Abstract
Background:
Many factors contribute to the risk for subsequent anterior cruciate ligament reconstruction (ACLR) within 2 years from the index procedure.
Purpose/Hypothesis:
The purpose of this study was 2-fold: (1) to evaluate the incidence of subsequent (revision or contralateral) ACLR at 2 years in a large cohort and (2) to explore the association between patient-specific factors and early subsequent ACLR risk by age group. We hypothesize that 2-year subsequent (revision or contralateral) ACLR rates will be low and that risk factors for subsequent (revision or contralateral) ACLR will vary depending on a patient’s age group.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
The California Office of Statewide Health Planning and Development Ambulatory Surgery Database was retrospectively reviewed to assess the incidence of 2-year subsequent (revision or contralateral) ACLR and to identify patient-specific risk factors for early subsequent (revision or contralateral) ACLR by age group between 2005 and 2014.
Results:
Of 94,108 patients included, the rate of subsequent (revision or contralateral) ACLR was highest in patients younger than 21 years (2.4 per 100 person-years; 95% CI, 2.3-2.6) and lowest in those older than 40 years (1.3 per 100 person-years; 95% CI, 1.2-1.4). Younger age, white race (compared with Hispanic in all age groups and Asian in age <21 or >40 years), private insurance if age younger than 21 years, public insurance or worker's compensation claims if age older than 30 years were significantly associated with an increased risk of subsequent (revision or contralateral) ACLR at 2 years.
Conclusion:
Results of the present study provide insight into subsequent (revision or contralateral) ACL reconstruction, which can be used to assess and modify treatment for at-risk patients and highlight the need for data mining to generate clinically applicable research using national and international databases.
Keywords: anterior cruciate ligament, ACL reconstruction, subsequent surgery, revision, contralateral, risk factors
Primary anterior cruciate ligament reconstruction (ACLR) can restore knee stability and improve function after ACL tears.20 Although the procedure has a high satisfaction rate in the literature, some patients eventually undergo subsequent ACLR procedures, including an ipsilateral or contralateral ACLR surgery.27
Graft-related factors (eg, type and method of fixation) have been reported as risk factors for subsequent (revision or contralateral) ACLR.11,18,19 Based on previous studies in patients who underwent primary ACLR, the rate of primary ACL graft rupture ranges from 4.4% to 7.7%, whereas the rate of contralateral ACL rupture in those patients falls between 4.4% and 11.8%.15,19,43 However, other variables have also been identified as independent risk factors for revision ACLR, including age, sex, race, body mass index (BMI), activity level, smoking status, and concomitant injury.1,4,19,23,24,26,41 Revision ACLR results in significantly inferior clinical and patient-reported outcomes compared with primary ACLR.20,21,35,41,42
In addition to reporting revision ACLR rates, studies have also reported the risk of contralateral ACLR surgery after primary ACLR. Roughly equal risk of revision and contralateral ACLR has been observed in the literature.27 The overall incidence rate of a subsequent ACLR procedure was 7.3% in the study by McCarthy et al,27 with 5.5% being ipsilateral procedures (revision) and 2.2% being contralateral ACLR. Andernord et al3,4 reported a 1.6% revision ACLR rate and 3% contralateral ACLR rate at 2 years postoperatively in a group of patients who underwent primary ACLR.
As mentioned, multiple factors have been reported to increase the risk for revision ACLR or injury of the contralateral ACL.19,40,41,43 Specifically, age has been shown to be a major contributor to revision ACLR rates and to modify the effect of other known risk factors after primary ACLR.24 The risk factors for contralateral ACLR have not been well studied. With the majority of previous studies focusing on large populations and long-term follow-up, age stratification of patient-specific risk factors for early subsequent (revision or contralateral) ACLR is not well documented.
The purpose of this study was 2-fold: (1) to evaluate the incidence of subsequent (revision or contralateral) ACLR at 2 years in a large cohort and (2) to explore the association between patient-specific factors and early subsequent ACLR risk by age group. Our hypothesis is that 2-year subsequent ACLR rates will be low and that risk factors for subsequent (revision or contralateral) ACLR will vary depending on a patient’s age group.
