Abstract
Purpose
Previous studies have shown that thumb interphalangeal (IP) joint arthrodesis is typically performed between 0 and 30° of flexion, with a recent study in healthy subjects having recommended a range of 15–30° to be an ideal functional IP joint fusion angle for various activities of daily living. The current study aimed to evaluate the ideal thumb IP fusion angle in patients with thumb carpometacarpal (CMC) osteoarthritis (OA).
Methods
Twenty-seven patients with thumb CMC OA were evaluated; five patients had bilateral pathology, for a total of thirty-two thumbs included. Hand dominance was noted and baseline unsplinted measurements were obtained for power tasks, precision tasks, pinch, and grip strength testing. Patients’ thumbs were then splinted at 0, 15, 30, and 45° with repeat measurements taken and compared to baseline. Outcomes were measured by use of a 10-point Visual Analogue Scale, timing of tasks, and a dynamometer. Outcomes were analyzed by Wilcoxon sign ranked tests for each category of trials.
Results
For significant outcomes, the most favorable simulated thumb fusion angles were 15° in the dominant hand and 0°, 15° in the nondominant hand (precision tasks); the least favorable position was found to be 45° in the dominant hand (precision tasks, pinch strength). When combining all outcomes that both reached and approached significance, the most favorable position was found to be 15° and least favorable position, 45°.
Conclusions
In patients with thumb CMC OA, an IP fusion angle of 15° is preferable, while a fusion angle of 45° is to be avoided.
Type of study/level of evidence
Therapeutic Study, Level III.
Keywords: Carpometacarpal arthritis, Joint arthrodesis, Osteoarthritis, Thumb arthritis
1. Introduction
Osteoarthritis (OA) of the carpometacarpal (CMC) joint of the thumb is a highly prevalent disease process, affecting as many as 15% of adults over the age of 30 and occurring more commonly than OA of the interphalangeal (IP) or metacarpophalangeal (MCP) joint.1 Although OA of the CMC joint is vastly more prevalent than thumb IP OA, it has been previously shown that CMC OA is associated with an increased risk of thumb IP joint OA.2,3 There is also evidence that thumb CMC OA is an underdiagnosed problem, as presence of OA may not always lead to functional disability.3 The surgical mainstay for treatment of IP joint OA has traditionally been arthrodesis.1 While Carroll et al. classically described the ideal position for thumb IP joint fusion as 15°; other studies have described a range of 0–30° as the ideal range for fusion, which has become the typical range in current clinical practice.4, 5, 6, 7, 8
Two recent studies have addressed the issue of thumb IP joint fusion ranges. Yao et al., in an effort to tailor treatment to modern functional needs, found that splinting of the thumb IP joint at 10° and 30° did not impair the use of a smartphone or sending text messages.9 McGowan et al., in the precursor study to the current work, focused on evaluating thumb fusion angles through a wider variety of activities mimicking daily tasks. It was found that a fusion angle between 15° and 30° provided the highest patient satisfaction and function; if fusion is to be performed outside this range, the 0° position was recommended.10
The purpose of the current study was to conduct a similar exercise in patients with OA of the thumb CMC joint, as the previous study was conducted in healthy subjects without OA of the thumb CMC joint. Our hypothesis was that optimal thumb IP joint position for the tasks tested would be either 15° or 30° with the least favorable position of thumb IP flexion during task performance at 45°.
2. Methods
Patients were identified for inclusion during office visits for treatment of thumb CMC OA. Inclusion criteria were age greater than 18 years, established diagnosis of thumb Eaton/Littler Stage II or III CMC OA, and ability to read, write, and understand English. Patients were excluded if they did not meet the above criteria, had significant instability or hyperextension at the thumb metacarpophalangeal joint, as well as if they had undergone prior surgical management for thumb osteoarthritis. Suitability for inclusion of CMC OA radiographic stage was determined by the senior author (board certified, hand fellowship trained orthopaedic surgeon) at the time of enrollment. Patients with bilateral pathology underwent separate test procedures for each side. Therefore, a total of 27 patients with thumb CMC OA were included for examination; five patients had bilateral pathology, for a total of 32 thumbs included. The study group consisted of 9 males and 18 females, with an average age of 62.4 years (median 62 years).
