to have its own norms, rules, and patterning, as well as its own distribution of disease. Adapting Matthew’s concept of “spatial polygamy” (Matthews, 2011), people belong to multiple nested and non-nested, social and geographic, past and present contexts. Each of these can be studied as a population. For example, racial hierarchy as a system of exposure can be studied at the scale of New Orleans, Louisiana, the South, or the U.S. Each of these levels represents a distinct population unit with its own system of racial hierarchy that exerts an inescapable influence on its members. Granted, the nesting of the population scales results in tremendous similarity and influence between each system of racial hierarchy, but there are also subtle distinctions that can be studied to reveal important insights about power and health. For example, racial disparities in teen pregnancy can be studied immediately before and immediately after the transitions away from de jure racial segregation (Liu, Linkletter, Loucks, Glymour, & Buka, 2012). This particular study found that the temporal change in the intersecting systems of racial and educational stratification reduced health inequality (Liu, Linkletter, Loucks, Glymour, & Buka, 2012). Another recent study compared the educational gradient in chronic disease across four time periods in Brazil and found evidence that a gradual weakening of the educational gradient resulted in smaller educational inequalities in chronic disease (Beltrán-Sánchez & Andrade, 2016). In this example, the place-time coordinates compared were: Brazil 1998, Brazil 2003, Brazil 2008 and Brazil 2013.
As Beltran-Sanchez and colleagues demonstrate, an advantage of transnational comparisons is that they allow us to study the effect of social inequality on health in populations with very different systems of social stratification. Especially now that researchers have access to harmonized survey data from different countries, it makes sense to use transnational comparison to study how systems of exposure vary. But transnational comparison introduces new challenges too. For one, there is the risk of flawed analysis due to a poor understanding of social hierarchies in the countries where researchers lack familiarity. Therefore, the most valuable transnational comparisons will incorporate local knowledge and historical context because modern social hierarchies have their origins in historical policies (e.g., racial hierarchy in the U.S. in 2020 continues to reflect the "one drop rule" of the past).
Transnational comparison may be the most obvious way to study variation in systems of exposure because it is easy for us to grasp that there are differences is systems of social hierarchy between, say, Finland and the United States. But there are also differences in systems of exposure at smaller geographic scales or which leverage temporal variation. While confounding variables and autocorrelation pose threats to inference, researchers can minimize these concerns by using quasi-experimental designs (e.g., Difference-in-Differences) to study sharp shifts in systems of exposure (i.e., the consequences of a major immigration raid or the U.S. Supreme Court decision protecting the right to same-sex marriage).
Patterning
Our recognition of fundamental causes is possible precisely because of the existence of social gradients in health. The gradation or stratification in a social condition is what creates the possibility for detectable variation in health or mortality. To borrow a classic example of ubiquitous cause from Rose (1992): if everyone in a population smoked a pack of cigarettes a day from age 18 onward, we would likely assume that lung cancer was a genetic disease because the main source of variation would be biological. Under this ubiquitous and uniform exposure, it would be nearly impossible to detect the influence of smoking on lung cancer. Unless we compare temporally across birth cohorts or spatially across populations, or find experimental ways to vary the cause’s patterning, we will not detect a ubiquitous cause. It is easier to detect fundamental causes with a dichotomous or categorical patterning because this is more visible to us and fits the human proclivity toward categorization. Gradients (i.e., continuous distributions of resources) are much harder to see if we are not explicitly looking for them. Similarly, stratification systems that influence disease susceptibility dynamically or gradually over time, rather than in fixed ways or acutely during critical periods, are harder to study with current methods.
The reason socioeconomic status is detectable is because it exhibits a patterned variation at the population level. The same is true for the effects of racial hierarchy or residential segregation. Those of us interested in disrupting the social production of health inequalities can, therefore, use theory to hypothesize what the pattern of variation should look like, and then compare populations that should differ in the system of exposure to see if the pattern changes.
