Abstract
Background:
Few studies have compared the clinical and radiological characteristics and outcomes in isolated subscapularis (SSC) and combined anterosuperior (AS) rotator cuff tears (RCTs). Furthermore, risk factors for retear after SSC repair and the effect of preoperative fatty degeneration require further evaluation.
Purpose:
To compare the functional and radiological outcomes of isolated SSC with combined AS RCTs after arthroscopic repair and to determine the risk factors for SSC retear in these 2 groups.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Data from 30 patients in the isolated SSC group were compared with data from 110 patients in the combined AS group. All patients underwent primary arthroscopic rotator cuff repair between 2010 and 2016. Clinical outcomes were assessed through use of the visual analog scale for pain, American Shoulder and Elbow Surgeons score, and Simple Shoulder Test at a mean follow-up of 26.7 months (range, 24-96 months). SSC tendon integrity was examined via magnetic resonance imaging, computed tomography arthrogram, or ultrasonography at least 1 year after surgery.
Results:
The isolated SSC group had a greater proportion of males and the patients were younger compared with the combined AS group (both P < .050). The incidence of trauma was high but not significantly different between groups (56.7% vs 40.9%; P = .180). Clinical outcome measures and radiological outcomes in terms of retear were not statistically different between both groups (16.7% vs 8/5%; P = .337). The optimal cutoff values for the risk of SSC tendon retear in both groups were 19-mm retraction and 16-mm superoinferior dimension (P = .048). Unfavorable preoperative fatty degeneration of the SSC muscle (grades 3 and 4) was a significant risk factor for retear (odds ratio, 9.8; P < .001).
Conclusion:
Isolated SSC and combined AS RCTs were comparable except for patient age and sex; both had a high incidence of traumatic history. The current data suggest that the risk factors for retear after SSC repair in RCTs involving the SSC were tear size greater than 19 mm of retraction and unfavorable fatty degeneration (grade 3 or higher) of the SSC muscle.
Keywords: subscapularis muscle, isolated subscapularis tears, combined anterosuperior tears, arthroscopic repair
Recently, an increase has been noted in the number of studies focused on rotator cuff tears (RCTs) involving the subscapularis (SSC) muscle to enable a better understanding of the diagnosis, management, and outcomes.35 The SSC is the largest rotator cuff tendon; it provides 50% of the rotator cuff force and plays an important role in shoulder stability and movements such as internal rotation, adduction, abduction, flexion, and extension.13,20,25,43 Hence, restoring the function of the SSC muscle after a tear is crucial for normal shoulder function.
The SSC muscle is reported to be involved in 78% of RCTs, most often in combination with other rotator cuff tendons.40 The incidence of isolated SSC RCTs is reported to be 4%,13 whereas combined RCTs involving the SSC and supraspinatus but without the infraspinatus (combined anterosuperior [AS]) are reported to account for 18% of all RCTs.42 In terms of etiology, the incidence of trauma is reported to be high (40%-80%) in patients with isolated SSC RCTs3,14,22,24,39,50,53 and combined AS RCTs.4,31,44 Moreover, because of the close proximity of the muscles in the rotator cuff, it is difficult to differentially diagnose isolated SSC and combined SSC RCTs; therefore, there is a need to evaluate the differences in their clinical and radiological characteristics as well as treatment outcomes.15,17,29,43 Notably, many previous studies have reported an improvement in SSC function after both open and arthroscopic repair compared with the preoperative status in isolated SSC3,6,22,27,39,41,45,52 and combined AS RCTs.5,12, 23
Furthermore, studies comparing the clinical outcomes in isolated SSC and combined AS RCTs have shown similar results after open repair.15 However, differences between isolated SSC and combined AS RCTs after arthroscopic repair in terms of functional and radiological outcomes merit further evaluation.
Negative radiological outcomes after SSC repair in terms of retear are associated with reduced functional outcomes upon postoperative assessment in isolated SSC and combined AS RCTs compared with healed tendon.15,17 Retear of the SSC has been attributed to preoperative high-grade fatty degeneration and the interval between injury and surgery after open repair.15 However, the risk factors for SSC retear after arthroscopic repair in isolated SSC and combined AS RCTs require further investigation.
The current study aimed to determine (1) whether the functional and radiological outcomes of isolated SSC RCTs are better than those of combined AS RCTs after arthroscopic repair; (2) the risk factors for SSC retear after arthroscopic repair in isolated SSC and combined AS RCTs; and (3) the incidence of high-grade fatty degeneration of the SSC muscle in these groups of patients and its association with the outcome.
Methods
Patient Enrollment
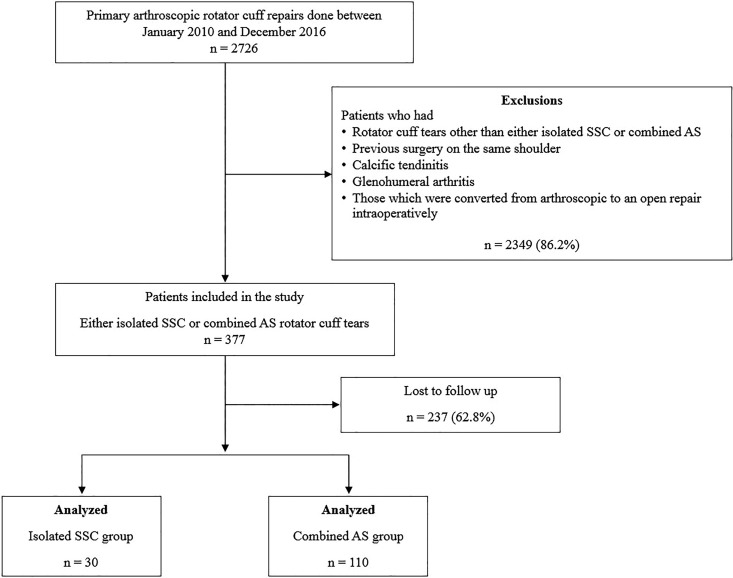
The prospectively collected data of 2726 patients who underwent primary rotator cuff repairs between January 2010 and December 2016 were retrospectively reviewed. Data collection and all protocols were approved by the institutional review board of the senior author’s (J.H.O.) institution. We included patients who had undergone arthroscopic repair for isolated SSC or combined AS RCTs during the study period. We excluded patients with RCTs other than isolated SSC or combined AS tears, patients who had undergone previous surgery on the same shoulder, patients with calcific tendinitis, patients with glenohumeral arthritis, and patients who had to be converted from arthroscopic to open repair intraoperatively. After assessment of the patient data according to the inclusion and exclusion criteria, 377 of 2726 patients (13.8%) who underwent rotator cuff repair for isolated SSC (n = 38) and combined AS (n = 339) RCTs were included in this study. Subsequently, 237 of the 377 patients (62.8%) were lost to a minimum 2-year follow-up in terms of functional and radiological outcomes, and their data were not analyzed. Hence, 30 patients in the isolated SSC group and 110 in the combined AS group were included for final analysis (Figure 1).
