Abstract
Glenoid rim fractures are recognized as a risk factor for recurrent instability after anterior shoulder dislocation. In addition to traditional open treatments of bony Bankart lesions, several arthroscopic techniques of fixation and reconstruction recently have been described. We present a technique of arthroscopic nonrigid fixation for large glenoid rim fractures, as an alternative to existing procedures.
Introduction (With Video Illustration)
Glenoid rim fractures can occur with anterior shoulder dislocations, contributing to recurrent instability.1 In the setting of significant anteroinferior glenoid bone loss from bony Bankart lesions or impression defects, arthroscopic soft-tissue Bankart repairs are predisposed to failure.2 As such, there recently has been considerable interest in developing new surgical procedures to specifically account for this bone loss. With a trend toward minimally invasive approaches, proposed arthroscopic techniques have included the Bristow–Laterjet procedure, as well as several more anatomic reconstructions using materials such as glenoid allograft, distal tibial allograft, or iliac crest autograft.3 In cases in which a large, displaced bony Bankart fracture is identified, fragment fixation also can be performed with screws or suture anchors, avoiding the need for graft material.4
Recently, anatomic glenoid reconstruction with distal tibial allograft has been described using arthroscopic transglenoid suture fixation.5 Taverna et al.6 have reported one case employing a similar strategy for fixation of an acute glenoid rim fracture. A modification of this technique was recently described by Avramidis et al.7 Here, we provide a detailed account of our preferred technique for arthroscopic transglenoid suture fixation of a displaced bony Bankart fracture in the lateral decubitus position (Tables 1 and 2, Video 1).
Table 1.
Advantages and Disadvantages of Arthroscopic Nonrigid Fixation of a Glenoid Rim Fracture
| Advantages | Disadvantages |
|---|---|
| All-arthroscopic technique | Technically challenging |
| No graft material needed | Reduction easiest in acute phase |
| Truly anatomic | Most suitable for large fragments |
Table 2.
Pearls and Pitfalls of the Technique
| Pearls | Pitfalls |
|---|---|
|
|
|
|
|
|
Technique
Preoperative Assessment
The preoperative clinical assessment begins with a standard history surrounding the mechanism of injury, previous episodes of instability, and documentation of any previous surgical interventions. This is followed by a physical examination, including tests of instability (e.g. apprehension, relocation, load-and-shift, and sulcus tests). Rotator cuff integrity is examined, and the Beighton score is assessed. Routine imaging includes anteroposterior, axillary, and scapular Y-views of the affected shoulder, in addition to a computed tomography scan with 3-dimensional reconstruction to optimally define the glenoid fracture, residual glenoid bone stock, and any Hill–Sachs lesion. A 3-dimensional printed model can assist with preoperative planning (Fig 1).
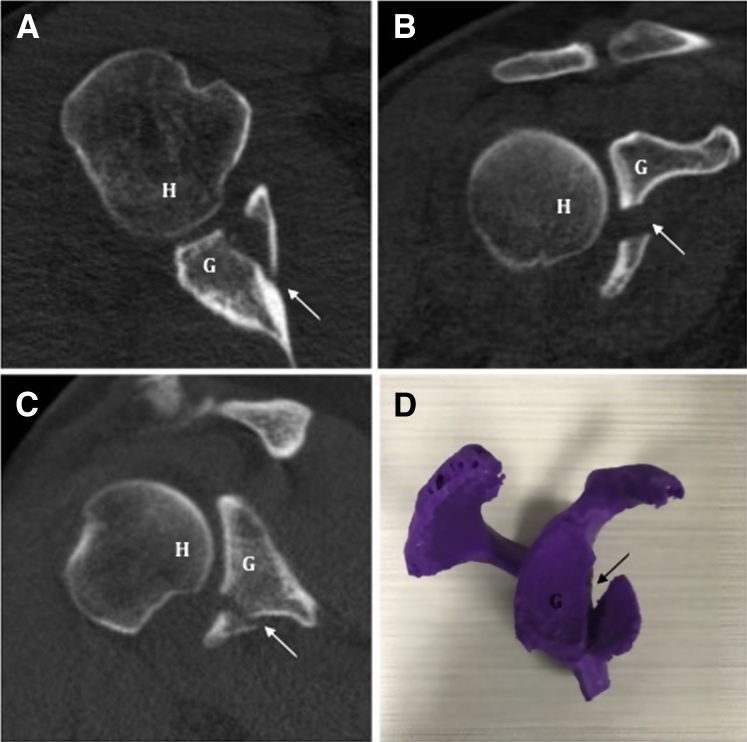
Fig 1.