Institutional Review Board approval was obtained and all patients underwent an approved informed consent process including consent in accordance with the Health Insurance Portability and Accountability Act (HIPAA) for collection of demographic information. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as approved by the institutional review committee. Guidelines as indicated by the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) initiative were adhered to in the preparation of the study findings.
Patients performed the following trials, designed to mimic daily activities: power tasks (opening/closing a tight jar, lifting a heavy glass, opening a door, pouring liquid from a gallon jug), precision tasks (zipping/unzipping a jacket, opening/closing a Velcro strip, writing, buttoning/unbuttoning a shirt, translating coins from hand to hand), and grip/pinch testing (Dynamometer, Lafayette Instruments, Lafayette, Indiana). Measurements were taken at baseline function, represented by activity measurements of the unsplinted affected thumb; hand dominance was documented. Patients with unilateral thumb CMC OA did not undergo testing of the contralateral hand.
Custom-made thumb orthoplast splints were then applied sequentially to the dorsum of the affected thumb, secured with Velcro straps, mimicking various angles of thumb IP fusion (0°, 15°, 30°, 45°). Accuracy of thumb angle was maximized by fitting patients with the proper size splint (small, medium, large) in an attempt to minimize thumb motion in splint during the trials. The splints were fashioned with the pad of the distal phalanx uncovered allowing easier performance of tasks. Measurements with splints applied were taken for each activity at each splinted thumb IP angle. These results were compared to the patient's baseline measurements for each activity. Outcomes for each task were recorded via use of a self-reported 10-point Visual Analogue Scale (VAS), where 0 indicated dissatisfaction/extreme difficulty with task and 10 indicated highest satisfaction/ease of task, timing of tasks, and dynamometer readings for grip and pinch strength. Time measurements for precision tasks were taken as the average of two measurements per task. Data was then analyzed by Wilcoxon sign ranked tests for each category of trials and grouped by hand dominance. As such, four matched ranks were analyzed for each trial in each activity (i.e. baseline-0°, baseline-15°, baseline-30°, baseline-45°) to evaluate for improvement or worsening of each outcome measure compared to baseline (VAS score, time to complete activity, grip/pinch strength). The mean and median values for all outcomes were also recorded. Unfortunately, due to an error in technique, grip/pinch strength data was not obtained for 8 patients with unilateral pathology (25% of thumbs). Significance was set at p < 0.05.
3. Results
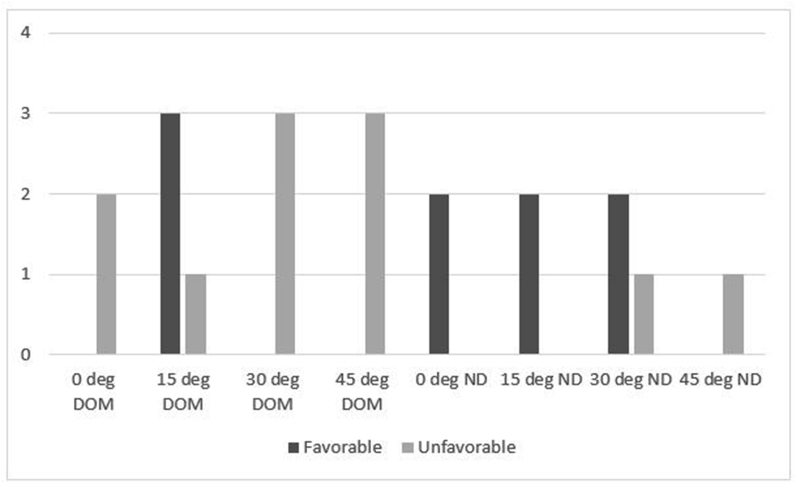
Of all trials conducted (10 functional activities, grip, pinch measurement at all splint angles), there were a total of 12 trials that resulted in a significant difference from baseline function (p < 0.05). These are highlighted in Table 1, Table 2, Table 3. Trials with a significant result are bolded and italicized in each table. For additional clarity, significant trials were summed based on whether the outcome represented an improvement or worsening from baseline function (Fig. 1). Notably, among these results, the splinted position of 15° at the thumb IP joint resulted in increased satisfaction with power task (opening jar) as well as increased satisfaction and faster performance time for precision task (Velcro). Conversely, the splinted position of 45° resulted in decreased pinch strength, and both decreased performance time and satisfaction with precision tasks (knot tying, coin translating). In general, for outcomes that reached significance, the most favorable thumb splinting angles were 15° in the dominant hand and 0°, 15° in the nondominant hand; the least favorable position was found to be 45° in the dominant hand.
