Abstract
According to recent anatomic studies, the anterior cruciate ligament (ACL) appears to be a flat, “ribbon-like” structure, with a thin, oval-shaped insertion on the femur and a C-shaped tibial insertion. According to this anatomy, we describe an ACL-reconstruction technique that aims to approximate this natural anatomy. The basic principle of this technique is not to use conventional round tunnels but create tunnel shapes that resemble more closely the original ACL insertion sites. Using either a rectangular quadriceps tendon graft or a “flat” hamstring graft may not only provide a biomechanical advantage with increased rotational stability but also improve bone–tendon healing due to increased bone–tendon contact and decreased diffusion length. Creating a C-shaped tibial tunnel also avoids laceration of the anterior horn of the lateral meniscus, which is frequently harmed during conventional tibial tunnel drilling.
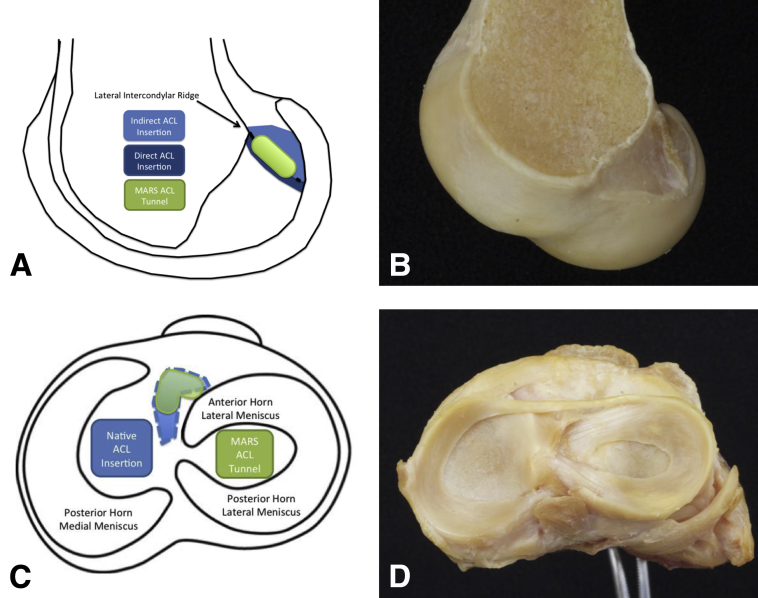
For more than 30 years, the anatomical features of the anterior cruciate ligament (ACL) and its bony attachments have been investigated, and the findings have resulted in modifications in the techniques of reconstruction following rupture.1 In particular, the double-bundle technique focused on an exact analysis of the insertional anatomy of the ACL.2 The anatomic description of Smigielski et al.3 finally formed the basis for our approach to anatomic ACL reconstruction. According to their findings3, 4, 5 and those of others,1,6,7 the ACL, including its femoral and tibial insertions, appears to be flat, “ribbon-like” after removing the synovial membrane (Fig 1). Smigielski et al.3 also rediscovered the “lost treasure” of the tibial relationship between ACL and the lateral meniscus described by Testut und Jacob in 1921, resulting in potential iatrogenic anterior root injury of the lateral meniscus in conventional single-bundle ACL reconstruction techniques.8, 9, 10
Fig 1.
Anatomy of the ACL insertion sites. Smigielski et al.3 describe the femoral insertion site as crescent-shaped, extending from the intercondylar ridge to the posterior articular margin of the lateral condyle, shown in schematic (A) and in a right cadaveric lateral femoral condyle viewed from medially, with the medial condyle removed (B). The native ACL insertion consists of 2 components: the direct type (dark blue), where fibers entered the bone almost at a right angle and the fanlike indirect fibers (light blue) extending to the articular margin. The location of a rectangular tunnel for reconstruction (green) is shown according to these landmarks. The tibial insertion is described as being C-shaped3,4 from along the lateral edge of the medial tibial spine to the anterior aspect of the anterior root of the lateral meniscus, accommodating within its concavity the insertion of the lateral meniscus. This relation is shown in a schematic drawing of a right tibial plateau viewed from above (C) with the native ACL insertion (light blue) and the C-shaped tunnel (green). (D) Illustration of the corresponding view of a right cadaveric tibial plateau with the native ACL resected 1 cm above its insertion site to demonstrate its relationship to the anterior root of the lateral meniscus. (ACL, anterior cruciate ligament.)
Therefore, the basic principle of this technique for ACL reconstruction is not to use round tunnels but create tunnel shapes that resemble more closely the original insertions. Commonly used ACL reconstruction techniques use drills to create bone tunnels, which naturally lead to circular insertion sites. The double-bundle techniques tried to better match the insertion sites and, more importantly, to improve graft biomechanics.
In vivo studies comparing ACL-reconstructed patients with matched controls in pivoting and cutting activities found that single-bundle ACL reconstruction surgery was not able to completely restore rotational kinematics and stability.11,12 Biomechanical data demonstrated 2 fiber bundles of the ACL with different patterns of length changes during knee motion and the resulting variations in tension.13 However, already at this time comparable kinematics could be shown in ACL reconstruction using rectangular bone tunnels.14, 15, 16
Apart from the biomechanical advantages, this technique could potentially provide interesting biological benefits. Because the graft is placed in bone tunnels in ACL reconstruction, the structure and composition of the direct insertion site is not reproduced. Instead, the graft heals with a fibrovascular scar at the graft–tunnel interface and forms perpendicular collagen bundles to counteract the shear stresses, attaching the tendon to the bone. These bundles resemble the Sharpey fibers of an indirect insertion site. Their size and number are positively correlated with the graft pull-out strength.17 Revascularization only starts after 4 weeks, progressing from the periphery of the graft to the entire diameter.18 As the contact area of a flat ACL graft is about 3 times greater in relation to its volume compared with a round one, the formation of Sharpey-like fibers as well as the vascularization can take place on an increased area and the distance to the central part of the graft is still limited. The idea is to prevent central necrosis as described in the early graft healing phase19 due to a reduced distance for diffusion. A recent animal study could show this positive biological effect on tendon to bone healing using a flattened bone tunnel. The flattened bone tunnel resulted in accelerated tendon to bone healing with a stronger regenerated tendon–bone interface.19 Furthermore, graft fixation is changed to cortical button fixation to reduce tunnel enlargement, which could be shown by Chiang et al.20 in the setting of double-bundle reconstruction. Hence, there were multiple aims for developing an ACL reconstruction technique with special features, as outlined in the 2 sections to follow.
Biomechanics
-
1.
Reconstruction of the rectangular anatomical femoral insertion.
-
2.
Reconstruction of the C-shaped tibial insertion with preservation of the anterior horn of the lateral meniscus and the possibility of a more anterior (anatomical) position of the tibial tunnel without notch impingement and extension deficit.
-
3.
Reconstruction with a flat tendon graft better fitting in the notch without reducing total graft volume and resembling the original ACL with different parts under tension throughout range of motion resulting in improved stability.
Biology
-
1.
Due to the flat configuration, the surface is increasing in relation to the volume and therefore the interface for tendon to bone healing is larger.
-
2.
The diffusion distance in the flat graft is reduced and therefore could improve or potentially accelerate revascularization and tendon to bone healing.
Technique
Positioning
The patient is positioned supine with a thigh tourniquet. Positioning should allow knee motion between 0 and 120°. We prefer the use of an electric leg holder (Maquet, Rastatt, Germany) and a hanging leg.
Graft Harvesting
Both quadriceps tendon (QT) and hamstring grafts are ideal for this technique and may be used according to surgeon's preference.
Quadriceps Tendon
QT may be harvested in a conventional open technique but a minimally invasive technique using special harvesting instrumentation (Medacta, Castel San Pietro, Switzerland) is preferable, resulting in more precise graft dimensions as well as improving wound cosmesis.
