Abstract
Sexual minority men (SMM) who drink heavily are at a greater risk for developing alcohol use disorders (AUD) and associated negative consequences. Barriers to treatment prevent SMM from accessing traditional care, and moderation-based alcohol treatment is a more desirable alternative. As such, investigating effective goal setting in moderation-based alcohol treatment, particularly, which goals yield the most effective outcomes, is warranted. Applying the tenets of Goal Setting Theory, this study explored the relationship between goal difficulty and goal achievement. In a secondary data analysis of a randomized controlled trial that delivered a combination of medication (i.e., naltrexone) and behavioral (i.e., Modified Behavioral Self-Control Training) treatment for SMM with AUD (N = 178), generalized estimating equations tested the effect of goal difficulty (defined as the proposed magnitude of change from current drinking in number of drinking days and number of heavy drinking days) on goal achievement at Months 0, 3, 6, and 9. Goal importance, self-efficacy, and AUD severity were tested as moderators. Findings yielded a significant positive relationship between goal difficulty and goal achievement for number of drinking days but a negative relationship for the number of heavy drinking days. Moderators of these relationships were not found. In order to increase the likelihood of achieving their goals in moderation-based alcohol treatment, SMM should initially consider setting more difficult goals for reducing drinking days. Additionally, goals of more conservative difficulty should be set for reducing heavy drinking days.
Keywords: alcohol use disorders, alcohol treatment, moderation, goal setting, goal setting theory, sexual minority men
1. AUD among Sexual Minority Men
Alcohol use disorders (AUD) are a public health concern among sexual minority men (SMM)—that is, gay, bisexual, and other men who are attracted to or have sex with men (Cochran & Cauce, 2006; Irwin, Morgenstern, Parsons, Wainberg, & Labouvie, 2006; Patterson, David, Hall, & Golder, 2009; Stall et al., 2001; Wray et al., 2016). SMM are at substantially greater risk for AUD and associated problems compared to heterosexual men (Cochran & Mays, 2009; Conron, Mimiaga, & Landers, 2010; Lipsky et al., 2012; McCabe, Hughes, Bostwick, West, & Boyd, 2009; Mereish & Bradford, 2014). For instance, one meta-analysis found that SMM are 1.5 times more likely to meet criteria for alcohol dependence than their heterosexual counterparts (King et al., 2008). Unique cultural attributes of SMM are linked to increased susceptibility to negative consequences of heavy drinking (Cochran, Keenan, Schober, & Mays, 2000; Hughes & Eliason, 2002; Mackesy-Amiti, Fendrich, & Johnson, 2009). These attributes include reliance on social settings (e.g., gay bars) that revolve around drinking (Hughes & Eliason, 2002; Wilkerson, Shenk, Grey, Rosser, & Noor, 2015), low (Green & Feinstein, 2012; Stall et al., 2001) as well as high social affiliation (Demant, Hides, White, & Kavanagh, 2018; Lelutiu-Weinberger et al., 2013), and having friends, family, or lovers living with HIV (Ghindia & Kola, 1996). The effect of stress—particularly, stress from oppression, discrimination, and prejudice—and its impact on SMM and their drinking patterns has also been studied (Keyes, Hatzenbuehler, & Hasin, 2011; Mereish, Kuerbis, & Morgenstern, 2018). An association has been found between high levels of perceived discrimination and greater alcohol use, as well as occurrence of AUD among SMM (Hatzenbuehler, Corbin, & Fromme, 2011; McCabe, Bostwick, Hughes, West, & Boyd, 2010; Schwartz & Meyer, 2010). Additionally, SMM are highly vulnerable to secondary health consequences from heavy drinking, such as greater risky sexual behavior and HIV and/or STI transmission (Mackesy-Amiti, Feindrich, & Johnson, 2009; Newcomb, 2013; Rehm, Shield, Joharchi, & Shuper, 2011; Sander et al., 2013; Vosburgh, Mansergh, Sullivan, & Purcell, 2012; Wray et al., 2016). Considering this public health concern, there is strong support for the development of appropriate and effective interventions for SMM with AUD (Coates, Richter, & Caceres, 2008; Vosburgh et al., 2012; Wray et al., 2016).
1.1. Alcohol Treatment Barriers among Sexual Minority Men with AUD
SMM experience unique barriers to AUD treatment. Green (2011) found that lesbian, gay, and bisexual (LGB) individuals reported having negative thoughts about treatment, not seeing their drinking as problematic, lack of motivation to change, stigma associated with treatment, and a lack of agreement with treatment goal choice (i.e., abstinence) as deterrents to traditional treatment for AUD. Others have also noted that an abstinence-based lifestyle that is typically required in formal treatment settings does not fit cultural norms among LGB individuals compared to their straight counterparts (e.g., Stall et al., 2001). Given the barriers to traditional care, engaging SMM in effective interventions for AUD is challenging. Individual goal choice (that is, having the ability to elect one’s goal for treatment whether it is abstinence or moderated drinking) is particularly relevant for SMM with AUD and facilitates their access to care. Morgenstern et al. (2007) found that SMM with AUD and at high risk for HIV transmission self-selected moderation drinking goals rather than abstinence, despite recommendations from providers. Many participants reported that being able to choose a drinking goal was the reason they enrolled in the study. Thus, treatment that allows for individual goal choice can engage SMM with AUD into treatment to reduce harm when they would not otherwise seek traditional care.
1.2. Goal Setting in Alcohol Treatment
Goal setting has been identified as an important component of alcohol treatment with both abstinence and moderation goals leading to reduction in drinking (DeMartini, et al., 2014; van Amsterdam & van den Brink, 2013). Research shows that expanding treatment goals to reduced-risk drinking (i.e., moderation-based goals) is as effective in reducing harm and improving treatment engagement as is abstinence (Kaner et al., 2007; Mann, Aubin, & Witkiewitz, 2017; Marlatt & Witkiewitz, 2002; Miller, Leckman, Delaney, & Tinkcom, 1992; Rosenberg & Davis, 1994; van Amsterdam & van den Brink, 2013). Despite the success of either goal leading to positive outcomes, limited research has been conducted on the effectiveness of specific goal characteristics in predicting optimal outcomes (Bujarski, O’Malley, Lunny, & Ray, 2013). For example, which are more effective for harm reduction—goals that require extensive changes to drinking or goals that involve small changes over time? Research shows that goals often change throughout treatment, and goals set at different points of treatment may be differentially associated with treatment outcomes (Ambrogne, 2002; DeMartini, et al., 2018; van Amsterdam & van den Brink, 2013). To the authors’ knowledge, there are no published studies on goal setting among SMM, other than overall goal choice as discussed above. More information about which goals are more likely to be achieved and promote behavior change is needed for treatment providers to make optimal recommendations to their patients and to SMM specifically.
1.3. Goal Setting Theory
Locke and Latham’s (1990, 2002, 2004) Goal-Setting Theory (GST) was authored in the context of organizational change and job performance, yet aspects of GST may offer important guidance on goal setting within the context of AUD treatment. According to GST, specific goals rather than general, “do-your-best” goals are more effective in driving performance (Locke & Latham, 1990, 2004; Locke, Shaw, Saari, & Latham, 1981). GST also posits that a positive, linear relationship exists between goal difficulty and performance, such that more difficult goals generally yield greater performance than easier goals (Locke & Latham, 2004; Locke, Shaw, Saari, & Latham, 1981); however, when goal difficulty is very high (as in, extreme difficulty due to goal complexity), performance is curtailed (Erez & Zidon, 1984). Locke and Latham (1990, 2002, & 2004) further identified goal commitment (defined as self-reported, goal importance and self-efficacy) as moderators of the goal difficulty and performance relationship. GST suggests that goals of greater difficulty yielded better performance outcomes when goal importance and self-efficacy were at higher levels (Klein, 1991; Locke & Latham, 1990, 2002). There have been no studies related to treatment for AUD that apply GST’s tenets of goal difficulty to guide effective behavior change (Strecher et al., 1995; Webb, Sniehotta, & Michie, 2010).