Figure 1.
Flowchart showing the patient enrollment in the study. AS, anterosuperior; SSC, subscapularis.
The mean follow-up period was 26.7 months (range, 24-96 months). Baseline characteristics of the 2 groups are provided in Table 1. Patients in the isolated SSC group were younger than those in the combined AS group (59.3 ± 8.9 vs 62.5 ± 7.3 years, respectively; P = .044), and the isolated SSC group had a higher proportion of male patients than the combined AS group (73.3% vs 47.3%, respectively; P = .020). The history of trauma was 56.7% in the isolated SSC group and 40.9% in the combined AS group, which was not statistically significant (P = .180). Fatty degeneration of the rotator cuff muscles on preoperative magnetic resonance imaging (MRI) was assessed with the Fuchs et al16 modification of the Goutallier et al19 classification scheme. The Fuchs classification was dichotomized as favorable (Goutallier grades 0, 1, and 2) or unfavorable (Goutallier grades 3 and 4) for the purpose of statistical evaluation in the current study. Furthermore, the coracohumeral distance (CHD) during internal rotation was noted in all patients, which was measured preoperatively by use of dynamic ultrasonography.48 The radiological parameters were evaluated by a musculoskeletal radiologist with 18 years of experience who was blinded to the details of the present study.
Table 1.
Baseline Characteristics of Patientsa
| Variables | Isolated SSC RCTs (n = 30) |
Combined AS RCTs (n = 110) |
P Value |
|---|---|---|---|
| Age, y | 59.3 ± 8.9 (43-77) | 62.5 ± 7.3 (37-82) | .044 |
| Male:female, n (% male) | 22:8 (73.3) | 58:52 (47.3) | .024 |
| Onset, mo | 9.7 ± 3.9 | 11.5 ± 3.1 | .471 |
| Body mass index, kg/m2 | 24.2 ± 4.4 (19.3-28.1) | 23.5 ± 3.2 (18.1-26.6) | .781 |
| History of trauma, n (%) | 17 (56.7) | 45 (40.9) | .183 |
| History of smoking, n (%) | 6 (20) | 26 (23.6) | .681 |
| Surgery on dominant hand, n (%) | 21 (70) | 81 (73.6) | .554 |
| Physical examinations, n (%) | |||
| Positive bear hug test | 25 (83.3) | 91 (82.7) | .881 |
| Positive belly press test | 19 (63.3) | 65 (59.1) | .699 |
| Positive internal rotation lag sign | 7 (23.3) | 38 (34.5) | .544 |
| Positive liftoff test | 7 (23.3) | 34 (30.9) | .671 |
| Tear retraction of SSC, mm | 19.9 ± 10.4 (5-50) | 13.3 ± 5.6 (5-35) | <.001 |
| Superoinferior tear dimension of SSC, mm | 19.6 ± 1.5 (5-50) | 11.8 ± 5.4 (5-35) | <.001 |
| Tear pattern of SSC, n (%) | |||
| Lafosse type II | 1 (3.3) | 6 (5.5) | .625 |
| Lafosse type III | 3 (10) | 80 (72.7) | <.001 |
| Lafosse type IV | 26 (86.7) | 24 (21.8) | .001 |
| Coracohumeral distance, mm | 11.0 ± 5.1 (0.8-19) | 8.1 ± 3.2 (0.3-17.4) | .001 |
| Patients receiving coracoplasty, n (%) | 6 (20) | 21 (19) | .998 |
aData are presented as mean ± SD (range) unless otherwise specified. AS, anterosuperior; RCT, rotator cuff tear; SSC, subscapularis.
Surgical Procedure and Rehabilitation
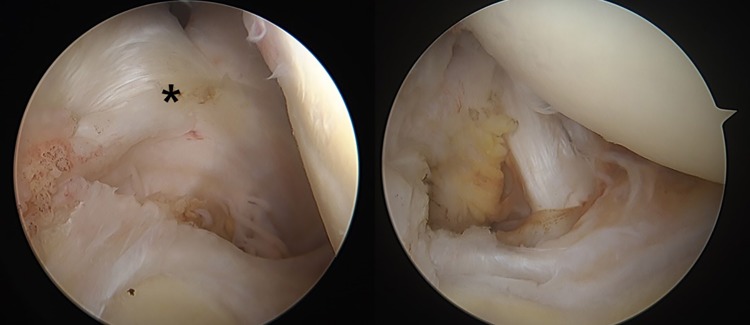
All procedures were performed arthroscopically by a senior surgeon (J.H.O.) who has been performing arthroscopic rotator cuff surgeries for more than 10 years. Patients were placed in the lateral decubitus position under general anesthesia. An arm traction device (Spider limb positioner; Smith & Nephew) was applied to the arm of the patient. The comma sign, which has been described37 as a comma-shaped arc in the superior glenohumeral ligament seen in patients with SSC tear, was recorded during diagnostic arthroscopy (Figure 2). After assessment of intra-articular lesions using the posterior portal as the viewing portal, the arthroscope was inserted into the subacromial space, and the anterior and AS lateral portals were used as working portals. Subacromial decompression and acromioplasty were performed in patients in the combined AS group if they had any evidence of subacromial or outlet impingement. Coracoplasty was performed in patients with a CHD less than 6 mm to allow an anterior working area for the SSC tendon repair and prevent possible abrasion to protect the repair.1,48 Notably, the mean CHD was greater in the isolated SSC group than in the combined AS group (11.0 ± 5.1 vs 8.1 ± 3.2 mm, respectively; P = .001). However, the proportion of patients in whom coracoplasty was performed was comparable in both groups (isolated SSC, 6 [20%]; combined AS, 21 [19%]; P = .990) (Table 1).
Figure 2.
The comma sign (asterisk) was found and recorded. The comma sign disappeared after arthroscopic subscapularis repair (right).