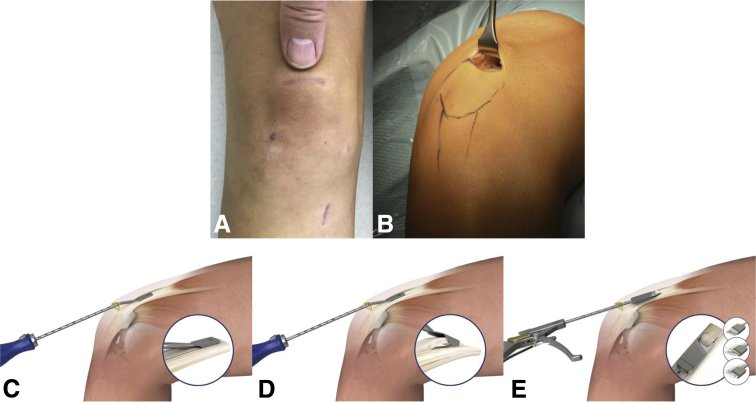
For minimal invasive graft harvest, the knee is flexed to 90° and a 2.5- to 3-cm transverse skin incision is placed over the superior boarder of the patella (Fig 2A). The prepatellar bursa is incised longitudinally and the QT is then carefully exposed. A long Langenbeck retractor is introduced and the QT subcutaneously exposed proximal to the patella (Fig 2B). A double knife (Medacta) in small, medium, or large (depending on the patient's size) is then introduced starting slightly lateral to the middle of the superior patellar boarder (Fig 2C) and advanced approximately 7 cm proximal and about 2 cm distal over the patella.
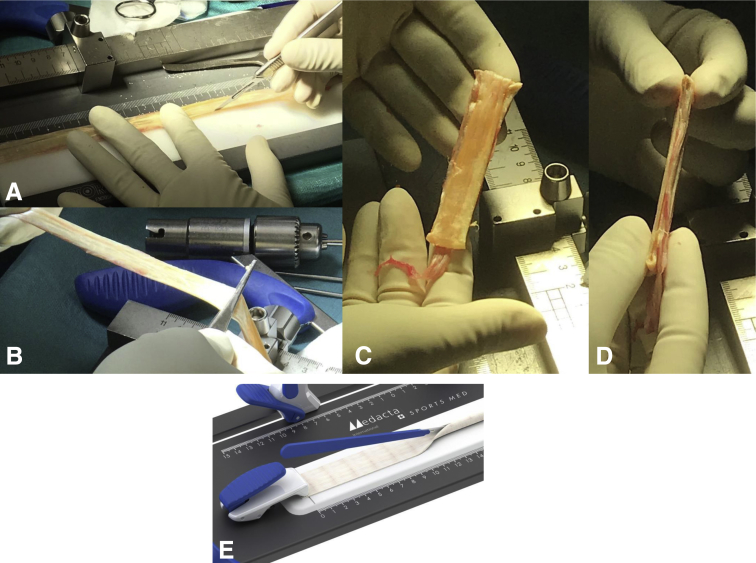
Fig 2.
QT graft harvesting. (A) The scar of a QT ACL 3 months postoperatively and is an example for the incision of harvesting the QT. (B).Left knee intraoperatively in 90° of flexion with subcutaneous dissection already done and a Langenbeck retractor inserted to expose the surface of the QT. After exposure of the tendon, a double knife (Medacta) with the adequate width (small, medium, large) is inserted, shown in (C), starting slightly lateral to the midpoint of the superior patellar border, to a minimum depth of 70 mm (judged using calibrations on the instrument handle) and extending 20 mm distally over the patella. Graft thickness is determined with a 4.5-mm tendon separator (Medacta), which undercuts the QT as shown in (D). The separator is inserted to the same length as the parallel-bladed double knife (min. 70 mm) as determined by calibrations on the instrument handle. In (E), proximal tendon division and retrieval are shown in a schematic knee. Both are accomplished using the tendon cutter/grasper (Medacta). A firm compression of the handle divides the tendon proximally subcutaneously. Keeping the tendon cutter closed around the tendon and retrieving it takes the proximal tendon end with it. (ACL, anterior cruciate ligament; QT, quadriceps tendon.)
Then, a tendon separator of 4.5-mm thickness (Medacta) is inserted and advanced to the appropriate length (Fig 2D). Finally, the graft is cut subcutaneously by a special tendon cutter (Medacta; Fig 2E) and retrieved. Over the patella, the periosteal strip of about 2 cm of the QT is carefully elevated and then cut.21
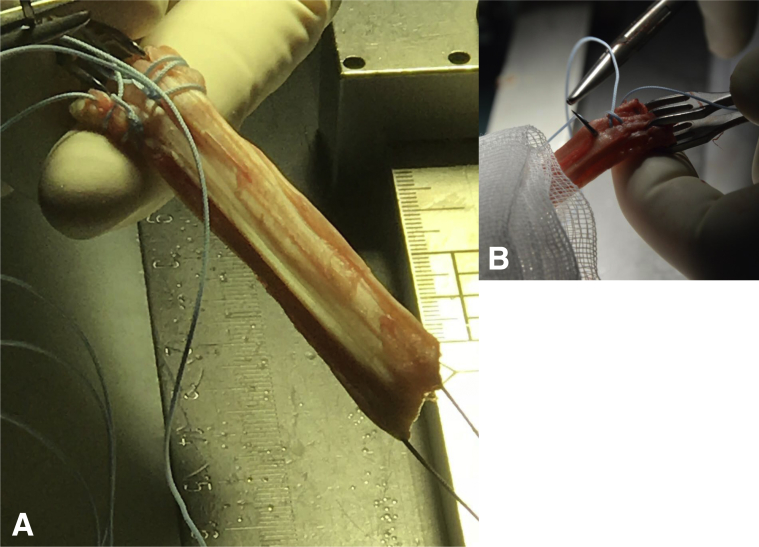
Graft Preparation Quad Tendon
The distal end of the graft (periosteum), which will become the femoral graft end, is folded over a suture (Fig 3A) that is removed after preparation and kept in place with a Lahey-goiter grasping forceps. Krackow-stitch sutures (Fig 4 A and B) are placed on each side of the graft using size 2 nonabsorbable sutures (FiberWire; Arthrex, Naples, FL). The stitches should be done in the outer 3 mm of the graft and the sutures should go back in the mid part of the graft using a simple spiral seam to get pulling strands in every portion of the proximal graft edge (Fig 4 A and C). Putting tension on all sutures shows a slight C-shape form of the proximal graft end and either the concavity or convexity should be marked as lateral or medial, respectively, for insertion. The tendinous end of the graft, which will become the tibial end of the implanted graft, is prepared using an interlocking suturing technique (Krackow-stitch) with two no. 2 non-absorbable sutures size 2 (FiberWire; Arthrex) but without the sutures in the mid part (Fig 3C). The size of the graft should be measured to define the final dimensions of the bone tunnels. The sutures of the proximal end of the graft are tied to the femoral fixation button (Medacta) at the appropriate length for the femoral bone tunnel (Fig 3C). The ideal length is such that the sutures will be slightly recessed into the femoral tunnel aperture or that at least 15 mm of the graft will lie within the tunnel. The length of the femoral tunnel should be marked on the graft. The sutures of the distal end of the graft are thread through the tibial fixation button Pull Suture Plate (PSP; Medacta) such that the concavity of the button looks to the lateral graft side (Fig 3C).