(A-C) Axial, coronal, and sagittal computed tomography images of a right anteroinferior glenoid rim fracture are shown. This fragment represents 30% loss of glenoid width. (D) A 3-dimensional printed model assists with preoperative planning. Arrows demonstrate the glenoid rim fracture. (G, stable glenoid; H, humeral head.)
Positioning, Preparation, and Diagnostic Arthroscopy
The patient is positioned in the lateral decubitus position on a standard operating table using a beanbag positioner, allowing the torso to rotate 30° posteriorly so the glenoid is parallel to the floor. The skin is prepared with chlorhexidine solution. The affected arm is free draped and placed in a pneumatic limb positioner (Spider 2; Smith & Nephew, Memphis, TN). The arm is then abducted to 60° in balanced suspension.
Skin landmarks are drawn on the patient, including the clavicle, acromioclavicular joint, acromion, and scapular spine. A posterior portal is established through a standard technique, after which diagnostic arthroscopy is performed. Anteroinferior and anterosuperior portals are created under direct visualization using an outside-in technique and maintained with arthroscopic cannulas (Fig 2).
Fig 2.

Lateral decubitus positioning and skin markings for standard shoulder arthroscopy portals (right shoulder). (AI, anteroinferior portal; AS, anterosuperior portal; P, posterior portal.)
Preparation of Fracture Fragment
Viewing from the anterosuperior portal, the glenoid fracture fragment is identified, probed, and debrided. A liberator knife is used to mobilize the fracture fragment. Subsequently, the bony surfaces within the fracture are prepared using a rasp, to expose bleeding cancellous bone. The fragment is then provisionally reduced to the anteroinferior glenoid. If satisfied with the bone quality and provisional reduction, the surgeon prepares for fracture fixation.
Nonrigid Glenoid Fixation
A bullet drill guide (Glenoid Drill Guide; Smith & Nephew) is inserted through the posterior portal, and its main arm is used to hold the fragment anatomically reduced (Fig 3). A small incision is made posteriorly, and the bullet guide is ratcheted against the posterior glenoid to stabilize the fragment. The 2.8-mm drill and sleeve are then advanced posterior-to-anterior across the fracture, without penetrating the anterior cortex. With the fragment now stabilized by the 2.8-mm drill, we release capsulolabral tissue from its anterior aspect, then advance the drill and sleeve through its anterior cortex. After removing the drill, a 2-mm monofilament is passed posterior-to-anterior through the drill sleeve and grasped through the anteroinferior portal.
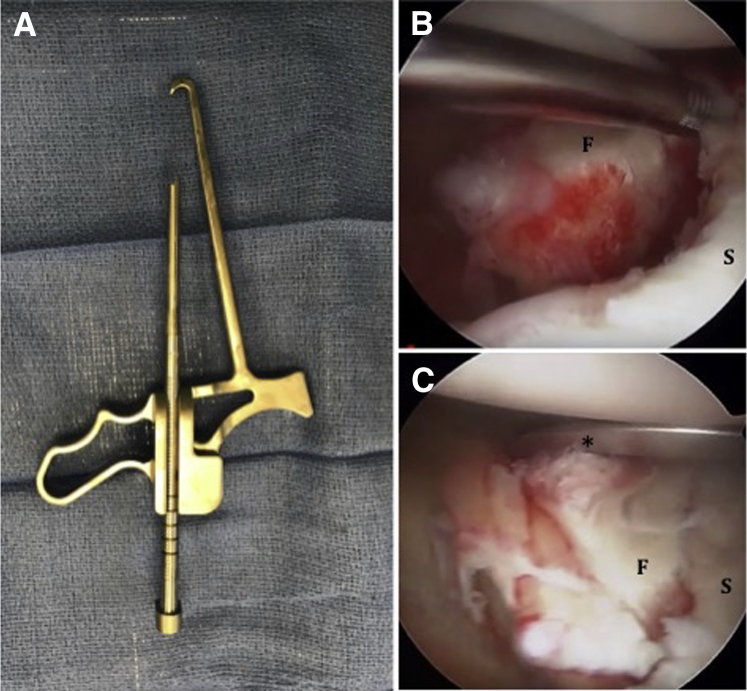
Fig 3.
