Abstract
Background
External ventricular drainage (EVD) is a standard approach for both monitoring intracranial pressure (ICP) and draining cerebrospinal fluid (CSF) for patients with subarachnoid hemorrhage (SAH). Documenting an accurate ICP value is important to assess the status of the brain, which would require the EVD system to be leveled properly and closed to CSF drainage for an adequate period of time. It is suggested that a minimum period of 5-min EVD closure is needed before documenting a true ICP, however, there is no commonly agreed upon standard for documenting ICP. To obtain an insight into how well the intermittent EVD clamping procedure is performed for ICP documentation, we conducted a retrospective analysis of ICP recordings obtained through EVD from 107 SAH patients.
Methods
The EVD was kept open for continuous CSF drainage, and then intermittently closed for ICP documentation. For each EVD closure, mean ICP, standard deviation of ICP, duration of EVD closure, time interval between two adjacent EVD closures were studied. The total number of EVD closures was calculated for each patient. We developed an algorithm to evaluate whether ICP reached a new equilibrium before the EVD was re-opened to drainage. The percentage of EVD closures that reach the equilibrium was calculated.
Results
The 107 patients had 32,755 EVD closures in total, among which 65.9% instances lasted less than 1 minute and only 16.3% of all the EVD closure episodes lasted longer than 5 minutes. The median duration of each EVD closure was 25 sec [IQR, 10.2 sec - 2.33 min]. Only 22.9% of the EVD closures reached ICP equilibrium before EVD re-opening.
Conclusion
A standard guideline and proper training are needed for bedside nurses, and a potential tool that can render ICP trend at a proper scale at bedside would help clinicians correctly document ICP.
Keywords: External Ventricular Drain, Intracranial Pressure, Subarachnoid Hemorrhage
Introduction
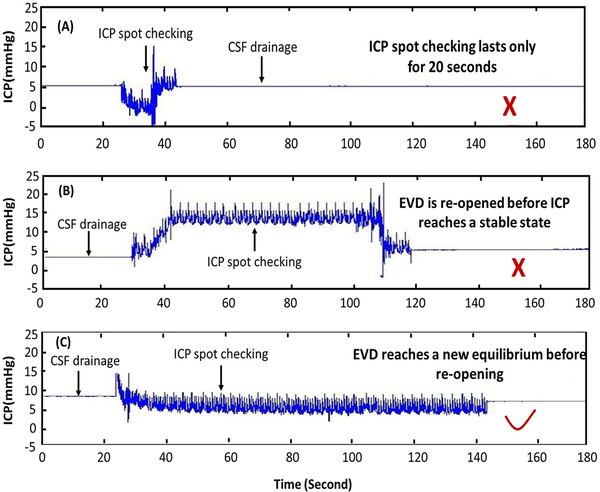
Intracranial pressure (ICP) monitoring can provide a necessary value for the quantification of cerebral perfusion pressure (CPP) and is a common practice to prevent secondary brain injury (e.g. cerebral ischemia). 1–8 Insertion of an external ventricular drain (EVD) is one of the most common lifesaving procedures in neurosurgery for subarachnoid hemorrhage (SAH) patients,9–11 which mainly includes two different methods of cerebral spinal fluid (CSF) drainage and ICP monitoring. The first method is continuous ICP monitoring with intermittent CSF drainage once ICP exceeds a certain threshold (monitor-first protocol); and the second method is continuous CSF drainage with intermittent clamping of ICP (drain-first protocol).10 Choosing one method over the other depends on the patient’s pathology, institutional policy and/or physicians’ and advanced practice providers’ preference. 12–18 Documenting an accurate ICP value is important to assess the healthy status of the brain, which would require the EVD system to be leveled properly and closed to CSF drainage for an adequate period of time. Most hospitals requires the bedside nurses/clinicians to enter the ICP value into the electronic medical records system manually every hour, or even more frequently in situations of suspected ICP elevation.19–21 This clinical practice still faces great challenges, 22 and recent studies has revealed wide practice variations associated with monitoring, treating and documenting ICP values (Supplementary Digital Content 1).14,23–25 As suggested by Rogers and his colleagues,11 it is not appropriate if we document the ICP value immediately after clamping EVD, as ICP dynamics have inherent hysteresis and require a certain amount of time to reach a new equilibrium after closing the system to CSF drainage. Illustrative examples of this situation can be seen in Fig.1. Rogers suggested that a minimum period of 5-min monitoring is required before documenting the ICP value in order to reflect true ICP.11
Figure.1.