1.4. This Study
This study explored goal setting in moderation-based alcohol treatment for SMM with AUD in an effort to better guide clinicians and patients in determining the types of goals to pursue for optimal treatment outcomes. In a secondary data analysis, we applied GST to investigate the relationship between goal difficulty and goal achievement. We hypothesized that the more difficult the goal, the more likely a patient would achieve that specific goal in the context of moderation treatment. We expected that participants would mobilize to achieve goals to reduce drinking days and heavy drinking days when those goals required greater change from current drinking (i.e., were more difficult). In addition, we tested the moderating impact of self-efficacy, goal importance, and AUD severity on the relationship between goal difficulty and goal achievement. Due to the direct relationship between self-efficacy and motivation (operationalized here as importance) with drinking described in drinking literature, we hypothesized that these constructs would interact with goal difficulty, such that as they increased, they would potentiate the impact of goal difficulty on goal achievement. In addition, we hypothesized that, in the presence of severe AUD, goal difficulty’s impact on goal achievement would be rendered inert because in a previous study it was found that SMM with AUD have greater difficulty moderating their drinking in the context of severe AUD (Kuerbis, Morgenstern, & Hail, 2012).
2. Method
This study was a secondary analysis implemented using longitudinal panel data from a randomized controlled trial, investigating the efficacy of a combined medication (i.e., naltrexone) and behavioral intervention treatment for moderating alcohol use among SMM (Morgenstern et al., 2012). A full review of the study procedures and findings can be found in Morgenstern et al. (2012). The procedures are briefly described here for the purpose of this study.
2.1. Participants
Participants (N = 340) were recruited via community outreach (at gay bars, events, and community centers), print media, and social networking internet sites (such as Craigslist and Manhunt). Participants were SMM interested in reducing their drinking but not stopping altogether. Participants were included in this study if they: 1) were between the ages of 18 to 65; 2) consumed an average of at least 24 standard drinks of alcohol per week over 90 days prior to baseline; 3) reported having sex with men in the last 90 days; and 4) read English at an eighth grade or higher level. Participants were excluded if they: 1) were diagnosed with schizophrenia and a bipolar or other psychotic disorder; 2) had untreated, active major depressive disorder; 3) reported past or current symptoms of physiological dependence on alcohol or other drugs, excluding nicotine or cannabis (i.e., physical withdrawal symptoms, including history of delirium tremens or seizures); 4) started or changed psychotropic medications during the six months prior to baseline; 5) were at risk for serious side effects from naltrexone (e.g., were taking contraindicated medications, had severe liver abnormalities); 6) reported regular opioid use; 7) were enrolled in another drug or alcohol related treatment during the three-month treatment phase of the study. Of the 340 participants recruited for the study, 200 were eligible and enrolled.
2.2. Procedure
Individuals, who responded to outreach, completed both phone and in-person screening to assess for eligibility. During the in-person screening and baseline assessment (if eligible, called Month 0), participants completed a battery of assessments implemented by a research assistant and computer. All participants were urn randomized (Wei, 1978) to one of four conditions: placebo only (PBO), naltrexone only (NTX), modified behavioral self-control training (MBSCT; Sanchez-Craig, Annis, Bornet, MacDonald, 1984), or NTX + MBSCT (described in Section 2.2.1). All participants attended bi-weekly medication management appointments. Those assigned to any MBSCT group also received 12, weekly, one-hour long therapy sessions. Repeated assessments were conducted at Months 3, 6, and 9, at which point their drinking and other related, psychological factors were evaluated. Participants, and both medical and research staff, were blinded to condition. Participants had the option to be learn about their condition at the end of treatment.
2.2.1. Interventions
2.2.1.1. Medication.
Participants were randomly assigned to receive PBO or NTX. Naltrexone is an oral, opioid antagonist found to be effective in the treatment of AUD (Rosner et al., 2010), but conflicting findings exist regarding its superior efficacy compared to behavioral interventions (e.g., Anton et al., 2006; Oslin et al., 2008). Participants were blind to medication condition. Medication was taken daily and titrated over three weeks from 25mg/day for the first week to 100mg/day by the third week until the end of treatment (Month 3). Psychiatrists recorded medication compliance during medication management appointments.
2.2.1.2. Medication Management.
All participants also received bi-weekly Brief Behavioral Compliance Enhancement Treatment (BBCET; Johnson, DiClemente, Ait-Daoud, & Stoks, 2003), which is a brief intervention for medication compliance. During BBCET, physicians advocated for the benefits and compliance of taking medications to reduce drinking and discussed possible side effects from these medications. Each BBCET session was about 20 minutes and occurred every week for the first three weeks of treatment during titration of medication and continued every other week for the remaining three months of treatment. Psychiatrists were blind to participants’ medication and behavioral intervention conditions. Protocol fidelity was monitored via audio-recordings and yielded 100.0% adherence (Morgenstern et al., 2012).
2.2.1.3. Behavioral Intervention.
Modified behavioral self-control training (MBSCT) is a manual-based combination of two empirically-supported methods for treating AUD: Motivational Interviewing (MI; Hettema, Steele, & Miller, 2005; Morgenstern et al., 2007) and Behavioral Self-Control Training (BSCT; Sanchez-Craig et al., 1984), an empirically-validated treatment method developed to teach controlled drinking (Hester, 1995; Walters, 2000). MBSCT was specifically tailored for SMM with AUD who wish to moderate alcohol consumption in AUD treatment (Morgenstern et al., 2007). MBSCT consisted of two initial sessions of MI and BSCT in the following 10 sessions. Each session was one-hour and conducted by a Masters- or doctoral-level psychotherapist. All but one clinician had more than five years of experience in substance use disorder treatment and with these interventions specifically. The ten therapists who implemented MBSCT obtained weekly supervision and sessions were videotaped to monitor protocol fidelity. Fidelity to the protocol was high (Morgenstern, et al., 2012). All therapists were blind to the medication condition of the participants.
2.3. Measures
2.3.1. Demographics.
Participants provided information about their age, race/ethnicity, education, employment, and psychiatric and substance use disorder treatment history in the initial phone screen and a questionnaire during Month 0.
2.3.2. Goals for frequency of any drinking and drinking to effect.
Participant goals for reducing drinking were measured via the Goals Questionnaire (GoalsQ) that was designed for this study. Participants indicated their goal for frequency of any drinking and frequency of “drinking to effect” (i.e., drinking 4 or more standard drinks) for the next month (30 days). Participants selected one of the following categories: “daily;” “5 to 6 days a week;” “3 to 4 days a week;” “1 to 2 days a week;” “1 to 3 days a month;” “no days, I plan to abstain during the next 30 days.” These categories were coded with values ranging from 5 to 0, respectively.
2.3.3. Goal difficulty.
Goal difficulty was defined as the extent participants wanted to reduce their drinking (based on their response to the goals questions) compared to their current drinking at each time point in the study (i.e., Month 0, 3, and 6). At each time point, goal difficulty was derived by calculating a difference score between the reported number of drinking days and the frequency of drinking set at that same time point. The same difference score was generated for the frequency of drinking to effect goal. Goal difficulty for both frequency of drinking and frequency of drinking to effect ranged from 0 (easiest) to 5 (most difficult). For example, if a participant’s number of drinking days at Month 0 was daily (categorized as 5 on the GoalsQ) and they indicated a frequency of drinking goal of “3 to 4 days a week” (categorized as 3 on the GoalsQ), their goal difficulty was 2 on a scale of 0 to 5.