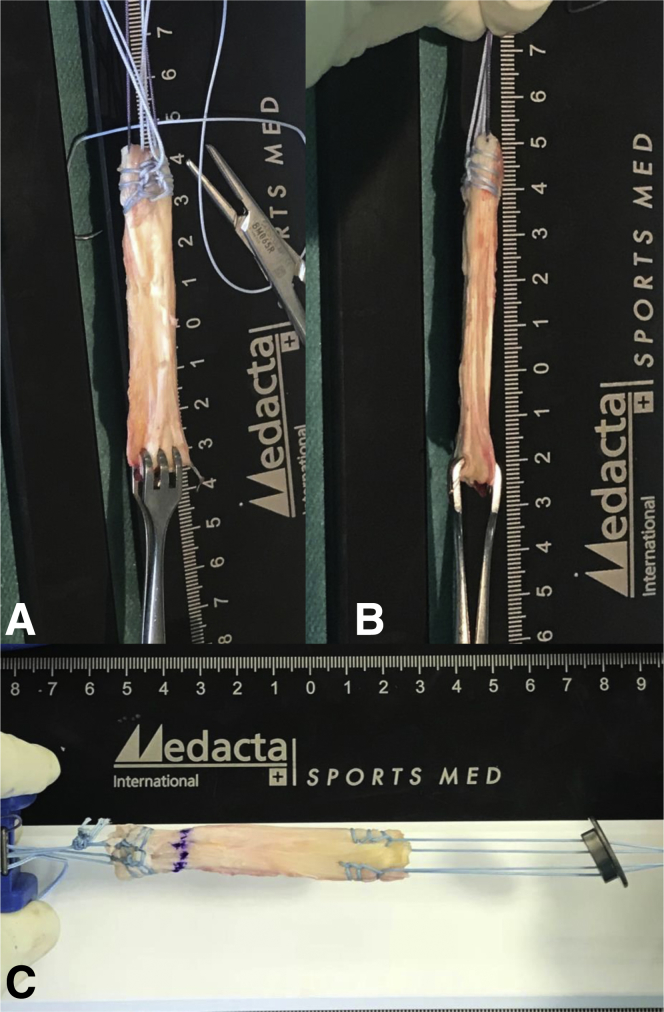
Fig 3.
Final quadriceps tendon graft. (A) The graft with the suture sling for folding the periosteum flap still in place and the proximally already reinforced graft with Krackow-stitches on the lateral edges and a spiral seam in the center. (B) The narrow part of the flat graft. The suturing technique for the distal graft end is Krackow-stitches on both sides, which can be seen in (C) with the PSP already in place. (PSP, Pull Suture Plate.)
Fig 4.
Reinforcement of the graft. For easier, the graft is first folded freely on the preparation board for the second time it should be folded over a suture sling attached to the board that is removed afterwards and the free ends are kept in place using a goiter grasping forceps (A). First, the free ends are prepared using an interlocking suturing technique with two size 2 nonabsorbable sutures (FiberWire; Arthrex). (B) Interlocking mechanism in a quadrupled semiT graft.
Graft Preparation SemiT (With Video Illustration)
The tendon is placed on a preparation table and the length is checked. A length of 26 cm or more should be reached. Then, the muscle is removed from the tendon and it is placed with the muscular side looking upwards on the board. At the end of the muscular insertion site, the tendon is opened up with a knife to the end of the tendon (Fig 5A and E, Video 1). Afterwards, the tendon can be smoothed out with a rasp and should show equal flat dimensions from end to end (Fig 5B). The tendon is folded twice in the middle. First, it is folded free on the board. The second time it should be folded over a suture that is removed after preparation and kept in place with a Lahey-goiter grasping forceps (Fig 3 A and B and Fig 4B). The distal end of the graft is prepared using an interlocking suturing technique (Krackow-stitch) with two no. 2 nonabsorbable sutures (FiberWire; Arthrex; Fig 4 A and B). Krackow-stitch sutures (Fig 4) are placed on the proximal end of the graft using nonabsorbable sutures size 2 (FiberWire; Arthrex). The stitches should be done in the outer 3 mm of the graft and the sutures should go back in the mid part of the graft using a simple spiral seam to get pulling strands in every portion of the proximal graft edge (Fig 6A). Putting tension on all sutures shows a slight C-shaped form of the proximal graft end and either the concavity or convexity should be marked as lateral or medial, respectively, for insertion. The size of the graft should be measured to define the dimensions of the bone tunnels. The sutures of the proximal end of the graft are tied to the femoral fixation button (Medacta) at the appropriate length for the femoral bone tunnel (Fig 6A). The ideal length is such that the sutures will be slightly recessed into the femoral tunnel aperture or that at least 15 mm of the graft will lie within the tunnel. The length of the femoral tunnel should be marked on the graft. The sutures of the distal end of the graft are thread through the tibial fixation button PSP (Medacta) such that the concavity of the button looks to the lateral graft side.
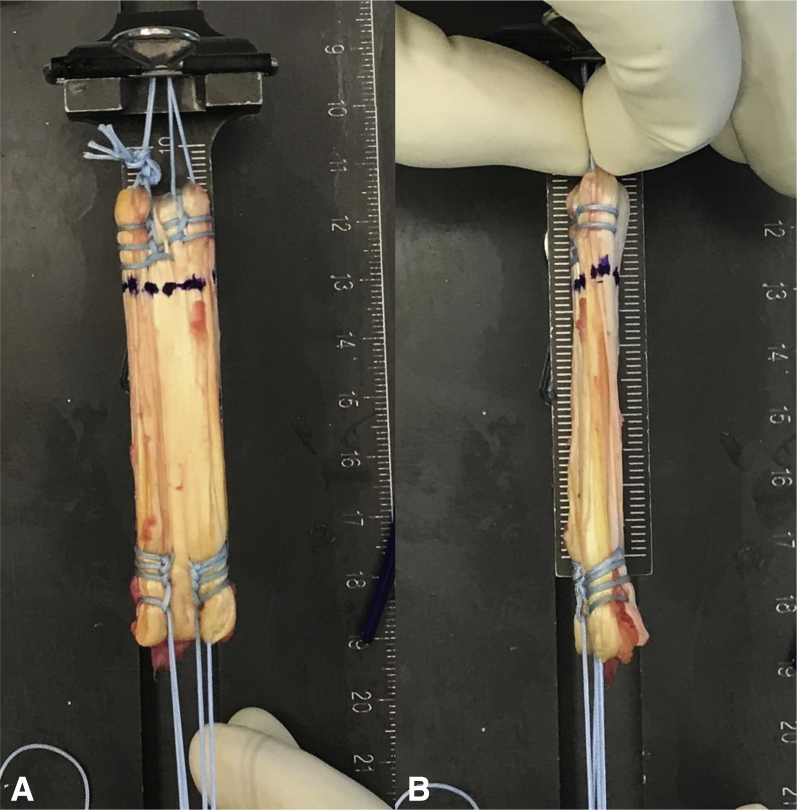
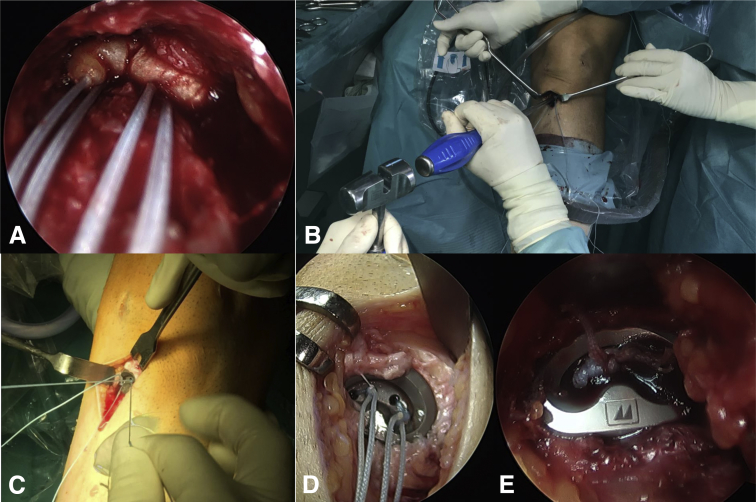
Fig 5.
