Abstract
The current study examined the interpersonal model of binge eating, which posits that interpersonal problems lead to negative affect which results in binge eating, over the course of two psychotherapy treatments (interpersonal psychotherapy and cognitive behavioral therapy) in 162 adults with binge-eating disorder. A series of longitudinal simple mediation analyses preliminarily showed that treatment addresses the mechanisms of the interpersonal model of binge eating as theoretically proposed in predicting reductions in binge eating, the primary dependent variable, as well as secondary dependent variables including global eating disorder psychopathology, shape concern, and weight concern, but not reductions in restraint or eating concern. Moderated mediation analyses did not fully support treatment differences, as changes in the mechanisms of the interpersonal model occurred in both treatments, and suggest both treatments addressed negative affect and interpersonal precipitants of eating disorder symptomatology. Future research should replicate this study using variables that do not overlap in time to investigate causation of the model, and more generally, further examine theoretical treatment models and treatment mediators as this research could help improve efficacy of treatment for binge-eating disorder.
Keywords: interpersonal model, binge-eating disorder, interpersonal problems, negative affect, psychological treatment
Introduction
Binge-eating disorder (BED) is the most prevalent eating disorder (ED) and is characterized by recurrent episodes of binge eating (i.e., eating an unusually large amount of food accompanied by the feeling of loss of control over eating), and marked distress associated with the binge eating (American Psychiatric Association [APA], 2013). BED occurs across a range of body weights; however, the majority of individuals seeking treatment for BED have overweight or obesity (APA, 2013; Hudson, Hiripi, Pope, & Kessler, 2007). The interpersonal model of binge eating (Wilfley, MacKenzie, Welch, Ayres, & Weissman, 2000) is one theoretical model that seeks to explain binge eating and related psychopathology (i.e., BED psychopathology). The interpersonal model proposes that difficulties with social functioning or interpersonal problems cause negative affect, which in turn results in binge eating (Figure 1). The interpersonal model of binge eating was an adaptation of the interpersonal model of depression (Klerman, Weissman, Rounsaville, & Chevron, 1984) and interpersonal theory (Sullivan, 1953).
Figure 1.
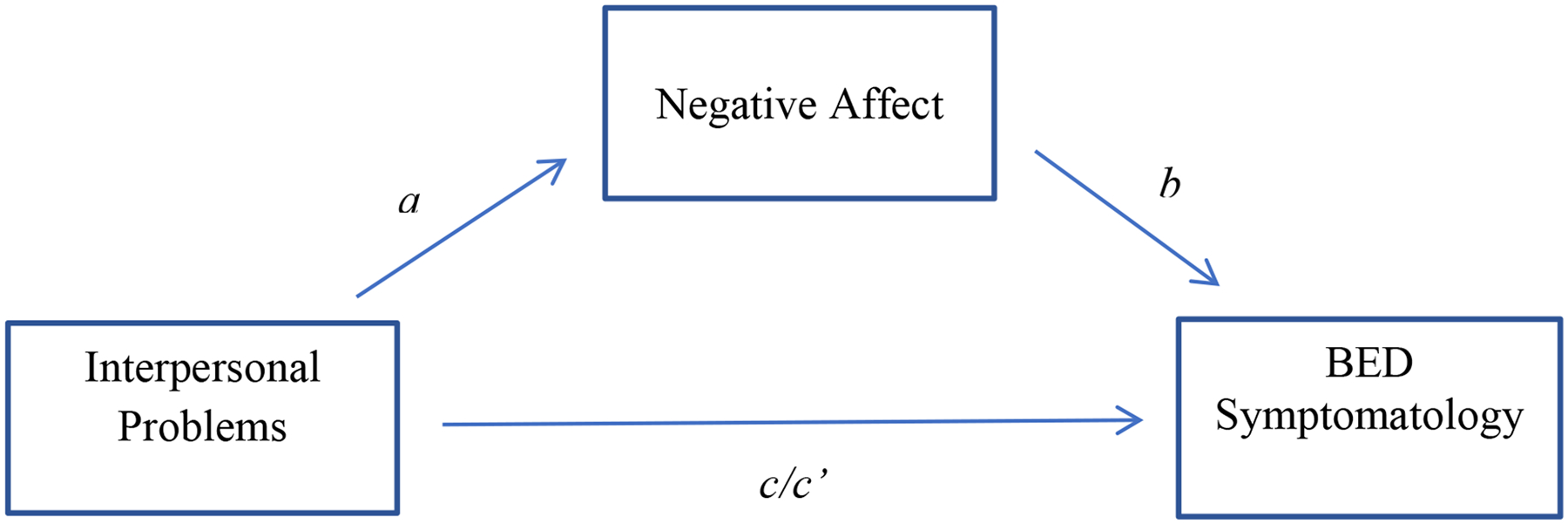
The interpersonal model of binge eating and related psychopathology.