Methods
Data Source
The California Office of Statewide Health Planning and Development (OSHPD) Ambulatory Surgery Database (ASD) is a publicly available health care data set from all state-licensed ambulatory surgery centers and hospitals licensed for outpatient surgery. The data are maintained and validated by OSHPD and amounted to approximately 130,000 cases per year during the study period. The data include detailed information on demographics, diagnoses, and procedures. Patients can be tracked longitudinally using a unique record linker number, regardless of whether a patient moves within California or sees a different physician. The OSPHD database has previously been used in multiple large-scale orthopaedic studies.14,37,38
Case Selection
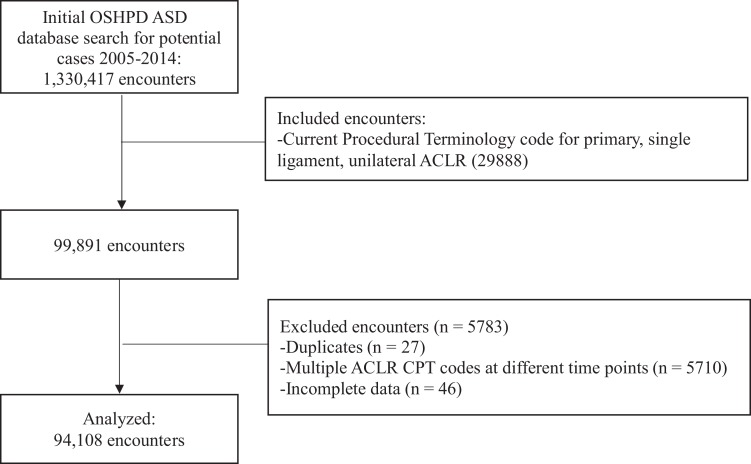
A search of the OSHPD ASD (years 2005-2014; 2005 is the first year ASD data were available) identified a total of 1,330,417 encounters. Of these, 99,891 had a Current Procedural Terminology (CPT) code for primary, single-ligament, unilateral ACLR (29888). Duplicate records were excluded (n = 27). Demographic data collected for each encounter included age, sex, race/ethnicity, and expected source of payment. Encounters were excluded if collected data were incomplete (n = 46). An additional 5710 encounters were excluded because they represented patients with multiple ACLR CPT codes at different time points; in these cases, the encounter data from the initial ACLR were kept. The final number of patients included for analysis in our study was 94,108 (Figure 1).
Figure 1.
Flowchart displaying the encounter selection process using the OSHPD database. ACLR, anterior cruciate ligament reconstruction; CPT, Current Procedural Terminology; OSHPD ASD, California Office of Statewide Health Planning and Development Ambulatory Surgery Database.
Outcome of Interest
The primary endpoint of the study was subsequent ACLR within 2 years of primary ACLR. Inherent limitations of the database made it impossible to specify laterality, and therefore, a subsequent ACLR was defined as second ACLR (ipsilateral-revision or contralateral), based on CPT code, within 2 years of the initial reconstruction for a given patient record. We made this assumption based on existing evidence showing that the overall risks of contralateral and ipsilateral ACLR are roughly equal after an index ACLR.3,27,29
Variables of Interest
Several patient characteristics were assessed as potential factors influencing the risk of subsequent (revision or contralateral) ACLR, including age at time of primary ACLR, sex, race/ethnicity (white, black, Hispanic, Asian/Pacific Islander, Native American, other, and not reported), and expected source of payment (ie, insurance type). Insurance type was defined as (1) private (preferred provider organization, point-of-service plan, exclusive provider organization, health maintenance organization, and Blue Cross/Blue Shield), (2) public (Medicare A or B, Medi-Cal), and (3) workers’ compensation health claims. Patients with an expected payment source not described by the composite insurance variables were excluded from the multivariable models described later (n = 9038). Analysis was performed in the overall cohort as well as in 4 age groups: <21, 21-30, 31-40, and >40 years of age. Patient age at the time of surgery determined the patient’s assignment to one of the age population subgroups. Follow-up time was defined as the time between primary ACLR and subsequent (revision or contralateral) ACLR or end of study period.
Statistical Analysis
Descriptive statistics and incidence of subsequent (revision or contralateral) ACLR estimates at 2 years after primary ACLR are provided for the overall cohort and for each of the 4 age groups. Risk of subsequent (revision or contralateral) ACLR was modeled in each age group using Kaplan-Meier curves and Cox proportional hazard models. Crude and adjusted hazard ratios (HRs) and 95% CIs are reported, using the age group older than 40 years as the reference because this group had the lowest incidence of subsequent surgery. Patient factors (age, sex, race, and insurance type) were deemed clinically relevant potential confounders and were included in the final multivariable model. Additional analysis was performed within each age group to identify age-based risk factors for subsequent (revision or contralateral) ACLR. The covariates described were evaluated as risk factors using Cox proportional hazards models, and HRs and 95% CIs are reported. All statistical analysis was performed using Stata Version 13.0 (IBM Corp). P < .05 was set as the level of significance.