2.3.4. Goal achievement.
Participants reported their drinking on the Timeline Follow-Back (TLFB; Sobell & Sobell, 1992), a retrospective record of an individual’s frequency and quantity of daily drinking that uses calendar-based memory aids. The TLFB demonstrates good reliability and validity ranging over 30 to 365 days (Carey, 1997; Sobell & Sobell, 1992, 1996; Sobell, Brown, Leo, & Sobell, 1996; Sobell, Maisto, Sobell, & Cooper, 1979; Sobell, Sobell, Leo, & Cancilla, 1988).
In this study, participants completed the TLFB during assessments implemented at Months 0, 3, 6, and 9, such that there was a continuous record of drinking from screen to month 9. Number of drinking days (NDD) was calculated as the average number of days participants reported drinking over the course of one month. Both heavy drinking days (HDD), or the number of days that a participant drank 4 or more standard drinks on one occasion across a month, and NDD were determined for Months 1, 4, and 7 to explore the outcome of drinking goals set in the prior-month’s assessments. These variables were then used to calculate goal achievement.
Goal achievement (GA) was defined as when a participant achieved or surpassed his drinking goal (set at the beginning of the month). GA was calculated for both NDD and HDD. Both GA variables were dichotomous (1 = achieved goal, 0 = did not achieve goal), and calculated for Months 1, 4, and 7.
2.3.5. Baseline drinking.
A baseline drinking variable (i.e., mean drinks per drinking day) was calculated from the Month 0 TLFB assessment and used as a covariate in the models.
2.3.6. Goal importance.
Goal importance was also assessed via the GoalsQ, where participants answered “How important is your goal?” and responded on a scale of 1 (“not at all important”) to 10 (“most important goal this month”). This question referred to both frequency of any drinking and frequency of drinking to effect, and it was measured at Months 0, 3, 6 when participants set their goals.
2.3.7. Self-efficacy.
Self-efficacy to reduce drinking was measured using the Situational Confidence Questionnaire (SCQ-39; Annis & Graham, 1988), a self-report measure, designed to evaluate self-efficacy for refusing to drink in eight types of relapse situations (Breslin, Sobell, Sobell, Agrawal, 2000; Kirisci & Moss, 1997). For this study, the SCQ-39 was specifically modified to reflect self-efficacy to reduce heavy drinking rather than abstain in drinking situations. For each item, participants responded on a six-point, Likert scale about how confident (not confident to very confident) they were that they could refuse to drink heavily in specific situations. A summed score of all the items in the SCQ-39 was used to quantify self-efficacy at Month 0, 3, and 6. Greater scores indicated greater self-efficacy to refuse to drink heavily in drinking situations. Cronbach’s alpha for this sample was .96.
2.3.8. AUD Severity.
AUD severity was measured at Month 0 using the Alcohol Dependence Scale (ADS; Skinner & Horn, 1984), which is a 25-item self-report measure in which scores for each item are summed. The ADS demonstrated high reliability and validity across substance using populations (Kahler, Strong, Hayaki, Ramsey, & Brown, 2003). Cronbach’s alpha for this study was .77.
2.4. Analytic Plan
Initially, multilevel mixed models were used to fit the current models; however, neither random intercept nor slope were significant. Thus, generalized estimating equations (GEE; Liang & Zeger, 1986) were used to test the impact of goal difficulty on GA for both NDD and HDD over the course of the study period. GEE is an extension of generalized linear modeling, a regression analysis performed on non-normally distributed dependent variables (McCullagh, & Nelder, 1989; Nelder & Wedderburn, 1972). It is robust to the violation of the assumption of independence of observations by accounting for highly correlated data. Models testing GA as a binary outcome variable utilized a binomial distribution specified with a log link function (Stokes, Davis, & Koch, 2000).
2.4.1. Model Building for Goal Difficulty Predicting GA.
In the first step, along with the covariates, goal difficulty was entered into the GEE model to determine its relationship to GA. In the second step, an interaction term of goal difficulty by time (goal difficulty*time) was entered into the model to test for the impact of the rate of change in goal difficulty on GA over time. All variables were grand mean centered.
2.4.2. Covariates.
To effectively test relationships between the variables of interest, covariates (i.e., study condition separated out into two dichotomous variables: medication condition and therapy condition; and baseline drinking) were tested as covariates of both the outcome variables in independent models. Those that were significant predictors at thep < .1 level were included in the models as covariates. Only baseline drinking was retained as a covariate for either model.
2.4.3. Testing for Moderation of Goal Difficulty on GA.
We tested self-efficacy, goal importance and AUD severity as moderators of goal difficulty on both types of goal achievement. In a third step with models for each outcome variable, an interaction term, including the potential moderator and goal difficulty, was tested in separate models to determine if there was a moderated relationship between goal difficulty and goal achievement. If an interaction term emerged as significant at the p < .1 level, it was input into a final model in which all interaction terms were tested simultaneously. This procedure was implemented to test for the independent effects of each moderator and then, simultaneously, to test for the combined effects of multiple moderators. All variables were grand mean centered.
2.4.4. Sample for this analysis.
Due to participant attrition rates (7.0% at Month 3, 11.0% at Month 6), 178 participants had complete data. We performed a sensitivity analysis by repeating all analyses with the total sample of 200. Results were equivalent. We reported results of regression models for the 178 participants with complete data.
3. Results
3.1. Descriptives
3.1.1. Demographics.
Baseline characteristics, including age, race, education, employment status, baseline drinking of the participants are displayed in Table 1. The typical participant was White, obtained a college degree or higher level of education, employed, and negative for HIV. Within this sample, 74% identified as White, 13% Hispanic/Latino, 10% African American, and 3% Asian; additionally, 50% of participants received at least some graduate education, and 76% were employed. On average, participants drank 43.1 standard drinks per week and 93.0% met DSM-IV criteria for alcohol dependence when enrolled into the study. The mean age of the participants was 40.3. Participants reported baseline mean drinks per drinking day of 8.30 (SD = 4.50).
Table 1.
Baseline Characteristics
| Total (N = 178) | ||
|---|---|---|
| Variable | M or % | SD |
| Demographics | ||
| Age | 40.3 | (11.1) |
| Race/Ethnicity | ||
| White, non-Hispanic | 74 | |
| African-American | 10 | |
| Asian | 3 | |
| Hispanic/Latino | 13 | |
| Education | ||
| High School/GED or less | 6 | |
| Some College/Associates | 17 | |
| Bachelor’s degree | 27 | |
| Some Graduate or above | 50 | |
| Employed | ||
| Employed | 76 | |
| Unemployed/looking work | 10 | |
| Not in labor force/not look | 14 | |
| Drinking Severity | ||
| Mean drinks per drinking day | 8.3 | (4.5) |
3.1.2. Goal Difficulty.
Table 2 shows means and standard deviations of goal difficulty for both NDD and HDD. Both varied over time, with goal difficulty for NDD increasing across months, and goal difficulty for HDD decreasing across months.
Table 2.
Descriptives of Predictors, Moderators, and Outcomes across Time
| Time | |||
|---|---|---|---|
| Month 0 | Month 3 | Month 6 | |
| M (SD) | M (SD) | M (SD) | |
| Predictors | |||
| Goal Difficulty NDD | .99 (.9) | .87 (1.1) | 1.1 (1.2) |
| Goal Difficulty HDD | 1.4 (1.2) | .74 (.9) | .75 (.9) |
| Moderators | |||
| Self-Efficacy | 106.6 (35.1) | 132.4 (40.3) | 130.1 (37.7) |
| Goal Importance | 7.1 (2.4) | 7.7 (2.2) | 7.3 (2.5) |
| Alcohol Dependence Scale | 13.7 (5.4) | NA | NA |
| Outcomes | Month 1 | Month 4 | Month 7 |
| Achieved Goal NDD | 42.3% | 49.7% | 46.4% |
| Achieved Goal HDD | 55.7% | 52.0% | 59.6% |
Note: NDD=Number of drinking days. HDD=Heavy drinking days. NA=Not applicable.