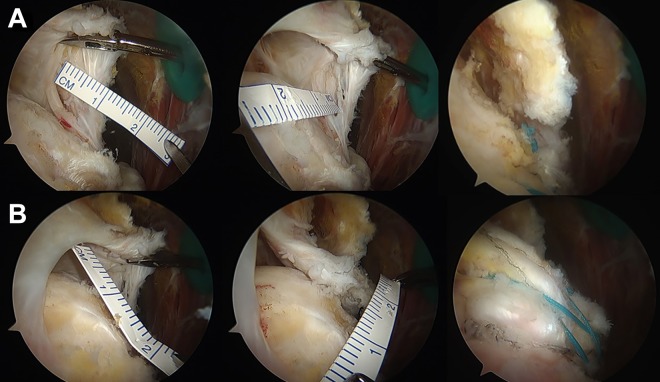
Inflamed bursal tissues and adhesions were removed, and debridement was performed at the edge of the torn cuff. The superoinferior and anteroposterior dimensions were measured for an SSC tear through use of a calibrated probe or plastic flexible ruler (Figure 3). The tear dimensions were measured in terms of retraction and anteroposterior dimension for a supraspinatus tear (Figure 3). The type of SSC tear was noted as per the classification proposed by Lafosse et al.32 The bleeding surface of tuberosities was prepared to enhance bone-to-tendon healing. Typically, in combined tears, the SSC was repaired first and then the supraspinatus. A single-row technique was performed as the standard procedure for SSC tendon repair (Figure 3). Supraspinatus tendon repair in the combined AS group was performed via a modified Mason-Allen suture technique for small RCTs (≤1 cm), a double-row suture bridge technique was used for medium to large RCTs (>1 cm to <3 cm), and a single-row repair was performed in patients who had massive tears (≥3 cm) in which torn tendon mobilization was limited to the medial part of the footprint (Figure 3). If the torn end of the rotator cuff tendon could not be attached to the footprint, intra- and extra-articular muscle releases were performed to allow for greater mobilization of the tendon. In cases where the torn tendon could not be attached to the footprint even with sufficient medial muscle release, footprint medialization up to 1 cm was performed by denuding the cartilage from the corresponding lateral articular surface of humerus.
Figure 3.
Arthroscopic views of the right shoulder by posterior portal. (A) The anterior to posterior tear size of the subscapularis was measured from the lateral wall of the lesser tuberosity to the retracted tendon. The superior to inferior tear size was measured from the margin of the bicipital groove to the inferior margin of the torn tendon. (B) The retraction of the tendon of supraspinatus was measured from the lateral wall of the greater tuberosity to the retracted tendon. The anterior to posterior tear size was measured from the margin of the bicipital groove to the posterior margin of the torn tendon.
The senior surgeon typically used 1 or 2 anchors for SSC repair. For supraspinatus repair, 1 to 4 nonmetallic anchors, either polyether ether ketone (PEEK), poly (l-lactic acid) (PLLA), or beta tricalcium phosphate (TCP) anchors, were used depending on the size of the tear (small tear, 1 anchor; medium tear, 2 anchors; large to massive tear, 3 or 4 anchors). Additionally, 2 anchors were used for the lateral row when performing a double-row suture bridge for supraspinatus repair. For the single-row repair or the medial row of a double-row suture bridge, we used 4.5-mm suture anchors made of PEEK, PLLA, or beta TCP material that had a nonabsorbable, braided, uncoated, ultra high–molecular weight polyethylene suture (CrossFT, ConMed Linvatec; Megasuture, ARC; and Healix Advance, Depuy Synthes), and a Samsung Medical Center knot configuration was used.26 When a double-row suture bridge was performed, the lateral row was fixed by a 5.5-mm anchor made of PEEK (Reelx STT; Stryker). For patients with bicipital groove tenderness and concomitant biceps abnormality, biceps tenodesis was performed in those who wanted to preserve supination strength; otherwise, biceps tenotomy was performed.47
Postoperatively, shoulders were immobilized with a brace for 4 to 6 weeks according to tear size. Shrugging of both shoulders, active elbow flexion-extension, active forearm supination-pronation, and active hand and wrist motion were encouraged immediately after surgery. Early passive range of motion (ROM) exercise was restricted during the brace-wearing period. After weaning from the brace, active and active-assisted shoulder ROM exercises were conducted for the next 5 to 6 weeks. If patients achieved satisfactory shoulder ROM, muscle strengthening exercises were started 9 to 12 weeks after surgery. Athletic activities were usually allowed 6 months postoperatively.
Outcome Assessment
Patients were asked to rate their postoperative pain and satisfaction using a 10-point visual analog scale (VAS); scores at the final follow-up visit were noted. Similarly, the American Shoulder and Elbow Surgeons (ASES) score,28 Simple Shoulder Test (SST) score,18 and Constant score11 were recorded at the final follow-up visit by a trained researcher who was blinded to the details of this study. The radiological outcomes in terms of tendon integrity were assessed with MRI at 1 year after the surgery. However, for patients who had implanted MRI-incompatible devices including pacemakers or who refused MRI because of its high cost, computed tomography arthrogram (CTA) or ultrasonography was utilized instead.
Statistical Analysis
All statistical analyses were performed with SPSS software (Version 21.0; IBM), and a P value less than .050 was considered significant. When the distribution of data was normal, independent t tests were used to evaluate the differences of outcomes in the 2 groups, and paired t tests were used to compare pre- and postoperative variables in a group. Patient demographics were analyzed with the chi-square test for categorical variables to assess differences between the 2 groups. Univariate logistic regression analysis was used to assess the risk factors for retear in both the groups.
Results
The mean SSC tear retraction (19.9 ± 10.4 vs 13.3 ± 5.6 mm; P < .001) and the superoinferior tear dimension (19.6 ± 11.5 vs 11.8 ± 5.4 mm; P < .001) were greater in the isolated SSC group than in the combined AS group. Similarly, the proportion of patients with a Lafosse type IV SSC tear was higher (86.7% vs 21.8%; P = .001) in the isolated SSC group (Table 1). The incidence of unfavorable fatty degeneration (Goutallier grades 3 and 4) in the SSC was similar in both groups (10.0% vs 13.3% in the isolated SSC vs combined AS groups; P = .630). However, none of the patients in the isolated SSC group had unfavorable fatty degeneration of the supraspinatus muscle, whereas 23.3% of patients in the combined AS group had unfavorable fatty degeneration (P = .003) (Table 2).
Table 2.
Incidence of Unfavorable (Goutallier Grades 3 and 4) Fatty Degeneration on Preoperative Magnetic Resonance Imaginga
| Isolated SSC RCTs (n = 30) |
Combined AS RCTs (n = 110) |
P Value | |
|---|---|---|---|
| Subscapularis | 3 (10) | 14 (13.3) | .630 |
| Supraspinatus | 0 (0) | 24 (23.3) | .003 |
| Infraspinatus | 0 | 1 | .588 |
| Teres minor | 0 | 0 | — |
aData are presented as n (%). Dash indicates statistical analysis need not be performed. AS, anterosuperior; RCT, rotator cuff tear; SSC, subscapularis.