Table 1.
Mean Grip/Pinch Strength by Thumb Position and Hand Dominance (Median, Range), all thumbs.
| Measurement | Grip Strength | Pinch Strength |
|---|---|---|
| Baseline ND | 23.9 | 11.8 |
| (16.5, 11–48) | (11, 5–19) | |
| 0° ND | 24.1 | 12.9 |
| (18, 12–42) | (12, 9–21) | |
| 15° ND | 23.1 | 12.7 |
| (17.5, 12–42) | (12.5, 6–22) | |
| 30° ND | 25.7 | 12.7 |
| (18.5, 10–53) | (11.5, 7–21) | |
| 45° ND | 25 | 12.9 |
| (18, 12–46) | (12.5, 7–21) | |
| Baseline Dom | 18.07 | 12.96 |
| (19.5, 8–26) | (13, 9–19) | |
| 0° Dom | 18.64 | 12.5 |
| (20, 8–28) | (12.5, 10–16) | |
| 15° Dom | 18.21 | 11.71 |
| (18.5, 8–28) | (12, 8–16) | |
| 30° Dom | 18.5 | 12.18 |
| (19.5, 8–30) | (12.5, 8–16) | |
| 45° Dom | 17.5 | 12.04 |
| (18.5, 9–28) | (12.25, 7–17) |
Bold/Italicized = statistically significant outcome (p < 0.05); ND = Nondominant, Dom = Dominant.
Table 2.
Time (seconds) for Precision Tasks by Thumb Position and Hand Dominance (Median, Range), all thumbs.
| Measurement | Zipper | Velcro | Knot | Writing | Buttons | Coins |
|---|---|---|---|---|---|---|
| Baseline ND | 10 | 10.6 | 10 | NT | 35.75 | 10.38 |
| (8.5, 5–17) | (10, 5–22) | (9, 6–22) | (35.5, 20–62) | (10, 6–15) | ||
| 0° ND | 9 | 10.87 | 9.75 | NT | 35.56 | 10.38 |
| (7.5, 5–16) | (10, 4–22) | (9, 6–18) | (33, 24–47) | (10, 7–14) | ||
| 15° ND | 9.33 | 11.07 | 9.69 | NT | 32.44 | 12.06 |
| (7.65, 5–21) | (9, 5–19) | (9.5, 7–13) | (32, 13–55) | (10, 6–36) | ||
| 30° ND | 8.19 | 11.13 | 10.44 | NT | 36.5 | 11.63 |
| (7.5, 5–12) | (9, 5–22) | (10, 7–17) | (38.5, 20–48) | (10.5, 7–19) | ||
| 45° ND | 8.84 | 12.83 | 10.06 | NT | 33.69 | 12.57 |
| (8, 6–18) | (13, 5–22) | (10, 8–14) | (32.5, 26–51) | (11.5, 9–19) | ||
| Baseline Dom | 10.13 | 12.13 | 9.31 | 20.79 | 37.56 | 12.38 |
| (9, 6–16) | (8.5, 5–30) | (9, 5–18) | (18, 13–45) | (30.5, 23–120) | (12, 6–20) | |
| 0° Dom | 9.88 | 11.63 | 12.13 | 20.5 | 40.13 | 12.19 |
| (8, 6–27) | (8.5, 4–30) | (9.5, 5–28) | (19.5, 13–43) | (30, 22–130) | (10, 6–30) | |
| 15° Dom | 9.56 | 9.63 | 9.44 | 21 | 32.13 | 13.06 |
| (9, 5–17) | (6.5, 4–27) | (9, 5–16) | (19, 15–50) | (29, 23–55) | (10.5, 6–36) | |
| 30° Dom | 11.13 | 13.44 | 10.56 | 20.57 | 38.63 | 13.25 |
| (9.5, 6–32) | (8, 4–50) | (9.5, 6–26) | (18, 13–50) | (28, 22–140) | (12, 7–32) | |
| 45° Dom | 9.88 | 11.38 | 11.56 | 19.57 | 37.94 | 14.2 |
| (9, 5–20) | (8, 3–40) | (11, 5–20) | (18, 12–35) | (30, 24–130) | (10, 7–36) |
Bold/Italicized = statistically significant outcome (p < 0.05); ND = Nondominant, Dom = Dominant; NT = Not tested.