Examples of ICP traces recorded by EVD for SAH patient. (A) ICP spot checking lasting only 20 seconds; (B) ICP spot checking with EVD re-opened before ICP reached an equilibrium; (C) ICP spot checking that allows ICP reach a new equilibrium. EVD: external ventricular drain; ICP: intracranial pressure; SAH: subarachnoid hemorrhage; CSF: cerebral spinal fluid.
The primary objective of this study is to analyze high resolution continuous ICP signals from a cohort of aneurysmal subarachnoid hemorrhage patients to determine the statistics of ICP recordings that are appropriate for accurate measurement of mean ICP. aSAH cohort is chosen because drain-first protocol of ICP monitoring is a prevailing practice for these patients. Recordings of continuous ICP signals provide an excellent opportunity to determine the episodes of EVD closure and open in an automated fashion and to check a prerequisite for accurate ICP measurement, i.e., whether ICP reaches a new equilibrium after EVD closure.
Methods and Materials
Data from 107 SAH patients admitted to the neurological intensive care unit (ICU) at the University of California, San Francisco (UCSF) Medical Center (California, USA) between February, 2013 and December, 2016 were analyzed. Eligible patients were SAH patients with a clinical need for ICP monitoring via EVD (into lateral ventricles). The study was approved by the local institutional review board (IRB). Informed consent was waived because of the retrospective nature of the study. Patients were managed according to the established national SAH guidelines (Supplementary Digital Content 2).12,26 The ICU protocol is to maintain an ICP < 20 mm Hg and cerebral perfusion pressure (CPP) > 70 mm Hg using both medical and surgical management. Once the patient neurologically improved with CSF diversion and had a normal ICP, the EVD weaning protocol was instituted to determine whether external CSF diversion was necessary. A CSF shunt was placed into the brain for patients whose EVD weaning test failed.
Data acquisition
ICP was monitored through EVD (LimiTorr 20 or 30 mL, Integra, New Jersey, USA) which is a closed sterile system allowing for drainage of CSF via a catheter tip that rests in the anterior horn of a lateral ventricle. The nurses followed the continuous CSF drainage with intermittent EVD clamping protocol (EVD Management General, Nursing Procedures Manual, UCSF Medical Center, Department of Nursing), which requires documenting ICP values at least once every two hours (Supplementary Digital Content 2). The protocol requires a minimum of 5 minutes before observing the waveform and documenting ICP values. All the signals were obtained using BedMaster™ system (Excel Medical, Florida, USA) at a sampling rate of 240 Hz.
Drainage-First Protocol
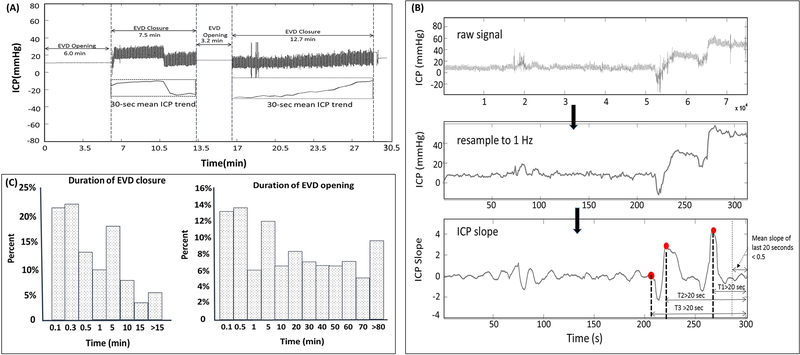
The data were collected during patients’ entire stay in the hospital and each patient had multiple clamping procedures for ICP documentation. Each recording session includes an EVD closure episode, during which intermittent ICP assessment is performed, and a CSF drainage episode, during which the EVD is open for CSF drainage (Fig 2A). For each EVD closure episode, the following were examined: 1) mean and standard deviation (SD) of ICP, 2) duration of the EVD closure, 3) time interval between two adjacent EVD closures, and 4) histogram of mean ICP. The total number of EVD closure episodes for each patient was calculated.