In the isolated SSC group, forward flexion was improved from 133.4° ± 18.3° to 161.3° ± 14.1°, external rotation from 48.2° ± 8.9° to 65.1° ± 11.3°, and internal rotation from thoracic vertebra level (T) 12.3 ± 2.2 to T 8.4 ± 1.7 (P = .003, .002, and .001, respectively). In the combined AS group, forward flexion improved from 144.7° ± 29.3° to 157.3° ± 21.5°, external rotation from 51.1° ± 13.2° to 64.6° ± 13.8°, and internal rotation from T 11.7 ± 2.4 to T 8.6 ± 1.3 (P = .005, <.001, and <.001, respectively). However, improved ROM at the final follow-up in both groups showed no statistical difference (all P > .05).
The clinical outcomes in terms of the VAS for pain and satisfaction, ASES, and SST scores were comparable in both groups (Table 3). At the final follow-up, the Constant score was higher in the isolated SSC group than in the combined group (73.6 vs 71.1; P = .030); however, this difference was not clinically significant.30 No postoperative neurovascular complications occurred in any of the patients in this study. There were 2 patients (2/30; 6.7%) in the isolated SSC group and 8 patients (8/110; 7.3%) in the combined AS group who had persistent joint stiffness at final follow-up. Radiological outcomes at final follow-up were available in a total of 136 patients: 28 in the isolated SSC group (11 MRI and 17 ultrasonography) and 108 in the combined AS group (81 MRI, 3 CTA, and 24 ultrasonography). SSC retear at 1 year postoperative was observed in 14 (10.4%) of these 136 patients, which was comparable in the isolated SSC and combined AS groups (5 [16.7%] vs 9 [8.5%], respectively; P = .337). In the combined AS group, supraspinatus retear was observed in 21 patients (19.1%), and 4 patients (3.6%) had retear of both the supraspinatus and the SSC tendons.
Table 3.
Clinical Outcomes at the Final Follow-up Visita
| Isolated SSC RCTs | Combined AS RCTs | P Value | |
|---|---|---|---|
| Pain VAS | 0.5 ± 1.2 | 1.3 ± 2.5 | .093 |
| Satisfaction VAS | 8.5 ± 2.1 | 8.8 ± 1.6 | .405 |
| ASES score | 93.7 ± 8.9 | 92.0 ± 13.6 | .517 |
| SST score | 10.7 ± 1.6 | 10.9 ± 2.1 | .637 |
| Constant score | 73.6 ± 5.5 | 71.1 ± 5.6 | .033 |
aData are presented as mean ± SD. AS, anterosuperior; ASES, American Shoulder and Elbow Surgeons; RCT, rotator cuff tear; SSC, subscapularis; SST, Simple Shoulder Test; VAS, visual analog scale.
The numbers of patients with retears in the isolated SSC (n = 5) and combined AS (n = 9) groups were too small to draw definitive conclusions from their comparison. Nonetheless, the proportion of patients with a Lafosse type IV tear was higher in the isolated SSC group compared with the combined AS group preoperatively (100% vs 44.4%; P = .037). Additionally, the preoperative retraction size of the torn SSC was greater in the isolated SSC group than in the combined AS group (28.6 ± 15 vs 14.8 ± 4.7 mm, respectively; P = .022). Similarly, superoinferior tear dimensions of the SSC were greater in the isolated SSC group than in the combined AS group (26.0 ± 9.6 vs 14.7 ± 4.8 mm, respectively; P = .012). In terms of clinical outcomes, only the VAS for satisfaction differed between groups (6.0 ± 3.9 in the isolated SSC group vs 9.6 ± 0.7 in the combined AS group; P = .019), but with the numbers available, no other comparisons reached significance (Table 4).
Table 4.
Comparison of Patients With Retears Between Both Groups in Terms of Tear Characteristics and Functional Outcomesa
| Isolated SSC RCTs (n = 5) |
Combined AS RCTs (n = 9) |
P Value | |
|---|---|---|---|
| Patients with Lafosse tear type IV, n (%) | 5 (100) | 4 (44.4) | .037 |
| Tear retraction of SSC, mm | 28.6 ± 15 | 14.8 ± 4.7 | .022 |
| Superoinferior tear dimensions of SSC, mm | 26 ± 9.6 | 14.7 ± 4.8 | .012 |
| Coracohumeral distance, mm | 13.3 ± 4.4 | 10.3 ± 5 | .369 |
| Patients with preoperative unfavorable fatty degeneration of SSC, n (%) | 3 (60) | 4 (44.4) | .557 |
| Pain VAS | 1 ± 2.2 | 0.8 ± 1.3 | .823 |
| Satisfaction VAS | 6 ± 3.9 | 9.6 ± 0.7 | .019 |
| ASES score | 86.3 ± 16.1 | 94.3 ± 5.4 | .191 |
| Simple Shoulder Test score | 9 ± 2.5 | 11 ± 2 | .128 |
| Constant score | 68.2 ± 5.4 | 69.9 ± 5.2 | .576 |
aData are presented as mean ± SD unless otherwise specified. AS, anterosuperior; ASES, American Shoulder and Elbow Surgeons; RCT, rotator cuff tear; SSC, subscapularis; VAS, visual analog scale.
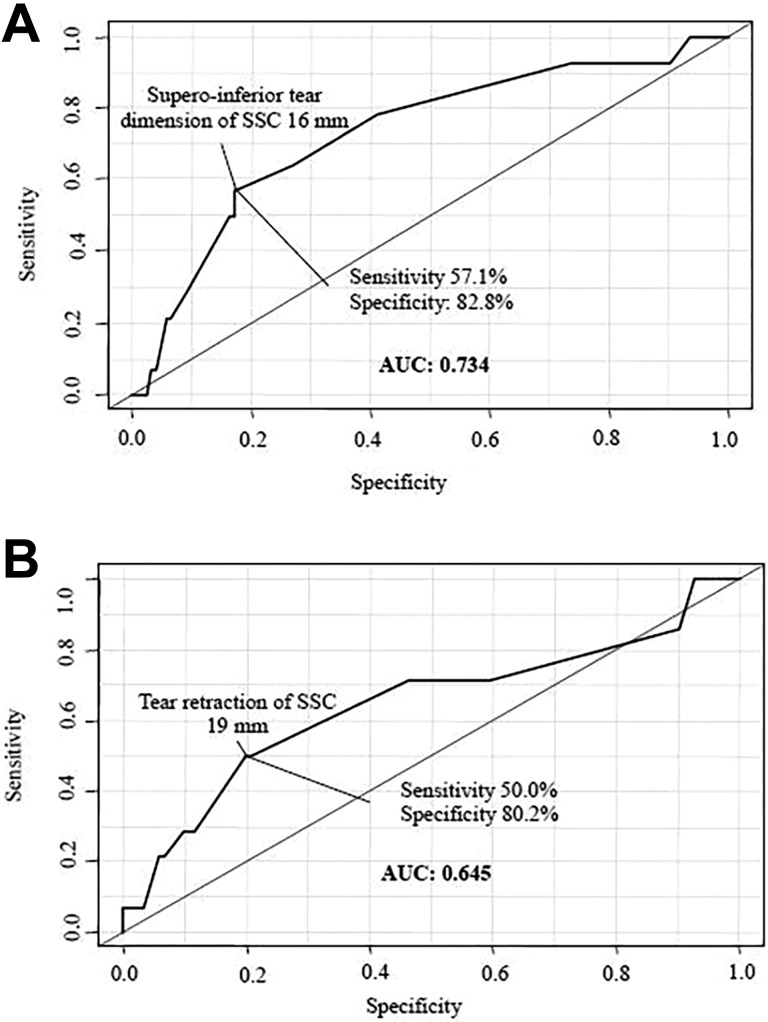
The univariate regression analysis for retear in both groups indicated that SSC tear retraction (odds ratio [OR], 1.1; P = .016) and the superoinferior tear dimension (OR, 1.1; P = .014) were significant risk factors for retear (Table 5). Additionally, patients with a Lafosse type IV SSC tear were at a higher risk of retear of the SSC tendon (OR, 5.1; P = .009). Preoperative unfavorable fatty degeneration in the SSC muscle was found to be a significant risk factor for SSC retear in both groups (OR, 9.8; P < .001). When we assessed the optimal cutoff tear size for risk of SSC retear (Figure 4), the area under the curve showed a tear retraction of 19 mm (sensitivity, 50%; specificity, 80%) and superoinferior tear dimension of 16 mm (sensitivity, 57.1%; specificity, 82.8%).