Table 3.
Visual Analogue Scores for Ease of Task Completion by Thumb Position and Hand Dominance (Median, Range), all thumbs.
| Measure | Open Jar | Lift Glass | Door | Pour | Zipper | Velcro | Knot | Writing | Buttons | Coins |
|---|---|---|---|---|---|---|---|---|---|---|
| Base ND | 8.85 | 9.11 | 6.24 | 7.97 | 8.9 | 7.59 | 8.04 | NT | 7.74 | 8.48 |
| (10, 4.6–10) | (9.9, 1.6–10) | (7.1, 0.1–10) | (9.9, 2.3–10) | (9.9, 3.7–10) | (9.8, 0.1–10) | (9.9, 2.7–10) | (8.3, 2.1–10) | (9.9, 2.5–10) | ||
| 0° ND | 8.92 | 9.33 | 6.13 | 8.11 | 8.78 | 8.83 | 8.21 | NT | 7.71 | 8.29 |
| (10, 2.6–10) | (10, 4.2–10) | (0.1–10) | (9.8, 0.1–10) | (10, 3.2–10) | (10, 0.1-10) | (9.9, 3–10) | (8.4, 3.9–10) | (9.7, 4–10) | ||
| 15° ND | 9.11 | 9.26 | 6.93 | 8.65 | 8.82 | 8.25 | 8.52 | NT | 8.45 | 8.34 |
| (10, 3.3–10) | (10, 4.2–10) | (0.1–10) | (9.95, 1.5–10) | (9.9, 3–10) | (10, 0.1-10) | (9.4, 4.2–10) | (9.9, 2.6–10) | (10, 3.6–10) | ||
| 30° ND | 9.22 | 9.29 | 7.14 | 8.89 | 9.31 | 8.68 | 6.54 | NT | 6.23 | 7.25 |
| (10, 3.5–10) | (10, 2–10) | (0.1–10) | (10, 0.9–10) | (10, 1.7–10) | (10, 0.1–10) | (5.1, 1.5–10) | (6.1, 1.6-10) | (7.7, 1–10) | ||
| 45° ND | 9.07 | 8.96 | 5.95 | 8.1 | 7.89 | 8.04 | 7.24 | NT | 7.02 | 7.06 |
| (9.9, 2.3–10) | (9.9, 2.1–10) | (0.1–10) | (9.9, 2.4–10) | (8.8, 1.4–10) | (9.8, 0.1–10) | (7.6, 0.5–10) | (7.4, 0.2–10) | (7.5, 1.3–10) | ||
| Base Dom | 8.83 | 9.58 | 6.66 | 8.83 | 9.09 | 9.02 | 8.01 | 8.53 | 8.43 | 9.26 |
| (10, 2.4–10) | (10, 5–10) | (7.3, 0.1–10) | (9.9, 2.5–10) | (9.7, 7.3–10) | (9.9, 3.8–10) | (8.8, 3.5–10) | (9.9, 5–10) | (9.9, 5–10) | (9.9, 7.4–10) | |
| 0° Dom | 9.11 | 9.52 | 6.6 | 9.01 | 9.46 | 9.33 | 7.44 | 7.93 | 8.68 | 8.89 |
| (9.9, 1.7–10) | (10, 6.9–10) | (5.4, 0.1–10) | (10, 5–10) | (9.9, 5.1–10) | (10, 3.9–10) | (7.5, 1.6–10) | (8.1, 2.3–10) | (10, 4.4–10) | (9.9, 4.9–10) | |
| 15° Dom | 9.86 | 9.44 | 7.17 | 8.71 | 9.44 | 9.53 | 7.95 | 8.98 | 8.99 | 8.58 |
| (10, 8.4-10) | (10, 5–10) | (7.5, 0.1–10) | (9.9, 4.4–10) | (10, 5–10) | (10, 5.1–10) | (8.5, 5–10) | (9.9, 5–10) | (10, 5–10) | (9.7, 4–10) | |
| 30° Dom | 9.11 | 9.19 | 6.73 | 8.73 | 8.93 | 8.94 | 6.99 | 8.85 | 7.46 | 7.39 |
| (10, 5–10) | (10, 5–10) | (6.8, 0.2–10) | (10, 4.9–10) | (9.9, 5–10) | (10, 4.9–10) | (7.2, 3.4–10) | (10, 5–10) | (7.2, 3.7–10) | (6.7, 3.9-10) | |
| 45° Dom | 9.04 | 9.44 | 5.81 | 8.65 | 9.11 | 9.59 | 6.59 | 8.91 | 7.76 | 6.97 |
| (10, 2.5–10) | (10, 5.1–10) | (5, 0.1–10) | (10, 3.9–10) | (9.9, 5–10) | (10, 7.5–10) | (5.7, 2.5–10) | (19, 3.3–10) | (9, 3.4–10) | (7.6, 0.1-10) |
Bold/Italicized = statistically significant outcome (p < 0.05); ND = Nondominant, Dom = Dominant; NT = Not tested.