3.1.3. Outcomes.
Table 2 shows the proportion of participants who achieved their goal across time. In regard to GA for NDD, between 42% and 50% of participants achieved or surpassed their drinking goal across time. For GA for HDD, 52% to 60% of participants achieved or surpassed their drinking goal across time.
3.1.4. Moderators.
Table 2 depicts the means and standard deviations of self-efficacy, goal importance, and AUD severity at Month 0, 3, and 6.
3.2. Goal Difficulty Predicting Goal Achievement in the Following Month
3.2.1. GA for NDD.
As shown in Table 3, when controlling for baseline drinking and time, goal difficulty was a significant predictor of GA, such that for every unit increase in goal difficulty, odds of goal achievement in the next 30 days increased by almost 300%. There was also a significant interactive effect, such that the positive impact of goal difficulty on GA was weakened over time (see Figure 1).
Table 3.
GEE of goal difficulty predicting drinking outcome and goal achievement
| Predictors | Goal Achievement NDD | Goal Achievement HDD | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | OR | 95% Confidence Interval of the OR | p | B | SE | OR | 95% Confidence Interval of the OR | p | |
| Baseline drinking | −0.05 | 0.02 | 0.96 | [0.91, 1.00] | .05 | 0.02 | 0.02 | 1.02 | [0.98, 1.06] | .45 |
| Time | −0.02 | 0.12 | 0.98 | [0.77, 1.24] | .86 | −0.06 | .11 | 0.94 | [0.76, 1.16] | .54 |
| Goal Difficulty | 1.08 | 0.22 | 2.94 | [1.9, 4.5] | <.001 | −0.46 | 0.10 | 0.63 | [0.51, 0.77] | < .001 |
| Goal Difficulty*Time | −0.67 | 0.23 | 0.51 | [0.33, 0.80] | <.01 | 0.20 | 0.12 | 1.22 | [0.97, 1.53] | .09 |
Note: SE = Standard Error for the B (the slope). OR = Odds Ratio. Parameter estimates for main effects of time and goal difficulty were generated without the interaction term in the model. All variables included in the models were centered at the grand mean.
Figure 1.
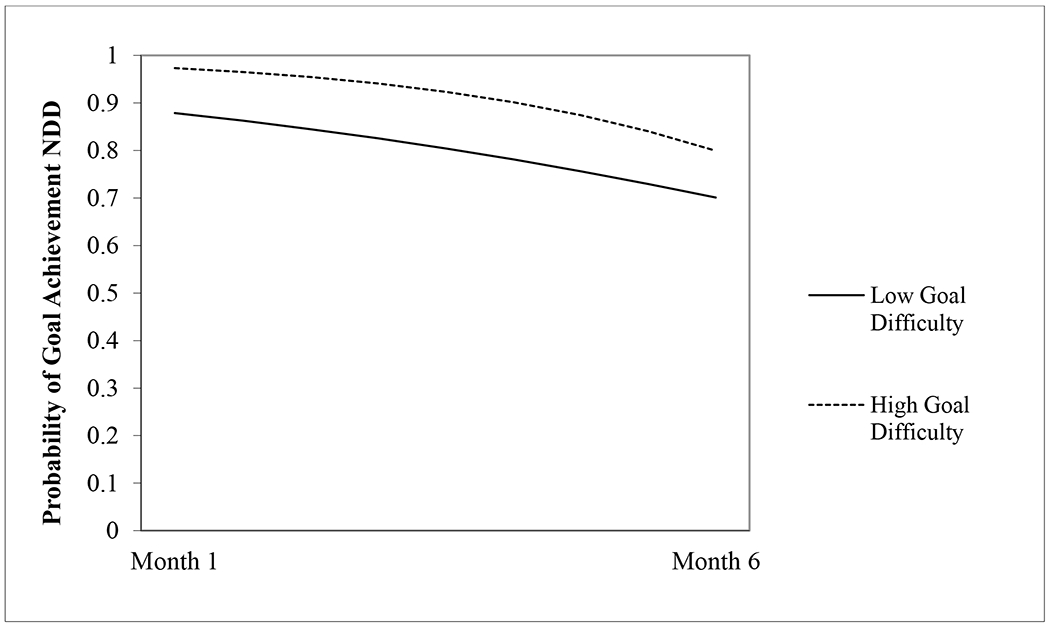
Impact of goal difficulty on goal achievement across time.
3.2.2. GA for HDD.
As shown in Table 3, when controlling for baseline drinking and time, goal difficulty was a significant predictor of GA, such that for every unit increase in goal difficulty, odds of GA decreased by 37%. There was no significant interaction effect with time.
3.2.3. Moderation of the relationship between goal difficulty and GA.
Table 4 shows the parameter estimates, ORs, and confidence intervals of each moderator’s main effect on each type of goal achievement and the impact as a moderator of goal difficulty across each outcome. There were no significant main effects of moderators, except AUD severity, such that, for both GA for NDD and HDD, for every unit increase past the mean of the ADS, odds of achieving the respective goal increased by 5%. There were no moderating effects of goal importance, self-efficacy, or AUD severity on goal difficulty’s impact on either goal achievement variables.
Table 4.
Moderation of the relationship between goal difficulty and goal achievement
| Goal Achievement NDD | Goal Achievement HDD | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | OR | 95% Confidence Interval of the OR | p | B | SE | OR | 95% Confidence Interval of the OR | p | |
| Goal importance | 0.06 | .04 | 1.06 | [0.98, 1.14] | .17 | −0.01 | 0.04 | 0.99 | [0.91, 1.08] | .82 |
| Goal difficulty*Goal importance | −0.04 | .08 | 0.96 | [0.81, 1.13] | .60 | 0.04 | 0.05 | 1.04 | [0.94, 1.16] | .44 |
| Self-efficacy | 0.00 | .002 | 1.00 | [0.99, 1.00] | .92 | −0.004 | .003 | 1.00 | [0.99, 1.00] | .17 |
| Goal difficulty*Self-efficacy | −0.01 | .004 | 0.99 | [0.99, 1.00] | .16 | −0.001 | .003 | 1.00 | [0.99, 1.00] | .69 |
| ADS | 0.05 | 0.02 | 1.05 | [1.01, 1.09] | .01 | −0.04 | 0.02 | 0.96 | [0.92, 0.998] | .04 |
| Goal difficulty*ADS | −0.02 | 0.04 | 0.98 | [0.92, 1.05] | .61 | −0.01 | 0.02 | 0.99 | [0.95, 1.04] | .74 |
Note: B = the estimated slope of the dependent variable as a function of the predictor; SE = Standard Error for the B; OR = Odds Ratio. Main effects of moderators shown here are those generated by models excluding the interaction term. Each moderator was tested independently (i.e., by itself, apart from the other moderators).
4. Discussion
Among this sample of SMM, as hypothesized and consistent with GST, there was a significant positive relationship between the difficulty of the goal set for frequency of drinking and goal achievement. When considering frequency of drinking days, participants with goals for greater change from current drinking were more likely to be successful. As explained by GST, more challenging goals evoke greater effort to work toward those goals (Locke & Latham, 2002, 2006). Over time, however, it appeared that the impact of goal difficulty on goal achievement diminished. There may be an exhaustion factor related to difficult goals, or it may be that the ability to set a difficult goal is finite, as goal achievement progresses. Given this finding, treatment providers should consider guiding SMM who drink heavily to set challenging goals related to reducing the number of days they drink at treatment initiation, as such goals may be more motivating and produce better outcomes. This is also consistent with previous research that demonstrated that individuals with AUD who committed to at least one day of abstinence per week were more likely to achieve moderation than those who did not commit to reducing their drinking days (Kuerbis, Armeli, Muench, & Morgenstern, 2014). As treatment progresses, less drastic changes in drinking should be pursued, as difficult goals may be less likely to be achieved.