Table 5.
Risk Factors for Retear of the Subscapularis According to Univariate Regression Analysisa
| Intact Tendon (n = 122) |
Retear (n = 14) |
Odds Ratio | P Value | |
|---|---|---|---|---|
| Age, y | 61.4 ± 7.9 | 64.1 ± 6.6 | 1.1 | .215 |
| Male:female (% male) | 63:59 (51.6) | 9:5 (64.3) | 0.6 | .373 |
| Tear retraction of SSC, mm | 14.2 ± 6.7 | 19.7 ± 11.4 | 1.1 | .016 |
| Superoinferior tear dimension of SSC, mm | 12.9 ± 7.6 | 18.8 ± 8.6 | 1.1 | .014 |
| Patients with Lafosse type IV, n (%) | 40 (32.8) | 10 (71.4) | 5.1 | .009 |
| Pain VAS | 1.0 ± 2.1 | 0.9 ± 1.59 | 1.0 | .878 |
| Satisfaction VAS | 8.9 ± 1.5 | 8.3 ± 2.9 | 0.9 | .237 |
| ASES score | 92.3 ± 13.2 | 91.4 ± 10.6 | 1.0 | .807 |
| Simple Shoulder Test score | 10.9 ± 2 | 10.3 ± 2.3 | 0.9 | .325 |
| Constant score | 71.8 ± 5.8 | 69.3 ± 5.1 | 0.9 | .122 |
aData are presented as mean ± SD unless otherwise specified. ASES, American Shoulder and Elbow Surgeons; SSC, subscapularis; VAS, visual analog scale.
Figure 4.
Receiver operating characteristic curve to determine the optimal cutoff tear size for risk of subscapularis (SSC) retear: (A) tear retraction of 19 mm (specificity, 80%) and (B) superoinferior tear dimension of 16 mm (specificity, 82.8%). Specificity signifies the number of retear cases under that size per the total number of healing successful cases. AUC, area under the curve.
Discussion
The present study demonstrated that patients with isolated SSC RCTs were younger with a similar incidence of trauma in addition to worse tear characteristics and similar clinical and radiological outcomes compared with the patients with combined AS RCTs. Additionally, in patients with SSC tendon retear, worse tear characteristics were observed in patients with isolated SSC RCTs, although they showed similar clinical outcomes to patients with combined AS RCTs. Finally, SSC tear retraction and superoinferior dimension in addition to preoperative high-grade fatty degeneration in the SSC were significant risk factors for SSC tendon retear in the patients with isolated SSC and combined AS RCTs.
Regarding the demographic characteristics of RCTs that involved the SSC, the patients with isolated SSC RCTs were younger and predominantly male. The observation that patients with isolated SSC RCTs tended to be younger was consistent with the results of a previous study.29 However, the age of both isolated SSC and combined AS tear patients was reported to be similar in other studies.17,24 The incidence of male predominance in RCTs involving the SSC has been reported in several previous studies that considered both isolated and combined AS RCTs.15,17,24,29 Moreover, the comparative results in our study suggest that the male predominance was present only in the isolated SSC group, whereas the combined AS group had a similar proportion of male and female patients.
The incidence of trauma in patients with a tear that involved the SSC was not statistically different between isolated SSC and combined AS RCT patients in the current study; a relatively high proportion of patients (isolated SSC group, 56.7%; combined AS group, 40.9%) recalled a trauma-related history for symptom onset. These findings are in line with previous studies evaluating the incidence of trauma in 46% to 83% of patients with isolated SSC RCTs14,24,39,50,53 and 47% to 73% of patients with combined AS RCTs.4,44 In contrast, a history of trauma was reported in a relatively low proportion of patients with isolated supraspinatus tears (27.1% in the study by Collin et al10) and isolated infraspinatus tears (16.6% in the study by Lee et al36). This probably indicates that the incidence of trauma would be more prevalent in both patients with isolated SSC tear and patients with combined supraspinatus and SSC tears.
Tear characteristics in terms of tear retraction and superoinferior tear dimensions were worse in the isolated SSC group in the present study. In contrast, Gerhardt et al17 reported that only a small number of patients with isolated SSC RCTs showed complete rupture of the SSC tendon (10.0%) compared with patients who had combined AS RCTs (22.9%). However, unlike our study, Gerhardt et al included patients with partial-thickness SSC tears for whom debridement was performed, which may have led to the difference in findings. A possible explanation for the lesser superoinferior tear dimension of SSC tears in the combined AS group in our study may be due to the intact rotator cuff cable in these patients, which prevents further progression of the SSC tear as the force couple is relatively balanced.8 However, further studies regarding the pattern of tear progression are required to confirm the difference in the SSC tear dimensions between isolated SSC and combined AS RCTs.
