Abstract
Latissimus dorsi tendon ruptures are less-common injuries that can occur in elite throwing athletes. Physical examination of the thrower with a latissimus injury may show ecchymosis of the upper arm and asymmetry of the posterior axillary fold along with possible weakness in shoulder adduction, extension, and internal rotation. Magnetic resonance imaging is used to confirm the diagnosis. Latissimus tendon ruptures are largely treated nonoperatively; surgical repair is only advocated for in professional throwing athletes with complete avulsion injuries or midsubstance latissimus tendon tears. Surgical repair options include the use of suture anchors, cortical suture buttons, or transosseous sutures via a single posterior axillary incision or a 2-incision technique. Given the limited literature on this topic, there have been no studies evaluating the different fixation options or surgical approaches for tendon repair. This article and accompanying video show the technique and discusses the technical pearls of a latissimus tendon repair using suture button fixation via a single-incision approach.
Latissimus dorsi tendon ruptures are less-common injuries and are of significance in the high-level athlete; these injuries have been documented in elite baseball pitchers, cross-fit athletes, in water-skiing sports, rocking climbing, tennis, and golf.1, 2, 3, 4 The latissimus originates from the inferior thoracic and lumbar spinous processes, iliac crests, and lower ribs, and externally rotates 90° before inserting onto the intertubercular groove of the humerus. The intimately associated teres major muscle run deeps and superior to the latissimus and inserts on the medial lip of the intertubercular groove but also can coalesce with the latissimus to form one tendon. These muscles function in internal rotation, extension, and adduction of the humerus and are most active during the late cocking and acceleration phases of the pitching cycle.5
Athletes with latissimus injuries may complain of posterior shoulder pain with possible deformity of the posterior axillary fold. On examination, patients may have ecchymosis about the arm and posterolateral chest wall with loss of the posterior axillary fold, and there may be weakness and pain with resisted shoulder adduction and extension. Plain radiographs will be unremarkable and may show a small bone fragment in cases of tendon avulsion. Magnetic resonance imaging is obtained to confirm the diagnosis and rule out any other injuries of the shoulder girdle (Fig 1). Standard shoulder magnetic resonance imaging may not capture the latissimus musculotendinous unit, so the clinician may need to obtain an extended field of view to include the lateral chest wall if suspicion for a latissimus injury is high.5 Injury can occur at any location along the muscle tendon unit, with most common injuries being muscle belly strains. Tendon avulsions and midsubstance tendon tears can be surgically repaired whereas musculotendinous junctional tears and muscle belly strains are treated nonoperatively.1
Fig 1.
Magnetic resonance images of a right shoulder of a professional baseball pitcher who sustained a latissimus tendon rupture are shown. Axial (A) and coronal (B) T2-weighted images show rupture of the latissimus tendon off of the humeral footprint with retraction and surrounding edema. (G, glenoid; H, humerus; LT, latissimus tendon.)
Nonoperative treatment consists of a period of rest and pain control, followed by progressive shoulder range-of-motion exercises, and finally strengthening exercises. For complete latissimus avulsion injuries or midsubstance tendon tears in the elite or professional overhead throwing athlete, surgical repair is advocated. The 2 surgical approaches for repair include a single-incision technique for both tendon retrieval and repair and a dual incision technique that uses a deltopectoral approach for exposure of the footprint and a posterior axillary incision for tendon retrieval. This article and accompanying video illustrate our technique for latissimus dorsi tendon repair using a single posterior axillary incision with suture button fixation (Video 1).