Converting a round tendon to a flat graft. The tendon is fixed on a preparation board and any fatty or muscular tissue is already removed. The round tendon part of the semiT then is dissected by knife to half of its diameter ([A], with a semiT graft; [E], schematic drawing) and subsequently smoothed into flat shape by blunt raspatorium at minimum pressure (B). As Domnick et al.22 showed, this does not affect the structural properties of the tissue. As in usual ACL reconstructions using a semiT, the tendon is folded twice after the flattening, however, still keeping its flat shape. We aim for a length of 6 to 7 cm. (C) View on the wide part of the quadrupled graft; and (D) on the narrow part. (ACL, anterior cruciate ligament.)
Fig 6.
Final SemiT graft. Krackow-stitches are placed on the outer edges of the proximal graft end. They should be done on the outer 3 mm of the graft and the sutures should go back in the mid part of the graft using a simple spiral seam (A). These sutures are used for suspensory fixation of the graft. The flat appearance is demonstrated on the wide (A) and the narrow (B) part.
Femoral Tunnel
After routine diagnostic arthroscopy in 90° of knee flexion, the ACL remnants are removed, preserving the tibial and femoral footprints showing with a close look the anatomic footprints described by Smigielski et al.3 (Fig. 1). With a knee hyperflexion of 110°, the guidewire with the laser mark (Medacta) for tunnel length measurement is drilled into the mid-portion of the native femoral ACL insertion through the medial portal, after marking the entry point with a microfracture awl (Fig 7 A, B, and D, and Video 1), until the mark on the wire is flush with the femoral condyle (Fig 7E). The position is double-checked viewing from both portals (Fig 7D). Tunnel length is measured extra-articularly over the guidewire, with an outside-in measurement system (Medacta) referencing from the lateral femoral cortex and the laser marking on the wire (Fig 7C and Video 1). The femoral guide (Medacta) is inserted over the guidewire through the central hole and oriented in line of the anatomic ACL insertion (Fig 8 A and C, and Video 1). Two other guidewires are drilled through the additional lateral holes in the femoral guide. They don't need to be drilled through the lateral cortex but about 30 mm (Fig 8 B, D, and I, and Video 1). The femoral aimer (Medacta) is removed and the lateral 2 wires are overdrilled with a 4.5-mm drill bit (Fig 8 E, H, and J, and Video 1) to a depth of 25 to 30 mm depending on the length of the femoral tunnel and the graft and afterwards removed. Overdrilling the lateral cortex should be avoided for these 2. The guidewire in the middle is overdrilled through the lateral cortex and left in place (Fig 8F). The femoral dilator (Medacta) matching the graft size (small, medium, large) is inserted over the guidewire intra-articularly (Fig 9 A and C, and Video 1) and oriented in line with the 2 other holes (Fig 9F). The dilator is inserted to a depth of 25 to 30 mm (Fig 9 B and F) by cautiously tapping the back. The canal should be 7 mm deeper than the length of the graft in the femoral tunnel to allow space for the femoral fixation button to flip. Afterwards, the dilator and the guidewire are removed (Fig 9 D and E, and Video 1). Bone wear should be removed meticulously with the shaver (Fig 9D).
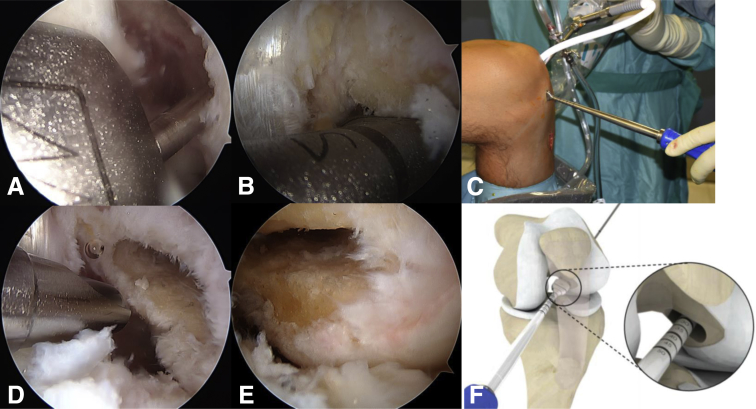
Fig 7.
Femoral tunnel placement. (A) Arthroscopic view of the medial wall of a lateral femoral condyle of a left knee from a lateral standard portal. The midpoint of the femoral origin of the ACL is marked with a microfracturing instrument. Thereafter, the position can be checked through a medial portal view (B). If the position looks adequate, the 2.4-mm guidewire marked for length measurement is inserted and drilled through until the mark is close to the lateral notch wall (D, arthroscopic view from the medial portal; E, schematic view). Finally, a small incision is made in the skin at the exit point of the guidewire for insertion of the indirect measuring instrument (C, intraoperative view of a left knee from lateral). (ACL, anterior cruciate ligament.)
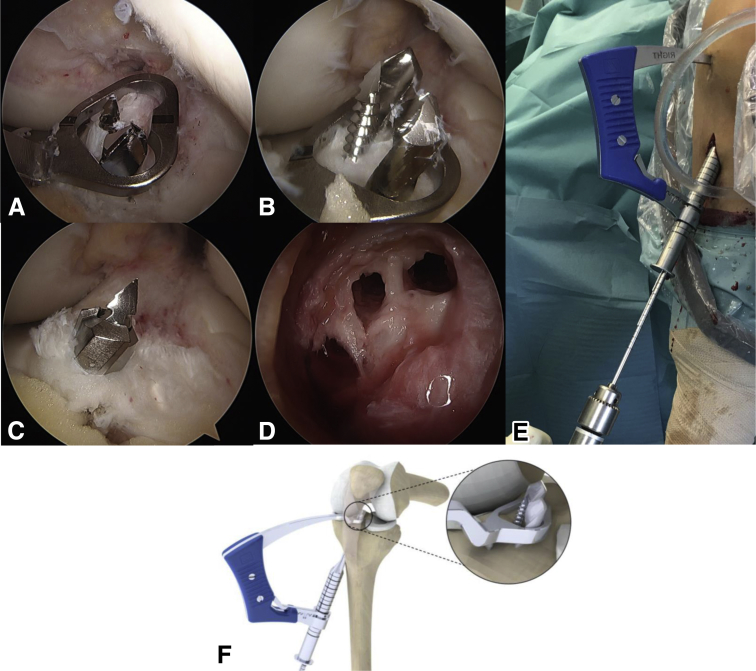
Fig 8.
Aiming for a flat femoral tunnel. (C) The insertion of the femoral guide primarily in line with the incision and in (D) (intraoperative view on a left knee from anterolateral), (I) (schematic drawing) oriented anatomically. (A) Arthroscopic view of the medial wall of the lateral femoral condyle with the first guidewire, described in the previous picture, and the femoral guide already in place from a lateral standard portal. The initial guidewire is inserted in the central hole of the guide and it is then oriented in line of the anatomic ACL insertion. Two other guidewires are drilled through the additional lateral holes in the femoral guide. They don't need to be drilled through the lateral cortex but about 30 mm (I). The femoral aimer is removed (B, arthroscopic view from a lateral standard portal; G, intraoperative view on a left knee in 110° of flexion from anterior) and the lateral 2 wires are overdrilled with a 4.5-mm drill bit to a depth of 25 to 30 mm (E, arthroscopic view from a lateral standard portal; H, intraoperative view on a left knee in 110° of flexion from anterior; J, schematic drawing) depending on the length of the femoral tunnel and the graft and afterwards removed. (F) Medial wall of the lateral condyle from a medial portal view, with the initial guidewire still in place and the 2 lateral drill holes.
Fig 9.