Hypotheses were not supported for goals related to the number of days drinking heavily (i.e., drinking to effect). An inverse relationship was observed between goal difficulty and goal achievement for heavy drinking, such that the more difficult the goal, the less likely participants were to achieve it. In the case of reducing the number of days of heavy drinking, incremental rather than difficult goals appear to lead to goal achievement. Although descriptively, and similar to drinking days, about half of participants achieved their goal to reduce their heavy drinking days. Participants may have found it more daunting to achieve difficult goals for reducing heavy drinking, especially for our sample of SMM, who have a ritualized habit of heavy drinking in certain contexts, select social milieus in which heavy drinking is encouraged, or experience strong craving while drinking. In the context of GST, it may be that curtailing one’s drinking, once started, is a highly complex goal and may have exceeded participants’ abilities given their existing habits and symptoms of AUD. Although perception of the difficulty of a goal was not measured here, research demonstrates that goals perceived to be threatening or overly challenging are dismissed by individuals and do not function as a motivating factor for better performance (Drach-Zahavy & Erez, 2002; Locke & Latham, 2006).
The role of craving in alcohol use may also explain participants’ inability to reduce heavy drinking days (e.g., McHugh, Fitzmaurice, Griffin, Anton, & Weiss, 2016; Subbaraman, Lendle, van der Laan, Kaskutas, & Ahern, 2013). Empirical evidence shows a bi-directional relationship between drinking and craving among men (Fazzino, Harder, Rose, & Helzer, 2013), such that while craving leads to drinking, drinking subsequently leads to greater craving. Thus, craving may have a greater impact on alcohol consumption among those who moderate rather than abstain, as higher levels of craving persist for longer among those who continue drinking (Hallgren, Delker, & Simpson, 2018). Considering the complexity of resisting drinking once it is initiated (in other words, moderating heavy drinking days), alcohol treatment providers may recommend less difficult goals for reducing heavy drinking days for SMM to achieve better treatment outcomes.
Self-control theory may also explain challenges in achieving goals related to heavy drinking days. Self-control theory (Gottfredson & Hirschi, 1990) posits that those who have difficulty refraining from engaging in behaviors with instantaneous gratification have low self-control. Studies have found a link between lack of self-control and alcohol consumption among college students (Gibson, Schrek, & Miller, 2004; Piquero, Gibson, & Tibbetts, 2002; Wolfe & Higgins, 2008). Specifically, low self-control has shown to predict binge drinking and alcohol-related problems (Gibson, Schrek, & Miller, 2004; Piquero, Gibson, & Tibbetts, 2002). Low self-control in this study’s sample may explain why goals for heavy drinking days were less likely to be achieved. Higher levels of self-control may be required to decrease heavy drinking days— days in which drinking is controlled after it has been initiated. Unfortunately, self-control and impulsivity were not measured in this study and could not be tested directly.
Contrary to hypotheses, self-efficacy and goal importance had no direct effect on goal achievement and were not moderators of the goal difficulty on goal achievement relationship. It is unclear why goal importance—a proxy for motivation to change drinking—and self-efficacy did not present significant main or moderating effects. Literature supports that both motivation to change and self-efficacy are predictors of alcohol treatment outcomes (Adamson, Sellman, & Frampton, 2009). It is likely that self-efficacy was not a significant predictor in this analysis because it measured general self-efficacy to moderate alcohol use rather than self-efficacy related to the specific goal. Similar to high self-efficacy to reduce drinking, goal importance may have been high for participants, but these indicators may have not translated to greater effort to make changes, as posited by GST. Participants may have experienced high motivation to change as well as self-efficacy to do so but may have failed to apply the necessary effort needed for goal achievement.
Hypotheses were also not supported related to the interactive effect of AUD severity on the goal difficulty and goal achievement relationship. Although there was no impact of AUD severity on difficult goals, it was, however, directly related to goal achievement—that is, those with greater number of symptoms of AUD were more apt to achieve their drinking goal. As demonstrated in other research (Adamson, Sellman, & Frampton, 2009), drinking reduction was more likely to be achieved among individuals with greater AUD severity. In accordance with GST’s explanation for the role of effort, it is likely that individuals with greater AUD severity utilized greater effort to achieve their goals because they recognized that they would have to exert more effort to changing their drinking behavior compared to those with fewer drinking problems. It is also possible that those with more severe AUD had greater urgency to change their drinking compared to their less severe drinking counterparts.
Collectively, these findings indicate that moderation-based interventions are a good fit for SMM with AUD, as they are able to set and achieve such drinking goals. As shown in previous studies (Morgenstern et al., 2007), moderation-based treatment is an alternative that overcomes the treatment barrier that SMM experience with traditional care, which calls for complete abstinence from alcohol use. Within such a treatment model, SMM may benefit from initially setting more difficult drinking goals, where they aim to make greater reductions in drinking days, to be more successful. However, over time in treatment, more difficult goals may be less relevant to success. Alternatively, in reducing heavy drinking days, SMM should aim to make gradual reductions in heavy drinking days.
4.1. Limitations
There are variety of limitations to the study, and findings should be interpreted accordingly. First, goal measurement on the GoalsQ was limited. Goal categories were only focused on the number of days of any drinking or heavy drinking and were reported in ranges, which did not allow for specificity and did not reflect the variety of ways to moderate alcohol use. This limited our ability to detect nuances in goal setting predicting goal achievement. Specific goals are a requisite part of goal setting as described in GST, and so this limited our ability to apply GST to this study. Additionally, the full range of progress toward a goal was not captured. Reduced intensity of drinking may not have been captured if it did not fall within the available categories in just the right way. For example, a person may have set a goal to reduce drinking on a particular day and achieved that goal, but this progress was not detected if there was no change in heavy drinking days. Furthermore, this study did not investigate goal difficulty on drink reduction in general. GST does not provide guidance on how goal setting may impact progress toward goals or partial goal achievement. It is possible that goal setting influenced participants’ reduced drinking in the absence of goal achievement.
Another limitation of the Goals Q was that for the drinking to effect (or heavy drinking) goal, participants were asked to make goals on the frequency of days drinking four or more standard drinks rather than five. While this question was originally intended to capture binge drinking, it instead captured a subthreshold level of binge drinking. As a result, it could not precisely capture binge drinking, limiting our ability to make conclusions about goal setting and binge drinking.
Furthermore, participants completed the GoalsQ during computer assessments conducted every three months. It is possible that, in between assessments, participants altered their drinking goals or set new ones. This may have been particularly evident among participants who received a behavioral intervention, as they could have developed alternative and more specific drinking goals in therapy sessions, though we found no differences among those who received MBSCT.
Similar constraints may have occurred in the measurement of self-efficacy for this study. GST posits that it is self-efficacy specific to achieving a particular goal that moderates the relationship between goal difficulty and performance. The SCQ-39 only measured self-efficacy for a broadly moderating heavy alcohol use. Goal importance was also measured to reflect both the frequency of drinking and drinking to effect goals rather than for each, individually. GST identified the moderating effect of individual goal commitment; therefore, the lack of a moderating effect of our goal importance variable could have been a result of its lack of specificity per goal. Notably, although we used the full sample of the moderation analyses, it is possible that we did not have a large enough sample to achieve the power necessary to detect an effect for any of the above moderators.
Finally, it is important to note that we were not able to capture how stigma, prejudice, and oppression, as well as sexual orientation or identity, may have facilitated or impeded goal setting and goal achievement in this sample of SMM. Sexual identity was not a significant covariate in this analysis; however, this does not preclude factors related to sexual minority status as impacting goal setting and goal achievement. These findings only generalize to cisgender men responding affirmatively that they are men who have sex with men. Furthermore, given the hidden nature of both heavy drinkers who do not present to formal treatment and SMM, we cannot accurately assess the representativeness of this sample compared to its population; however, the sample is quite similar to other studies we and others have implemented (e.g., Morgenstern et al., 2007).