In the literature, the correlation between CHD and SSC tears is unclear. Lo and Burkhart38 proposed a correlation between narrowed coracohumeral space and SSC tendon tears via a mechanism called the “roller-wringer effect”; they defined subcoracoid stenosis as a CHD less than 6 mm. Similarly, Richards et al51 reported that the CHD was significantly narrowed in patients with a torn SSC. In contrast, Bergin et al7 reported no significant relationship between the measured subcoracoid interval on the axial MRI image and the severity of the SSC tendon abnormality. Similarly, another clinical study did not find any correlation between CHD and SSC tear, although the investigators did observe a significantly greater incidence of SSC tears in patients with dynamic subcoracoid stenosis (CHD <6 mm in internal rotation and flexion).48 In the current study, we did not find any correlation between the narrowed CHD and poor tear characteristics of the SSC, as the CHD was wider in isolated SSC patients whose tear characteristics were worse. Furthermore, a narrowed CHD was found in 19.0% of patients in our study compared with 43.0% in a previous study, which included patients with SSC tears who underwent arthroscopic repair.1 These findings may be explained by the high proportion of patients with a history of trauma in the current study, whereas narrowed CHD was shown to be associated with degenerative SSC tears.2
The postoperative clinical outcomes in terms of VAS for pain and satisfaction, ASES score, SST score, and Constant score were similar in both groups in the current study, which is consistent with the findings of studies assessing open repair,15 arthroscopic debridement and repair,17 and arthroscopic repair.24 In contrast, Kreuz et al29 reported better Constant score in the patients with isolated SSC RCTs after open repair, which was attributed to reduced postoperative abduction, longer delay between trauma and definitive treatment, a relatively older patient group (45 vs 55 years), and a more invasive procedure in the patients with combined AS RCTs. The similar clinical outcomes in our study may be explained by the similar patient age and incidence of preoperative unfavorable muscle fatty degeneration in both patient groups as well as the repair being performed arthroscopically, which may have mitigated the invasiveness in patients with combined AS RCTs.
The current data showed no significant difference in the rate of SSC retear after arthroscopic repair in isolated SSC (16.7%) and combined AS (8.5%) tear patients. In contrast, Jeong et al24 reported no retear in isolated SSC patients but an 8.8% rate of SSC retear in combined AS patients at a minimum follow-up of 2 years. Notably, the rate of SSC retear in all patients in our study (10.4%) was similar to that previously reported by Flury et al15 (13.0%). The characteristics of SSC tears, including more retraction, the superoinferior dimension, and Lafosse type IV tears, were significant risk factors for SSC retear. Warner et al55 suggested that SSC tear size was a risk factor for poor clinical outcomes after combined AS tears. In contrast, Maqdes et al42 and Bartl et al4 reported no difference in the clinical outcomes due to SSC tear size. Furthermore, previous studies have reported good to excellent functional results with acceptable rates of tendon healing after arthroscopic repair in patients with Lafosse type III and IV isolated SSC or combined AS lesions.21,33 Nonetheless, to the best of our knowledge, the optimal cutoff values for risk of retear of the repaired SSC in terms of tear dimensions (19-mm retraction and 16-mm superoinferior dimension) have not been previously reported.
In terms of repair technique, all patients in this study underwent single-row fixation for SSC repair, which has been shown to have favorable results in previous studies.2,22,24 In contrast, another study indicated that the double-row repair technique for SSC tears may give better outcomes in higher grade tears.21 Nonetheless, future prospective, comparative studies are needed to determine whether single- or double-row fixation provides better clinical and radiological outcomes after SSC RCT repair.52 Regarding postoperative physical management, all of the patients in the current study were immobilized for 4 to 6 weeks with restriction of passive ROM, similar to previous reports that focused on tears that involved the SSC.1,50 However, authors of some previous studies allowed passive mobilization during the first 6 weeks while active movements were restricted.3,15 Evidence is lacking regarding the optimum postoperative rehabilitation protocol after repairs of RCTs involving the SSC, a topic that requires further comparative studies in the future.
The current data suggest that grade 3 and 4 fatty degeneration in the SSC muscle on the preoperative MRI was a risk factor for retear, which is consistent with findings of previous studies.15,42 These results further strengthen the prognostic importance of the preoperative assessment of fatty infiltration of the SSC muscle in patients with SSC tear. Flury et al15 reported a 50% rerupture rate of the SSC in patients with grade 3 fatty degeneration and recommended that direct reinsertion of the SSC is unacceptable in patients with grade 3 and 4 fatty degeneration in the SSC. We believe that studies comparing the outcomes of different treatment modalities in patients with high-grade SSC fatty degeneration are needed to allow recommendations regarding the treatment of choice in such cases. We must also note that among the 4 patients with supraspinatus and SSC tendon retear, 3 patients had unfavorable fatty degeneration of the supraspinatus preoperatively.
Our study has certain limitations that must be considered. First, the study design was retrospective in nature. Second, of the 377 patients who were included in the study, only 140 patients with 2-year follow-up data could be analyzed. Third, the preoperative delay between the onset of symptoms and surgery might have led to progression of fatty degeneration, which could adversely affect the outcomes of surgery. However, the correlation between such a preoperative delay and the progression of fatty degeneration was not determined in the current study. Fourth, the findings of pre- and postoperative physical examination and quantitative muscle strength are not reported in the current study; such findings would have allowed better comparison and correlation of outcome variables between the 2 groups. Fifth, the mean follow-up of the patient cohort available in the current study (26.7 months) was short. Sixth, the radiological outcome was not available in all patients, which might have contributed to the selection bias. Furthermore, the postoperative radiological outcomes were evaluated using ultrasonography instead of an advanced imaging technique such as MRI in some patients. However, previous studies have shown ultrasonography to be accurate for the assessment of shoulder abnormality after surgery.49 Additionally, ultrasonography and CTA have been shown to be comparable with MRI for evaluating repaired rotator cuff status.9,34,46 Seventh, the repair integrity on follow-up radiological imaging was not evaluated using the Sugaya classification, which could have enabled better correlation with clinical outcomes.54
Nonetheless, this study has certain strengths. To the best of our knowledge, we have evaluated the largest cohort of patients who underwent arthroscopic repair for isolated SSC and combined AS RCTs reported in the literature so far. Furthermore, we compared the clinical outcomes in both groups using ASES and SST scores, unlike previous similar studies that used only the Constant score.15,17,29 Finally, the unique findings of this study are the optimal cutoff values for the risk of retear of the repaired SSC in terms of tear dimensions, which have not been reported previously.
Conclusion
Isolated SSC and combined AS tear groups were comparable except for patient age and sex; both had a high incidence of traumatic history. The current data suggest that the risk factors for retear after SSC repair in RCTs involving the SSC were a tear size greater than 19 mm of retraction and unfavorable fatty degeneration (grade 3 or higher) of the SSC muscle.
Footnotes
Final revision submitted September 23, 2019; accepted October 9, 2019.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Seoul National University Bundang Hospital Institutional Review Board (No. B-1901/517-102).