System enforcement
Another important way conceptualizing systems of exposure counters the tendency to naturalize stratification is by emphasizing how stratification systems are produced and maintained through laws, culture, institutions, and social interaction. We can use the legal terminology of “de facto” and “de jure” to specify whether a system of exposure is enforced formally through laws and policy (de jure enforcement), or informally through norms and culture (de facto enforcement). It is helpful to specify system enforcement to our best ability because, as we see in studies of school desegregation (Liu, Linkletter, Loucks, Glymour, & Buka, 2012) and anti-immigrant laws (Torche & Sirois, 2019), changes in system enforcement, from de facto to de jure or the reverse, can alter fundamental cause associations with health outcomes.
In summary, stratification systems are dynamic. By ignoring their dynamism we miss an opportunity to learn about the influence of fundamental causes on health. Studying dynamics in social structures, such as stratification systems, can reveal the contingent nature of fundamental cause associations. It can uncover how these seemingly intractable health disparities are created and maintained through social policy, institutions, and culture.
Examples: articulating systems of exposure in existing research
Next I highlight four studies that succeed in making comparison across temporal or spatial populations. These studies leverage a sharp shift in social meaning of relative locations with a stratification system to show that social stratification has consequences for health. Though they are not framed by the authors in these terms, I hope that by reframing the investigations as studies of systems of exposure, I can both demonstrate the ease of applicability of the approach and hold up these studies as models for future work (See Table 1).
Lauderdale, D. S. (2006). Birth outcomes for Arabic-named women in California before and after September 11. Demography, 43(1), 185–201.
Table 1.
Articulating Systems of Exposure with four examples from the health inequalities literature.
| System of Exposure | Scale | System Patterning | Patterning Over the Life-Course | System Enforce-ment | Comparison of Place–Time Population Coordinates | Outcome(s) | Found Variation in System of Exposure? | |
|---|---|---|---|---|---|---|---|---|
| Beltrán-Sánchez, Alberto and Riosmena, Wong, (2016) | SES gradient X Ethnic hierarchy | Nation | Intersectional: Continuous SES gradient X Ordinal ethnic hierarchy | Cumulative, with discontinuity in exposure upon immigration | De facto | Spatial: (Mexico, Mexican-born 2006); (U.S., Mexican-born 1999–2010); (U.S., U.S.-born Mexican American 1999–2010); (U.S., U.S.-born Non-Hispanic White 1999–2010) | Prevalence of metabolic syndrome | Yes |
| Lauderdale (2006) | Ethnic hierarchy | Nation | Ordinal ethnic hierarchy | Critical period | De facto | Temporal: (California 2000-2001) (California 2001-2002) | Incidence of low birth weight and pre-term birth | Yes |
| Krieger, Chen, Coull, Waterman, and Beckfield (2013) | Racial hierarchy | Region | Gradient | Critical period | De jure and de facto | Temporal: (Jim Crow polity 1940-1964); (Jim Crow polity 1965–2006) vs. (Non-Jim Crow polity 1940-1964); (Non-Jim Crow polity 1965–2006) | Incidence of infant death | Yes |
| Novak, Geronimus, & Martinez-Cardoso (2017) | Immigration status X Ethnic hierarchy | State | Intersectional: Dichotomous immigration status X Ordinal ethnic hierarchy | Critical period | De jure and de facto | Temporal: (Iowa 2007-2008); (Iowa 2008-2009) | Incidence of low birth weight | Yes |
Note: The “X” indicates an interaction between two systems of exposure.
In this study, Lauderdale used a temporal comparison to demonstrate the effects of 9/11 on adverse birth outcomes among babies born to mothers with Arab-sounding last names in California. Lauderdale found that the surge in anti-Arab sentiment that followed 9/11 was associated with increased risk of preterm birth and low birth weight among babies born to Arab-American mothers. Lauderdale acknowledged a key strength of her study: “By focusing on a period effect at the population level, this study circumvents the complexities and ambiguities of subjective reports of discrimination experiences” (Lauderdale, 2006:198).