BED= binge eating disorder.
Binge Eating and Interpersonal Problems
Research has shown that individuals with BED (and other EDs [Hartmann, Zeeck, & Barrett, 2010]) have increased levels of interpersonal problems (Blomquist, Ansell, White, Masheb, & Grilo, 2012; Tasca, Balfour, Presniak, & Bissada, 2012; Ung et al., 2017). One study found that women who were obese with deficiencies in assertiveness, ability to express feelings, capacity to deal with strangers, and ability to understand the perspective of others had a higher probability of presenting with a BED diagnosis (Duchesne et al., 2012). Further, women with BED who have obesity show greater levels of interpersonal hostility and distress than women who are obese without BED (Duchesne et al., 2012), lower levels of interpersonal problem-solving skills than controls who are overweight (Svaldi, Dorn, and Trentowska, 2011), and more negative marital interactions than women with or without other psychological disorders (Whisman, Demeteyva, Baucom, & Bulik, 2012).
Binge Eating and Negative Affect
Negative affect has also been associated with binge eating. Negative affect is a general dimension of subjective distress that includes a variety of aversive mood states, such as nervousness, sadness, hostility, anger, and contempt (Watson & Tellegen, 1985; Watson, Clark, & Tellegen, 1988). According to negative affect theory, binge eating functions to regulate negative affect, or provide comfort and distraction from negative mood states (Stice, 2002; Stice & Agras, 1999). A meta-analysis of both experimental and correlational studies supported this theory, as it showed that negative mood is reliably associated with and precedes binge eating (Haedt-Matt & Keel, 2011). Further, individuals with BED often binge eat in response to stress and negative affect (Masheb & Grilo, 2006), and report more distress and lower tolerance of negative mood states (Kenardy, Arnow, & Agras, 1996). Using ecological momentary assessment (EMA), negative mood and hunger have been shown to be significantly higher before a binge-eating episode compared to non-binge times (Berg et al., 2017).
Empirical Support for the Interpersonal Model of Binge Eating
Based on the theoretical interpersonal model of binge eating, Wilfley and colleagues developed and tested interpersonal psychotherapy (IPT) for the treatment of BED (Wilfley et al., 2000, Wilfley et al., 2002). The short- and long-term success of IPT for the treatment of BED in adults supports the plausibility of the interpersonal model of binge eating (Hilbert et al., 2012; Wilfley et al., 2002), and recent efforts have more directly evaluated the interpersonal model empirically and found support in non-treatment-seeking children and adolescents (Elliot et al., 2010), non-clinical adults (Ansell, Grilo, and White, 2012), in individuals with obesity with and without BED (Lo CoCo et al., 2016), as well as clinical samples of women with BED (Ivanova et al., 2015). Evidence also suggests that the interpersonal model transcends ED diagnoses as support for the interpersonal model of binge eating was found in women with anorexia nervosa restricting type, bulimia nervosa, BED, and ED not otherwise specified (Ivanova, Tasca, Proulx, & Bissasda, 2016). Moreover, Stice, Gau, Rohde, and Shaw (2017) found that impaired interpersonal functioning and negative affect are transdiagnostic eating disorder risk factors, and the only ones that predicted future onset of BED, bulimia nervosa, purging disorder, and anorexia nervosa.
Although these studies supported the interpersonal model using cross-sectional data, only longitudinal data can reveal and inform the casual relations inherent in mediational models (Maxwell, Cole, & Mitchell, 2011; Cole & Maxwell, 2003; Maxwell & Cole, 2007). Two experimental studies to date have tested the model in a temporally sensitive way (Russell, Haynos, Crow, & Fruzzetti, 2017; Shank et al., 2017). Female adolescents with loss of control eating completed assessments of recent social stress and negative affect, then consumed lunch from a multi-item laboratory test meal; in line with the interpersonal model of binge eating, findings revealed that pre-meal state anxiety mediated the relation between recent social stress and palatable food intake (Shank et al., 2017). In another laboratory test meal study, researchers examined the effect of a real-time interpersonal stressor on negative affect and binge eating in a sample of individuals who endorsed recent regular binge eating, and findings suggested that over-consumption or under-consumption of food (i.e., “extreme intake”) was triggered by laboratory-induced interpersonal stress in individuals who binge eat (Russell et al., 2017).