References
- 1. Adams CR, Schoolfield JD, Burkhart SS. The results of arthroscopic subscapularis tendon repairs. Arthroscopy. 2008;24(12):1381–1389. [DOI] [PubMed] [Google Scholar]
- 2. Balke M, Banerjee M, Greshake O, Hoeher J, Bouillon B, Liem D. The coracohumeral distance in shoulders with traumatic and degenerative subscapularis tendon tears. Am J Sports Med. 2016;44(1):198–201. [DOI] [PubMed] [Google Scholar]
- 3. Bartl C, Salzmann GM, Seppel G, et al. Subscapularis function and structural integrity after arthroscopic repair of isolated subscapularis tears. Am J Sports Med. 2011;39(6):1255–1262. [DOI] [PubMed] [Google Scholar]
- 4. Bartl C, Senftl M, Eichhorn S, Holzapfel K, Imhoff A, Salzmann G. Combined tears of the subscapularis and supraspinatus tendon: clinical outcome, rotator cuff strength and structural integrity following open repair. Arch Orthop Trauma Surg. 2012;132(1):41–50. [DOI] [PubMed] [Google Scholar]
- 5. Bennett WF. Arthroscopic repair of anterosuperior (supraspinatus/subscapularis) rotator cuff tears. Arthroscopy. 2003;19(1):21–33. [DOI] [PubMed] [Google Scholar]
- 6. Bennett WF. Arthroscopic repair of isolated subscapularis tears: a prospective cohort with 2- to 4- year follow-up. Arthroscopy. 2003;19:131–143. [DOI] [PubMed] [Google Scholar]
- 7. Bergin D, Parker L, Zoga A, Morrison W. Abnormalities on MRI of the subscapularis tendon in the presence of a full-thickness supraspinatus tendon tear. Am J Roentgenol. 2006;186:454–459. [DOI] [PubMed] [Google Scholar]
- 8. Burkhart SS. Reconciling the paradox of rotator cuff repair versus debridement: a unified biomechanical rationale for the treatment of rotator cuff tears. Arthroscopy. 1994;10(1):4–19. [DOI] [PubMed] [Google Scholar]
- 9. Charousset C, Bellaiche L, Duranthon LD, Grimberg J. Accuracy of CT arthrography in the assessment of tears of the rotator cuff. J Bone Joint Surg Br. 2005;87:824–828. [DOI] [PubMed] [Google Scholar]
- 10. Collin P, Kempf JF, Molé D, et al. Société Française de Chirurgie Orthopédique et Traumatologique (SoFCOT). Ten-year multicenter clinical and MRI evaluation of isolated supraspinatus repairs. J Bone Joint Surg Am. 2017;99(16):1355–1364. [DOI] [PubMed] [Google Scholar]
- 11. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 12. Denard PJ, Jiwani AZ, Lädermann A, Burkhart SS. Long-term outcome of a consecutive series of subscapularis tendon tears repaired arthroscopically. Arthroscopy. 2012;28(11):1587–1591. [DOI] [PubMed] [Google Scholar]
- 13. Edwards TB, Walch G, Nové-Josserand L, et al. Arthroscopic debridement in the treatment of patients with isolated tears of the subscapularis. Arthroscopy. 2006;22(9):941–946. [DOI] [PubMed] [Google Scholar]
- 14. Edwards TB, Walch G, Sirveaux F, et al. Repair of tears of the subscapularis. J Bone Joint Surg Am. 2005;87(4):725–730. [DOI] [PubMed] [Google Scholar]
- 15. Flury MP, John M, Goldhahn J, Schwyzer HK, Simmen BR. Rupture of the subscapularis tendon (isolated or in combination with supraspinatus tear): when is a repair indicated? J Shoulder Elbow Surg. 2006;15(6):659–664. [DOI] [PubMed] [Google Scholar]
- 16. Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8:599–605. [DOI] [PubMed] [Google Scholar]
- 17. Gerhardt C, Bartl C, Voigt C, et al. Recovery of subscapularis and shoulder function following arthroscopic treatment of isolated anterior and combined anterosuperior rotator cuff lesions. Arch Orthop Trauma Surg. 2016;136(1):75–81. [DOI] [PubMed] [Google Scholar]
- 18. Godfrey J, Hamman R, Lowenstein S, Briggs K, Kocher M. Reliability, validity, and responsiveness of the simple shoulder test: psychometric properties by age and injury type. J Shoulder Elbow Surg. 2007;16(3):260–267. [DOI] [PubMed] [Google Scholar]
- 19. Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12:550–554. [DOI] [PubMed] [Google Scholar]
- 20. Gray H, Clemente CD. Anatomy of the Human Body. 30th American ed Philadelphia, PA: Lea & Febiger; 1985. [Google Scholar]
- 21. Grueninger P, Nikolic N, Schneider J, et al. Arthroscopic repair of traumatic isolated subscapularis tendon lesions (Lafosse type III or IV): a prospective magnetic resonance imaging-controlled case series with 1 year of follow-up. Arthroscopy. 2014;30:665–672. [DOI] [PubMed] [Google Scholar]
- 22. Heikenfeld R, Gigis I, Chytas A, Listringhaus R, Godolias G. Arthroscopic reconstruction of isolated subscapularis tears: clinical results and structural integrity after 24 months. Arthroscopy. 2012;28(12):1805–1811. [DOI] [PubMed] [Google Scholar]
- 23. Ide J, Tokiyoshi A, Hirose J, Mizuta H. Arthroscopic repair of traumatic combined rotator cuff tears involving the subscapularis tendon. J Bone Joint Surg Am. 2007;89(11):2378–2388. [DOI] [PubMed] [Google Scholar]
- 24. Jeong JY, Pan HL, Song SY, Lee SM, Yoo JC. Arthroscopic subscapularis repair using single-row mattress suture technique: clinical results and structural integrity. J Shoulder Elbow Surg. 2018;27(4):711–719. [DOI] [PubMed] [Google Scholar]
- 25. Keating JF, Waterworth P, Shaw-Dunn J, Crossan J. The relative strengths of the rotator cuff muscles: a cadaver study. J Bone Joint Surg Br. 1993;75(1):137–140. [DOI] [PubMed] [Google Scholar]
- 26. Kim SH, Ha KI. The SMC knot—a new slip knot with locking mechanism. Arthroscopy. 2000;16(5):563–565. [DOI] [PubMed] [Google Scholar]
- 27. Kim SH, Oh I, Park JS, Shin SK, Jeong WK. Intra-articular repair of an isolated partial articular-surface tear of the subscapularis tendon. Am J Sports Med. 2005;33(12):1825–1830. [DOI] [PubMed] [Google Scholar]
- 28. Kirkley A, Griffin S, Dainty K. Scoring systems for the functional assessment of the shoulder. Arthroscopy. 2003;19(10):1109–1120. [DOI] [PubMed] [Google Scholar]