Lauderdale hypothesized the biological mechanism for the health effects of 9/11 was exposure to acute stress during fetal development. Applying system-of-exposure thinking, 9/11 can be conceptualized as a mass disruption of the existing system of ethnic stratification in the U.S. such that Arab-Americans became excluded from social resources in a new way. Arab-Americans went from being “White, but not quite White” prior to 9/11, to being distinctly-racialized “others” after 9/11 (Jamal & Naber, 2008). Thus, the system of exposure under study was ethnic stratification in California 2000-2001, contrasted with California 2001-2002. Prior to 9/11, Arab-Americans were positioned along the periphery of the White majority. After 9/11, Arab-Americans dropped to a lower status in the ethnic hierarchy, making them targets of ethnic discrimination. Lauderdale defined the system of exposure at the national scale and studied it at the state scale. The system’s enforcement is de facto and Lauderdale detailed how increased violence and workplace discrimination against Arab-Americans as an ethnic group influenced Arab-American pregnant women across California. Integrating a life course perspective, Lauderdale tested for effects during a critical period (sensitive period) of exposure: fetal development. Birth outcomes are like the canary in the coal mine for population health research because of their sensitivity to even subtle shifts in systems of exposure. With its population-level comparative design and careful attention to dynamics in racial/ethnic discrimination, this study avoided the two pitfalls I discussed previously and made a major advance in research on how racism/ethnic discrimination impacts health.
Novak, N. L., Geronimus, A. T., & Martinez-Cardoso, A. M. (2017). Change in birth outcomes among infants born to Latina mothers after a major immigration raid. International Journal of Epidemiology, 46(3), 839–849.
Novak and colleagues use a temporal comparison of birth outcomes at the scale of state population to test the effects of a major immigration raid. Applying the system of exposure concept, we can reframe their exposure of interest as the intersecting stratification systems of immigration status and ethnic hierarchy. A major immigration raid in 2008 plausibly altered the social meaning of immigration status and Latinx ethnicity in the state of Iowa. While the immigration raid was a sharp change in de jure stratification system enforcement, the larger system of ethnic hierarchy persists with de facto enforcement. Novak and colleagues compared the incidence of low birth rate from Iowa 2007-2008 to Iowa 2008-2009 across Latinx ethnicity-by-immigration status subgroups. Like Lauderdale, the authors leveraged the critical period of fetal development to detect the system change.
Krieger, N., Chen, J. T., Coull, B., Waterman, P. D., & Beckfield, J. (2013). The unique impact of abolition of Jim Crow laws on reducing inequities in infant death rates and implications for choice of comparison groups in analyzing societal determinants of health. American Journal of Public Health, 103(12), 2234–2244.
Krieger’s work exemplifies the spirit of my call to study systems of exposure. In this 2013 study, Krieger and colleagues intentionally studied dynamics in race relations, stating that “conceptualizing Jim Crow legislation as a political determinant of health shifts the focus from 'race/ethnicity' to race relations as a causal exposure” (Krieger et al., 2013:2234). The end of de jure racial stratification through Jim Crow legislation marked a dramatic transformation of the system of racial stratification in Jim Crow polities and in the U.S. as whole. While Lauderdale and Novak and colleagues focused on a sharp disruption in a system of exposure and looked at the immediate consequences, Krieger and colleagues took a longer view. But they still leveraged the sensitivity of the critical period in early life in their choice of infant death as the health outcome. By comparing populations distinguished by region (i.e., states with Jim Crow legislation vs. states with no Jim Crow legislation) and time scales (i.e., years pre- and years post-1964 U.S. Civil Rights Act), Krieger and colleagues found a convergence in infant death rates between Blacks in the Jim Crow states and Blacks in non-Jim Crow states in the period immediately after the 1964 Civil Rights Act which ended de jure racial segregation through Jim Crow laws. A major strength of this study is that it moves beyond the default of Black-White subgroup comparison to compare Blacks across population moments. Krieger and colleague’s careful attention to racial stratification as a dynamic system helped them design a study that revealed how the influence of race on infant mortality is changed by our laws.
Beltrán-Sánchez, H., Palloni, A., Riosmena, F., & Wong, R. (2016). SES Gradients Among Mexicans in the United States and in Mexico: A New Twist to the Hispanic Paradox? Demography, 53(5), 1555–1581.