Results
Study Population
Of the 94,108 patients in the study population, the majority were male, white, and privately insured. Table 1 shows detailed participant characteristics in the overall cohort and stratified by age group. In patients who underwent subsequent (revision or contralateral) ACLR, the mean age was 28 ± 12 years, 63% were male, 58% were white, and 82% had private insurance. On average, the time from primary ACLR to subsequent (revision or contralateral) ACLR was 0.97 ± 0.55 years.
Table 1.
Patient Demographicsa
| Age Group | |||||
|---|---|---|---|---|---|
| Overall Cohort (N = 94,108) |
<21 y (n = 21,346) |
21-30 y (n = 22,800) |
31-40 y (n = 24,109) |
>40 y (n = 25,853) |
|
| Age, y, mean ± SD | 32.5 ± 12.1 | 17.7 ± 2.1 | 25.8 ± 2.7 | 35.3 ± 3.0 | 48.1 ± 6.4 |
| Male sex | 60,375 (64.2) | 12,107 (56.7) | 16,708 (73.3) | 16,676 (69.2) | 14,884 (57.6) |
| Race/ethnicity | |||||
| White | 51,528 (54.8) | 9908 (46.4) | 11,360 (49.8) | 13,053 (54.1) | 17,207 (66.6) |
| Black | 4569 (4.9) | 1752 (8.2) | 1108 (4.9) | 951 (3.9) | 758 (2.9) |
| Hispanic | 20,224 (21.5) | 5908 (27.7) | 5422 (23.8) | 5154 (21.4) | 3740 (14.5) |
| Asian/Pacific Islander | 7830 (8.3) | 1793 (8.4) | 2309 (10.1) | 2220 (9.2) | 1508 (5.8) |
| Native American | 360 (0.4) | 70 (0.3) | 85 (0.4) | 101 (0.4) | 104 (0.4) |
| Other | 3535 (3.8) | 852 (4.0) | 1022 (4.5) | 910 (3.8) | 751 (2.9) |
| Not reported | 6062 (6.4) | 1063 (5.0) | 1494 (6.6) | 1720 (7.1) | 1785 (6.9) |
| Payer | |||||
| Private | 71,417 (84.0) | 16,796 (86.1) | 17,353 (86.3) | 18,322 (83.8) | 18,946 (80.4) |
| Public | 5929 (7.0) | 2434 (12.5) | 1036 (5.2) | 1042 (4.8) | 1417 (6.0) |
| Workers’ compensation | 7724 (9.1) | 277 (1.4) | 1730 (8.6) | 2508 (11.5) | 3209 (13.6) |
aReported as number (percentage) unless otherwise noted.
Subsequent ACLR Risk
Overall, 2957 (3.1%) patients in the study went on to subsequent (revision or contralateral) ACLR within 2 years. In our age-group analysis (Table 2), subsequent (revision or contralateral) ACLR was highest in patients younger than 21 years (2.4 procedures per 100 person-years; 95% CI, 2.3-2.6) and lowest in those older than 40 years (1.3 procedures per 100 person-years; 95% CI, 1.2-1.4). After adjusting for sex, race/ethnicity, and insurance type, and compared with patients older than 40 years, patients younger than 21 years were 2.1 times (95% CI, 1.9-2.3; P < .001) more likely to undergo subsequent (revision or contralateral) ACLR at 2 years, and patients age 21 to 30 years were 1.3 times (95% CI, 1.2-1.4; P < .001) more likely to do so. Patients aged 31 to 40 years did not have a significantly different subsequent (revision or contralateral) ACLR risk compared with those older than 40.
Table 2.
Crude Subsequent (Revision or Contralateral) ACLRs, Incidence Rate of Subsequent ACLR, and Subsequent ACLR Riska
| Age Group | |||||
|---|---|---|---|---|---|
| Overall Cohort | <21 y | 21-30 y | 31-40 y | >40 y | |
| Subsequent (revision or contralateral) ACLR, n (%)a | 2957 (3.14) | 1006 (4.71) | 685 (3.00) | 622 (2.58) | 644 (2.49) |
| Incidence rate of subsequent (revision or contralateral) ACLR per 100 person-years (95% CI) | 1.60 (1.54-1.65) | 2.41 (2.26-2.56) | 1.53 (1.41-1.64) | 1.31 (1.21-1.41) | 1.26 (1.17-1.36) |
| Crude HR (95% CI)b | 1.91 (1.73-2.10) | 1.21 (1.08-1.34) | 1.03 (0.93-1.16) | Reference | |
| P value | <.001 | .001 | .54 | Reference | |
| Adjusted HR (95% CI)b,c | 2.10 (1.89-2.34) | 1.29 (1.15-1.44) | 1.07 (0.95-1.20) | Reference | |
| P value | <.001 | <.001 | .25 | Reference | |
aValues are reported as number, incidence rate, or hazard ratio. ACLR, anterior cruciate ligament reconstruction; HR, hazard ratio.
bAge group >40 used as reference, as this group had the lowest incidence rate of subsequent ACLR.
cModels adjusted for age, sex, race/ethnicity, and insurance type.