4.2. Future Research
Considering the clinical importance for improving AUD treatment for SMM via the application of GST tenets, these findings should be replicated among this group as well as other vulnerable groups who may avoid treatment in an effort to improve generalizability. Future research should consider alternative methods of collecting goal data, including having participants identify specific frequency and heavy drinking goals on a continuous scale (i.e., indicating how much participants wish to drink per day and per week as well as how many days to not drink), report their perception of difficulty, and offer more frequent measurements of goals in treatment. Specific self-efficacy and importance or commitment to achieve a drinking goal and a measure of effort in doing so should be investigated as moderators of the goal difficulty and goal achievement relationship. Investigating the role of craving in this relationship may explain the differences between reducing quantity of drinks in a sitting and drinking days (whether binge drinking days or not). Furthermore, future research should study the relationship between goal difficulty and drinking reduction in general, when goals for drinking can be more carefully manipulated. Whether or not certain goals are achievable, it is possible that certain goals effectively motivate individuals to make reductions in their drinking, even if goals are not achieved. Finally, further exploration as to potential moderators of goal difficulty on drink reduction and goal achievement should be implemented and expanded to include impulsivity, craving, and self-control.
4.3. Conclusion
Research has called for the development of effective interventions to reduce heavy alcohol use among SMM. In the context of its limitations, this study informs alcohol treatment providers and SMM on the types of drinking goals to consider when moderating alcohol use. Goal difficulty, as defined by the proposed magnitude of change in drinking, emerged as an important factor in goal achievement. Goals of greater difficulty should be established for reducing the number of drinking days, while reducing heavy drinking days should be guided by less difficult goals among SMM with AUD. With limited research providing guidance on goal setting in moderation-based alcohol treatment, this study is a first step in identifying what types of drinking goals should guide treatment to yield better outcomes in drinking reduction. Future research should expand findings with additional ways to capture drinking goals and commitment to reduce drinking.
Highlights.
Goal Setting Theory was tested as a framework for treating alcohol use disorders
Drink goals of greater difficulty yield greater reduction in number days drinking
Effect of difficult drink goals on number days drinking diminishes over time
Drink goals of greater difficulty yield lower reduction in heavy drinking days
Sexual minority men should pursue difficult drink goals in moderation treatment
Acknowledgments
Author Note: This study was supported with funding from the National Institute on Alcohol Abuse and Alcoholism (Grant R01 AA015553; PI: Morgenstern).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: Authors have nothing to declare.
References
- Adamson SJ, Sellman JD, & Frampton CMA (2009). Patient predictors of alcohol treatment outcomes: A systematic review. Journal of Substance Abuse Treatment, 36(1), 75–86. [DOI] [PubMed] [Google Scholar]
- Annis HM, & Graham JM (1988). Situational confidence questionnaire. Toronto: Addiction Research Foundation. [Google Scholar]
- Anton RF, O’Malley SS, Ciraulo DA, Ciraulo DA, Cisler RA, Couper D, … Zweben A (2006). Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA, 295(11), 2003–2017. doi: 10.1001/jama.295.17.2003 [DOI] [PubMed] [Google Scholar]
- Ambrogne JA (2002). Reduced-risk drinking as a treatment goal. What clinicians need to know. Journal of Substance Abuse Treatment, 22, 45–53. 10.1016/S0740-5472(01)00210-0. [DOI] [PubMed] [Google Scholar]
- Breslin FC, Sobell LC, Sobell MB, & Agrawal S (2000). A comparison of a brief and long version of the Situational Confidence Questionnaire. Behaviour Research and Therapy, 38, 1211–1220. [DOI] [PubMed] [Google Scholar]
- Bujarski S, O’Malley SS, Lunny K, & Ray LA (2013). The effects of drinking goal on treatment outcome for alcoholism. Journal of Consulting and Clinical Psychology, 57(1), 13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB (1997). Reliability and validity of the time-line follow-back interview among psychiatric outpatients: A preliminary report. Psychology of Addictive Behaviors, 77(1), 26–33. doi: 10.1037/0893-164X.11.1.26 [DOI] [Google Scholar]
- Coates TJ, Richter L, & Caceres C (2008). Behavioural strategies to reduce HIV transmission: how to make them work better. Lancet, 23, 669–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran BN, & Cauce AM (2006). Characteristics of lesbian, gay, bisexual, and transgender individuals entering substance abuse treatment. Journal of Substance Abuse Treatment, 30, 135–146. [DOI] [PubMed] [Google Scholar]
- Cochran SD, Keenan C, Schober C, & Mays VM (2000). Estimates of alcohol use and clinical treatment needs among homosexually active men and women in the U.S. population. Journal of Consulting and Clinical Psychology, 68(6), 1062–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran SD, & Mays VM (2009) Burden of psychiatric morbidity among lesbian, gay, and bisexual individuals in the California Quality of Life Survey. Journal of Abnormal Psychology, 118(3), 647–658. doi: 10.1037/a0016501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor JP, Haber PS, & Hall WD (2016). Alcohol use disorders. Lancet, 387, 988–998. 10.1016/50140-6736(15)00123-3. [DOI] [PubMed] [Google Scholar]
- Conron KJ, Mimiaga MJ, & Landers SJ (2010). A population-based study of sexual orientation identity and gender differences in adult health. American Journal of Public Health, 100, 1953–1960. 10.2105/AJPH.2009.174169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis AK & Rosenberg H (2013). Acceptance of non-abstinence goals by addiction professionals in the United States. Psychology of Addictive Behaviors, 27(4), 1102–1109. Doi: 10.1037/a0030563. [DOI] [PubMed] [Google Scholar]
- Demant D, Hides L, White KM, & Kavanagh DJ (2018). Effects of participation in and connectedness to the LGBT community on substance use involvement of sexual minority young people. Addictive Behaviors, 81, 167–174. 10.1016/j.addbeh.2018.01.028. [DOI] [PubMed] [Google Scholar]
- DeMartini KS, Devine EG, DiClemente CC, Martin DJ, Ray LA, & O’Malley SS (2014). Predictors of pretreatment commitment to abstinence: results from the COMBINE study. Journal of Studies on Alcohol and Drugs, 75, 438–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drach-Zahavy A, & Erez M (2002).Challenge versus threat effects on the goal-performance relationship. Organizational Behavior and Human Performance, 88, 667–682. doi: 10.1016/S0749-5978(02)00004-3 [DOI] [Google Scholar]
- Erez M, & Zidon I (1984). Effect of goal acceptance on the relationship of goal difficulty to performance. Journal ofApplied Psychology, 69, 69–78. [Google Scholar]
- Fazzino TL, Harder VS, Rose GL, & Helzer JE (2013). A daily process examination of the bidirectional relationship between craving and alcohol consumption as measured via interactive voice response. Alcoholism: Clinical and Experimental Research, 57(12), 2161–2167. doi: 10.1111/acer.12191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghindia DJ, & Kola LA (1996). Co-factors affecting substance abuse among homosexual men: An investigation within a midwestern gay community. Drug and Alcohol Dependence, 41, 167–177. [DOI] [PubMed] [Google Scholar]