Fig. 1.
Number of Favorable/Unfavorable Outcomes (statistically significant outcomes only) by Thumb Angle and Hand Dominance.
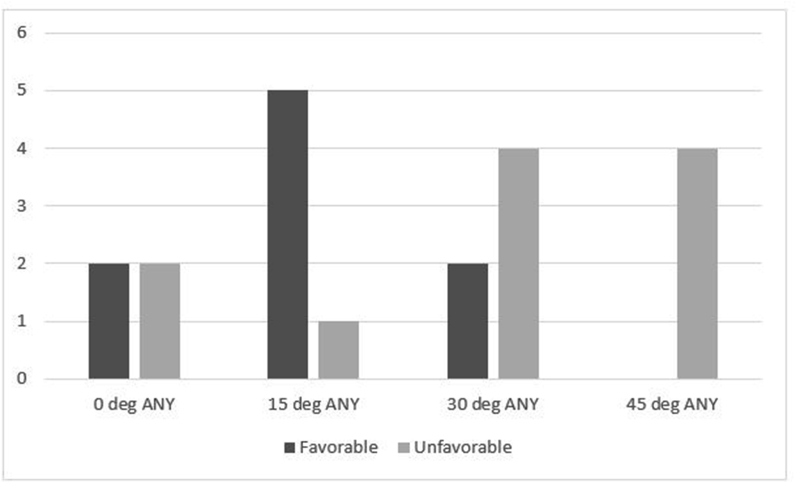
Given the small sample size of the subjects tested, trials that approached significance were also examined. There were 8 such trials that are detailed in Table 4. Inclusion of these results with those that attained significance are represented in Fig. 2. A summation of all trials that met or approached significance according to type of outcome is shown in Fig. 3. These combined results show that for all positions of the thumb IP joint and hand dominance across all trials, the most preferable angle was found to be 15°; the least preferable angle for thumb IP positioning was found to be 45°.
Table 4.
Trial outcomes that approached statistical significance.
| Splint Angle, Dominance | Outcome (Baseline; Trial Value) | p-value Favorable/Unfavorable |
|---|---|---|
| 0°, ND | VAS, lift glass | p = 0.062 |
| (9.1, 9.3) | Favorable | |
| 0°, DOM | VAS, knot tying | p = 0.08 |
| (8, 7.4) | Unfavorable | |
| 15°, DOM | VAS, zipper | p = 0.057 |
| (8.9, 9.4) | Favorable | |
| 15°, ND | VAS, buttons | p = 0.053 |
| (7.7, 8.5) | Favorable | |
| 30°, ND | Time, zipper | p = 0.072 |
| (10s, 8.2s) | Favorable | |
| 30°, ND | VAS, open door | p = 0.062 |
| (6.2, 7.1) | Favorable | |
| 30°, Dom | VAS, knot tying | p = 0.059 |
| (8, 6.54) | Unfavorable | |
| 30°, Dom | VAS, buttons | p = 0.077 |
| (8.4, 7.5) | Unfavorable |
ND = Nondominant, Dom = Dominant.
Fig. 2.
Number of Favorable/Unfavorable Outcomes (all outcomes approaching significance) by Thumb Angle and Hand Dominance.
Fig. 3.
Number of Favorable/Unfavorable Outcomes (all outcomes approaching significance) by Thumb Angle for All Trials.