The study by Beltran Sanchez and colleagues ((Beltrán-Sánchez et al., 2016)) on the Hispanic paradox is an example of the kind of theory-informed population-level comparison approach that systems-of-exposure thinking can prompt. Beltran Sanchez and colleagues compared educational gradients in metabolic syndrome between four populations: Mexicans in Mexico, Mexican immigrants to the U.S., U.S.-born Mexican Americans, and U.S.-born Non-Hispanic Whites. They explicitly theorized schooling levels as a proxy for SES and as “markers of the opportunity structure available to people and their actual social position” (Beltrán-Sánchez et al., 2016:18). With this comprehensive population-level comparison they were able to test multiple hypotheses related to the influence of SES gradients and ethnic stratification on health. They dismissed the possibility that weaker SES gradients in health among Mexican immigrants are due to low SES gradients in Mexico ((Beltrán-Sánchez et al., 2016). In addition, they found that Mexican immigrants in the U.S. experience significantly weaker SES gradients than the Non-Hispanic White population ((Beltrán-Sánchez et al., 2016)).
The four studies I highlighted found variation in fundamental cause associations by looking at the effects of system perturbations on a specific health outcome. But fundamental causes, by definition, influence multiple disease outcomes through multiple risk factors so it makes sense to look for the effects of systems of exposure in various health outcomes. In this sense, each of these studies can be viewed as a springboard for further work to document influence of these same systems of exposure on additional health outcomes.
Where to look for the health effects of variation in a system of exposure depends on how the system is enforced, whether through policy or through culture. Systems enforced by policy are often easier to study for two reasons. First, they have the potential to change more abruptly than systems enforced only through culture. Second, the scale at which the system is defined and varies is explicit. Birth outcomes are useful for studying changes in systems of exposure that happen through policy because they are highly sensitive in the short term. But shifts in systems of exposure are often gradual so we are unlikely to detect them in the short term. All-cause mortality may be one of the easier outcomes for detecting the effects of systems change in the long term. This is because it is a catch-all variable whereby the effects of relative social disadvantage can happen via various biological mechanisms, yet they will eventually funnel to death. More challenging is identifying chronic disease outcomes that are likely to show effects of a shift in social hierarchy. Still, any health outcome in which scholars have documented racial disparities or an SES gradient is appropriate for applying the system of exposure framework.
These four studies show the value of turning our search for fundamental causes of health inequality to the study of differences between contexts, and specifically, to the study of dynamics in systems of exposure. There are three key benefits to reframing the fundamental causes of health inequality as systems of exposure. First is flexiblility of social scale. Second is an intersectional perspective. Third is a relational perspective. I discuss these benefits to future research briefly in the section that follows.
Benefit 1: flexibility of social scale
Although health researchers tend to study “populations” at the national scale, stratification systems also exist at smaller scales of aggregation. An approach that reframes fundamental causes as systems of exposure urges us to think flexibly about the social scale at which the system will be defined. To illustrate this, consider racism. Racism has been theorized as a fundamental cause (Phelan & Link, 2015). Racism or racial hierarchy tends to be thought of as a national stratification system, which it is. But racism as a system of exposure also varies greatly by region within the U.S., by state within the U.S., and even by city. Once we reframe fundamental causes as systems of exposure to the determinants of health, we see that the system is actually context-specific. Its patterning varies depending on the social scale at which it is defined and maintained. For example, racial segregation in the American South in 1950 was a distinct system of exposure from racial segregation in Louisiana in 1950, and distinct still from racial segregation in New Orleans in 1950. As I argued previously, systems of exposure should be studied across population moments – a glimpse of a population in a particular spatiotemporal context. But we need not look for systems of exposure only in national population moments. Rather, with systems of social stratification, the meaningful scale can be a much smaller area such as a city or even a neighborhood. The scale need only be a social context with an intact system of social stratification that distributes access to the determinants of health. This flexibility is important because we can and should be studying the ways that social stratification varies at subnational levels.
The system-of-exposure concept is also flexible beyond geography. We can apply it to social conditions that are not formal stratification systems, but which can differentiate stigma and power, nonetheless. Whether a specific variable works as a system of exposure depends on how we theorize it. The key is to articulate the social condition as a system that differentiates social resources and power. For example, to the extent that body size (i.e., fatness) carries varying degrees of stigma in different time periods, it could be studied as a system of exposure. Obesity had a different social meaning in the U.S. in the early 1900’s than it did in the early 2000’s; a major shift followed the transition to industrialism with additional shifts in the 1980’s (Stearns, 1997). It was not until the 1920’s that attendance at Fat Men’s Clubs dwindled and physicians began advocating dieting and being underweight instead of overweight (Stearns, 1997). Here is an instance where system-of-exposure framing could be used as an insight-generating practice. For example, as a way of studying how long it takes for norms around health behavior to change, one could compare fat stigma at various population moments in the U.S. to observe how fat stigma emerged and spread across the U.S.