Surgical Technique
Patient Positioning
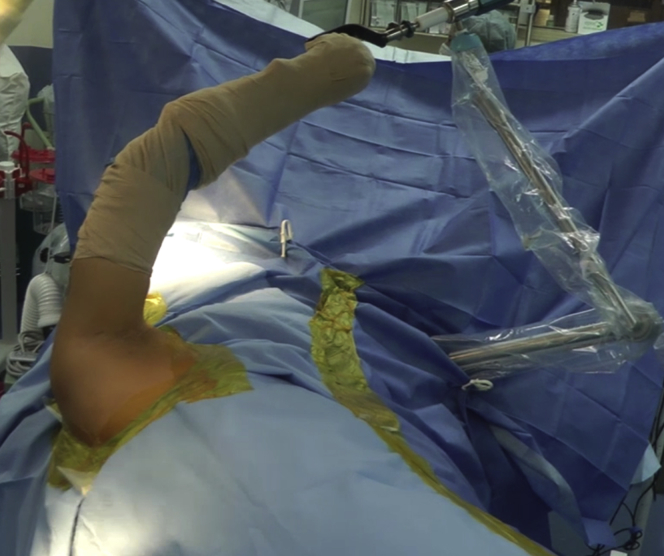
After anesthesia is administered, the patient is placed in the lateral decubitus position with the use of a bean bag immobilizer with the arm placed in a dynamic limb positioner (SPIDER2; Smith & Nephew, London, United Kingdom). The forearm is secured into the positioner so that the arm is abducted and internally rotated (Fig 2).
Fig 2.
The patient is positioned in the left lateral decubitus position with the use of a bean bag and the operative right upper extremity is placed in a dynamic limb positioner as shown (SPIDER2; Smith & Nephew). The forearm is secured to the positioner so that the arm is abducted and internally rotated to allow access to the posterior axillary fold for this single incision repair technique.
Exposure
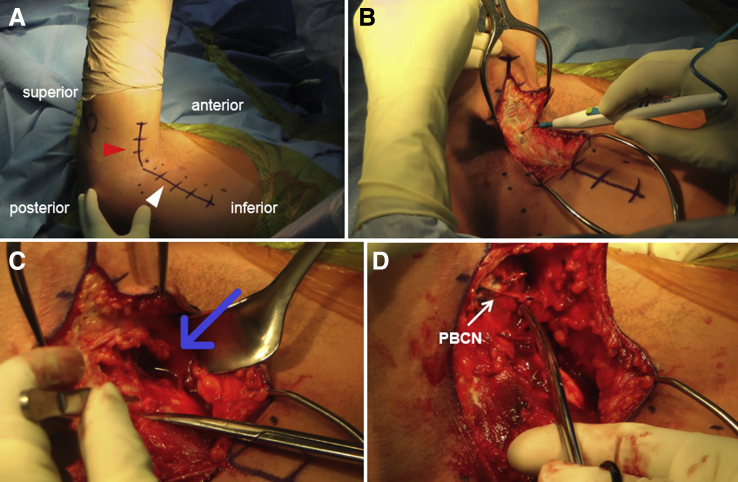
The skin is marked extending from the arm into the posterior chest wall along the posterior axillary fold (Fig 3A). The incision along the arm is for the humeral footprint exposure, which remains relatively constant, and the incision along the posterior chest wall can be extended as needed for a retracted tendon. An 8- to 10-cm incision is made and taken down to the fascia. Self-retaining retractors are placed to tension the skin and subcutaneous tissues to aid in visualization and dissection (Fig 3B). A mix of blunt and sharp dissection is used in between the triceps and the pectoralis major to identify the retracted latissimus dorsi tendon along with the associated teres major. A seroma cavity often is encountered when dissection is performed near the tendon stump (Fig 3C). As dissection proceeds toward the humerus, care is taken to identify and preserve branches of the posterior brachial cutaneous nerve (Fig 3D). Once identified, the posterior brachial cutaneous nerve can be retracted posteriorly along with the triceps.
Fig 3.
The patient is positioned in the left lateral decubitus position with the right upper extremity draped onto a limb positioner to keep the arm abducted and internally rotated. (A) The skin is marked along the posterior axillary fold with the incision along the humerus corresponding to the exposure for the humeral footprint (red arrowhead) and the inferior aspect of the incision along the posterior chest wall (white arrowhead) is for retrieval of the retracted latissimus tendon and can be extended as needed. (B) Retractors are used to tension the skin as dissection continues through the soft tissues down to fascia. A mixture of sharp and blunt finger dissection is used in between the pec major and triceps to identify the latissimus tendon. (C) A seroma cavity can be encountered (blue arrow) as dissection continues near the tendon stump. (D) As dissection proceeds toward the humerus, branches of the posterior brachial cutaneous nerve (white arrow) are identified and protected as they lay over the triceps. (PBCN, posterior brachial cutaneous nerve.)