4. Discussion
Arthrodesis of the IP joint of the thumb is a mainstay of surgical treatment for the painful arthritic joint that is refractory to non-operative management. The most common indications for arthrodesis include osteoarthritis, inflammatory and posttraumatic arthritis, as well as fixed contractures or instability secondary to tendon or ligament injury.6 Recent studies have revealed mechanical stresses to be a contributing factor to thumb IP joint OA and obesity to be a contributor to the development of thumb CMC OA.1,3,6 Although OA of the CMC joint is far and away more prevalent of a disease process, it is associated with an increased risk of thumb IP joint OA.2,3
Multiple previous authors have addressed the ideal angle for thumb IP joint arthrodesis. The traditionally described ideal position for thumb IP joint fusion was 15°, whereas other studies have described a range of 0–30° as the ideal range for fusion.4, 5, 6, 7, 8 Sieber et al. further recommended that angle of fusion be adapted to professional requirements. Their group stated that the ideal range of fusion for occupations requiring instrument or power grip be fused at 5–10° and those requiring significant precision grip be fused at 20–30°.8 Jemec et al. investigated the effect of pronation at the IP joint and found that increased pronation occurs during power grip and manual work, whereas fine dexterous work required less pronation of the IP joint. Although it was recommended that pronation be incorporated into IP joint arthrodesis according to the patient's functional demands, there is currently limited clinical outcome data to support this practice.11 Degree of thumb IP joint pronation was not addressed as part of the current study, however.
Recent studies have attempted to hone in on the ideal IP fusion angle to best accommodate the needs of a patient participating in a wide variety of activities. Yao et al. considered the needs of the 21st century patient who often requires use of a smartphone and text communication. They found that splinting of the thumb IP joint at 10° and 30° did not impair the use of a smartphone or sending text messages.9 This study did add a valuable data point to the established literature, but did not examine activities beyond phone usage. The precursor study to the current work by McGowan et al. (2016) recommended a thumb IP fusion angle between 15° and 30° to optimize patient satisfaction and function across a wide range of daily activities, with the suggestion to fuse at 0° and avoid 45° if fusing outside that range.10 However, the previous study was performed in healthy volunteers with no known degenerative changes of the thumb joints. The objective of the current study was to build upon these findings and evaluate simulated thumb IP fusion angles in patients with known thumb CMC OA.
When looking purely at the results of the current study that attained significance, the simulated fusion angle of 15° unequivocally provided the highest patient satisfaction and functionality, whereas the simulated fusion angle of 45° caused the most dissatisfaction and limited functionality. When results were expanded to include averages of outcomes that approached significance as well, the findings were unchanged, with both favorable and unfavorable trials seen at simulated fusion angles of 0° and 30°. In terms of hand dominance, the most favorable angles were 15° in the dominant hand and 0°, 15° in the nondominant hand (for precision tasks). Interestingly, throughout all trials, there were no favorable outcomes for the thumb splinted at 45°. The primary recommendation of the current study to fuse the thumb IP joint at 15° to provide the widest range of functionality and satisfaction indeed does not fall outside of the fusion angle recommended by multiple prior authors.4,6,10 The findings of the current study that splinting of the thumb IP joint decreases pinch strength at 15° and 45° in the dominant hand (see Table 1), however, are contradictory to the findings of Goetz et al. (2012) where static splinting of the thumb did not have any effect on pinch strength.12
There were various strengths and weaknesses to the current study. Strengths include the fact that human subjects with thumb CMC OA were evaluated, which allows more applicable findings to this large population, than a study involving healthy volunteers. The study benefits from the fact that it is not retrospective in nature, thus eliminating a source of potential bias. Another strength is the wide variety of the activities tested, thereby presenting scenarios that closely mimic daily activities.
In terms of weaknesses, the study may have benefited from examination of a larger number of patients; results approaching statistical significance may have reached significance with a larger sample size. Another limitation was lacking grip and pinch data on 8 patients, which may have affected outcomes in an unknown way. One drawback to enrolling patients with degenerative pathology is that pain experienced throughout the testing period may have manifested in impaired function while splinted at 45°, possibly skewing data into worse outcomes, as this angle was tested last in the series. This may have been avoided by randomizing the order of tasks at different degrees of IP joint splinting. There are also limitations inherent to the model of using thermoplast splints to simulate joint arthrodesis. As pointed out by Domalain et al. (2011), there may be up to 4° of mobility at the time of digit contact with use of splints; similarly, a surgically fused joint may be somewhat shortened, thereby altering the digit mechanics in vivo.13 Although this may have implications in applicability of the results to clinical practice, it likely did not affect the results of the current study, as all subjects used the same set of orthoplast splints. The current study attempted to minimize this variability by utilizing multiple splint sizes accordingly to patient thumb size.