Patient-Specific Risk Factors
Patient-specific risk factors for 2-year subsequent (revision or contralateral) ACLR were assessed in the overall cohort and in each of the 4 age groups. A complete list of risk factors is included in Table 3. Older age at the time of initial ACLR was associated with decreased risk of subsequent (revision or contralateral) ACLR in each age group, with the greatest effect observed in patients younger than 21 years (HR, 0.83; 95% CI, 0.81-0.85; P < .001). Similarly, Hispanic ethnicity compared with white was associated with a decreased subsequent (revision or contralateral) ACLR risk in all age groups, with patients younger than 21 years showing the strongest association (HR, 0.67; 95% CI, 0.57-0.79; P < .001). Black race showed a trend toward a lower subsequent (revision or contralateral) ACLR risk in patients younger than 21 years (HR, 0.78; 95% CI, 0.60-1.00; P = .05). Asian/Pacific Islander ethnicity was associated with a decreased risk of subsequent ACLR compared with white, specifically in age younger than 21 years (HR, 0.76; 95% CI, 0.60-0.98; P = .03) and age older than 40 years (HR, 0.58; 95% CI, 0.38-0.89; P = .01). Native American ethnicity was not associated with subsequent (revision or contralateral) ACLR risk in any analyses. Public insurance compared with private was associated with a decreased subsequent (revision or contralateral) ACLR risk in patients younger than 21 years (HR, 0.70; 95% CI, 0.56-0.88; P = .002) but a greater risk in patients older than 30 years (HR, 1.73; 95% CI, 1.26-2.38; P = .001 for age 31-40 years; HR, 2.06; 95% CI, 1.54-2.75; P < .001 for age >40 years). Workers’ compensation was associated with a higher risk of subsequent (revision or contralateral) ACLR in the older age groups (HR, 1.68; 95% CI, 1.34-2.10; P < .001 for age 31-40 years; HR, 1.47; 95% CI, 1.18-1.83; P = .001 for age >40 years) whereas no statistically significant association was observed in the younger groups. Sex was not associated with subsequent (revision or contralateral) ACLR risk in any analysis (overall HR, 1.04; 95% CI, 0.97-1.13; P = .27).
Table 3.
Adjusted Patient-Specific Risk Factors for Subsequent (Revision or Contralateral) ACLRa
| Age Group | |||||
|---|---|---|---|---|---|
| Overall Cohort | <21 y | 21-30 y | 31-40 y | >40 y | |
| Age at primary ACLR | 0.97 (0.97-0.97) | 0.83 (0.81-0.85) | 0.84 (0.82-0.86) | 0.90 (0.87-0.92) | 0.96 (0.94-0.97) |
| P value | <.001 | <.001 | <.001 | <.001 | <.001 |
| Female sex (reference: male) | 1.04 (0.97-1.13) | 0.95 (0.83-1.08) | 0.93 (0.78-1.12) | 0.88 (0.72-1.06) | 1.05 (0.89-1.24) |
| P value | .27 | .43 | .45 | .17 | .58 |
| Race/ethnicity (reference: white) | |||||
| Black | 0.78 (0.65-0.93) | 0.78 (0.60-1.00) | 0.80 (0.54-1.19) | 0.73 (0.46-1.16) | 0.66 (0.39-1.12) |
| P value | .01 | .05 | .27 | .19 | .13 |
| Hispanic | 0.70 (0.63-0.77) | 0.67 (0.57-0.79) | 0.75 (0.61-0.93) | 0.75 (0.60-0.93) | 0.68 (0.53-0.99) |
| P value | <.001 | <.001 | .01 | .01 | .003 |
| Asian/Pacific Islander | 0.73 (0.63-0.85) | 0.76 (0.60-0.98) | 0.83 (0.62-1.10) | 0.77 (0.56-1.05) | 0.58 (0.38-0.89) |
| P value | <.001 | .03 | .12 | .10 | .01 |
| Native American | 0.97 (0.53-1.76) | 0.85 (0.27-2.66) | Not enough observations | 1.86 (0.77-4.49) | 1.10 (0.35-3.42) |
| P value | .93 | .79 | .17 | .87 | |
| Other | 0.81 (0.66-0.99) | 0.87 (0.62-1.22) | 0.67 (0.43-1.06) | 0.97 (0.64-1.49) | 0.82 (0.50-1.35) |
| P value | .04 | .43 | .09 | .91 | .43 |
| Not reported | 1.01 (0.87-1.18) | 0.95 (0.70-1.29) | 1.30 (0.98-1.74) | 0.91 (0.66-1.27) | 1.00 (0.73-1.37) |
| P value | .89 | .73 | .07 | .59 | .99 |
| Payer (reference: private) | |||||
| Public | 1.11 (0.96-1.28) | 0.70 (0.56-0.88) | 0.95 (0.65-1.41) | 1.73 (1.26-2.38) | 2.06 (1.54-2.75) |
| P value | .16 | .002 | .82 | .001 | <.001 |
| Workers’ compensation | 1.39 (1.21-1.58) | 1.50 (0.86-2.61) | 1.19 (0.90-1.57) | 1.68 (1.34-2.10) | 1.47 (1.18-1.83) |
| P value | <.001 | .15 | .22 | <.001 | .001 |
aValues are reported as hazard ratio (95% CI). Bolded P values indicate statistical significance. Models were adjusted for age, sex, race/ethnicity, and insurance type. ACLR, anterior cruciate ligament reconstruction.