The practice of articulating systems of exposure makes it possible to consider various axes of social dis/advantage such as sexual orientation, gender identity, disability status, and rurality. It matters less if a social condition truly warrants being classified as a system of exposure. More important is using the concept to locate, imagine, and articulate to the fullest extent possible the systems of exposure that shape access to the determinants of health. Doing this helps clarify how far we need to broaden the scope of our research and what an effect might look like. In this sense, reframing fundamental causes as systems of exposure helps guide our research so that we can identify social processes that modify health inequalities.
One challenge to systems-of-exposure analysis is autocorrelation - both spatial and temporal. This is why some of the most promising research designs employ econometric methods and leverage a quasi-experimental shock to the system. There is also promise in using Bayesian hierarchical models to combine individual and aggregate data and reduce bias due to the modifiable area unit problem. Ultimately, while thinking about the scale of fundamental causes introduces potential pitfalls, this approach is truer to the dynamic nature of social reality.
Benefit 2: intersectional perspective
This essay is written for researchers interested in reducing health disparities, particularly racial health disparities. I advocate moving away from studying race as a fixed exposure. The health consequences of race are determined by a larger system of exposure which we can call racial hierarchy, and which intersects with other systems of exposure. Rather than designing a study that compares two racial subgroups, we should design studies that leverage variation over time or place to compare, for example, “System A of racialization” to “System B of racialization.” System change can happen through people being racialized differently over time and place, as well as through the relative position of certain groups of racialized peoples in a racial hierarchy shifting. We simply cannot understand racial health disparities by theorizing race as an individual trait, rather than a position in a dynamic system of exposure.
So far, I have only discussed systems of exposure that involve a single system of stratification, a single fundamental cause association (e.g., racism). However, intersectionality theory reminds us that people’s lives are shaped by intersecting axes of oppression (Crenshaw, 1989). One advantage of reframing fundamental causes as systems of exposure is that it makes it easier to consider the influence of multiple, intersecting fundamental causes at once. Instead of thinking of a fundamental cause as present or absent, we can think of positions within an intersectional system of exposure that incorporates multiple axes of social hierarchy, such as patriarchy plus racism. Intersectional systems of exposure are shaped by a multitude of intervening factors: demographics, culture, history, policy, and geography. Distinct combinations of these factors create variation in social hierarchies and in the extent to which overlapping social hierarchies determine health. Attention to this variation can reveal how social policies change that distribution of power and resources and how, in turn, they change health inequalities.
As mentioned previously, contextual variation in health inequalities is due in part to differences in social hierarchies themselves, and in part to differences in the extent to which health can be “bought” with social resources. In places where policy, culture, and even geography make it harder to buy one’s way into good health, we might expect to see a flatter social gradient in health than in places where social position is rewarded by way of health. Likewise, in spatiotemporal contexts averse to government regulation and which lack initiatives to ensure access to the determinants of health, stratification by SES and race will be more deterministic in its influence on health trajectories and mortality. The result is that in some places poverty is more likely to condemn someone to a shorter, sicker life because of the ways it is further stigmatized by an intersecting social hierarchy. States in the U.S. are a good example of intersectional systems of exposure. They encompass multiple intersecting stratification systems, such as socioeconomic stratification, racial hierarchy, and residential segregation. Further, with the rise of state’s rights in recent decades, states are increasingly able to shape the distribution of social resources and control access to the social determinants of health (Montez et al., 2017; Nathan, 2005). Thus, research that compares systems of exposure between states or over time is a promising direction for future research (See Corrigan et al., 2005 for a nice example of this approach).
Benefit 3: relational perspective
Fundamental Cause Theory tells us that social inequality is linked to health inequality, not just because of the constraints placed on people with low status but also because of the health advantages enjoyed by those with high status (Clouston et al., 2016; Link and Phelan 1995). So a focus on resource distribution is productive because it moves us away from, “theorizing health deficits,” a common pitfall of health disparities research, and instead gives us traction to think relationally about how health inequalities are socially produced. This is one of the major contributions of FCT. We come to see fundamental causes not merely as risk factors that are present or absent, but as positions within a system of resource distribution – a stratification system. Every position is relational.