Taking into account the above factors, findings of the established literature, and the results of the current study, the authors therefore recommend a thumb IP joint fusion angle of 15° for the vast majority of patients to provide the highest level of functionality throughout a wide range of daily activities. Should a patient's occupation or clinical picture require fusion outside this range, angles of 0° and 30° also provide acceptable levels of functionality. The angle of 45° should be avoided if at all possible. Future studies that prospectively evaluate clinical outcome data in patients that have undergone thumb IP joint fusion would be a valuable addition to the literature.
Statement of funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The author(s) declare the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: author KM has received consulting fees from DePuy Synthes and Integra Life Sciences.
References
- 1.Berger A.J., Meals R.A. Management of osteoarthrosis of the thumb joints. J Hand Surg Am. 2015;40(4):843–850. doi: 10.1016/j.jhsa.2014.11.026. [DOI] [PubMed] [Google Scholar]
- 2.Chaisson C.E., Zhang Y., McAlindon T.E. Radiographic hand osteoarthritis: incidence, patterns, and influence of pre-existing disease in a population based sample. J Rheumatol. 1997;24(7):1337–1343. [PubMed] [Google Scholar]
- 3.Haara M.M., Heliövaara M., Kröger H. Osteoarthritis in the carpometacarpal joint of the thumb. Prevalence and associations with disability and mortality. J Bone Jt Surg Am. 2004;86-A(7):1452–1457. doi: 10.2106/00004623-200407000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Carroll R.E., Hill N.A. Small joint arthrodesis in hand reconstruction. J Bone Jt Surg Am. 1969;51(6):1219–1221. [PubMed] [Google Scholar]
- 5.Ferlic D.C., Turner B.D., Clayton M.L. Compression arthrodesis of the thumb. J Hand Surg Am. 1983;8(2):207–210. doi: 10.1016/s0363-5023(83)80019-7. [DOI] [PubMed] [Google Scholar]
- 6.Rizzo M. Thumb arthrodesis. Tech Hand Up Extrem Surg. 2006;10(1):43–46. doi: 10.1097/00130911-200603000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Shin E.K., Osterman A.L. Treatment of thumb metacarpophalangeal and interphalangeal joint arthritis. Hand Clin. 2008;24(3):239–250. doi: 10.1016/j.hcl.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 8.Sieber H.P., Segmuller G. [Arthrodesis of the interphalangeal joint of the thumb: indication, technic, results] Handchir Mikrochir Plast Chir. 1983;15(1):11–16. [PubMed] [Google Scholar]
- 9.Yao J., Park M.J., Davis D., Chang J. Ideal position for thumb interphalangeal arthrodesis in the era of smartphones and text communication. Orthopedics. 2012;35(11):955–957. doi: 10.3928/01477447-20121023-07. [DOI] [PubMed] [Google Scholar]
- 10.McGowan S.M., Deisher M., Matullo K.S. Functional fusion angle for thumb interphalangeal joint arthrodesis. Hand (N Y) 2016;11(1):59–64. doi: 10.1177/1558944715614858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jemec B., Verjee L.S., Jain A., Sandford F. Rotation in the interphalangeal thumb joint in vivo. J Hand Surg Am. 2010;35(3):425–429. doi: 10.1016/j.jhsa.2009.11.019. [DOI] [PubMed] [Google Scholar]
- 12.Goetz T.J., Costa J.A., Slobogean G., Patel S., Mulpuri K., Travlos A. Contribution of flexor pollicis longus to pinch strength: an in vivo study. J Hand Surg Am. 2012;37(11):2304–2309. doi: 10.1016/j.jhsa.2012.07.027. [DOI] [PubMed] [Google Scholar]
- 13.Domalain M., Evans P.J., Seitz W.H., Jr., Li Z.M. Influence of index finger proximal interphalangeal joint arthrodesis on precision pinch kinematics. J Hand Surg Am. 2011;36(12):1944–1949. doi: 10.1016/j.jhsa.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]