Using EMA, Ranzenhofer et al. (2014) evaluated the temporal associations between interpersonal problems, negative affect, and loss of control eating in a sample of overweight and obese adolescent girls; findings corroborated the predictive value of interpersonal problems for loss of control eating on a momentary level. Ambwani, Roche, Minnick, and Pincus (2015) also used EMA among a non-clinical sample of young adult women with recurrent binge eating and found that that momentary negative affect was associated with momentary binge eating behavior, but average levels of negative affect over the study period were not. This study also revealed that interpersonal problems moderated the relation between negative affect and binge eating; results suggested that those who have a tendency of being too cold and distant from others may be particularly prone to binge eat in response to negative affect.
The Interpersonal Model of Binge Eating and Psychological Treatment
Empirical studies on the interpersonal model have called for the need of future research to use longitudinal designs and clinical samples to evaluate the interpersonal model over the course of psychotherapies, and especially those interpersonal in nature, for EDs (Ivanova et al., 2015, Ivanova et al., 2016). Ivanova et al. (2015) theorized that interpersonal psychotherapies for EDs may be addressing the underlying interpersonal-affective deficits, and in effect reduce ED symptomatology. Thus far, research has provided good support for the interpersonal model of binge eating, however, the mechanisms underlying the model have not been tested longitudinally over the course of any psychotherapy treatment among a clinical sample of adult individuals with BED. Given IPT was developed with the theoretical interpersonal model of binge eating in mind, investigating the model over the course of IPT would be particularly informative. The current study aims to empirically examine the interpersonal model of binge eating over the course of treatment in a clinical sample of individuals with BED who received either IPT or cognitive behavioral therapy (CBT).
According to theoretical principles of the interpersonal model of binge eating, IPT would reduce interpersonal problems, which would lead to decreased negative affect and, in turn, cause a reduction in binge eating and related psychopathology (i.e., solid lines in Figure 2). The theoretical underpinnings of CBT for BED propose that restraint causes binge eating, which leads to more restraint and, in turn, precipitates a cycle of binge eating (Fairburn, Cooper, & Shafran, 2003). CBT interrupts this cycle by attempting to reduce dietary restriction and chaotic eating through behavioral (e.g., promoting eating regular meals and snacks, self-monitoring of behaviors) and cognitive (e.g., restructuring dysfunctional thoughts and beliefs about one’s body weight and shape) interventions in order to reduce binge eating (Fairburn et al., 2003). CBT does not directly address interpersonal problems, whereas IPT does, highlighting an important area for research to determine if change in the mechanisms of the interpersonal model of binge eating depend on treatment type received (i.e., an interpersonal therapy).
Figure 2.
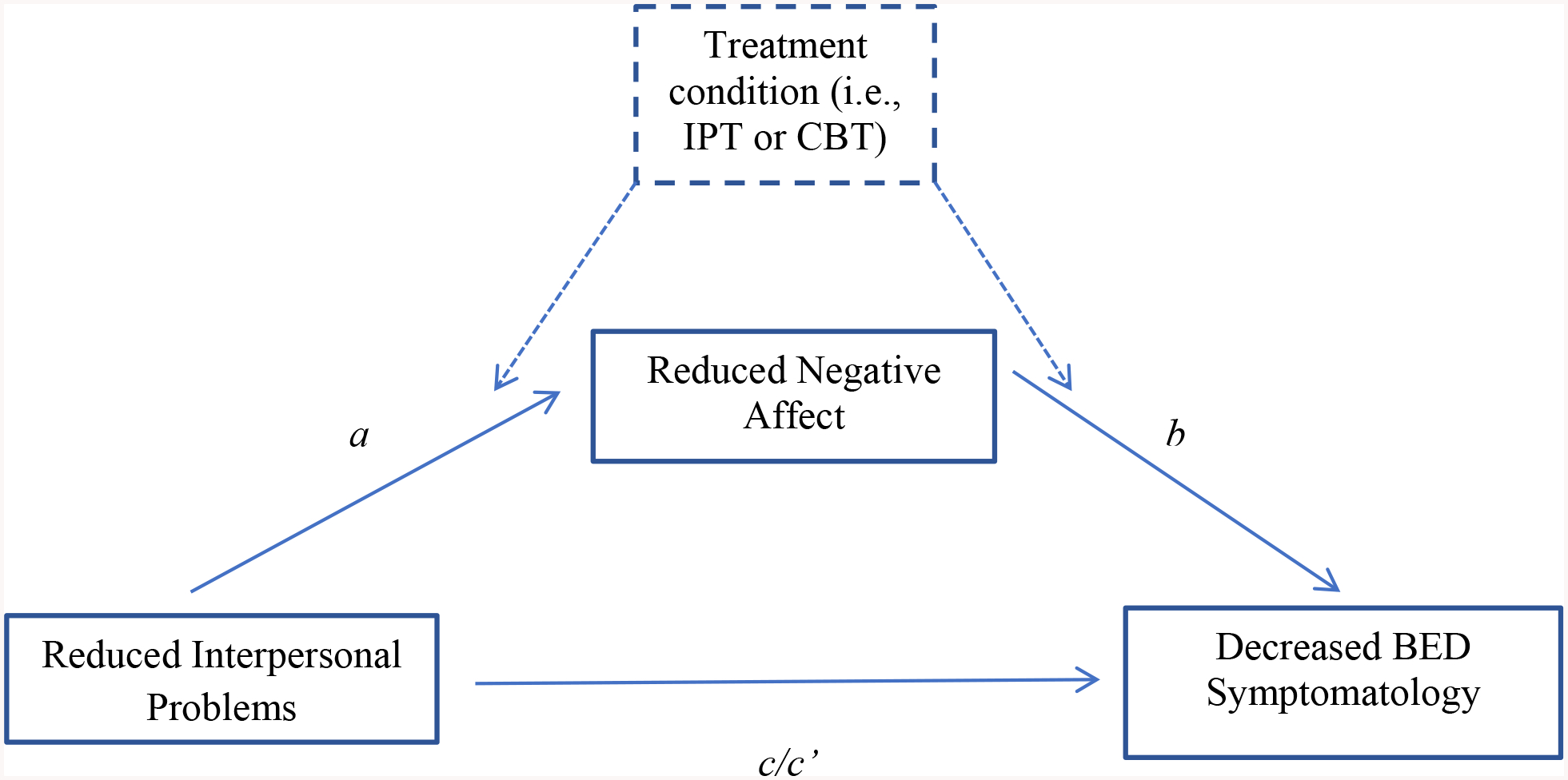
Treatment mediation models of the longitudinal interpersonal model of binge eating and related psychopathology.