However, in the application of FCT, there is a strong tendency to lose the relational perspective and to think of fundamental causes as just other individual risk factors. Reframing fundamental causes as systems of exposure emphasizes the relational nature of health inequality. For example, racism is a system of exposure to the determinants of health. Everyone holds a position in the system of racial hierarchy. Although the health effects of racism on White people are rarely studied explicitly or conceptualized as dynamic, they should be. White people are not just the reference category; they are the beneficiaries of racism as a dynamic system of exposure. Studying racism and other forms of stratification as systems of exposure helps bring out the way that “unmarked” privileged categories may convert their power and privilege into health through the exploitation of others.
In studies of health inequality, the dominant group is often assumed to be unmarked by health disadvantage. For example, in studies of the negative health effects of irregular work schedules among low-wage workers, the beneficiaries of their labor are ignored. Studies demonstrate that graveyard shifts and highly variable shift work are disruptive for sleep and worsen physical and mental health among the workers (Drake, Roehrs, Richardson, Walsh, & Roth, 2004). But what about the people who benefit from this labor? What about the health benefits that come from the convenience of being able to buy anything at any hour of the night? To what extent does the adage “my loss is your gain,” apply to health? Of course, health disadvantages may not be linked to health advantages in a way that is outcome-specific. It is possible that a disadvantage in one health outcome is connected to an advantage in another health outcome through a relationship of exploitation. But these are the kinds of questions we can explore with a relational perspective. A relational perspective guides us to focus on points of contact or conflict between subgroups that occupy different locations within a system of exposure (Desmond, 2014). Rather than simply comparing the subgroups categorized by a fundamental cause (e.g., working class vs. middle class vs. upper class), we can study variation in the categorization process itself. We know that health behaviors are constrained by being working class, but how is the social reality of being working class boundaried? How do those boundaries vary with economics or culture? A focus on the relationships between locations within a system of exposure guides us to consider the health effects of domination and exploitation.
Conclusion
In this article, I have highlighted an opportunity to advance how we study the association between systems of social stratification and health inequalities. The goal in reframing fundamental causes as systems of exposure is to produce research that illuminates dynamics in the influence of social stratification on health and also to reveal the potential for context to modify social gradients in health. The systems of exposure framing also lends itself to research evaluating the health consequences of broad-based social interventions that disrupt fundamental cause associations, such as school desegregation, reparations, or free college. Ultimately, the two questions health equity scholars must begin to answer are: When do systems of exposure change? And why? For the special case of fundamental causes that are stratification systems (e.g., SES gradient, racism), we may not be able to estimate the Average Treatment Effect of a change in the system of exposure. But we may not need to. Rather, we just need to demonstrate some change in health inequality at a population level as a result of variation in a system of exposure. Articulating systems of exposure and documenting the health consequences of their variation across contexts can make visible the connections between the policies and institutions we support or oppose and the health disparities we tolerate. We need to grow the evidence base that links policy change or cultural change to shifts in systems of exposure and, in turn, to successful reductions in health inequity. Although formidable institutions maintain the systems of oppression that differentiate exposure to the social determinants of health, studies that document the potential for change are valuable in that they can be used by community organizers and activists in their work to challenge existing power structures.
Ethics approval
No Ethics Approval Required. This article is theoretical/conceptual and did not require the collection or analysis of data from human subjects
CRediT authorship contribution statement
Alicia R. Riley: Conceptualization, Writing - original draft, Writing - review & editing.
Acknowledgements:
Many thanks to Diane Lauderdale, John Levi Martin, Maria Glymour, Linda Waite, and anonymous reviewers for their helpful feedback. The author received grant support for this research through the National Institute on Aging: T32 AG049663/AG/NIA NIH HHS/United States.