Finalizing the flat femoral tunnel. (C) Insertion of the rectangular dilator (Medacta) in the corresponding size—small, medium, or large in line with the medial incision. (A) Insertion over the guidewire intra-articularly viewed from a lateral standard portal. Like shown in (B) (arthroscopic view from a lateral standard portal) and (F) (schematic drawing) the dilator is then oriented along the other 2 drill holes and impacted to a depth of 25 to 30 mm determined by the calibrations on the instrument handle. (D) The final cleaning of the flat tunnel with the shaver viewed from the lateral standard portal and (E) the corresponding medial portal view.
Tibial Tunnel
The threaded k-wire is inserted in the tip hole of the bullet according to the graft size and inserted it in the tibial guide (Medacta). The tibial aimer (Medacta) is inserted through the medial portal (Fig 10E) with the knee in 90° of flexion again and placed around the anterior horn of the lateral meniscus and with reference to the ACL remnant (Fig 10 A and B, and Video 1). The already inserted guidewire is drilled into the joint (Fig 10 C and D). Now, the short 4.5-mm drill bit is drilled through the anterior hole in the tibial guide into the joint and left in place (Fig 11 A, E, and F, and Video 1). Afterwards, the long 4.5-mm drill bit is drilled through the posterior hole until visible under arthroscopy (Fig 11B) and then both drill bits and the aimer are removed. Now, the cannulated 4.5-mm drill bit is used to over drill the guidewire (Fig 11C) and both are removed (Fig 11D). The blunt guidewires are inserted in the tibial dilator (Medacta) (Fig 12C) and then in the anterior and posterior tibial tunnel (Fig 12 A and G, and Video 1). The dilator should be oriented with its concavity to the lateral meniscus. By tapping the back of the handle, the tibial dilator (Medacta) is inserted in the tibia until visible under arthroscopy (Fig 12B, and Video 1) and then removed (Fig 12 D and E). The first centimeter of the tunnel should always be dilated with the large dilator for perfect fit of the fixation button. Bone wear should again be removed meticulously with the shaver.
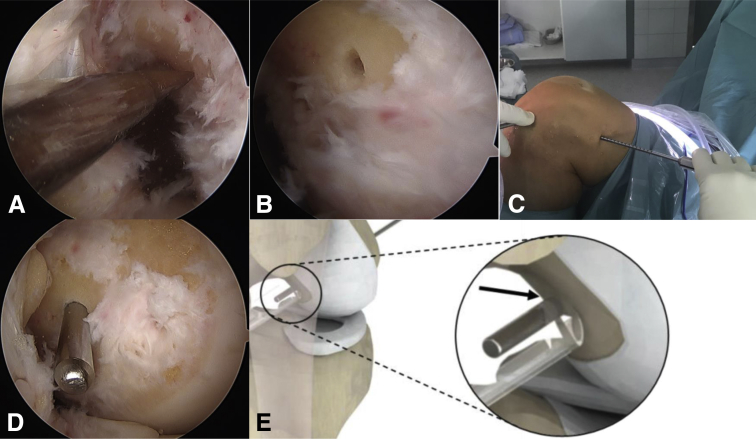
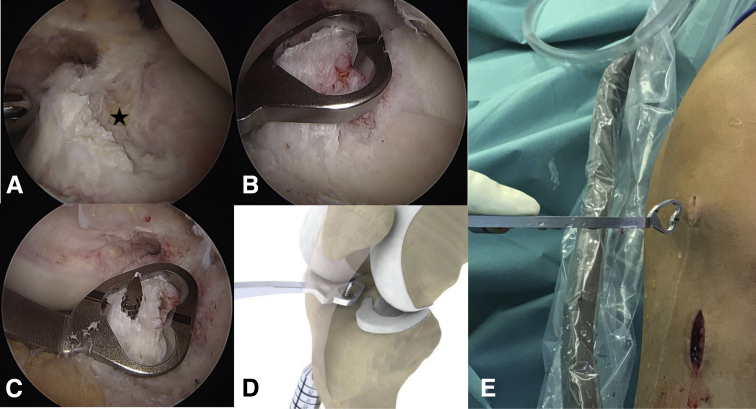
Fig 10.
Aiming for a C-shaped tibial tunnel. (A) Arthroscopic view of the C-shaped tibial insertion site of the ACL and the small fat pad on top of the anterior lateral meniscus root (asterisk) from a lateral standard portal. (E) The insertion of the tibial guide in line with the medial incision (intraoperative view of a left knee from anterior). (B) The tibial aimer is put in place over the remaining ACL stump, sparing the anterior root of the lateral meniscus viewed from a lateral standard portal. (C) The guidewire is inserted and the position is again checked from a lateral standard portal. (D) The corresponding schematic drawing of the tibial guide in a left knee. (ACL, anterior cruciate ligament.)
Fig 11.
Preparation of the C-shaped tibial tunnel. To get the C-shaped tunnel additionally to the first guidewire, two 4.5-mm drill holes on each side of the guidewire need to be placed through the guide (E, intraoperative view of a left knee viewed from anteriorly; F, schematic drawing). (A) The guide and the first wire still in place and the first drill bit already inserted anteriorly. (E) The anterior drill bit should be the short one and the posterior the long one to facilitate instrument handling. (B) The corresponding arthroscopic view with the second drill bit in place is shown from a lateral standard portal. (C) The next step, where the tibial guide and the drill bits are removed and the guidewire is over reamed with a cannulated 4.5-mm drill bit viewed from a lateral standard portal. (D) The final 3 drill holes on the tibial metaphysis are shown.
Fig 12.
Finalizing the C-shaped tibial tunnel. To finalize the C-shaped tunnel, a C-shaped dilator needs to be inserted. The extra-articular preparation with 2 blunt guidewires for the anterior and posterior drill holes is shown in (C). The 2 wires are then inserted in these holes and the dilator oriented with its concavity looking laterally (G, schematic drawing; A, arthroscopic view from a lateral standard portal). By tapping the back of the handle the dilator is inserted into the tibia (F, intraoperative view of a left knee from anterior) until seen intra-articularly (B, arthroscopic view of the dilator with from a lateral standard portal). To do no harm with the guidewires, they glide back into the dilator while insertion as can be seen in (B). (D-E) The final C-shaped tunnel arthroscopically (D) and looking up into the tunnel from outside (E).
Graft Insertion
A Beath pin is introduced via the medial portal and used to pass a Vicryl suture through the femoral tunnel (Fig 13A). The suture loop is grasped intra-articularly via the tibial tunnel (Fig 13B) and pulled extra-articularly distally. The loop is then used to pull the lead sutures for the femoral button through the knee and out through the femoral tunnel aperture proximo-laterally (Fig 13G, and Video 1). The graft is introduced by pulling on the lead sutures. Correct orientation within the tibial tunnel is again with the concavity looking laterally. The graft should be marked on the medial or lateral side before to make it easier. Flipping of the button is confirmed under arthroscopic vision to ensure there is no entanglement of the lead sutures. Key Maneuver: Once the graft emerges from the proximal tibial tunnel into the joint space, before insertion into the femoral tunnel, the knee should be extended to get proper torque of the graft in flexion (Fig 13 C-F). The graft is pulled completely into the flat bone tunnel until the femoral fixation button (Medacta) can be flipped. This is achieved by pulling initially on the leading end of the button until the trailing end has also cleared the lateral cortical bone. There is usually a palpable reduction in resistance as the trailing end of the femoral button (Medacta) clears the 4.5-mm proximal tunnel. Clearance is confirmed by toggling both of the lead sutures, before pulling on the distal/tibial sutures to snug the button against the lateral femur. With tension on the distal sutures of the graft, the knee is cycled from 0 to 90° ten times to condition the graft (Video 1). The mark on the graft should be in line with the femoral tunnel entrance and the lead sutures should get caught between button and bone which can be felt as resistance when pulling on one end. For tibial fixation, the PSP (Medacta) is pulled toward the tibia along the sutures until it sits on the tibial cortex. Now, the PSP impactor (Medacta) is used to place it in the tunnel (Fig 14B). Then, the sutures are tightened again and tied so that the knot is recessed within the PSP (Medacta; Figure 14 C-E, and Video 1).