Note: the simple mediation model (solid lines) depicts the longitudinal interpersonal model of binge eating symptomatology over the course of psychotherapy treatment; the moderated mediation model (solid + dashed lines) tested whether treatment condition moderated the longitudinal interpersonal model of binge eating symptomatology over the course of psychotherapy. BED= binge eating disorder. IPT=interpersonal psychotherapy. CBT=cognitive behavioral therapy.
The purpose of the current study is to extend the literature by examining the interpersonal model over the course of two different psychotherapy treatments (CBT and IPT) among a clinical sample of adult women and men with BED. This will shed light on whether change in the mechanisms of the interpersonal model of binge eating are driving treatment outcomes (i.e., decreases in interpersonal problems will lead to decreases in negative affect and, in turn, reductions in binge eating). Thus, the primary dependent variable in this study is binge eating. We will secondarily evaluate whether other ED psychopathology outcomes follow this model including restraint, eating concern, shape concern, weight concern, and global ED psychopathology. It is hypothesized that the interpersonal model will be supported. For outcome variables that demonstrate support for the interpersonal model, we will test whether treatment differences exist, hypothesizing that this model will hold more strongly for the IPT treatment group compared to those who received CBT.
Methods
Participants
Participants were 162 individuals with overweight or obesity and BED, and were part of a larger comparative treatment trial examining the use of group CBT and group IPT for the treatment of BED, conducted at Yale University and San Diego State University. Participants were primarily middle-aged (mean age = 43) females (83%), with mean BMI of 37.65, and the majority of whom were married at the time of the study (60%). Most participants identified as White (93%), 4% as African American, 3% as Hispanic, and <1% as American Indian. The majority of participants had a college (45%) or graduate school degree (40%), with a minority whose highest level of education was a high school degree (15%). Additional information on the sample, treatments, and procedures in this study have been described in greater detail in the main outcome paper (see Wilfley et al., 2002) but are also summarized below.
Recruitment was conducted through advertisements targeting “compulsive eating.” Interested individuals contacted the clinics and were preliminarily screened for inclusion criteria which included: Diagnostic and Statistical Manual (DSM)-IV research criteria for BED; being between the ages 18 and 65; having body mass index (BMI) (kg/m2) between 27 and 48 kg/m2; not currently being pregnant or planning to become pregnant; not taking weight-affecting or psychotropic medications; absence of psychiatric conditions warranting immediate treatment (e.g., suicidality, substance dependence, psychotic symptoms); and not currently enrolled in a weight-loss program or psychotherapy.
Procedure
All procedures were approved by both universities’ Institutional Review Boards. Participants completed structured clinical interviews, self-report measures, and anthropometric measures (i.e., height and weight) to confirm eligibility criteria and gather pre-treatment data. Following informed consent, participants were blocked by gender then randomly assigned to either group CBT (n=81) or group IPT (n=81). Post-treatment assessments were administered shortly after the last treatment session.