Tendon Preparation
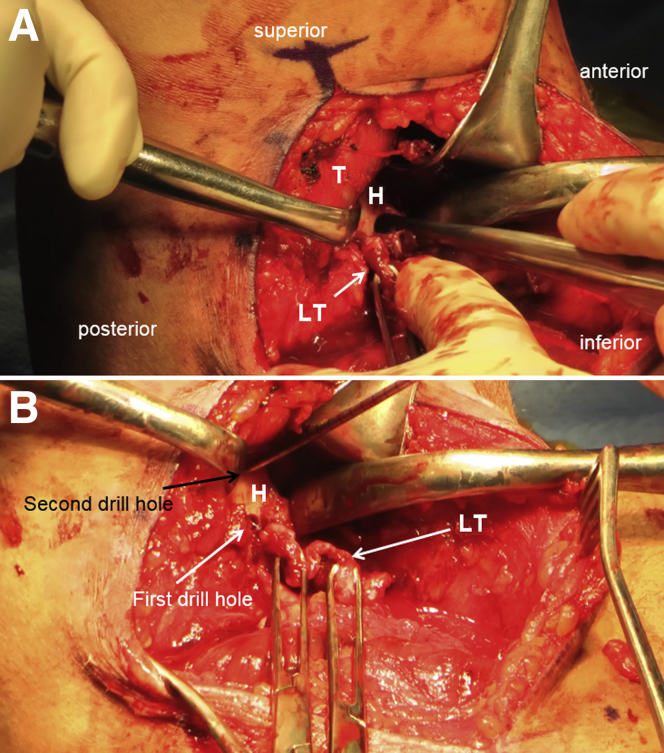
Once the latissimus tendon is identified, a mixture of blunt and sharp dissection is used to mobilize the tendon from its proximal adhesions (Fig 4A) to allow for excursion back to its footprint onto the humerus. The tendon is provisionally tensioned and placed over the footprint to determine whether there is adequate mobilization of the tendon. Two SutureTape sutures (Arthrex; Naples, FL) are then passed through the tendon in simple running locking Krackow fashion to create 4 limbs of suture (Fig 4B). The tendon is then repeatedly tensioned to minimize creep. It is important to be aware of the proximity of the axillary nerve during this procedure, which is expected to be just deep and proximal to the tendon in the floor of the exposure.
Fig 4.
The patient is positioned in the left lateral decubitus position with the right latissimus tendon exposed through a single posterior axillary incision. (A) Once identified, the latissimus tendon stump is controlled with clamps and a mixture of sharp and blunt finger dissection is used to mobilize the tendon from its proximal adhesions to allow for excursion back to its footprint onto the humerus. Once adequately mobilized, 2 SutureTape sutures (Arthrex) are passed through the tendon in simple running locking Krackow fashion to create four limbs of suture as shown (B). The tendon is then repeatedly tensioned to minimize creep. (LT, latissimus tendon.)
Footprint Preparation
The humerus is maximally internally rotated to expose the intertubercular groove. One retractor is placed anteriorly to retract and protect the pectoralis major, biceps, and radial nerve. A second retractor is placed posteriorly to retract the triceps and branches of the posterior brachial cutaneous nerve, and a third retractor is placed at the apex of the wound to aid in visualization. Any remaining soft tissue on the footprint is debrided and the bone is abraded with a curette (Fig 5A). Once adequate exposure of the footprint is obtained, 2 unicortical drill holes are made with the appropriate drill size, one proximal and one distal about 1-2cm apart (Fig 5B), to accommodate passage of 2 suture buttons unicortically.
Fig 5.