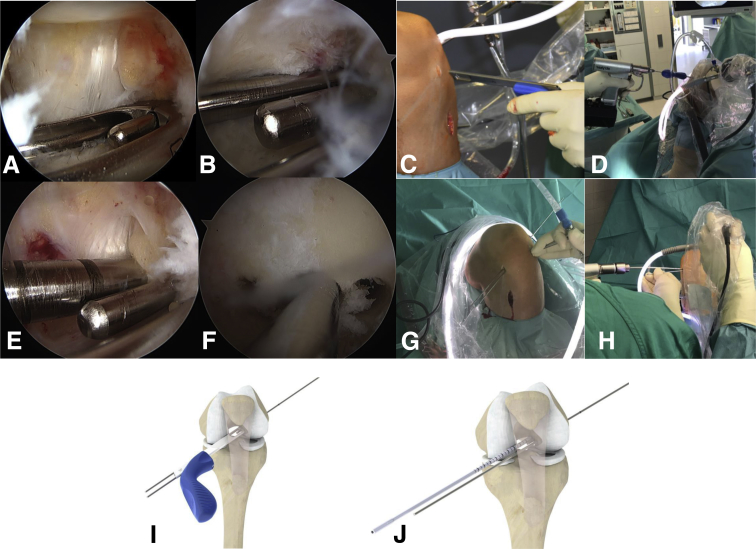
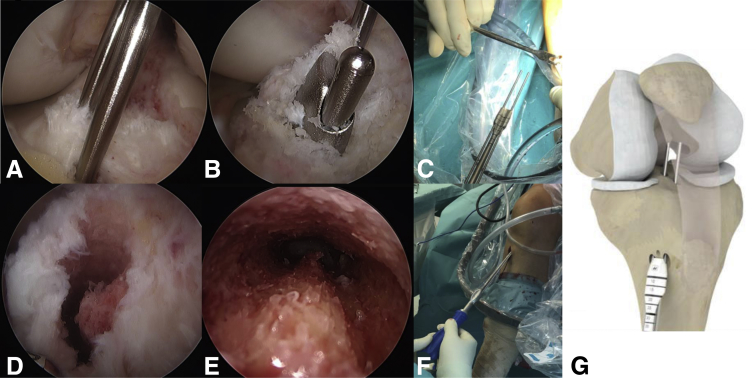
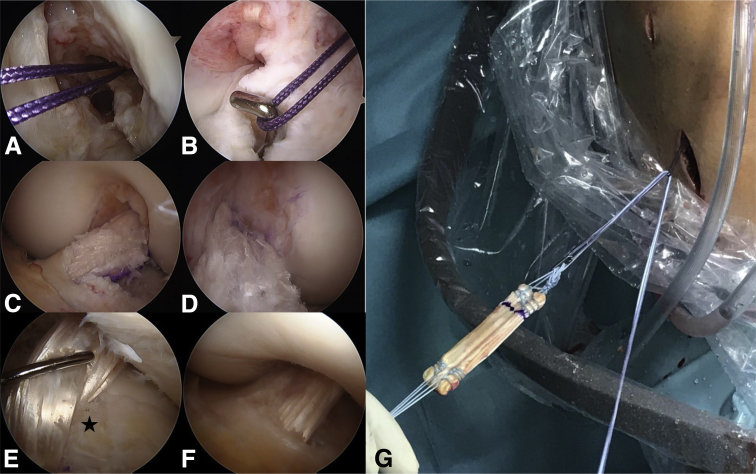
Fig 13.
Graft insertion and final graft appearance. To insert the graft, a shuttle loop is needed: It is first set using a Beath pin via the anteromedial portal seen in (A). The loop is then pulled into the joint and grasped via the tibial tunnel with a hook and pulled extra-articularly distally (B). Using this shuttle loop, the graft is then inserted with its pulling strands, as can be seen in (G) looking on a left knee intraoperatively from anterior, in this case using a flat semiT graft. For insertion, the graft needs to be oriented with its concavity (in G looking up) looking laterally. (C-D) The final quadriceps tendon graft with its natural fiber orientation intra-articularly from a lateral standard portal view and a medial portal view respectively. (E-F) A semiT graft is shown intra-articularly from a lateral standard portal view in 90° of knee flexion (E, asterisk: anterior lateral meniscus root) and close to extension (F).
Fig 14.
Tibial graft fixation. (A) A semiT graft in the C-shaped tibial tunnel looking upwards with the arthroscope. (B) The PSP (Medacta) is tapped into the bone oriented along the C-shaped tunnel with PSP impactor in a left knee. Afterwards, the sutures are again tightened as can be seen in (C) intraoperatively in a left knee. (D) The sutures are so that the knot is recessed within the PSP and in (E) the sutures are cut and the final appearance of the tibial fixation is demonstrated. (PSP, Pull Suture Plate.)
Postoperative Care
Postoperatively, a hinged knee brace limiting flexion to 90° is applied in case of no additional meniscus injuries. Active range-of-motion exercises focusing predominately on gaining full extension are initiated immediately. The patient is mobilized partially weight-bearing (15-20 kg) for 2 weeks. Full weight-bearing and free range of motion are commenced thereafter as tolerated and no additional meniscus injury provided. Physical therapy is recommended 2 to 3 times per week for at least 8 to 12 weeks.
Discussion
We describe a versatile single-bundle anatomic ACL reconstruction technique using either a quad-tendon or a semiT graft that appears to be close to the current view of native ACL anatomy (Fig 1 A-D, and Video 1) Pearls and pitfalls are described in Table 1, and advantages and disadvantages comparing it with a conventional round-tunnel, single-bundle ACL reconstruction are listed in Table 2.
Table 1.
Pearls and Pitfalls
| Surgical Steps | Pearls and Pitfalls |
|---|---|
| Graft preparation | Make sure you have pulling strands in every portion of the proximal graft end; otherwise, you will struggle getting the midportion in the tibial tunnel. Afterwards, put the sutures under tension and mark the convex side as medial. |
| Femoral tunnel | Use the medial portal as a viewing portal after marking the desired position of the femoral tunnel to double-check the planned tunnel is in the correct position. |
| Tibial tunnel | Check the correct position of the tibial guide with a C-shape around the anterior horn of the lateral meniscus—further anterior than usual; otherwise, the anterior horn is at risk with dilating the tibial tunnel. |
| Graft insertion | Before insertion, meticulously clean up the tibial entrance to avoid soft-tissue interference with the graft and put the convex side of the graft looking medially. When the graft enters the joint, put the knee close to extension and you will obtain the right orientation of the graft automatically. |
| Tibial fixation | Always open the first 5 mm of the tibial tunnel using the large dilator to make sure the PSP sits in the tunnel properly and then tie the sutures and place the knot in the recess. |
PSP, Pull Suture Plate.
Table 2.
Advantages and Disadvantages
| Technical Aspect | Advantages | Neutral | Disadvantages |
|---|---|---|---|
| Flat “ribbon-like” graft | Recreates native fiber arrangement with either a quadriceps tendon or a hamstring graft. | No difference in graft size (cross-sectional area). | Learning curve for graft preparation. |
| Rectangular femoral tunnel | Recreates anatomic ACL origin. Reduces the distance for blood vessel ingrowth. |
Guidewire location is the same. | More surgical steps in tunnel preparation. |
| C-shaped tibial tunnel | Recreates anatomic “C”-shaped insertion. Preserves the anterior tibial insertion of the lateral meniscus. Reduces the distance for blood vessel ingrowth. |
– | More steps in tunnel preparation. |
| Graft insertion | Graft orientation during insertion is achieved with simply extending the knee. | – | Exact graft preparation is required to avoid problems with insertion due to high frictional resistance. |
ACL, anterior cruciate ligament.