Treatment
Both treatment groups consisted of 20 weekly 90-minute group meetings, in addition to three individual sessions designed to address each participant’s individual goals and progress. Each group contained nine participants, and groups were led by two therapists. At least one therapist was at the doctoral level, and the other was either at the doctoral level or a clinical psychology doctoral student. To ensure standardization of treatments within and across sites, all therapists followed detailed treatment manuals (Wilfley et al., 1993; Wilfley et al., 2000). Treatment adherence was measured throughout treatment, and treatment integrity was confirmed using blind independent ratings (Wilfley et al., 2002). CBT and IPT for BED are both evidence-based treatments for BED and designed to reduce the frequency of binge eating.
Group CBT.
Group CBT for BED is marked by three phases. The first phase (sessions 1–6) provided education about the CBT model and highlighted the associations between pressures to be thin, restrictive dieting, negative self-talk, low self-esteem, and binge eating. Behavioral strategies (e.g., self-monitoring of eating habits) were used to help patients monitor food intake and encourage healthy and realistic eating patterns. The second phase (sessions 7–13) helped patients learn cognitive skills (e.g., cognitive restructuring) to counter thinking patterns that are thought to prompt binge eating. During the final phase (sessions 14–20), relapse prevention techniques, such as problem solving and coping in vulnerable situations, were presented with the hope of maintaining changes made in treatment.
Group IPT.
IPT for group (Wilfley et al., 2000) is marked by three phases associated with specific tasks and strategies linked to the resolution of a specified problem area. The four problem areas include grief, interpersonal role disputes, role transitions, and interpersonal deficits. The initial phase (sessions 1–5) involves the examination of a patient’s interpersonal history to identify the interpersonal problem area(s) associated with the onset and maintenance of binge-eating symptoms. During the intermediate phase (sessions 6–15), the focus is on implementing strategies to help make changes in identified problem areas. In the final phase (sessions 16–20), patients review and evaluate gains, produce plans for maintaining improvements, and outline remaining work.
Measures
All measures were given at pre-treatment and post-treatment except demographic information, which was only collected at pre-treatment.
Demographics.
Self-report items were used to assess participant demographic characteristics, including: age (in years), BMI, sex, racial/ethnic background (i.e., Non-Hispanic White, African/African American, American Indian), marital status, and years of education.
Interpersonal Problems.
Interpersonal problems were measured using the Inventory of Interpersonal Problems (IIP; Horowitz, Rosenberg, Baer, Ureno, & Villasenor, 1988). The IIP consists of 127 items designed to assess distress related to interpersonal problems and interpersonal functioning. The IIP’s items are measured on a 5-point scale, with higher scores corresponding to great levels of interpersonal problems. The IIP contains a total score and the following eight subscales: domineering, vindictive, cold, social, nonassertive, exploitable, intrusive, and overly nurturant. The current study used the total IIP score. The IIP has been shown to discriminate psychiatric samples from controls, and has adequate test reliability and stability (Woodward, Murrell, & Bettler, 2005).
Negative affect.
The Symptom Checklist-90-Revised (SCL-90-R; Derogatis & Cleary, 1977) was used to measure negative affect. The SCL-90-R is an established self-report instrument that measures psychiatric distress, and consists of a checklist of 90 psychological and physical symptoms. Participants rate their degree of distress associated with each symptom experienced during the past seven days on a 5-point scale, with higher scores reflecting more severe symptomatology. The SCL-90-R has nine subscales: somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. In the current study, the mean ratings of the depression, anxiety, and hostility subscales of the SCL-90-R were used to create a composite score of negative affect. The SCL-90-R has been found to have high internal consistency, test-retest reliability, split-half reliability, and satisfactory validity (Buckelew, Burk, Brownlee-Duffect, & DeGood, 1988; Derogatis & Cleary, 1977; Derogatis, Rickels, & Rock, 1976; Groth-Marnat, 2009).
Binge-eating disorder symptomatology.
The Eating Disorder Examination 12th Edition (EDE; Fairburn & Cooper, 1993) is an interview-based measure of binge eating and ED psychopathology and was conducted by assessors blind to treatment condition. Binge eating, the primary dependent variable, was assessed in terms of the number of objective bulimic episodes (i.e., the consumption of an unusually large amount of food given the circumstances, accompanied by a feeling of loss of control over eating; Fairburn & Cooper, 1993) that had occurred over the past 28 days. ED psychopathology was assessed by the four EDE subscales: restraint, eating concern, shape concern, and weight concern. In addition to the subscales, the EDE has a global score reflecting overall ED psychopathology by averaging the four subscale scores (referred to as global ED psychopathology). The global ED psychopathology subscale and other four subscales are secondary dependent variables. The EDE’s subscale items are measured on a 7-point scale, with higher scores corresponding to great levels of BED psychopathology. The EDE demonstrated good psychometric support in a systematic review, including validity (ability to distinguish cases from non-cases), test-retest reliability, inter-rater reliability, and internal consistency (Berg, Peterson, Frazier, & Crow, 2012).