(A) Viewing the right shoulder through an anterosuperior portal, the bullet drill guide is used to manipulate (B) the glenoid fracture fragment into (C) its reduced position. *The bullet drill guide. (F, glenoid fracture fragment; S, stable glenoid.)
At this point, suture tails from a round ENDOBUTTON (Smith & Nephew) are placed through the monofilament and shuttled anterior-to-posterior through the transglenoid tunnel, exiting through the posterior portal (Fig 4). Manually tensioning these sutures reduces the fracture, which can be further compressed using a rasp anteriorly. A second ENDOBUTTON is then applied posteriorly, and the construct is secured with a Nice knot.8 While maintaining direct visualization, a tensioning device is used to compress the fracture with a force of 100 N. We then add 3 half-hitch knots for further security. The fragment is now probed to assess stability.
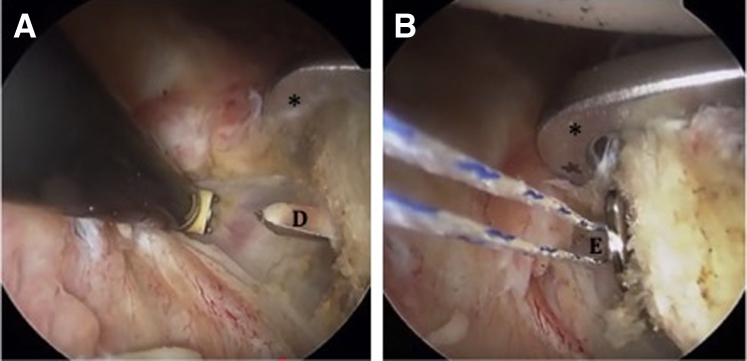
Fig 4.
(A) Viewing the right shoulder through an anterosuperior portal, a 2.8-mm drill is advanced through the anterior cortex under direct visualization, establishing a tunnel through which (B) the ENDOBUTTON is then passed. *The bullet drill guide. (D, 2.8-mm drill; E, ENDOBUTTON device.)
Bankart Repair
After appropriate release of the torn capsulolabral complex, a standard Bankart repair is performed using a 1.8-mm suture anchor positioned just superior to the fracture fragment (Q-Fix; Smith & Nephew). At the conclusion of our procedure, we visually confirm concentric reduction of the humeral head within the glenoid fossa (Fig 5).
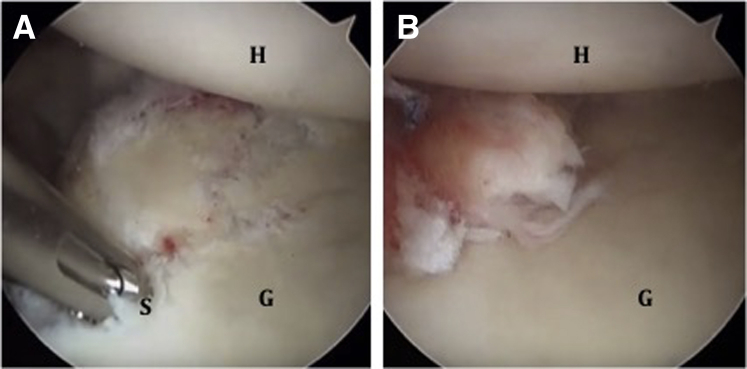
Fig 5.
(A) Viewing the right shoulder through an anterosuperior portal, a 1.8-mm suture anchor is positioned just superior to the reduced glenoid fragment. (B) This enables our final Bankart repair, which creates a concentrically reduced glenohumeral joint. (G, repaired glenoid; H, humeral head; S, placement of the suture anchor.)
Postoperative Management
The shoulder is immobilized in a sling, and the patient is given detailed postoperative rehabilitation instructions (Table 3).
Table 3.