- Gibson C, Schrek CJ, & Miller JM (2004). Binge drinking and negative alcohol-related behaviors: A test of self-control theory. Journal of Criminal Justice, 32(5), 411–420. https://doi.Org/10.1016/j.jcrimjus.2004.06.003 [Google Scholar]
- Gottfredson MR, & Hirschi T (1990). A general theory of crime. Stanford, CA: Stanford University Press. [Google Scholar]
- Green KE (2011). Barriers and treatment preferences reported by worried drinkers of various sexual orientations. Alcoholism Treatment Quarterly, 29, 45–63. doi: 10.1080/07347324.2011.538311 [DOI] [Google Scholar]
- Green KE, & Feinstein BA (2012). Substance use in lesbian, gay, and bisexual populations: an update on empirical research and implications for treatment. Psychology of Addictive Behaviors, 26(2), 265–278. doi: 10.1037/z0025424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallgren KA, Delker BC, & Simpson TL (2018). Effects of initiating abstinence from alcohol on daily craving and negative affect: Results from a pharmacotherapy clinical trial. Alcoholism: Clinical and Experimental Research, 42(3), 634–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Corbin WR, & Fromme K (2011). Discrimination and alcohol-related problems in emerging adults: A prospective examination of mediating effects. Drug and Alcohol Dependence, 115(3), 213–220. 10.1016/j.drugalcdep.2010.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hester RK (1995). Behavioral self-control training In Hester RK & Miller WR (Eds.), Handbook of alcoholism treatment approaches: Effective alternatives (2 ed, pp. 148–159). Needham Heights, MA: Allyn & Bacon. [Google Scholar]
- Hettema J, Steele J, & Miller WR (2005). Motivational Interviewing. Annual Review of Clinical Psychology, 1, 91–111. 10.1146/annurev.clinpsy.1.102803.143833 [DOI] [PubMed] [Google Scholar]
- Hughes TL & Eliason M (2002). Substance use and abuse in lesbian, gay, bisexual, and transgender populations. The Journal of Primary Prevention, 22(3), 263–298. 10.1023/A:1013669705086 [DOI] [Google Scholar]
- Irwin TW, Morgenstern J, Parsons JT, Wainberg M, & Labouvie E (2006). Alcohol and sexual HIV risk behavior among problem drinking men who have sex with men: an event level analysis of timeline followback data. AIDS Behavior, 10, 299–307. [DOI] [PubMed] [Google Scholar]
- Johnson BA, DiClemente CC, Ait-Daoud N, & Stoks SM (2003). Brief Behavioral Compliance Enhancement Treatment (BBCET) manual: In: Johnson BA, Ruiz P, Galanter M (Eds.) Handbook of Clinical Alcoholism Treatment (pp. 282–201). Baltimore, MD: Lippincott, Williams, & Wilkins. [Google Scholar]
- Kahler CW, Strong DR, Hayaki J, Ramsey SE, & Brown RA (2003). An item response analysis of the Alcohol Dependence Scale in treatment-seeking alcoholics. Journal of Studies on Alcohol and Drugs, 64(1), 127–136. 10.15288/jsa.2003.64.127 [DOI] [PubMed] [Google Scholar]
- Kaner EFS, Beyer F, Dickinson HO, Pienaar E, Campbell F, Schlesinger C … Burnand B (2007). Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Systems Review, CD004148. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Hatzenbuehler ML, & Hasin DS (2011). Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main type of stressors. Psychopharmacology, 218, 1–17. Doi: 10.1007/s00213-011-2236-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M, Semlyen J, Tai S, Killaspy H, Osborn D, Popelyuk D, & Nazareth I (2008). A systematic review of mental disorder, suicide, and deliberate self-harm in lesbian, gay, and bisexual people. BMC Psychiatry, 8(70), 1–17. 10.1186/1471-244X-8-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirisci L, & Moss HB (1997). Reliability and validity of the situational confidence questionnaire in an adolescent sample: confirmatory factor analysis and item response. Measurement and Evaluation in Counseling and Development, 30(3), 146. [Google Scholar]
- Klein HJ (1991). Further evidence on the relationship between goal setting and expectancy theories. Organizational Behavior and Human Decision Processes, 49, 230–257. doi: 10.1016/0749-5978(91)90050-4 [DOI] [Google Scholar]
- Kuerbis A, Armeli S, Muench F, & Morgenstern J (2014). Profiles of confidence and commitment to change as predictors of moderated drinking: A person-centered approach. Psychology ofAddictive Behaviors, 25(4), 1065–1076. 10.1037/a0036812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuerbis A, Morgenstern J, & Hail LA (2012). Predictors of moderated drinking in a primarily alcohol dependent sample of men who have sex with men. Psychology of Addictive Behaviors, 26(3), 484–495. doi: 10.1037/a0026713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lelutiu-Weinberger C, Pachankis JE, Golub SA, Walker JJ, Bamonte AJ, Parsons JT (2013). Age cohort differences in the effects of gay-related stigma, anxiety and identification with the gay community on sexual risk and substance use. AIDS Behavior, 17, 340–349. 10.1007/sl0461-011-0070-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang KY, & Zeger SL (1986). Longitudinal data analysis using Generalized Linear Models. Biomelrika, 73, 13–22. [Google Scholar]
- Lipsky S, Krupski A, Roy-Byrne P, Huber A, Lucenko BA, & Mancuso D (2012). Impact of sexual orientation and co-occurring disorders on chemical dependence treatment outcomes. Journal of Studies on Alcohol and Drugs, 75(3), 401–412. 10.15288/jsad.2012.73.401 [DOI] [PubMed] [Google Scholar]
- Locke EA, & Latham GP (1990). A Theory of Goal Setting and Task Performance. Prentice Hall: Englewood Cliffs, NJ. [Google Scholar]
- Locke EA, & Latham GP (2002). Building a practically useful theory of goal setting and task motivation. American Psychologist, 57, 705–717. [DOI] [PubMed] [Google Scholar]
- Locke EA, & Latham GP (2004). What should we do about motivation theory? Six recommendations for the 21st century. Academy of Management Review, 29, 388–403. [Google Scholar]
- Locke EA, & Latham GP (2006). New Directions in Goal-Setting Theory. Current Directions in Psychological Science, 15, 265–268. doi: 10.1111/j.1467-8721.2006.00449.x [DOI] [Google Scholar]
- Locke EA, Shaw KN, Saari LM, & Latham GP (1981). Goal setting and task performance: 1969-1980. Psychological Bulletin, 90, 125–152. [Google Scholar]
- Mann K, Aubin H, & Witkiewitz K (2017). Reduced drinking in alcohol dependence treatment, what is the evidence? European Addiction Research, 23, 219–230. Doi: 10.1159/000481348. [DOI] [PubMed] [Google Scholar]
- Mackesy-Amiti ME, Fendrich M, & Johnson TP (2009). Substance-related problems and treatment among men who have sex with men in comparison to other men in Chicago. Journal of Substance Abuse Treatment, 36, 227–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA & Witkiewitz K (2002). Harm reduction approaches to alcohol use: Health promotion, prevention, and treatment. Addictive Behaviors, 27, 867–886. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Bostwick WB, Hughes TL, West BT, & Boyd CJ (2010). The relationship between discrimination and substance use disorders among lesbian, gay, bisexual adults in the United States. American Journal of Public Health, 100, 1946–1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, Bostwick WB, West BT, & Boyd CJ (2009). Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction, 104, 1333–1345. doi: 10.1111/j.1360-0443.2009.02596.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullagh P, & Nelder JA (1989). Generalized Linear Models (2 ed.). London: Chapman and Hall. [Google Scholar]