Data Analyses
All analyses were conducted using SPSS version 25. The simple mediation (solid lines in Figure 2) and moderated mediation (solid + dashed lines in Figure 2) models were examined using the PROCESS macro developed by Hayes (2013). Using bootstrapping procedures in PROCESS, the significance of indirect effects (i.e., mediation effects) was tested. Bias-corrected 95% confidence intervals (CI) were computed using 5,000 bootstrap resamples for each indirect effect estimate. CIs that do not contain a zero value indicate a significant indirect effect. When examining mediation longitudinally with two waves of data, MacKinnon (2008) advocates that one viable option for analysis is using difference scores (where the time 1 value is subtracted from the time 2 value of all mediation variables X, Y, and M). Thus, change in all mediation variables was calculated by subtracting post-treatment values from pre-treatment values. In contrast to mediation methods popularized by Baron and Kenny (1986), Hayes (2009, 2018) indicates the significance or nonsignificance for individual paths (e.g., path a, path b, path c, path c’) in a mediation model is not pertinent or essential to the significance of an indirect effect.
To test the simple mediation model (solid lines in Figure 2), separate ordinary least squares regression (OLS) analyses using PROCESS model 4 (Hayes, 2013) assessed mediating effects of change in negative affect on the association between change in interpersonal problems and change in binge-eating frequency (i.e., primary dependent variable), as well as the following secondary dependent variables: change in global ED psychopathology, change in restraint, change in eating concern, change in shape concern, and change in weight concern. Significance of individual paths in the simple mediation model will be evaluated at the p < .05 level. A significant indirect effect (i.e., mediation effect) will be concluded for CIs that do not contain a zero value, and suggest that the relation between change in interpersonal problems and change in BED symptomatology over the course of treatment is significantly explained by change in negative affect.
Follow-up moderated mediation analyses (solid + dashed lines in Figure 2) will be conducted on significant simple mediation effects to determine if treatment condition moderates the mediated effect of change in interpersonal problems on BED symptomatology improvement through change in negative affect. Separate OLS analyses using PROCESS model 58 (Hayes, 2013) assessed moderated mediation effects of change in negative affect on the association between change in interpersonal problems and change in BED symptomatology variables that were statistically significant based on simple mediation analyses. PROCESS generates an index of moderated mediation, which is a test of the equality of the conditional indirect effects in the two groups. Thus, moderated mediation is thought to occur when the CIs do not contain a zero value. A significant moderated indirect effect would suggest that the pathways of interpersonal model of binge eating during treatment course differed as a function of treatment condition.
In terms of power, Fritz and MacKinnon (2007) examined six methods of examining mediation (i.e., Baron and Kenny’s causal-steps test, joint significance test, Sobel first-order test, product confidence limits for the indirect effect [PRODCLIN], percentile bootstrap, and bias-corrected bootstrap) and reported on the necessary sample sizes needed for each of these approaches to detect an effect. Findings demonstrated that results for the bias-corrected bootstrap method showed it to consistently be the most powerful of all of the methods. Using the bias-corrected bootstrap method, results showed that to achieve a power of 0.8, with medium effects of the a and b pathways, approximately 71 participants were determined to be needed to detect a significant mediation effect (Fritz & MacKinnon, 2007). In line with this finding, the current study’s sample size of 159 participants suggests the analyses in this study are adequately powered.
Results
Three participants were missing baseline data and were therefore excluded from the analyses of the current study resulting in a sample size of 159 individuals. There were no significant differences between treatment groups on any demographic variable (e.g., gender, age, BMI, race, marital status, and education) or prevalence of comorbid psychiatric disorder (Wilfley et al., 2002). Table 1 demonstrates means and standard deviations for all study variables at pre-treatment and post-treatment. As expected, all variables significantly (i.e., p < .05) decreased from pre-treatment to post-treatment.
Table 1.