The patient is positioned in the lateral decubitus position and the right latissimus tendon has been exposed, mobilized, and controlled with suture. Next, the footprint of the latissimus tendon on the humerus is exposed between the triceps and pectoralis major. One retractor is placed anteriorly to retract and protect the pectoralis major, biceps, and radial nerve. A second retractor is placed posteriorly to retract the triceps and branches of the posterior brachial cutaneous nerve and a third retractor is placed at the apex of the wound to aid in visualization. (A) Any remaining soft tissue on the footprint is debrided and the bone is abraded with a curette. Once adequate exposure of the footprint is obtained, 2 unicortical drill holes are made with the appropriate drill size, one proximal and one distal about 1 to 2 cm apart (B), to accommodate passage of 2 suture buttons unicortically. (H, humerus; LT, latissimus tendon; T, triceps.)
Fixation
Two suture buttons will be used for tendon fixation. The first set of SutureTape controlling the tendon is loaded onto a suture button in standard fashion according to the tension-slide technique with one limb entering proximally and exiting distally and the other limb entering distally and exiting proximally (Fig 6A). With the button inserter, the loaded suture button is then placed through one of the unicortical drill holes and flipped to engage the cortex (Fig 6B). The same sequence of events is repeated for the second suture button as it is loaded with the second set of SutureTape controlling the tendon, inserted through the second drill hole, and flipped to engage the cortex. It is essential to keep in mind that the latissimus tendon externally rotates 90° before inserting onto the humerus so the appropriate buttons are placed in the appropriate proximal or distal drill hole according to the orientation of the tendon as it would insert onto the footprint.
Fig 6.
The patient is positioned in the lateral decubitus position, and the right latissimus tendon is repaired back to its footprint on the humerus. A suture button is placed unicortically through each drill hole. (A) Each SutureTape suture that is passed through the latissimus tendon is loaded onto a suture button using the tension-slide technique with one strand of suture entering proximally and exiting distally on the button and the other suture strand entering distally and entering proximally. (B) The loaded suture button is placed unicortically through the drill hole using the inserter and the button is flipped to engage the cortex. The same sequence of events is repeated for the second suture button. Once the buttons are placed, flipped, and are engaging the cortex, one suture tail from each of the buttons is passed through the substance of the tendon from deep to superficial using a free needle. These limbs that are passed through the tendon allow for the knots to lay superficially on the tendon and will serve as the post strand for knot tying. The suture limbs from each SutureTape are sequentially tensioned to reduce the tendon back to its footprint (C). Both sets of suture are then tied using an arthroscopic knot pusher to facilitate knot tension deep in the wound (D). An arthroscopic cutter is then used to leave short tails. (AKP, arthroscopic knot pusher; LT, latissimus tendon; SB, suture button; SBI, suture button inserter; ST, SutureTape.)
Once the buttons are placed, flipped, and are engaging the cortex, one suture tail from each of the buttons is passed through the substance of the tendon from deep to superficial using a free needle. These limbs that are passed through the tendon allow for the knots to lay superficially on the tendon and will serve as the post strand for knot tying. The suture limbs from each SutureTape are sequentially tensioned to reduce the tendon back to its footprint (Fig 6C). Both sets of sutures are then tied using an arthroscopic knot pusher to facilitate knot tension deep in the wound (Fig 6D). An arthroscopic cutter is then used to leave short tails.
Closure
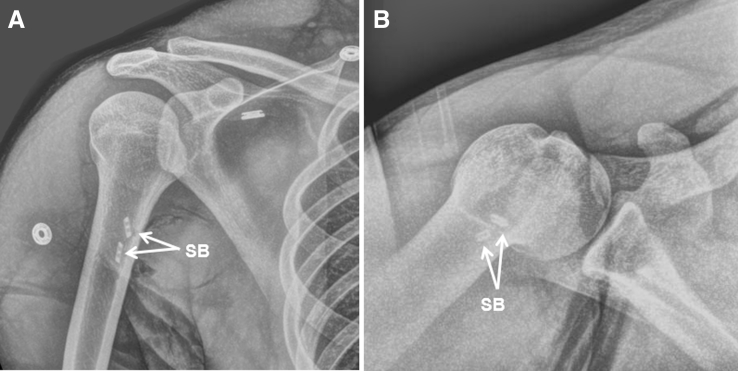
After irrigation, closure of the wound is performed in layers with buried interrupted absorbable suture for the deep dermal layer and a running subcuticular absorbable suture for the skin. A sterile dressing is applied, and the patient is placed in a sling. Postoperative radiographs are obtained to visualize the suture buttons abutting the cortex (Fig 7).