Discussion
This database study evaluated the age-related incidence of early subsequent (revision or contralateral) ACLR and the association between early subsequent ACLR and sex, race, and insurance type. The 2-year subsequent (revision or contralateral) ACLR rates were highest in patients younger than 21 years, and patient-specific risk factors for subsequent ACLR are age-dependent at 2 years. In particular, race was found to be a risk factor for subsequent (revision or contralateral) ACLR in all age groups, and insurance type was a risk factor for patients younger than 21 or older than 30 years. Workers’ compensation increased subsequent (revision or contralateral) ACLR risk, except in patients younger than 21 years.
Subsequent (revision or contralateral) ACLR at 2 years was associated with younger age in our study. The incidence of subsequent (revision or contralateral) ACLR was the highest in patients younger than 21 years, and within each age group, younger age was associated with a greater likelihood of subsequent ACLR, which has been demonstrated in previous studies.1,4,7,15,19,22,24–26 Andernord et al4 reported a 2.67 and 2.25 times greater likelihood of 2-year revision ACLR in adolescent (age 13-19 years) males and females, respectively. Maletis et al24 showed a revision rate of 5.3% at 2 years in patients younger than 21 years compared with the Andernord cohort, with a rate of 4.71%. The higher rates of subsequent ACLR in young patients are thought to be due to participation in high-risk athletic activities or poor compliance with postoperative precautions.6,8 It should also be noted that patients aged 31 to 40 years did not have an increased risk of subsequent (revision or contralateral) ACLR, suggesting that age older than 30 years may be an important cutoff point with regard to subsequent risk stratification. Taken together, our findings underscore the challenge of caring for younger patients with primary ACLR and emphasize the need for future studies to define an optimal treatment and rehabilitation protocol for this patient population.
Sex was not associated with the risk of early subsequent (revision or contralateral) ACLR in the overall cohort or in any age group. Understanding sex-based differences in subsequent (revision or contralateral) ACLR is of particular importance as several studies have shown increased incidence of primary ACLR in women.5,34,36 In contrast, 64% of the patients who underwent primary ACLR in this cohort were male. Conflicting reports have previously been published on sex as a risk factor for revision ACLR.4,7,18,24,26 In a meta-analysis, Ryan et al32 found no significant difference in ACLR failure risk by sex but acknowledged that additional high-quality studies are needed. Dynamic neuromuscular control of the knee is one factor associated with a higher risk of ACL injury in women, and studies have shown that neuromuscular training reduces the level of ACL injury to that of males.2,16,17 Other factors may play a role in subsequent (revision or contralateral) ACLR rates in male and female populations. Although multiple factors, including differing responses to particular graft types and degree of postoperative laxity in male and female patients,32 have been postulated to potentially alter subsequent ACLR rates, this is not demonstrated by the results of our data.
Race/ethnicity was a risk factor for subsequent (revision or contralateral) ACLR in our study, which has not been well documented in the literature. We showed that black race (compared with white) was associated with a 22% reduced risk of early subsequent (revision or contralateral) ACLR in the overall cohort and trended toward significance in the age group younger than 21 years. Similarly, Maletis et al26 reported that black patients were 46% less likely to undergo revision ACLR at 5 years compared with white patients. In a subsequent age-group analysis, Maletis et al24 found a similar association in patients younger than 21 years, and this group drove the effect observed in the overall cohort. Of note, the 2 studies by Maletis et al24,26 were performed using the Kaiser Permanente National Anterior Cruciate Ligament Reconstruction Registry, and access to services or insurance type therefore should not have been different between individuals. Our study did not directly evaluate the interaction between insurance type and race, but when we controlled for insurance type in the adjusted models, black race was still an independent predictor of reduced subsequent (revision or contralateral) ACLR risk in the overall cohort.