- McHugh RK, Fitzmaurice GM, Griffin ML, Anton RF, & Weiss RD (2016). Association between a brief alcohol craving measure and drinking in the following week. Addiction, 111(6), 1004–1010. doi: 10.1111/add.13311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mereish EEL, & Bradford JB (2014). Intersecting identities and substance use problems: sexual orientation, gender, race, and lifetime substance use problems. Journal of Studies on Alcohol and Drugs, 75(1), 179–188. 10.15288/jsad.2014.75.179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mereish EH, Kuerbis A, & Morgenstern J (2018). A daily diary study of stressful and positive events, alcohol use, and addiction severity among heavy drinking sexual minority men. Drug and Alcohol Dependence, 187, 149–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Leckman AL, Delaney HD, & Tinkcom M (1992). Long-term follow-up of behavioral self-control training. Journal of Studies on Alcoholism, 53, 249–261. 10.15288/jsa.1992.53.249 [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Kuerbis AN, Chen AC, Kahler CW, Bux DA, & Kranzler HR (2012). A Randomized clinical trial of naltrexone and behavioral therapy for problem drinking men who have sex with men. Journal of Consulting and Clinical Psychology, 80(5), 863–75. doi: 10.1037/a0028615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, Irwin TW, Wainberg ML, Parsons JT, Muench F, Bux DA, … Shulz-Heik J (2007). A randomized controlled trial of goal choice interventions for alcohol use disorders among men-who-have-sex-with-men. Journal of Consulting and Clinical Psychology, 75(1), 72–84. [DOI] [PubMed] [Google Scholar]
- Nelder JA, & Wedderburn RWM (1972). Generalized linear models. Journal of the Royal Statistical Society, Series A, 135, 370–384. [Google Scholar]
- Newcomb ME (2013). Moderating effect of age on the association between alcohol use and sexual risk in MSM: evidence for elevated risk among younger MSM. AIDS Behavior, 17, 1746–1754. doi: 10.1007/sl0461-013-0470-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oslin DW, Lynch KG, Pettinati HM, Kampman KM, Gariti P Gelfand L, … O’Brien CP (2008). A placebo-controlled randomized clinical trial of naltrexone in the context of different levels of psychosocial intervention. Alcoholism: Clinical and Experimental Research, 32(1), 1299–1308. doi: 10.1111/j.l530-0277.2008.00698.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson SW, David A, Hall M, & Golder S (2009). Beliefs and behaviors regarding substance use and HIV risk among men who have sex with men (MSM) in a mid-sized US community. Journal of HIV AIDS & Social Services, 30, 135–146. [Google Scholar]
- Piquero AR, Gibson C, & Tibbetts S (2002). Does self-control account for the relationship between binge drinking and alcohol related behaviours? Criminal Behaviour and Mental Health, 12, 135–154. 10.1002/cbm.492 [DOI] [PubMed] [Google Scholar]
- Rehm J, Shield KD, Joharchi N, & Shuper PA (2011). Alcohol consumption and the intention to engage in unprotected sex: Systematic review and meta-analysis of experimental studies. Addiction, 107, 51–59. doi: 10.1111/j.1360-0443.2011.03621.x [DOI] [PubMed] [Google Scholar]
- Rosenberg H & Davis LA (1994). Acceptance of moderation drinking by alcohol treatment services in United Stat3es of America. Journal of Studies on Alcoholism, 13, 85–92. [DOI] [PubMed] [Google Scholar]
- Rosner S, Hackl-Herrwerth A, Leucht S, Vecchi S, Srisurapanont M, & Soyka M (2010). Opioid antagonists for alcohol dependence. Cochrane Database Systematic Review, 8(12), CD001867. [DOI] [PubMed] [Google Scholar]
- Sanchez-Craig M, Annis HM, Bomet AR, & MacDonald KR (1984). Random assignment to abstinence and controlled drinking: evaluation of cognitive-behavioral program for problem drinkers. Journal of Consulting and Clinical Psychology, 52, 390–403. [DOI] [PubMed] [Google Scholar]
- Sander PM, Cole SR, Stall RD, Jacobson LP, Eron JJ, Napravnik S, … Ostrow DG (2013). AIDS, 27(5), 815–823. doi: 10.1097/QAD.0b013e32835cff4b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz S, & Meyer IH (2010). Mental health disparities research: the impact of within and between group analyses on test of social stress hypotheses. Social Science & Medicine, 70, 1111–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HA, & Horn JL (1984). Alcohol Dependence Scale: Users guide. Toronto, Ontario, Canada: Addiction Research Foundation. [Google Scholar]
- Sobell LC, Brown J, Leo GI, & Sobell MB (1996). The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug and Alcohol Dependence, 42(1), 49–54. 10.1016/0376-8716(96)01263-X [DOI] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, & Cooper AM (1979). Reliability of alcohol abusers’ self-reports of drinking behavior. Behaviour Research and Therapy, 77(2), 157–160. 10.1016/0005-7967(79)90025-1 [DOI] [PubMed] [Google Scholar]
- Sobell LC, & Sobell MB (1992). Timeline Follow-Back In: Litten RZ, Allen JP (Eds.) Measuring Alcohol Consumption. Totowa, NJ: Humana Press; 10.1007/978-l-4612-0357-5_3 [DOI] [Google Scholar]
- Sobell MB, & Sobell LC (1996). Problem drinkers: Guided self-change treatment. New York, NY: Guilford Press. [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, & Cancilla A (1988). Reliability of a timeline method: Assessing normal drinkers’ reports of recent drinking and a comparative evaluation across several populations. British Journal of Addiction, 52(4), 393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x [DOI] [PubMed] [Google Scholar]
- Stall R, Paul JP, Greenwood G, Pollack LM, Bein E, Crosby GM, … Catania JA (2001). Alcohol use, drug use and alcohol-related problems among men who have sex with men: The Urban Men’s Health Study. Addiction, 96, 1589–1601. doi: 10.1080/09652140120080723 [DOI] [PubMed] [Google Scholar]
- Stokes ME, Davis CS, & Koch GG (2000). Categorical data analysis using the SAS system (2nd ed.). Cary, NC: SAS Institute Inc. [Google Scholar]
- Strecher VJ, Seijts GH, Kok GJ, Latham GP, Glasgow R, DeVellis B, … Bulger DW (1995). Goal setting as a strategy for health behavior change. Health Education Quarterly, 22, 190–200. doi: 10.1177/109019819502200207 [DOI] [PubMed] [Google Scholar]
- Subbaraman MS, Lendle S, van der Laan M, Kaskutas LA, & Ahem J (2013). Cravings as a mediator and moderator of drinking outcomes in the COMBINE study. Addiction, 705(10), 1737–1744. doi: 10.1111/add.12238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Amsterdam J & van den Brink W (2013). Reduced-risk drinking as a viable treatment goal in problematic alcohol use and alcohol dependence. Journal of Psychopharmacology, 27(11), 987–997. Doi: 10.1177/0269881113495320. [DOI] [PubMed] [Google Scholar]
- Vosburgh HW, Mansergh G, Sullivan PS, & Purcell DW (2012). A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behavior, 16, 1394–1410. [DOI] [PubMed] [Google Scholar]
- Walters GD (2000). Behavioral self-control training for problem drinkers: A meta-analysis of randomized control studies. Behavior Therapy, 31, 135–149. doi: 10.1016/S0005-7894(00)80008-8 [DOI] [Google Scholar]
- Webb TL, Sniehotta FF, & Michie S (2010). Using theories of behavior change to inform interventions for addictive behaviours. Addiction, 105, 1879–1892. Doi: 10.1111/j.1360-0443.2010.03028.x [DOI] [PubMed] [Google Scholar]
- Wei LJ (1978). An application of the Urn model to the design of sequential controlled clinical trials. Journal of the American Statistical Association, 75(363), 559–563. [Google Scholar]
- Wilkerson JM, Shenk JE, Grey JA, Rosser BR, & Noor SW (2015). Recruitment strategies of methamphetamine-using men who have sex with men into an online survey. Journal of Substance Use, 20(1), 33–37. doi: 10.3109/14659891.2013.868936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe SE, & Higgins GE (2008). Self-control and perceived behavioral control: An examination of college student drinking. Applied Psychology in Criminal Justice, 4(1), 108–134. [Google Scholar]
- Wray TB, Grin B, Dorfman L, Glynn TR, Kahler CW, Marshall BDL, … Operario D (2016). Systematic review of interventions to reduce problematic alcohol use in men who have sex with men. Drug and Alcohol Review, 35, 148–157. doi: 10.1111/dar.12271 [DOI] [PMC free article] [PubMed] [Google Scholar]