Fig 7.
Postoperative radiographs of the right shoulder of a baseball pitcher status after right latissimus tendon repair as shown in this case. Anteroposterior (A) and axillary lateral (B) views show 2 suture buttons appropriately placed and engaging the humeral cortex. (SB, suture button.)
Postoperative Rehabilitation
The patient is placed in a sling postoperatively. Passive range-of-motion exercises are initiated 2 weeks postoperatively followed by strengthening exercises at 8 weeks. For pitchers, a throwing program is initiated by 16 weeks and return to sport is permitted 6 months postoperatively.
Discussion
The majority of patients with latissimus tendon injuries are treated successfully nonoperatively and surgical repair is only considered in elite or professional overhead athletes. Given that latissimus tendon injuries are uncommon, the literature contains mostly case reports and small case series. There have been some case series of professional baseball players showing successful outcomes with high rates of return to sport with nonoperative treatment.6,7 However, the level of return to sport, effectiveness, and longevity of the professional athlete with this injury have been called into question after nonoperative treatment. Erickson et al.8 reported on the largest case series of 11 latissimus ruptures treated operatively, showing excellent outcomes with all patients able to return to sport to the same level of competition. Other studies of latissimus ruptures treated operatively are limited to much smaller case series or single case reports.9,10 Other fixation options for latissimus tendon injuries include suture anchor or transosseous tunnel fixation.11 Given the rarity of this injury, there have been no studies comparing the single- and dual-incision techniques or different fixation options. Advantages and disadvantages of our single-incision latissimus tendon repair technique are presented in Table 1 followed by pearls and pitfalls of the procedure in Table 2.
Table 1.
Advantages and Disadvantages of Latissimus Tendon Repair Through a Single-Incision Approach With Suture Button Fixation in the Lateral Decubitus Position
| Advantages |
|
| Disadvantages |
|
Table 2.
Pearls and Potential Pitfalls of Single-Incision Latissimus Tendon Repair With Suture Button Fixation in the Lateral Decubitus Position
| Pearls |
|
| Potential pitfalls |
|
Footnotes
The authors report the following potential conflict of interest or source of funding: C.S.A. reports grants and personal fees from Arthrex, grants from Major league Baseball, personal fees from At Peak, personal fees from Lead Player, and grants from Stryker, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video shows the technique of a latissimus tendon repair in a professional baseball pitcher in the lateral decubitus position utilizing a single incision posterior axillary incision with suture button fixation. The patient is positioned in the lateral decubitus position with the right upper extremity placed into a limb positioner (SPIDER2; Smith & Nephew, London, United Kingdom) in a way to maintain the humerus abducted and internally rotated. The skin is marked extending from the arm into the posterior chest wall along the posterior axillary fold. An 8- to 10-cm incision is made and taken down to the fascia. Self-retaining retractors are placed to tension the skin and subcutaneous tissues to aid in visualization and dissection. A mix of blunt and sharp dissection is used in between the triceps and the pectoralis major to identify the retracted latissimus dorsi tendon. A seroma cavity is often encountered when dissection is performed near the tendon stump. As dissection proceeds toward the humerus, care is taken to identify and preserve branches of the posterior brachial cutaneous nerve which are retracted posteriorly along with the triceps. Once the latissimus tendon is identified, a mixture of blunt and sharp dissection is used to mobilize the tendon from its proximal adhesions to allow for excursion back to its footprint onto the humerus. Two SutureTape sutures (Arthrex, Naples, FL) are then passed through the tendon in simple running locking Krackow fashion to create 4 limbs of suture. The tendon is then repeatedly tensioned to minimize creep. It is important to be aware of the proximity of the axillary nerve during this procedure which is expected to be just deep and proximal to the tendon in the floor of the exposure. The humerus