A novel finding of our study was the association between Hispanic ethnicity and subsequent (revision or contralateral) ACLR risk. In the adjusted models, Hispanic ethnicity was associated with a significantly decreased subsequent (revision or contralateral) ACLR risk in all age groups. Further, a 30% reduction in subsequent ACLR risk was seen in the group younger than 21 years. Maletis et al24 reported a similar decrease in revision risk but only in Hispanic individuals aged 31 to 40 years. Although the proportions of Hispanic and white individuals in the 2 studies were similar, the larger population size in the current study may be responsible for the improved detection of this association in other age groups. Although representing a smaller subset of our study population, our analysis revealed a significant decrease in subsequent (revision or contralateral) ACLR risk in Asian patients in both the under-21 and over-40 age groups. To our knowledge, this is the first report of an association between Asian race and subsequent (revision or contralateral) ACLR risk. Race and ethnicity present multifaceted concepts with a high degree of complex interplay of social and biological variables. Further research into subsequent ACLR and race may shed more light on race as a risk factor. Based on these data, there were differences by race. This represents an opportunity for further study.
Previous studies on primary ACLR reported that younger age, lower socioeconomic status, and public insurance are all associated with delays in care and additional surgeries at time of primary reconstruction.9,10,30,31 In our study, insurance was evaluated as a potential risk factor for subsequent (revision or contralateral) ACLR. We found no difference in subsequent (revision or contralateral) ACLR risk between public and private insurance in the overall cohort. However, patients younger than 21 years and with public insurance (compared with private) were 30% less likely to undergo subsequent ACLR at 2 years. In patients aged 31-40 and >40 years, public insurance was associated with a significantly higher risk of subsequent (revision or contralateral) ACLR. The finding in patients younger than 21 years with public insurance may be related to decreased access to care. In future work, it would be useful to elucidate whether the decreased subsequent ACLR rate in these populations is due to a lower retear rate or less access to care for subsequent (revision or contralateral) ACLR surgery.
Workers’ compensation was a risk factor for subsequent (revision or contralateral) ACLR at 2 years and demonstrated age dependence. In patients older than 31 years of age, claiming workers’ compensation was associated with a significantly increased risk of subsequent (revision or contralateral) ACLR compared with patients who had private insurance. Workers’ compensation was not associated with subsequent (revision or contralateral) ACLR risk in patients younger than 21 years or those 21 to 30 years. Our findings are consistent with previous studies that have shown that workers’ compensation status has a detrimental effect on orthopaedic outcomes,12,13,28 particularly for ACL outcomes.39 The results of the present study are important for physicians to consider when discussing the risks and benefits of surgery in individuals older than 30 years who have a workers’ compensation claim.
The main drawback of this study was the inability to lateralize the side of ACLR due to the use of CPT codes, which stems from limitations of the database. Specifically, all second ACLR codes associated with a patient’s identification number were recorded as “revision ACLR,” which includes ipsilateral (revision) ACLR or contralateral ACLR. As mentioned above, our decision to investigate the risk factors of subsequent ACLR procedure (revision or contralateral) was based on previous studies reporting roughly equal risk of revision and contralateral ACLR after an index ACLR. This, however, compromises the external validity of our results. To overcome similar deficiencies in future studies that use national or international databases to evaluate the risk factors and outcomes of surgical procedures, data mining is absolutely necessary to produce clinically applicable results. In reference to the data set used in this analysis, ACL data registries should include the nature and laterality of subsequent procedures performed to allow for the identification of risk factors and the development of prevention strategies.
Database deficiencies in coding have also demonstrated inherent limitations and error, as described by Sanders et al.33 Moreover, the OSHPD database lacked many patient- and surgery-specific factors that have previously been related to subsequent (revision or contralateral) ACLR and precluded the analysis of their impact on subsequent ACLR in our cohort. The database was also unable to account for patients who left California during the study period. We noted a decline in reported cases from 2007 to 2014; this is a presumed result of a change in license requirements of ambulatory surgery centers in California in 2007 (Capen v. Shewry, No. C047172 [Cal. Ct. App. Sept. 19, 2007]). Nonetheless, the case volume remained high, with 7125 reported in the final year of our study. Finally, ACLR was used as the endpoint of our study and cannot account for cases that were treated nonoperatively.
