Abstract
There has been increased emphasis on medial meniscus repair in the anterior cruciate ligament–reconstructed knee, as this improves stability. We describe an arthroscopic sign of an unstable medial meniscal tear that is diagnostic. The “crevice sign” is a longitudinal fissure located on the distal medial femoral condyle. In the anterior cruciate ligament–deficient knee, there is increased strain on the medial meniscus. A posterior longitudinal medial meniscal tear can occur at the time of the index injury or with subsequent instability events. During this injury, the knee pivots and the anterior edge of the unstable medial meniscus digs into the articular cartilage of the medial femoral condyle, resulting in a longitudinal split of the distal femoral condyle articular cartilage. If this sign is observed during arthroscopy, it is recommended that surgeons thoroughly probe the medial meniscus to ensure no pathology is missed.
Combined injuries to the medial meniscus (MM) and anterior cruciate ligament (ACL) are frequently seen. These represent severe injuries, and the association of ACL injury and medial meniscus tear with early post-traumatic osteoarthritis in young patients has been well established.1 Consequently, there has been increased emphasis on meniscal repair over the past 3 decades, as this structure is essential in preventing osteoarthritis.2 However, meniscal lesions encountered at the time of anterior cruciate ligament reconstruction (ACLR) present surgeons with a treatment dilemma. They must decide, based on the location and extent of the lesion, to repair, remove, or leave the lesion in situ. One of the criterion to make this decision is meniscus stability at the time of surgery. Surgeons assess torn meniscus mobility using a probe. Commonly, a lesion is considered unstable if the meniscus can be displaced over the middle of the femoral condyle. Yet, this maneuver is subjective and might be, in some cases, falsely negative. In a tight knee, it also may be difficult to adequately probe the posterior horn of the medial meniscus. Based on our experience of ACLR and meniscal repair, we have noticed that a horizontal cartilage fissure of the medial femoral condyle is associated with unstable MM tears. Thus, this sign is pathognomonic for an unstable MM tear and has been named “the crevice sign.” This study aims to describe precisely this novel sign.
Description of the “Crevice Sign” (With Video Illustration)
During a standard ACL reconstruction procedure, both cartilage and the menisci are arthroscopically evaluated (Figs 1 and 2, Video 1). When the medial compartment is explored, the whole cartilage surface of the medial femoral condyle is inspected. The “crevice sign” appears to be 1 or 2 longitudinal cartilage fissures on the distal medial femoral condyle. The split can be palpated to ensure it is superficial and stable. The optimal position to visualize it is with the patient's knee flexed at 90°. In this case, the palpation of the medial meniscus is paramount. Moreover, the presence or absence of this sign does not prevent the surgeon from hooking the medial meniscus and determining its stability.
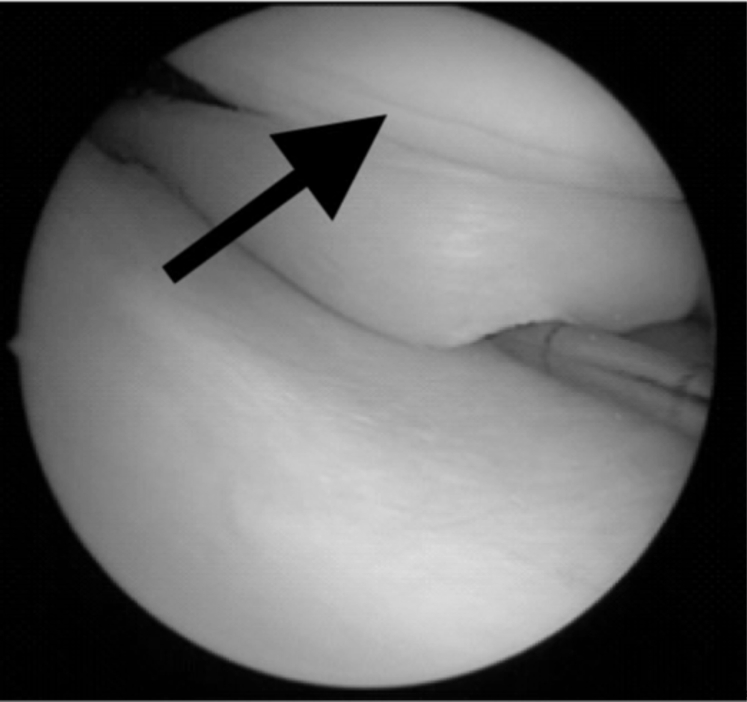
Fig 1.