is maximally internally rotated to expose the intertubercular groove. Any remaining soft tissue on the footprint is debrided and the bone is abraded with a curette. Once adequate exposure of the footprint is obtained, 2 unicortical drill holes are made with the appropriate drill size, one proximal and one distal about 1 to 2 cm apart, to accommodate passage of 2 suture buttons unicortically. The first set of SutureTape controlling the tendon is loaded onto a suture button in standard fashion according to the tension-slide technique with one limb entering proximally and exiting distally, and the other limb entering distally and exiting proximally. Using the button inserter, the loaded suture button is then placed through one of the unicortical drill holes and flipped to engage the cortex. The same sequence of events is repeated for the second suture button as it is loaded with the second set of SutureTape. It is essential to keep in mind that the latissimus tendon externally rotates 90° before inserting onto the humerus so the appropriate buttons are placed in the appropriate proximal or distal drill hole according to the orientation of the tendon as it would insert onto the footprint. Once the buttons are placed, flipped, and are engaging the cortex, one suture tail from each of the buttons is passed through the substance of the tendon from deep to superficial using a free needle. These limbs that are passed through the tendon allow for the knots to lay superficially on the tendon and will serve as the post strand for knot tying. The suture limbs from each SutureTape are sequentially tensioned to reduce the tendon back to its footprint. Both sets of suture are then tied using an arthroscopic knot pusher to facilitate knot tension deep in the wound. An arthroscopic cutter is then used to leave short tails. After irrigation, closure of the wound is performed in layers with buried interrupted absorbable suture for the deep dermal layer and a running subcuticular absorbable suture for the skin. A sterile dressing is applied and the patient is placed in a sling.
References
- 1.George M.S., Khazzam M. Latissimus dorsi tendon rupture. J Am Acad Orthop Surg. 2019;27:113–118. doi: 10.5435/JAAOS-D-17-00581. [DOI] [PubMed] [Google Scholar]
- 2.Donohue B.F., Lubitz M.G., Kremchek T.E. Sports injuries to the latissimus dorsi and teres major. Am J Sports Med. 2017;45 doi: 10.1177/0363546516676062. 2428-2335. [DOI] [PubMed] [Google Scholar]
- 3.Friedman M.V., Stensby J.D., Hillen T.J., Demertzis J.L., Keener J.D. Traumatic tear of the latissimus dorsi myotendinous junction: Case report of a crossfit-related injury. Sports Health. 2015;7:548–552. doi: 10.1177/1941738115595975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park J.Y., Lhee S.H., Keum J.S. Rupture of latissimus dorsi muscle in a tennis player. Orthopedics. 2008;31(10) [PubMed] [Google Scholar]
- 5.Erickson B.J., Ahmad C.S., Romeo A.A. Latissimus dorsi and teres major muscule injuries in pitchers. In: Ahmad C.S., Romeo A.A., editors. Baseball sports medicine. Wolters Kluwer; Philadelphia: 2019. pp. 231–244. [Google Scholar]
- 6.Schickendantz M.S., Kaar S.G., Meister K., Lund P., Beverley L. Latissimus dorsi and teres major tears in professional baseball pitchers: A case series. Am J Sports Med. 2009;37:2016–2020. doi: 10.1177/0363546509335198. [DOI] [PubMed] [Google Scholar]
- 7.Nagda S.H., Cohen S.B., Noonan T.J., Raasch W.G., Ciccotti M.G., Yocum L.A. Management and outcomes of latissimus dorsi and teres major injuries in professional baseball pitchers. Am J Sports Med. 2011;39:2181–2186. doi: 10.1177/0363546511422219. [DOI] [PubMed] [Google Scholar]
- 8.Erickson B.J., Chalmers P.N., Waterman B.R., Griffin J.W., Romeo A.A. Performance and return to sport in elite baseball players and recreational athletes following repair of the latissimus dorsi and teres major. J Shoulder Elbow Surg. 2017;26:1948–1954. doi: 10.1016/j.jse.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 9.Cox E.M., McKay S.D., Wolf B.R. Subacute repair of latissimus dorsi tendon avulsion in the recreational athlete: Two-year outcomes of 2 cases. J Shoulder Elbow Surg. 2010;19(6):e16–e19. doi: 10.1016/j.jse.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 10.Ellman M.B., Yanke A., Juhan T., Verma N.N., Nicholson G.P., Bush-Joseph C. Open repair of an acute latissimus tendon avulsion in a Major League Baseball pitcher. J Shoulder Elbow Surg. 2013;22:e19–e23. doi: 10.1016/j.jse.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 11.Lim J.K., Tilford M.E., Hamersly S.F., Sallay P.I. Surgical repair of an acute latissimus dorsi tendon avulsion using suture anchors through a single incision. Am J Sports Med. 2006;34:1351–1355. doi: 10.1177/0363546506286787. [DOI] [PubMed] [Google Scholar]