Figure 2.
(A) An example of EVD closure and EVD opening. The two lines in the squares are the 30-sec mean trend of ICP. EVD: external ventricular drain; ICP: intracranial pressure. (B) Data processing to determine whether ICP researched an equilibrium before EVD-reopening. (A) Raw ICP data at sampling frequency of 240 Hz; (B) Resampled ICP at 1 Hz. (C) ICP is considered to reach new equilibrium by fulfilling all of the three criteria below: i) the length of the EVD closure > 1 minute; ii) the mean absolute ICP slopes in the last 20 seconds before EVD re-opening < 0.5 mmHg/sec; iii) the top 3 greatest absolute slope changes occurred 20 seconds before re-opening EVD. (C) Left: Histogram of time duration of EVD closures for 107 SAH patients; Right: Histogram of time duration of EVD opening episodes for all the patients. EVD: external ventricular drain; SAH: subarachnoid hemorrhage.
ICP equilibrium determination
We developed an algorithm to determine whether ICP reached a new equilibrium before re-opening the EVD. The original ICP signal was resampled to 1 Hz, and a robust linear regression with a 10-second moving window was applied to each EVD closure episode. The ICP is considered to reach a new equilibrium by fulfilling all three criteria below (Fig 2B): 1. the length of the EVD closure is longer than one minute; 2. the mean absolute ICP slopes in the last 20 seconds before EVD re-opening is smaller than 0.5 mmHg/sec; 3. the top three greatest absolute slope changes occurred 20 seconds before re-opening EVD.
SPSS software (version 21, IBM, Armonk, NK, USA) was used for histogram graph creation. The histogram graph of duration of EVD closure and the duration of EVD opening was created.
Results
The mean age of this cohort was 59.7± 13.3 (mean ± SD) years old, ranging from 29 to 85 years old. 25% were male. Mean ICP during EVD clamping was 6.43 ± 8.65 mmHg (mean ± SD). 30.8% of the EVD weaning tests failed.
The 107 patients had 32,755 EVD closure episodes in total, among which 21,593 episodes (65.9%) lasted less than 1 minute. The median duration of each EVD closure episode was 0.42 [IQR, 0.17– 2.33] minutes, ranging from 0.08 minutes to 840 minutes (Supplementary SFig.4A). The median monitoring duration of each EVD drainage episode (EVD opening) was 9.42 [IQR, 0.5–43.9] min, ranging from 0.08 to 1494 min (Fig 2C). 16.3% of all the EVD closure episodes lasted longer than 5 minutes and 65.9% of intermittent closures were less than 1 minute. Only 7,491 of 32,755 (22.9%) EVD closure episodes meet our criteria of ICP equilibration before re-opening EVD.
Discussion
The data analyzed in this manuscript were from a cohort of SAH patients who need EVD during their stay in hospital. Despite advances in medical and surgical management, SAH remains a major cause of premature mortality, accounting for 27% of all stroke-related years of potential life lost before age 65.28,29 Continuous and accurate monitoring of ICP aids in the early detection of secondary cerebral insults for SAH patients. Increased ICP and a resultant decrease in cerebral perfusion play a major role in inducing ischemic brain tissue.