Paired sample t-test results comparing means and standard deviations of study variables at pre-treatment and post-treatment.
| Dependent Variable | Pre-treatment Mean (SD) | Post-treatment Mean (SD) | t statistic, significance level | Cohen’s d |
|---|---|---|---|---|
| IIP total | 1.17(.59) | .98 (.56) | t(145)=4.63, p<.01* | .37 |
| Negative affect | 42.04 (6.80) | 35.51 (6.07) | t(145)=11.90, p<.01* | .94 |
| Binge-eating frequency | 20.65 (11.98) | .85 (2.56) | t(157)=20.41, p<.01* | 1.62 |
| Global ED psychopathology | 2.80 (.75) | 1.41 (.68) | t(154)=21.15, p<.01* | 1.68 |
| Restraint | 1.96 (1.25) | 1.25 (1.05) | t(157)=6.50, p<.01* | .52 |
| Eating concern | 2.27 (1.35) | .65 (.78) | t(157)=15.39, p<.01* | 1.22 |
| Shape concern | 3.81 (.98) | 2.36 (1.25) | t(157)=14.49, p<.01* | 1.15 |
| Weight concern | 3.25 (1.10) | 2.07 (1.18) | t(157)=10.55, p<.01* | .84 |
p<.05
SD = standard deviation; IIP = inventory of interpersonal problems; ED = eating disorder.
Table 2 presents the beta coefficients of the bootstrapping procedures that were used to test the significance of the indirect effect for the simple mediation model of the longitudinal interpersonal model of binge eating over the course of psychotherapy treatment (solid lines in Figure 2). Change in negative affect was assessed as the mediator of change in interpersonal problems and change in binge-eating frequency and other BED psychopathology variables. Significant bootstrapped indirect effects were found for the following dependent variables (Table 2): the primary dependent variable of binge-eating (95% CI [0.48, 5.91]), and secondary dependent variables of global ED psychopathology (95% CI [0.08, 0.42]), shape concern (95% CI [0.11, 0.67), weight concern (95% CI [0.02, 0.65]). These results suggest that the change in negative affect mediated the relation between change in interpersonal problems and change in binge-eating frequency, global ED psychopathology, shape concern and weight concern. Change in negative affect did not emerge as a mediator between change in interpersonal problems and change in restraint or eating concern, which were secondary dependent variables.
Table 2.
Regression analyses of simple mediation: The longitudinal interpersonal model of binge eating and related psychopathology over the course of psychotherapy treatment (solid lines in Figure 2).
| Dependent variable: | Effect of IIP total on NA (path a) | Effect of NA on DV (path b) | Total Effect (path c) | Direct Effect (path c’) | Indirect Effect (a X b) | 95% CI for Indirect Effect |
|---|---|---|---|---|---|---|
| Primary dependent variable: | ||||||
| Binge-eating frequency n =145 | 6.69* | .38* | −1.35 | −3.87 | 2.52* | (.48, 5.91) |
| Secondary dependent variables: | ||||||
| Global ED psychopathology n =143 | 6.69* | .03* | .39* | .17 | .22* | (.08, .42) |
| Restraint n = 145 | 6.69* | .03 | −.03 | −.25 | .22 | (−.07, .55) |
| Eating concern n =145 | 6.69* | .03 | .48* | .31 | .17 | (−.08, .46) |
| Shape concern n =145 | 6.69* | .05* | .53* | .19 | .34* | (.11, .67) |
| Weight concern n =145 | 6.69* | .04* | .67* | .39 | .28* | (.02, .65) |
p<.05;
p<.07
DV=dependent variable; IIP=inventory of interpersonal problems; ED=eating disorder; CI=confidence interval; NA = negative affect; Bolded CIs indicate a significant indirect effect.
Significant indirect effects from the simple mediation model were followed up with a test of moderated mediation (i.e., index of moderated mediation) to determine whether the pathways of the interpersonal model of binge eating depended upon psychotherapy received (i.e., CBT or IPT). Table 3 presents the beta coefficients of the moderated mediation model (solid + dashed lines in Figure 2). The index of moderated mediation for all outcome variables contained a zero value (Table 3), indicating the longitudinal model of binge eating did not significantly differ as a function of treatment condition for any outcome. However, the separate within group conditional indirect effects were differentially significant for binge eating and shape concern for those in IPT, and were differentially significant for weight concern for those who received CBT.
Table 3.
Bootstrapped regression analyses of moderated mediation: Treatment condition moderates the longitudinal interpersonal model of binge eating and related psychopathology over the course of psychotherapy treatment (solid + dashed lines in Figure 2).
| Dependent variable | Treatment type | Effect | Bootstrapped | ||
|---|---|---|---|---|---|
| SE | 95% CI | 95% CI for Index of Moderated Mediation | |||
| Primary dependent variable: | |||||
| Binge-eating frequency n =145 | CBT | 1.72 | 1.60 | (−.48, 6.13) | (−3.35, 6.48) |
| IPT | 3.13 | 2.15 | (.04, 8.23) | ||
| Secondary dependent variables: | |||||
| Global ED psychopathology n =143 | CBT | .17 | .09 | (.02, .38) | (−.20, .40) |
| IPT | .24 | .13 | (.05, .57) | ||
| Shape concern n =145 | CBT | .26 | .17 | (−.02, .63) | (−.35, .64) |
| IPT | .39 | .21 | (.09, .87) | ||
| Weight concern n =145 | CBT | .30 | .18 | (.02, .73) | (−.55, .47) |
| IPT | .24 | .22 | (−.09, .79) | ||
ED=eating disorder; SE=standard error; CI=confidence interval; Bolded CIs indicate a significant indirect effect.