Scope view right knee (medial compartment). Visualization of the “crevice sign” (arrow): 1 or 2 longitudinal fissures of the distal medial femoral condyle. The meniscal tear can be displaced to the crevice proving the meniscal involvement in the cartilage split.
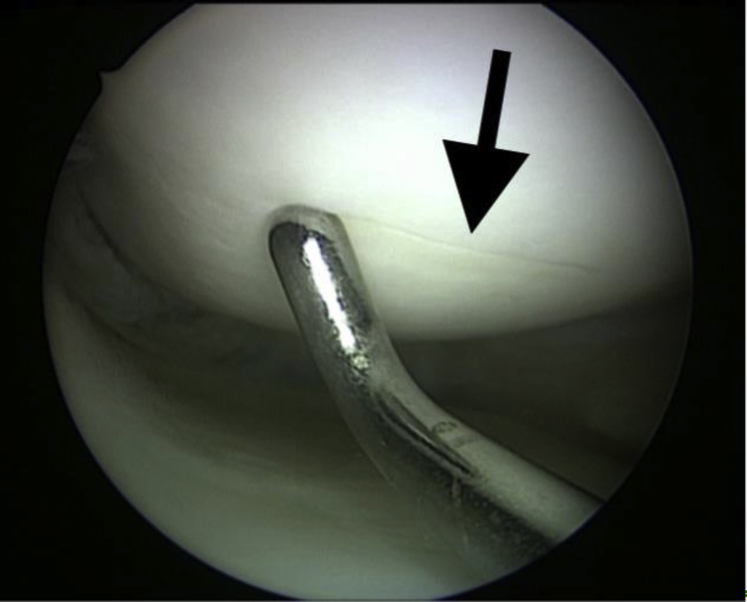
Fig 2.
Scope view right knee (medial compartment). The arrow shows the longitudinal cartilage split (“crevice sign”) on the medial femoral condyle.
In our experience, this sign has not been observed with an intact medial meniscus, which made us consider it to be pathognomonic for an unstable medial meniscal tear. It is noteworthy that on magnetic resonance imaging we can't identify a “crevice sign” or a medial subchondral bone edema related to this fissure.
Pathogenesis
Our hypothesis for this sign is explained by the pivoting maneuver that occurs with an ACL-deficient knee. The lateral femur subluxes posterolaterally and as it pivots around the medial axis of the knee. The medial femoral condyle pivots, tearing the posterior horn of the medial meniscus. Consequently, the anterior edge of the medial meniscus digs into the articular cartilage of the medial femoral condyle, resulting in a longitudinal split.
Discussion
This is the first time this sign has been described in the literature. On identification, it is our recommendation that the stability of the medial meniscus is explored and treated accordingly (Tables 1 and 2). In a tight knee, it may be difficult to adequately probe the posterior horn of the medial meniscus. If the crevice sign is observed and it is difficult to assess the posterior meniscus, we advocate pie-crusting the medial collateral ligament with an 18-gauge needle to improve visualization.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Patient positioning must allow for free mobilization of the limb | If there's no crevice sign, it doesn't mean that there's no meniscal tear. Surgeons should still assess meniscus status meticulously. |
| The crevice sign is generally seen at roughly 90° of knee flexion, so it's important to seek for it at this flexion. | This sign does not occur on the lateral compartment. |
| In case of a crevice sign, it is paramount to assess properly the stability of the medial meniscus with a probe. | Be careful when you palpate the crevice sign not to damage the cartilage. |
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| The presence of a crevice sign suggests that there is an unstable medial meniscal tear. | Surgeons should always assess meniscus stability; an unstable medial meniscus tear can occur without a crevice sign. |
| This is an easy and fast way to determine if we should repair a meniscal tear (because it means this is unstable). | The crevice sign is never seen on the lateral compartment. |
Recent articles support our pathogenesis hypothesis. Biomechanical studies have shown that the contact pressure between the meniscus and the femoral condyle is increased in the knee flexed position3 when compared with the extended position. At 90° of flexion, Inoue et al.4 reported that in ACL-deficient knees, the posterior portion of the MM is deformed due to compression against the medial femoral posterior condyle. The contact between the medial meniscus and the distal medial femoral condyle (where the “crevice sign” is detected) is clearly observed on magnetic resonance imaging.5
Meniscal repair is advocated in the ACL-reconstructed knee.2 Meniscal tears associated with ACL injuries are one of the main risk factors for progressive osteoarthritis.1 In vivo and in vitro studies have demonstrated the importance of the meniscus for knee stability, force distribution, proprioception, as well as joint lubrication and nutrition.2,6 In the ACL-deficient knee, the posterior segment of the medial meniscus acts as a secondary stabilizer of anterior tibial translation and plays a role in controlling knee instability.7 Okazaki et al.5 demonstrated that the torn medial meniscus moves posteriorly at 90° of knee flexion in ACL-deficient knees. In this study, concurrent medial meniscal repair and ACL reconstruction improved the deformed morphology and posterior extrusion, preventing excessive anterior knee laxity. Sarraj et al.6 showed that ACLR combined with meniscal repair results in decreased anterior knee joint laxity, as evidenced by improved patient-reported outcomes in the long term despite more reoperation rates. Finally, in a long-term perspective, there's evidence confirming that repairing MM dramatically decreases the risk of osteoarthritis in comparison with meniscal resection in ACL-deficient knees.8 Therefore, surgeons should consider meniscal repair as the first option when they encounter a meniscal tear. The “crevice sign” is useful sign to alert surgeons to the likelihood of an unstable medial meniscal tear that may need repair.