References
- Beltrán-Sánchez H., Alberto P., Riosmena F., Wong R. SES gradients among Mexicans in the United States and in Mexico: A new twist to the hispanic paradox? Demography. September 21, 2016;53(5):1555–1581. doi: 10.1007/s13524-016-0508-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beltrán-Sánchez H., Andrade F.C.D. Time trends in adult chronic disease inequalities by education in Brazil: 1998–2013. International Journal for Equity in Health. 2016;15(1):139. doi: 10.1186/s12939-016-0426-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M.S., Hawks B.L. A debunking of the myth of healthy Asian Americans and Pacific Islanders. American Journal of Health Promotion: AJHP. 1995;9(4) doi: 10.4278/0890-1171-9.4.261. 261–68. [DOI] [PubMed] [Google Scholar]
- Clouston S.A.P., Rubin M.S., Phelan J.C., Link B.G. A social history of disease: Contextualizing the rise and fall of social inequalities in cause-specific mortality. Demography. August 16, 2016;53(5):1631–1656. doi: 10.1007/s13524-016-0495-5. [DOI] [PubMed] [Google Scholar]
- Corrigan P.W., Watson A.C., Heyrman M.L., Warpinski A., Gracia G., Slopen N., Hall L.L. Structural stigma in state legislation. Psychiatric Services. 2005;56(5):557–563. doi: 10.1176/appi.ps.56.5.557. [DOI] [PubMed] [Google Scholar]
- Crenshaw K. University of Chicago Legal Forum; 1989. Demarginalizing the intersection of race and sex: A Black feminist critique of antidiscrimination doctrine; pp. 139–168. [Google Scholar]
- Cylus J., Glymour M.M., Avendano M. Health effects of unemployment benefit program generosity. American Journal of Public Health. December 18, 2014;105(2):317–323. doi: 10.2105/AJPH.2014.302253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desmond M. Relational ethnography. Theory and Society. August 27, 2014;43:547–579. [Google Scholar]
- Diez Roux A.V. Invited Commentary: The Virtual Epidemiologist—Promise and Peril. American Journal of Epidemiology. 2015;181(2):100–102. doi: 10.1093/aje/kwu270. [DOI] [PubMed] [Google Scholar]
- Diez Roux A.V. The study of group-level factors in epidemiology: Rethinking variables, study designs, and analytical approaches. Epidemiologic Reviews. July 1, 2004;26(1) doi: 10.1093/epirev/mxh006. 104–11. [DOI] [PubMed] [Google Scholar]
- Diez Roux A.V. Integrating social and biologic factors in health research: A systems view. Annals of Epidemiology. July 1, 2007;17(7) doi: 10.1016/j.annepidem.2007.03.001. 569–74. [DOI] [PubMed] [Google Scholar]
- Diez Roux A.V. Next steps in understanding the multilevel determinants of health. Journal of Epidemiology & Community Health. November 1, 2008;62(11) doi: 10.1136/jech.2007.064311. 957–59. [DOI] [PubMed] [Google Scholar]
- Diez Roux A.V. Health in cities: Is a systems approach needed? Cadernos de Saúde Pública. November 2015;31:9–13. doi: 10.1590/0102-311XDE01S115. [DOI] [PubMed] [Google Scholar]
- Drake C.L., Roehrs T., Richardson G., Walsh J.K., Roth T. Shift Work Sleep Disorder: Prevalence and Consequences Beyond that of Symptomatic Day Workers. Sleep. 2004;27(8):1453–1462. doi: 10.1093/sleep/27.8.1453. [DOI] [PubMed] [Google Scholar]
- Ford C.L., Airhihenbuwa C.O. The public health critical race methodology: Praxis for antiracism research. Social Science & Medicine. 2010;71:1390–1398. doi: 10.1016/j.socscimed.2010.07.030. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler M.L. Structural stigma: Research evidence and implications for psychological science. American Psychologist. 2016;71(8):742–751. doi: 10.1037/amp0000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House J.S., Lepkowski J.M., Kinney A.M., Mero R.P., Kessler R.C., Herzog A.R. The social stratification of aging and health. Journal of Health and Social Behavior. 1994;35(3):213–234. [PubMed] [Google Scholar]
- Jamal A.A., Naber N. Syracuse University Press; 2008. Race and Arab Americans before and after 9/11: From invisible citizens to visible subjects. [Google Scholar]