Graft Orientation and Tunnel Geometry
Commonly used ACL reconstruction techniques use drills to create bone tunnels for graft insertion. However, this seems to be the only explanation for them being round, because neither the femoral nor the tibial insertion sites are round. Flat and C-shaped tunnels respectively offer obvious and potential advantages.
On the femoral side, the flat tunnel mimics the direct insertion fibers (Fig 1 A and B and Fig 15 A and E) and the flat graft resembles the native ACL changing its fiber orientation in different flexion angles and therefore facilitating the reconstruction of all functional fiber bundles without overstuffing the notch.
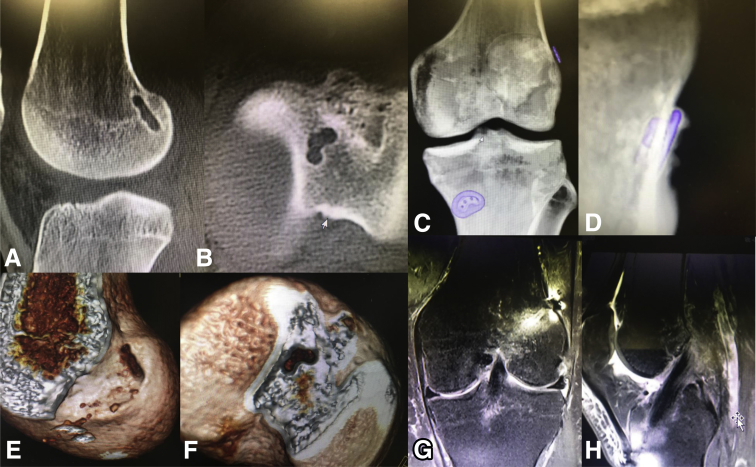
Fig 15.
Postoperative imaging. (A) Sagittal cut of the femur postoperatively and the flat femoral tunnel in continuity of the posterior femoral cortex as described by Smigielski et al.3 (B) The axial cut of a right tibia is visible with the C-shaped tibial tunnel. (E) (femoral) and (F) (tibial) show the corresponding 3-dimensional volume renderings of a right knee. (C-D) The femoral and tibial fixation material is demonstrated in 3-dimensional volume renderings with the tibial PSP sitting tight in the bone (C, anteroposterior view of a left knee; D, tangential view of the tibial button of the same knee). (G) The frontal cut and (H) a sagittal cut of a left knee 3 months after Medacta Antomic Ribbon Surgery (MARS; Medacta International, Castel San Pietro, Switzerland) reconstruction. Almost no fluid can be seen around the graft and hardly any bone edema. (PSP, Pull Suture Plate.).
The native tibial insertion site has been shown to be C-shaped (67%) or J-shaped (24%)3 (Fig 1 C and D, and Video 1), which can be achieved most closely with the C-shaped tunnel (Fig 15 B and F) in the tibia. Furthermore, the C-shaped tunnel of the tibia potentially avoids laceration of the anterior horn of the lateral meniscus compared with conventional round tunnel placement.10
The increased graft–bone contact area of a flat ACL graft compared with a round graft with similar cross-sectional area may provide a biological advantage, leading to accelerated ingrowth19 and probably less central graft necrosis. The flat graft appearance may also present biomechanical advantages similar to ACL double bundle reconstruction or rectangular bone tunnels.14, 15, 16 All of these theoretical advantages of the aforementioned technique are currently investigated thoroughly using sequential magnetic resonance imaging and computed tomography scans (Fig 15 A-H) as well as robotic technology.
Conclusions
Early clinical experience of this ACL reconstruction technique is very promising, with no adverse effects to date. However, whether this technique will lead to long-term benefits over conventional ACL reconstruction techniques remains to be seen.
Footnotes
The authors report the following potential conflict of interest or source of funding: R. Smigielski reports personal fees from Medacta, during the conduct of the study. R. Siebold reports personal fees from Medacta, outside the submitted work. In addition, R. Siebold has a patent from Medacta with royalties paid. M.H. reports personal fees from Medacta, outside the submitted work. C.F. reports personal fees from Medacta, during the conduct of the study; and personal fees from Karl Storz, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video shows a single-bundle ACL reconstruction technique according to the recent ACL anatomy, which describes the ACL as a flat, “ribbon-like” structure with a thin, oval-shaped insertion on the femur and a C-shaped tibial insertion. This reconstruction technique can be performed using quadriceps or semitendinosus tendon. Hamstring grafts can be easily converted to a flat shape by cutting the graft 50% of the diameter in the tubular aspect of the graft. Afterwards, the graft can be squeezed with a forceps or rasp to convert the graft into flat shape without any negative impact on structural properties of the graft. The graft can be folded 2 times to end up in a 4-folded hamstring graft. After suture fixation of the semitendinosus graft at femoral and tibial ending with Krackow stitches, the graft shows a permanent flat shape. Alternatively, the quadriceps tendon is a very useful graft. It can be harvested minimal invasively with special instruments in a small, medium, or large × 4.5-mm flat shape and fixed with the buttons in a similar way as the semitendinosus tendon. Medacta Antomic Ribbon Surgery (MARS; Medacta International, Castel San Pietro, Switzerland) operation technique: After cleaning the lateral notch wall, the central position of the femoral tunnel is marked with a microfracture awl and using a special aimer 3 K-wires are placed in horizontal position in 110° of knee flexion. After overdrilling the k-wires, the rectangular femoral socket is produced using a k-wire–guided dilator in 3sizes (small, medium, or large) depending on the graft size. A special tibial aimer that fits very nicely on the C-shaped ACL insertion is used to place a central k-wire and two 4.5-mm drill holes. After overdrilling the central k-wire, the tibial tunnel is finished by using C-shaped dilators (sizes small, medium, or large). The graft is inserted with correct orientation of the anterior/posterior tibial and femoral fibers and is fixed on both sides with a cortical button to preserve a wide bone to tendon contact surface for optimal biological healing. Alternatively, a hybrid fixation could be done following the preferences of the surgeon. Magnetic resonance imaging and computed tomography scans of clinical cases show fiber orientation close to the native ACL and tunnel shapes resembling the natural insertion of the ACL origin described by Smigielski et al.3,5 (ACL, anterior cruciate ligament.).