Conclusions
The “crevice sign” is pathognomonic for an unstable longitudinal medial meniscal tear in ACL-deficient knees. If this sign is observed during arthroscopic procedure, surgeons should ensure they probe the medial meniscus carefully and treat accordingly.
Footnotes
The authors report the following potential conflict of interest or source of funding: M.C. reports other from Arthrex and personal fees from Johnson & Johnson, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic view of the medial compartment (left knee). The “crevice sign” is visualized on the medial femoral condyle surface. Its relation to the stability of the meniscus is shown on the video.
References
- 1.Neuman P., Englund M., Kostogiannis I., Friden T., Roos H., Dahlberg L.E. Prevalence of tibiofemoral osteoarthritis 15 years after nonoperative treatment of anterior cruciate ligament injury: A prospective cohort study. Am J Sports Med. 2008;36:1717–1725. doi: 10.1177/0363546508316770. [DOI] [PubMed] [Google Scholar]
- 2.Pujol N., Beaufils P. Save the meniscus again! Knee Surg Sports Traumatol Arthrosc. 2019;27:341–342. doi: 10.1007/s00167-018-5325-4. [DOI] [PubMed] [Google Scholar]
- 3.Muriuki M.G., Tuason D.A., Tucker B.G., Harner C.D. Changes in tibiofemoral contact mechanics following radial split and vertical tears of the medial meniscus an in vitro investigation of the efficacy of arthroscopic repair. J Bone Joint Surg Am. 2011;93:1089–1095. doi: 10.2106/JBJS.I.01241. [DOI] [PubMed] [Google Scholar]
- 4.Inoue H., Furumatsu T., Miyazawa S., Fujii M., Kodama Y., Ozaki T. Improvement in the medial meniscus posterior shift following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:434–441. doi: 10.1007/s00167-017-4729-x. [DOI] [PubMed] [Google Scholar]
- 5.Okazaki Y., Furumatsu T., Miyazawa S. Meniscal repair concurrent with anterior cruciate ligament reconstruction restores posterior shift of the medial meniscus in the knee-flexed position. Knee Surg Sports Traumatol Arthrosc. 2019;27:361–368. doi: 10.1007/s00167-018-5157-2. [DOI] [PubMed] [Google Scholar]
- 6.Sarraj M., Coughlin R.P., Solow M. Anterior cruciate ligament reconstruction with concomitant meniscal surgery: A systematic review and meta-analysis of outcomes. Knee Surg Sports Traumatol Arthrosc. 2019;27:3441–3452. doi: 10.1007/s00167-019-05389-3. [DOI] [PubMed] [Google Scholar]
- 7.Seon J.K., Gadikota H.R., Kozanek M., Oh L.S., Gill T.J., Li G. The effect of anterior cruciate ligament reconstruction on kinematics of the knee with combined anterior cruciate ligament injury and subtotal medial meniscectomy: An in vitro robotic investigation. Arthroscopy. 2009;25:123–130. doi: 10.1016/j.arthro.2008.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Claes S., Hermie L., Verdonk R., Bellemans J., Verdonk P. Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1967–1976. doi: 10.1007/s00167-012-2251-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic view of the medial compartment (left knee). The “crevice sign” is visualized on the medial femoral condyle surface. Its relation to the stability of the meniscus is shown on the video.