- 29. Kreuz PC, Remiger A, Erggelet C, Hinterwimmer S, Niemeyer P, Gächter A. Isolated and combined tears of the subscapularis tendon. Am J Sports Med. 2005;33(12):1831–1837. [DOI] [PubMed] [Google Scholar]
- 30. Kukkonen J, Kauko T, Vahlberg T, Joukainen A, Aärimaa V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J Shoulder Elbow Surg. 2013;22(12):1650–1655. [DOI] [PubMed] [Google Scholar]
- 31. Lafosse L, Brozska R, Toussaint B, Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. J Bone Joint Surg Am. 2007;89:1533–1541. [DOI] [PubMed] [Google Scholar]
- 32. Lafosse L, Lanz U, Saintmard B, Campens C. Arthroscopic repair of subscapularis tear: surgical technique and results. Orthop Traumatol Surg Res. 2010;96(8):S99–S108. [DOI] [PubMed] [Google Scholar]
- 33. Lanz U, Fullick R, Bongiorno V, Saintmard B, Campens C, Lafosse L. Arthroscopic repair of large subscapularis tendon tears: 2- to 4-year clinical and radiographic outcomes. Arthroscopy. 2013;29:1471–1478. [DOI] [PubMed] [Google Scholar]
- 34. Lee E, Choi JA, Oh JH, et al. Fatty degeneration of the rotator cuff muscles on pre- and postoperative CT arthrography (CTA): is the Goutallier grading system reliable? Skeletal Radiol. 2013;42:1259–1267. [DOI] [PubMed] [Google Scholar]
- 35. Lee J, Shukla DR, Sánchez-Sotelo J. Subscapularis tears: hidden and forgotten no more. JSES Open Access. 2018;2(1):74–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lee KY, Kim SH, Oh JH. Isolated ruptures of the infraspinatus: clinical characteristics and outcomes. Clinics in Shoulder and Elbow. 2017;20(1):30–36. [Google Scholar]
- 37. Lo IK, Burkhart SS. The comma sign: an arthroscopic guide to the torn subscapularis tendon. Arthroscopy. 2003;19(3):334–337. [DOI] [PubMed] [Google Scholar]
- 38. Lo IK, Burkhart SS. The etiology and assessment of subscapularis tendon tears: a case for subcoracoid impingement, the roller-wringer effect, and TUFF lesions of the subscapularis. Arthroscopy. 2003;19:1142–1150. [DOI] [PubMed] [Google Scholar]
- 39. Mall NA, Chahal J, Heard WM, et al. Outcomes of arthroscopic and open surgical repair of isolated subscapularis tendon tears. Arthroscopy. 2012;28(9):1306–1314. [DOI] [PubMed] [Google Scholar]
- 40. Mall NA, Lee AS, Chahal J, et al. An evidenced-based examination of the epidemiology and outcomes of traumatic rotator cuff tears. Arthroscopy. 2013;29(2):366–376. [DOI] [PubMed] [Google Scholar]
- 41. Mancuso F, Di Benedetto P, Beltrame A, Cainero V, Causero A. Arthroscopic treatment of isolated subscapularis lesions: our experience. Acta Biomed. 2014;85:20–24. [PubMed] [Google Scholar]
- 42. Maqdes A, Abarca J, Moraiti C, et al. Does preoperative subscapularis fatty muscle infiltration really matter in anterosuperior rotator cuff tears repair outcomes? A prospective multicentric study. Orthop Traumatol Surg Res. 2014;100(5):485–488. [DOI] [PubMed] [Google Scholar]
- 43. Morag Y, Jamadar DA, Miller B, Dong Q, Jacobson JA. The subscapularis: anatomy, injury, and imaging. Skeletal Radiol. 2011;40(3):255–269. [DOI] [PubMed] [Google Scholar]
- 44. Nové-Josserand L, Collin P, Godenèche A, et al. SOFCOT. Ten-year clinical and anatomic follow-up after repair of anterosuperior rotator cuff tears: influence of the subscapularis. J Shoulder Elbow Surg. 2017;26(10):1826–1833. [DOI] [PubMed] [Google Scholar]
- 45. Nove-Josserand L, Hardy MB, Leandro Nunes Ogassawara R, Carrillon Y, Godeneche A. Clinical and structural results of arthroscopic repair of isolated subscapularis tear. J Bone Joint Surg Am. 2012;94:e125. [DOI] [PubMed] [Google Scholar]
- 46. Oh JH, Kim JY, Choi JA, Kim WS. Effectiveness of multidetector computed tomography arthrography for the diagnosis of shoulder pathology: comparison with magnetic resonance imaging with arthroscopic correlation. J Shoulder Elbow Surg. 2010;19:14–20. [DOI] [PubMed] [Google Scholar]
- 47. Oh JH, Lee YH, Kim SH, et al. Comparison of treatments for superior labrum-biceps complex lesions with concomitant rotator cuff repair: a prospective, randomized, comparative analysis of debridement, biceps tenotomy, and biceps tenodesis. Arthroscopy. 2016;32(6):958–967. [DOI] [PubMed] [Google Scholar]
- 48. Oh JH, Song BW, Choi JA, Lee GY, Kim SH, Kim DH. Measurement of coracohumeral distance in 3 shoulder positions using dynamic ultrasonography: correlation with subscapularis tear. Arthroscopy. 2016;32(8):1502–1508. [DOI] [PubMed] [Google Scholar]
- 49. Prickett WD, Teefey SA, Galatz LM, Calfee RP, Middleton WD, Yamaguchi K. Accuracy of ultrasound imaging of the rotator cuff in shoulders that are painful postoperatively. J Bone Joint Surg Am. 2003;85-A(6):1084–1089. [DOI] [PubMed] [Google Scholar]
- 50. Rhee YG, Lee YS, Park YB, Kim JY, Han KJ, Yoo JC. The outcomes and affecting factors after arthroscopic isolated subscapularis tendon repair. J Shoulder Elbow Surg. 2017;26(12):2143–2151. [DOI] [PubMed] [Google Scholar]
- 51. Richards DP, Burkhart SS, Campbell SE. Relation between narrowed coracohumeral distance and subscapularis tears. Arthroscopy. 2005;21(10):1223–1228. [DOI] [PubMed] [Google Scholar]
- 52. Saltzman BM, Collins MJ, Leroux T, et al. Arthroscopic repair of isolated subscapularis tears: a systematic review of technique-specific outcomes. Arthroscopy. 2017;33(4):849–860. [DOI] [PubMed] [Google Scholar]
- 53. Seppel G, Plath JE, Völk C, et al. Long-term results after arthroscopic repair of isolated subscapularis tears. Am J Sports Med. 2017;45(4):759–766. [DOI] [PubMed] [Google Scholar]
- 54. Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21(11):1307–1316. [DOI] [PubMed] [Google Scholar]
- 55. Warner JJ, Higgins L, Parsons IM IV, Dowdy P. Diagnosis and treatment of anterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2001;10(1):37–46. [DOI] [PubMed] [Google Scholar]