Conclusion
Our study found that age younger than 21 years was the biggest risk factor for subsequent (revision or contralateral) ACLR. A lower risk of subsequent (revision or contralateral) ACLR was found in black, Asian, and Hispanic groups compared with white patients in all age groups. In addition, we showed that workers’ compensation status is an independent risk factor for subsequent (revision or contralateral) ACLR, but only in older patients. Results of this study may be used to inform clinical decision making and to more appropriately counsel patients undergoing primary ACLR.
Footnotes
Final revision submitted October 30, 2019; accepted November 6, 2019.
The authors would like to acknowledge The Cappo Family Research Fund.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.P.P. has received educational support from DePuy and hospitality payments from Zimmer Biomet, Exactech, and Integra Lifesciences. G.F.H. has received speaking fees from Arthrex, educational support from Micromed, and honoraria from Fidia Pharma. A.E.W. has received educational support from Arthrex and Smith & Nephew, speaking fees from Arthrex, and hospitality payments from Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Ahldén M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40(10):2230–2235. [DOI] [PubMed] [Google Scholar]
- 2. Alentorn-Geli E, Myer GD, Silvers HJ, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players, part 2: a review of prevention programs aimed to modify risk factors and to reduce injury rates. Knee Surg Sports Traumatol Arthrosc. 2009;17(8):859–879. [DOI] [PubMed] [Google Scholar]
- 3. Andernord D, Björnsson H, Petzold M, et al. Surgical predictors of early revision surgery after anterior cruciate ligament reconstruction: results from the Swedish National Knee Ligament Register on 13,102 patients. Am J Sports Med. 2014;42(7):1574–1582. [DOI] [PubMed] [Google Scholar]
- 4. Andernord D, Desai N, Björnsson H, Ylander M, Karlsson J, Samuelsson K. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med. 2015;43(1):121–127. [DOI] [PubMed] [Google Scholar]
- 5. Arendt EA, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999;34(2):86–92. [PMC free article] [PubMed] [Google Scholar]
- 6. Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009;37(12):2362–2367. [DOI] [PubMed] [Google Scholar]
- 7. Bourke HE, Salmon LJ, Waller A, Patterson V, Pinczewski LA. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40(9):1985–1992. [DOI] [PubMed] [Google Scholar]
- 8. Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40(11):2517–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Collins JE, Katz JN, Donnell-Fink LA, Martin SD, Losina E. Cumulative incidence of ACL reconstruction after ACL injury in adults: role of age, sex, and race. Am J Sports Med. 2013;41(3):544–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42(3):675–680. [DOI] [PubMed] [Google Scholar]
- 11. Eysturoy NH, Nissen KA, Nielsen T, Lind M. The influence of graft fixation methods on revision rates after primary anterior cruciate ligament reconstruction. Am J Sports Med. 2018;46(3):524–530. [DOI] [PubMed] [Google Scholar]
- 12. Gruson KI, Huang K, Wanich T, Depalma AA. Workers’ compensation and outcomes of upper extremity surgery. J Am Acad Orthop Surg. 2013;21(2):67–77. [DOI] [PubMed] [Google Scholar]
- 13. Harris I, Mulford J, Solomon M, van Gelder JM, Young J. Association between compensation status and outcome after surgery: a meta-analysis. JAMA. 2005;293(13):1644–1652. [DOI] [PubMed] [Google Scholar]
- 14. Hawker GA, Coyte PC, Wright JG, Paul JE, Bombardier C. Accuracy of administrative data for assessing outcomes after knee replacement surgery. J Clin Epidemiol. 1997;50(3):265–273. [DOI] [PubMed] [Google Scholar]
- 15. Hettrich CM, Dunn WR, Reinke EK, Spindler KP, Group M. The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med. 2013;41(7):1534–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hewett TE, Myer GD, Ford KR. Reducing knee and anterior cruciate ligament injuries among female athletes: a systematic review of neuromuscular training interventions. J Knee Surg. 2005;18(1):82–88. [DOI] [PubMed] [Google Scholar]
- 17. Hewett TE, Zazulak BT, Myer GD, Ford KR. A review of electromyographic activation levels, timing differences, and increased anterior cruciate ligament injury incidence in female athletes. Br J Sports Med. 2005;39(6):347–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kaeding CC, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3(1):73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Spindler KP; MOON Consortium. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43(7):1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kamath GV, Redfern JC, Greis PE, Burks RT. Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(1):199–217. [DOI] [PubMed] [Google Scholar]