EVD Assessment in Intensive Care Unit
In ICU, it is the nurses’ responsibility to observe, adjudicate and document ICP, that requires skill and training in order to ensure documenting the correct value of ICP.11,12 Acquiring accurate ICP values via EVD is critically important, as ICP values may be underestimated or overestimated due to improper operation. Incomplete understanding of CSF physiology and pathophysiology during use of an EVD can contribute to variations in clinical practice and place patients at risk for untoward complications. There are still great challenges with ICP monitoring and documenting. For patients with continuous CSF drainage, the EVD needs to be intermittently clamped to assess the ICP value. Due to the hysteretic nature of ICP dynamics, the nurse needs to wait for a certain time for ICP equilibrium before documenting the value. However, there is no standard about the optimal period for which an EVD should be closed to obtain an accurate ICP value. Rogers suggested a minimum wait-time of five minute. They showed that the probability of observing the maximum ICP within the first three minutes would be 0.0124 and within 5 minutes was 0.0181.11 In the current study, we retrospectively reviewed ICP recordings from 107 SAH patients and separated the episodes associated with EVD opening to drain CSF fluid and EVD closing for intermittent ICP assessment. We found that only 16.3% of all the EVD closure episodes lasted longer than five minutes and 65.9% of intermittent closures were less than one minute. The result is crucial and it raises great concerns about current practice of clamping EVD to measure ICP and obtain accurate readings. A standard guideline and proper training to nurses is needed for ICP intermittent checking.
This study has the potential for a broad interest. For the first time, we summarize the time length of each EVD closure at bedside and we defined a way to check whether ICP reaches an equilibrium. To empower bedside clinicians to more effectively and accurately appreciate equilibrium, trends, and more complex temporal patterns in the monitored physiological variables, further innovations are needed because the existing bedside patient monitors provide poor support of this critical needs of the clinicians. For example, it would be of great help, if we can have a bedside multi-modality display to show the vital signals (e.g. ABP, ICP, temperature, PbtO2) at a proper time scale to facilitate the recognition of these long-term changes of physiological variables in addition to the default display of fast-moving waveforms and numerical values of vital signs. Such a tool will not only help achieve an accurate documentations of vital signals, it will also help clinicians to glance at the changes of these signals to assess the health status and evaluate the effectiveness of clinical interventions. This hypothesis warrants further studies in the future.
Limitations
The criteria and algorithm used to determine whether an ICP reached a new equilibration before EVD re-opening was empirically developed, as no commonly accepted criteria exist. Other methods and suggestions should be tested and compared with the current definition. In addition, we did not apply the algorithm to determine whether any recordings under one minute would have reached an equilibrium. Therefore, we may have underestimated the percentage of ICP recordings that might be appropriate for measuring ICP.
Conclusion
This study provides us insight into current practice of documenting ICP via EVD for SAH patients and it shows that leaving a drain clamped for a new equilibration before EVD re-opening can help identify whether the patient truly has high ICP or the high ICP value is dependent on CSF drainage. A standard guideline and proper training are needed for bedside nurses, and a potential tool that can render ICP trend at a proper temporal scale at bedside would help clinicians better recognize whether ICP dynamic system reaches equilibrium after EVD closure, thus allowing them to accurately measure ICP.
Supplementary Material
Supplemental Digital Content 2. Flow diagram depicting the decision-making process of the neurological intensive care team with regard to ICP monitoring in patients with SAH. EVD: external ventricular drain; ICP: intracranial pressure.
Acknowledgments
Conflicts of Interest and Source of Funding
Prof Xiao Hu has received Middle Career Scientist Award from UCSF Institute for Computational Health Sciences, and National Institutes of Health Award (R01NS089771A1). For the remaining authors none were declared.