- Krieger N., Chen J.T., Coull B., Waterman P.D., Beckfield J. The unique impact of abolition of Jim Crow laws on reducing inequities in infant death rates and implications for choice of comparison groups in analyzing societal determinants of health. American Journal of Public Health. December 2013;103(12):2234–2244. doi: 10.2105/AJPH.2013.301350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale D.S. Birth outcomes for Arabic-named women in California before and after september 11. Demography. February 2006;43(1):185–201. doi: 10.1353/dem.2006.0008. [DOI] [PubMed] [Google Scholar]
- Lieberson S. University of California Press; 1985. Making it count: The improvement of social research and theory. [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995:80–94. [PubMed] [Google Scholar]
- Liu S.Y., Linkletter C.D., Loucks E.B., Glymour M.M., Buka S.L. Decreased births among Black female adolescents following school desegregation. Social Science & Medicine. 2012;74(7) doi: 10.1016/j.socscimed.2011.12.029. 982–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey D.S. Russell Sage Foundation; 2007. Categorically unequal: The American stratification system. [Google Scholar]
- Matthews S.A. Spatial polygamy and the heterogeneity of place: Studying people and place via egocentric methods. In: Burton L.M., Matthews S.A., Leung M.C., Kemp S.P., Takeuchi D.T., editors. Communities, neighborhoods, and health: Expanding the boundaries of place. Springer New York; New York, NY: 2011. pp. 35–55. Social Disparities in Health and Health Care. [Google Scholar]
- Montez J.K., Zajacova A., Hayward M.D., Woolf S.H., Chapman D., Beckfield J. Educational disparities in adult mortality across U.S. States: How do they differ, and have they changed since the mid-1980s? Demography. 2019;56(2):621–624. doi: 10.1007/s13524-018-0750-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez J.K., Hayward M.D., Wolf D.A. Do U.S. States' socioeconomic and policy contexts shape adult disability? Social Science & Medicine. April 2017;178:115–126. doi: 10.1016/j.socscimed.2017.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nathan R.P. Federalism and health policy. Health Affairs. November 1, 2005;24(6) doi: 10.1377/hlthaff.24.6.1458. 1458–66. [DOI] [PubMed] [Google Scholar]
- Navarro V. Why the white working-class mortality and morbidity is increasing in the United States: The importance of the political context. International Journal of Health Services. April 1, 2019;49(2):197–203. doi: 10.1177/0020731419832236. [DOI] [PubMed] [Google Scholar]
- Novak N.L., Geronimus A.T., Martinez-Cardoso A.M. Change in birth outcomes among infants born to Latina mothers after a major immigration raid. International Journal of Epidemiology. 2017;46(3):839–849. doi: 10.1093/ije/dyw346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omi M., Winant H. Routledge; 2014. Racial formation in the United States.https://www.taylorfrancis.com/books/9781135127510 [Google Scholar]
- Palloni A., Morenoff J.D. Interpreting the paradoxical in the hispanic paradox. Annals of the New York Academy of Sciences. 2001;954(1) doi: 10.1111/j.1749-6632.2001.tb02751.x. 140–74. [DOI] [PubMed] [Google Scholar]
- Pearson J.A. Can't buy me whiteness: New lessons from the Titanic on race, ethnicity, and health. Du Bois Review: Social Science Research on Race. 2008;5(1):27–47. [Google Scholar]
- Phelan J.C., Link B.C. Is racism a fundamental cause of inequalities in health? Annual Review of Sociology. 2015;41(1):311–330. [Google Scholar]
- Phelan J.C., Link B.G., Parisa T. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior. March 2010;51(1_suppl) doi: 10.1177/0022146510383498. S28–40. [DOI] [PubMed] [Google Scholar]
- Rose G. Oxford University Press; 1992. The strategy of preventive medicine. [Google Scholar]
- Rose Geoffrey. “Sick individuals and Sick populations. International Journal of Epidemiology. March 1, 1985;14(1):32–38. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- Stearns P.N. New York University Press; 1997. Fat history: Bodies and beauty in the modern west. [Google Scholar]
- Torche F., Sirois C. Restrictive immigration law and birth outcomes of immigrant women. American Journal of Epidemiology. January 1, 2019;188(1):24–33. doi: 10.1093/aje/kwy218. [DOI] [PubMed] [Google Scholar]