- 21. Liechti DJ, Chahla J, Dean CS, et al. Outcomes and risk factors of rerevision anterior cruciate ligament reconstruction: a systematic review. Arthroscopy. 2016;32(10):2151–2159. [DOI] [PubMed] [Google Scholar]
- 22. Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40(7):1551–1557. [DOI] [PubMed] [Google Scholar]
- 23. Magnussen RA, Borchers JR, Pedroza AD, et al. Risk factors and predictors of significant chondral surface change from primary to revision anterior cruciate ligament reconstruction: a MOON and MARS cohort study. Am J Sports Med. 2018;46(3):557–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Maletis GB, Chen J, Inacio MC, Funahashi TT. Age-related risk factors for revision anterior cruciate ligament reconstruction: a cohort study of 21,304 patients from the Kaiser Permanente anterior cruciate ligament registry. Am J Sports Med. 2016;44(2):331–336. [DOI] [PubMed] [Google Scholar]
- 25. Maletis GB, Granan LP, Inacio MC, Funahashi TT, Engebretsen L. Comparison of community-based ACL reconstruction registries in the U.S. and Norway. J Bone Joint Surg Am. 2011;93(suppl 3):31–36. [DOI] [PubMed] [Google Scholar]
- 26. Maletis GB, Inacio MC, Funahashi TT. Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR registry. Am J Sports Med. 2015;43(3):641–647. [DOI] [PubMed] [Google Scholar]
- 27. McCarthy M, Mallett K, Abola M, Vassallo S, Nguyen J. Hospital for Special Surgery ACL registry: 2-year outcomes suggest low revision and return to OR rates. HSS J. 2017;13(2):119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Morris BJ, Haigler RE, Laughlin MS, Elkousy HA, Gartsman GM, Edwards TB. Workers’ compensation claims and outcomes after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24(3):453–459. [DOI] [PubMed] [Google Scholar]
- 29. Nagelli CV, Hewett TE. Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? Biological and functional considerations. Sports Med. 2017;47(2):221–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Newman JT, Carry PM, Terhune EB, et al. Delay to reconstruction of the adolescent anterior cruciate ligament: the socioeconomic impact on treatment. Orthop J Sports Med. 2014;2(8):2325967114548176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nordenvall R, Marcano AI, Adami J, et al. The effect of socioeconomic status on the choice of treatment for patients with cruciate ligament injuries in the knee: a population-based cohort study. Am J Sports Med. 2017;45(3):535–540. [DOI] [PubMed] [Google Scholar]
- 32. Ryan J, Magnussen RA, Cox CL, Hurbanek JG, Flanigan DC, Kaeding CC. ACL reconstruction: do outcomes differ by sex? A systematic review. J Bone Joint Surg Am. 2014;96(6):507–512. [DOI] [PubMed] [Google Scholar]
- 33. Sanders TL, Pareek A, Desai VS, et al. Low accuracy of diagnostic codes to identify anterior cruciate ligament tear in orthopaedic database research. Am J Sports Med. 2018;46(12):2894–2898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Schilaty ND, Bates NA, Nagelli C, Krych AJ, Hewett TE. Sex-based differences in knee kinetics with anterior cruciate ligament strain on cadaveric impact simulations. Orthop J Sports Med. 2018;6(3):2325967118761037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Spindler KP, Huston LJ, Chagin KM, et al. Ten-year outcomes and risk factors after anterior cruciate ligament reconstruction: a MOON longitudinal prospective cohort study. Am J Sports Med. 2018;46(4):815–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sutton KM, Bullock JM. Anterior cruciate ligament rupture: differences between males and females. J Am Acad Orthop Surg. 2013;21(1):41–50. [DOI] [PubMed] [Google Scholar]
- 37. Vitale MA, Arons RR, Hyman JE, Skaggs DL, Roye DP, Vitale MG. The contribution of hospital volume, payer status, and other factors on the surgical outcomes of scoliosis patients: a review of 3,606 cases in the State of California. J Pediatr Orthop. 2005;25(3):393–399. [DOI] [PubMed] [Google Scholar]
- 38. Vogel LA, Moen TC, Macaulay AA, et al. Superior labrum anterior-to-posterior repair incidence: a longitudinal investigation of community and academic databases. J Shoulder Elbow Surg. 2014;23(6):e119–e126. [DOI] [PubMed] [Google Scholar]
- 39. Wexler G, Bach BR, Bush-Joseph CA, Smink D, Ferrari JD, Bojchuk J. Outcomes of anterior cruciate ligament reconstruction in patients with workers’ compensation claims. Arthroscopy. 2000;16(1):49–58. [DOI] [PubMed] [Google Scholar]
- 40. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wright R, Spindler K, Huston L, et al. Revision ACL reconstruction outcomes: MOON cohort. J Knee Surg. 2011;24(4):289–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wright RW, Gill CS, Chen L, et al. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94(6):531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93(12):1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]