References
- 1.Rangel-Castillo L, Robertson CS. Management of Intracranial Hypertension. Crit Care Clin. 2006;22(4):713–732. doi: 10.1016/j.ccc.2006.06.003 [DOI] [PubMed] [Google Scholar]
- 2.Czosnyka Z, Czosnyka M. Long-term monitoring of intracranial pressure in normal pressure hydrocephalus and other CSF disorders. Acta Neurochir (Wien). 2017;159(10):1979–1980. doi: 10.1007/s00701-017-3282-1 [DOI] [PubMed] [Google Scholar]
- 3.Chari A, Dasgupta D, Smedley A, et al. Intraparenchymal intracranial pressure monitoring for hydrocephalus and cerebrospinal fluid disorders. Acta Neurochir (Wien). 2017;159(10):1967–1978. doi: 10.1007/s00701-017-3281-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rahmanian A, Haghnegahdar A, Rahmanian A, Ghaffarpasand F. Effects of Intracranial Pressure Monitoring on Outcome of Patients with Severe Traumatic Brain Injury; Results of a Historical Cohort Study. Bull Emerg trauma 2014;2(4):151–155. [PMC free article] [PubMed] [Google Scholar]
- 5.Mak CHKC Lu YYY, Wong GKCG. Review and recommendations on management of refractory raised intracranial pressure in aneurysmal subarachnoid hemorrhage. Vasc Heal risk …. 2013;9:353–359. doi: 10.2147/VHRM.S34046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mak CHK, Lu YY, Wong GKC. Review and recommendations on management of refractory raised intracranial pressure in aneurysmal subarachnoid hemorrhage TL - 9. Rev Recomm Manag Refract Rais intracranial Press aneurysmal subarachnoid hemorrhage. 2013;9 VN-re(1) http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed15&AN=369395120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. VI. Indications for intracranial pressure monitoring. J Neurotrauma. 2007;24 Suppl 1(212):S37–S44. doi: 10.1089/neu.2007.9990 [DOI] [PubMed] [Google Scholar]
- 8.Dey M, Jaffe J, Stadnik A, Awad IA. External ventricular drainage for intraventricular hemorrhage. Curr Neurol Neurosci Rep. 2012;12(1):24–33. doi: 10.1007/s11910-011-0231-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Slazinski T, Anderson TA, Cattell E, Al E. Care of the patient undergoing intracranial pressure monitoring/external ventricular drainage or lumbar drainage. Am Assoc Neurosci Nurses 2011:1–3. [Google Scholar]
- 10.Kim GS, Amato A, James ML, et al. Continuous and intermittent CSF diversion after subarachnoid hemorrhage: A pilot study. Neurocrit Care. 2011. doi: 10.1007/s12028-010-9401-y [DOI] [PubMed] [Google Scholar]
- 11.Rogers M, Stutzman SE, Atem FD, Sengupta S, Welch B, Olson DM. Intracranial Pressure Values Are Highly Variable after Cerebral Spinal Fluid Drainage. J Neurosci Nurs. 2017. doi: 10.1097/JNN.0000000000000257 [DOI] [PubMed] [Google Scholar]
- 12.Muralidharan R External ventricular drains: Management and complications. Surg Neurol Int. 2015;6(7):271. doi: 10.4103/2152-7806.157620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Helbok R, Olson DW, Le Roux P, et al. Intracranial Pressure and Cerebral Perfusion Pressure Monitoring in Non-TBI Patients: Special Considerations. Neurocrit Care. 2014. doi: 10.1007/s12028-014-0040-6 [DOI] [PubMed] [Google Scholar]
- 14.Olson DM, Zomorodi M, Britz GW, Zomorodi AR, Amato A, Graffagnino C. Continuous cerebral spinal fluid drainage associated with complications in patients admitted with subarachnoid hemorrhage. J Neurosurg. 2013. doi: 10.3171/2013.6.jns122403 [DOI] [PubMed] [Google Scholar]
- 15.Griesdale DEG, McEwen J, Kurth T, Chittock DR. External ventricular drains and mortality in patients with severe traumatic brain injury. Can J Neurol Sci. 2010;37(1):43–48. doi: 10.1017/S031716710000963X [DOI] [PubMed] [Google Scholar]