- 12.Mazzocca A.D., Burton K.J., Romeo A.A., Santangelo S., Adams D.A., Arciero R.A. Biomechanical evaluation of 4 techniques of distal biceps brachii tendon repair. Am J Sports Med. 2007;35:252–258. doi: 10.1177/0363546506294854. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video shows the technique of a latissimus tendon repair in a professional baseball pitcher in the lateral decubitus position utilizing a single incision posterior axillary incision with suture button fixation. The patient is positioned in the lateral decubitus position with the right upper extremity placed into a limb positioner (SPIDER2; Smith & Nephew, London, United Kingdom) in a way to maintain the humerus abducted and internally rotated. The skin is marked extending from the arm into the posterior chest wall along the posterior axillary fold. An 8- to 10-cm incision is made and taken down to the fascia. Self-retaining retractors are placed to tension the skin and subcutaneous tissues to aid in visualization and dissection. A mix of blunt and sharp dissection is used in between the triceps and the pectoralis major to identify the retracted latissimus dorsi tendon. A seroma cavity is often encountered when dissection is performed near the tendon stump. As dissection proceeds toward the humerus, care is taken to identify and preserve branches of the posterior brachial cutaneous nerve which are retracted posteriorly along with the triceps. Once the latissimus tendon is identified, a mixture of blunt and sharp dissection is used to mobilize the tendon from its proximal adhesions to allow for excursion back to its footprint onto the humerus. Two SutureTape sutures (Arthrex, Naples, FL) are then passed through the tendon in simple running locking Krackow fashion to create 4 limbs of suture. The tendon is then repeatedly tensioned to minimize creep. It is important to be aware of the proximity of the axillary nerve during this procedure which is expected to be just deep and proximal to the tendon in the floor of the exposure. The humerus is maximally internally rotated to expose the intertubercular groove. Any remaining soft tissue on the footprint is debrided and the bone is abraded with a curette. Once adequate exposure of the footprint is obtained, 2 unicortical drill holes are made with the appropriate drill size, one proximal and one distal about 1 to 2 cm apart, to accommodate passage of 2 suture buttons unicortically. The first set of SutureTape controlling the tendon is loaded onto a suture button in standard fashion according to the tension-slide technique with one limb entering proximally and exiting distally, and the other limb entering distally and exiting proximally. Using the button inserter, the loaded suture button is then placed through one of the unicortical drill holes and flipped to engage the cortex. The same sequence of events is repeated for the second suture button as it is loaded with the second set of SutureTape. It is essential to keep in mind that the latissimus tendon externally rotates 90° before inserting onto the humerus so the appropriate buttons are placed in the appropriate proximal or distal drill hole according to the orientation of the tendon as it would insert onto the footprint. Once the buttons are placed, flipped, and are engaging the cortex, one suture tail from each of the buttons is passed through the substance of the tendon from deep to superficial using a free needle. These limbs that are passed through the tendon allow for the knots to lay superficially on the tendon and will serve as the post strand for knot tying. The suture limbs from each SutureTape are sequentially tensioned to reduce the tendon back to its footprint. Both sets of suture are then tied using an arthroscopic knot pusher to facilitate knot tension deep in the wound. An arthroscopic cutter is then used to leave short tails. After irrigation, closure of the wound is performed in layers with buried interrupted absorbable suture for the deep dermal layer and a running subcuticular absorbable suture for the skin. A sterile dressing is applied and the patient is placed in a sling.