Postoperative Rehabilitation Protocol after Arthroscopic Nonrigid Fixation of a Glenoid Rim Fracture
| 0-2 weeks: | Sling Immobilization; Passive ROM Exercises for the wrist, Elbow, and hand; Gentle Passive Shoulder ROM Starting Postoperative day 3 |
| 2-6 weeks: | Sling; passive ROM; consider active-assisted ROM at week 5 |
| 6-12 weeks: | Discontinue sling; active ROM |
| >12 weeks: | Continue ROM; progressive limb strengthening |
ROM, range of motion.
Discussion
This Technical Note adds to the existing literature through its detailed description of an arthroscopic transglenoid suture fixation technique for displaced glenoid rim fractures. Similar techniques have, to our knowledge, only been presented twice in the existing orthopaedic literature, and our report provides additional detail on preferred positioning, fragment preparation, maintenance of reduction, sequence of ENDOBUTTON fixation, and capsulolabral repair.6,7 Positive aspects of this technique include its all-arthroscopic nature, the potential cost savings of not requiring allograft, and the avoidance of donor-site morbidity from autograft harvest.
Risks, Complications, and Limitations
Although we have had no complications from this procedure to date, its overall risk profile remains unknown. In addition to the general risks of shoulder arthroscopy, theoretical risks include nonunion, reoperation for hardware removal, and recurrent instability.5 In addition, eccentric drilling of the transosseous tunnel (or errant placement of a suture anchor during Bankart repair) could potentially cause fracture comminution, compromising stability. Furthermore, it remains unknown during what postinjury time frame bony Bankart fragments can be successfully mobilized and reduced in this manner; in our experience, we have only performed this procedure within 1 month of a first-time dislocation. With smaller bony fragments, this technically challenging operation could become more difficult. For these reasons, it may be wise to consider having allograft available as a second option, should fragment reduction prove unsuccessful.
Overall, we acknowledge that further research is required to fully understand the learning curve, best applications, and long-term outcomes of this technique. However, we have been pleased with our early results. In the rapidly evolving field of shoulder instability, we believe this procedure offers several advantages through its arthroscopic approach and anatomic repair, meriting consideration when treating large glenoid rim fractures.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Viewing the right shoulder through posterior, anterosuperior, and anteroinferior portals to demonstrate the arthroscopic, nonrigid fixation of a displaced glenoid fracture after anterior shoulder dislocation in lateral decubitus position.
References
- 1.Griffith J.F., Antonio G.E., Yung P.S. Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patients. AJR Am J Roentgenol. 2008;190:1247–1254. doi: 10.2214/AJR.07.3009. [DOI] [PubMed] [Google Scholar]
- 2.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill–Sachs lesion. Arthroscopy. 2000;16:677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 3.Fortun C.M., Wong I., Burns J.P. Arthroscopic iliac crest bone grafting to the anterior glenoid. Arthrosc Tech. 2016;5:e907–e912. doi: 10.1016/j.eats.2016.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheibel M., Hug K., Gerhardt C., Kruger D. Arthroscopic reduction and fixation of large solitary and multifragmented anterior glenoid rim fractures. J Shoulder Elbow Surg. 2016;25:781–790. doi: 10.1016/j.jse.2015.09.012. [DOI] [PubMed] [Google Scholar]
- 5.McNeil D., Coady C., Wong I.H. Arthroscopic anatomic glenoid reconstruction in lateral decubitus position using allograft with nonrigid fixation. Arthrosc Tech. 2018;7:1115–1121. doi: 10.1016/j.eats.2018.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taverna E., Guarrella V., Freehill M.T., Garavaglia G. Arthroscopic reduction with Endobutton fixation for glenoid fracture. Joints. 2017;5:127–130. doi: 10.1055/s-0037-1603675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Avramidis G., Brilakis E., Deligeorgis A., Antonogiannakis E. All-arthroscopic treatment of glenoid rim fractures. Arthrosc Tech. 2019;8:e1121–e1124. doi: 10.1016/j.eats.2019.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boileau P., Alami G., Rumian A., Schwartz D.G., Trojani C., Seidl A. The double-suture Nice knot. Orthopedics. 2017;40:e382–e386. doi: 10.3928/01477447-20161202-05. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Viewing the right shoulder through posterior, anterosuperior, and anteroinferior portals to demonstrate the arthroscopic, nonrigid fixation of a displaced glenoid fracture after anterior shoulder dislocation in lateral decubitus position.