- 16.Mack WJ, King RG, Ducruet AF, et al. Intracranial pressure following aneurysmal subarachnoid hemorrhage: monitoring practices and outcome data. Neurosurg Focus. 2003;14(4):e3 http://www.ncbi.nlm.nih.gov/pubmed/15679302. [DOI] [PubMed] [Google Scholar]
- 17.Kang D-H, Park J, Park S-H, Kim Y-S, Hwang S-K, Hamm I-S. Early Ventriculoperitoneal Shunt Placement After Severe Aneurysmal Subarachnoid HemorrhageRole of Intraventricular Hemorrhage and Shunt Function. Neurosurgery. 2010;66(5):904–909. 10.1227/01.NEU.0000368385.74625.96. [DOI] [PubMed] [Google Scholar]
- 18.Akbik OS, Carlson AP, Yonas H. The roles of ventricular and parenchymal intracranial pressure monitoring. Curr Neurobiol 2016;7(1):1–6. doi: 10.4172/0975-9042.000107 [DOI] [Google Scholar]
- 19.Hickey JV, Olson DM Intracranial hypertension: theory and management of increased intracranial pressure In: Hickey JV, ed. . 6th ed., PA: Wolters Kluwer/Lippincott Williams & Wi. In: Hickey JV, ed. The Clinical Practice of Neurological and Neurosurgical Nursing. 6th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2009:270–307. [Google Scholar]
- 20.Slazinkski T, Anderson T, Cattell E, Eigsti J, Heimsoth S. Care of the Patient Undergoing Intracranial Pressure Monitoring / External Ventricular Drainage or Lumbar Drainage. AANN Clin Pract Guidel Ser. 2011:1–38. [Google Scholar]
- 21.Mahdavi ZK, Olson DM, Figueroa SA. Association Patterns of Simultaneous Intraventricular and Intraparenchymal Intracranial Pressure Measurements. Neurosurgery. 2016;79(4):561–566. doi: 10.1227/NEU.0000000000001265 [DOI] [PubMed] [Google Scholar]
- 22.Olson DWM, McNett MM, Lewis LS, Riemen KE, Bautista C. Effects of nursing interventions on intracranial pressure. Am J Crit Care. 2013. doi: 10.4037/ajcc2013751 [DOI] [PubMed] [Google Scholar]
- 23.Chung DY, Mayer SA, Rordorf GA. External Ventricular Drains After Subarachnoid Hemorrhage: Is Less More? Neurocrit Care. 2018. doi: 10.1007/s12028-017-0443-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kasuya H, Shimizu T, Kagawa M. The effect of continuous drainage of cerebrospinal fluid in patients with subarachnoid hemorrhage: A retrospective analysis of 108 patients. Neurosurgery. 1991. doi: 10.1227/00006123-199101000-00009 [DOI] [PubMed] [Google Scholar]
- 25.Olson DM, Rogers MS, Stutzman SE. Electronic Medical Record Validation: Exploring the Reliability of Intracranial Pressure Data Abstracted From the Electronic Medical Record–Pilot. J Nurs Meas. 2015. doi: 10.1891/1061-3749.23.3.532 [DOI] [PubMed] [Google Scholar]
- 26.Connolly ES, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: A guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2012. doi: 10.1161/STR.0b013e3182587839 [DOI] [PubMed] [Google Scholar]
- 27.Kirkman MA, Smith M. Intracranial pressure monitoring, cerebral perfusion pressure estimation, and ICP/CPP-guided therapy: A standard of care or optional extra after brain injury? Br J Anaesth. 2014;112(1):35–46. doi: 10.1093/bja/aet418 [DOI] [PubMed] [Google Scholar]
- 28.Rincon F, Rossenwasser RH, Dumont A. The epidemiology of admissions of nontraumatic subarachnoid hemorrhage in the United States. Neurosurgery. 2013;73(2):217–222. doi: 10.1227/01.neu.0000430290.93304.33 [DOI] [PubMed] [Google Scholar]
- 29.Johnston SC, Selvin S, Gress DR. The burden, trends, and demographics of mortality from subarachnoid hemorrhage. Neurology. 1998;50(5):1413–1418. doi: 10.1212/WNL.50.5.1413 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 2. Flow diagram depicting the decision-making process of the neurological intensive care team with regard to ICP monitoring in patients with SAH. EVD: external ventricular drain; ICP: intracranial pressure.