References
- 1.Mochizuki T., Muneta T., Nagase T., Shirasawa S., Akita K.I., Sekiya I. Cadaveric knee observation study for describing anatomic femoral tunnel placement for two-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2006;22:356–361. doi: 10.1016/j.arthro.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 2.Kyung B.S., Kim J.G., Chang M., Jang K.M., Lee S.S., Ahn J.H. Anatomic double-bundle reconstruction techniques result in graft obliquities that closely mimic the native anterior cruciate ligament anatomy. Am J Sports Med. 2013;41:1302–1309. doi: 10.1177/0363546513484692. [DOI] [PubMed] [Google Scholar]
- 3.Smigielski R., Zdanowicz U., Drwiega M., Ciszek B., Williams A. The anatomy of the anterior cruciate ligament and its relevance to the technique of reconstruction. Bone Joint J. 2016;98-B:1020–1026. doi: 10.1302/0301-620X.98B8.37117. [DOI] [PubMed] [Google Scholar]
- 4.Siebold R., Schuhmacher P., Fernandez F. Flat midsubstance of the anterior cruciate ligament with tibial "C"-shaped insertion site. Knee Surg Sports Traumatol Arthrosc. 2015;23:3136–3142. doi: 10.1007/s00167-014-3058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smigielski R., Zdanowicz U., Drwiega M., Ciszek B., Ciszkowska-Lyson B., Siebold R. Ribbon like appearance of the midsubstance fibres of the anterior cruciate ligament close to its femoral insertion site: A cadaveric study including 111 knees. Knee Surg Sports Traumatol Arthrosc. 2015;23:3143–3150. doi: 10.1007/s00167-014-3146-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kawaguchi Y., Kondo E., Takeda R., Akita K., Yasuda K., Amis A.A. The role of fibers in the femoral attachment of the anterior cruciate ligament in resisting tibial displacement. Arthroscopy. 2015;31:435–444. doi: 10.1016/j.arthro.2014.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nawabi D.H., Tucker S., Schafer K.A. ACL fibers near the lateral intercondylar ridge are the most load bearing during stability examinations and isometric through passive flexion. Am J Sports Med. 2016;44:2563–2571. doi: 10.1177/0363546516652876. [DOI] [PubMed] [Google Scholar]
- 8.Karakasli A., Acar N., Basci O., Karaarslan A., Erduran M., Kaya E. Iatrogenic lateral meniscus anterior horn injury in different tibial tunnel placement techniques in ACL reconstruction surgery—A cadaveric study. Acta Orthop Traumatol Turc. 2016;50:514–518. doi: 10.1016/j.aott.2016.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Watson J.N., Wilson K.J., LaPrade C.M. Iatrogenic injury of the anterior meniscal root attachments following anterior cruciate ligament reconstruction tunnel reaming. Knee Surg Sports Traumatol Arthrosc. 2015;23:2360–2366. doi: 10.1007/s00167-014-3079-1. [DOI] [PubMed] [Google Scholar]
- 10.LaPrade C.M., Smith S.D., Rasmussen M.T. Consequences of tibial tunnel reaming on the meniscal roots during cruciate ligament reconstruction in a cadaveric model, Part 1: The anterior cruciate ligament. Am J Sports Med. 2015;43:200–206. doi: 10.1177/0363546514554769. [DOI] [PubMed] [Google Scholar]
- 11.Logan M.C., Williams A., Lavelle J., Gedroyc W., Freeman M. Tibiofemoral kinematics following successful anterior cruciate ligament reconstruction using dynamic multiple resonance imaging. Am J Sports Med. 2004;32:984–992. doi: 10.1177/0363546503261702. [DOI] [PubMed] [Google Scholar]
- 12.Ristanis S., Giakas G., Papageorgiou C.D., Moraiti T., Stergiou N., Georgoulis A.D. The effects of anterior cruciate ligament reconstruction on tibial rotation during pivoting after descending stairs. Knee Surg Sports Traumatol Arthrosc. 2003;11:360–365. doi: 10.1007/s00167-003-0428-x. [DOI] [PubMed] [Google Scholar]
- 13.Amis A.A. The functions of the fibre bundles of the anterior cruciate ligament in anterior drawer, rotational laxity and the pivot shift. Knee Surg Sports Traumatol Arthrosc. 2012;20:613–620. doi: 10.1007/s00167-011-1864-7. [DOI] [PubMed] [Google Scholar]
- 14.Zhang J., Hu X., Liu Z., Zhao F., Ma Y., Ao Y. Anatomical single bundle anterior cruciate ligament reconstruction with rounded rectangle tibial tunnel and oval femoral tunnel: A prospective comparative study versus conventional surgery. Am J Transl Res. 2019;11:1908–1918. [PMC free article] [PubMed] [Google Scholar]
- 15.Herbort M., Tecklenburg K., Zantop T. Single-bundle anterior cruciate ligament reconstruction: a biomechanical cadaveric study of a rectangular quadriceps and bone–patellar tendon–bone graft configuration versus a round hamstring graft. Arthroscopy. 2013;29:1981–1990. doi: 10.1016/j.arthro.2013.08.030. [DOI] [PubMed] [Google Scholar]
- 16.Jacobi M., Magnussen R.A., Villa V., Demey G., Neyret P. The concept of double bundle ACL simulation with a single bundle patellar tendon graft. A cadaveric feasibility study. Sports Med Arthrosc Rehabil Ther Technol. 2012;4:19. doi: 10.1186/1758-2555-4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hexter A.T., Pendegrass C., Haddad F., Blunn G. Demineralized bone matrix to augment tendon-bone healing: A systematic review. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117734517. 2325967117734517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Janssen R.P., Scheffler S.U. Intra-articular remodelling of hamstring tendon grafts after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22:2102–2108. doi: 10.1007/s00167-013-2634-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao F., Hu X., Zhang J. A more flattened bone tunnel has a positive effect on tendon-bone healing in the early period after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:3543–3551. doi: 10.1007/s00167-019-05420-7. [DOI] [PubMed] [Google Scholar]
- 20.Chiang E.R., Chen K.H., Chih-Chang Lin A. Comparison of tunnel enlargement and clinical outcome between bioabsorbable interference screws and cortical button-post fixation in arthroscopic double-bundle anterior cruciate ligament reconstruction: A Prospective, randomized study with a minimum follow-up of 2 years. Arthroscopy. 2019;35:544–551. doi: 10.1016/j.arthro.2018.08.039. [DOI] [PubMed] [Google Scholar]
- 21.Fink C., Herbort M., Abermann E., Hoser C. Minimally invasive harvest of a quadriceps tendon graft with or without a bone block. Arthrosc Tech. 2014;3:e509–e513. doi: 10.1016/j.eats.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Domnick C., Herbort M., Raschke M.J. Converting round tendons to flat tendon constructs: Does the preparation process have an influence on the structural properties? Knee Surg Sports Traumatol Arthrosc. 2017;25:1561–1567. doi: 10.1007/s00167-015-3749-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video shows a single-bundle ACL reconstruction technique according to the recent ACL anatomy, which describes the ACL as a flat, “ribbon-like” structure with a thin, oval-shaped insertion on the femur and a C-shaped tibial insertion. This reconstruction technique can be performed using quadriceps or semitendinosus tendon. Hamstring grafts can be easily converted to a flat shape by cutting the graft 50% of the diameter in the tubular aspect of the graft. Afterwards, the graft can be squeezed with a forceps or rasp to convert the graft into flat shape without any negative impact on structural properties of the graft. The graft can be folded 2 times to end up in a 4-folded hamstring graft. After suture fixation of the semitendinosus graft at femoral and tibial ending with Krackow stitches, the graft shows a permanent flat shape. Alternatively, the quadriceps tendon is a very useful graft. It can be harvested minimal invasively with special instruments in a small, medium, or large × 4.5-mm flat shape and fixed with the buttons in a similar way as the semitendinosus tendon. Medacta Antomic Ribbon Surgery (MARS; Medacta International, Castel San Pietro, Switzerland) operation technique: After cleaning the lateral notch wall, the central position of the femoral tunnel is marked with a microfracture awl and using a special aimer 3 K-wires are placed in horizontal position in 110° of knee flexion. After overdrilling the k-wires, the rectangular femoral socket is produced using a k-wire–guided dilator in 3sizes (small, medium, or large) depending on the graft size. A special tibial aimer that fits very nicely on the C-shaped ACL insertion is used to place a central k-wire and two 4.5-mm drill holes. After overdrilling the central k-wire, the tibial tunnel is finished by using C-shaped dilators (sizes small, medium, or large). The graft is inserted with correct orientation of the anterior/posterior tibial and femoral fibers and is fixed on both sides with a cortical button to preserve a wide bone to tendon contact surface for optimal biological healing. Alternatively, a hybrid fixation could be done following the preferences of the surgeon. Magnetic resonance imaging and computed tomography scans of clinical cases show fiber orientation close to the native ACL and tunnel shapes resembling the natural insertion of the ACL origin described by Smigielski et al.3,5 (ACL, anterior cruciate ligament.).