Discussion
The present study examined the interpersonal model of binge eating and associated psychopathology over the course of two psychotherapy treatments (CBT and IPT) among a clinical sample of adult women and men with BED. This is the first study to examine the interpersonal model over the course of any psychotherapy treatment. It is important to highlight a significant limitation of the current study’s analytic plan. To truly determine cause inherent in mediation, the independent variable must temporally precede the mediator variable, and the mediator variable must temporally precede the dependent variable (Maxwell, Cole, & Mitchell, 2011). In other words, effect must come after cause. Because of study design limitations, the current study is unable to examine the interpersonal model of binge eating consistent with the most robust way to examine mediation such that variables do not overlap in time. Although this analytical shortcoming limits our ability to conclude causation, this method can preliminarily shed light on associations of mediation and provide justification for future research to more robustly investigate the casual pathways of the mediation model (MacKinnon, 2008).
Despite these analytic limitations, results suggested the interpersonal model of binge eating was supported for reductions in binge eating, the primary dependent variable, as well as some secondary dependent variables including global ED psychopathology, shape concern, and weight concern. Given the interpersonal model was theorized specifically to predict binge eating, this finding corroborates theory. Moreover, global ED psychopathology, shape concern, and weight concern all seem to have body image in common – potentially, treatment successfully reduces body image dissatisfaction, in addition to binge eating, through the mechanisms of the interpersonal model. Secondary outcome variables restraint and eating concern were not supported within the interpersonal model. It is possible that restraint was not significant due to a floor effect; at pre-treatment, participants reported relatively low levels of restraint (see Table 1), and even though mean levels decreased statistically by post-treatment, perhaps the limited range of data reduced variability and prohibited finding a statistical effect. Lastly, perhaps the eating concern subscale did not emerge as a significant outcome since the focus of both treatments is on reducing binge eating instead of broader eating concern, which is what is assessed in this EDE subscale.
Significant BED symptomatology variables (i.e., change in binge-eating frequency, global ED psychopathology, shape concern, weight concern) were followed-up with using moderated mediation analyses to determine if treatment effects existed, such that treatment type received differentially impacted the significance of the interpersonal model of binge eating. It was hypothesized that moderated mediation would occur such that IPT would produce greater support for the interpersonal model of binge eating given this treatment more directly addresses the interpersonal context in which binge eating occurs. This hypothesis was not fully supported; the index of moderated mediation was not significant for any of the outcome variables evaluated. However, the separate within-group indirect effects were differentially significant for IPT for outcome variables binge eating (i.e., the primary dependent variable) as well as shape concern, while outcome variable weight concern was differentially significant for CBT. It is possible weight concern emerged stronger for CBT because CBT has participants directly confront attitudes and disturbances about their weight, or because patients could have experienced weight stability through normalization of eating patterns. Although analyses for simple mediation were adequately powered in this study (Fritz & MacKinnon, 2007), it is possible that the moderated mediation analyses might have been underpowered. Perhaps moderated mediation findings may have been statistically significant with greater power given the difference in significance between IPT and CBT in the within-group indirect effects for change in binge-eating frequency, shape concern, and weight concern; however, these differential within-group indirect effects should be interpreted with caution given the index of moderated mediation was not significant. In fact, moderated mediation findings suggest little difference in the interpersonal model between IPT and CBT, and point to overall support for the model across treatments which suggests both treatments addressed negative affect and interpersonal precipitants to eating disorder symptomatology, although likely through different treatment strategies. For example, CBT targeted triggers for binge eating, which are often related to interpersonal problems and negative affect, and helps patients cope better by improved problem solving to these binge eating precipitants. IPT, on the other hand, targeted changing interpersonal patterns and intervening within the interpersonal context in which the eating disorder was maintained.
The findings of this study are in line with previous research demonstrating support for the interpersonal model of binge eating, and extend past findings by using a longitudinal model over the course of treatment. Findings of the current study provide support, for the first time, that psychotherapy produces changes in the mechanisms of the interpersonal model of binge eating as theoretically proposed; change in negative affect was found to mediate reductions in interpersonal problems and reductions in binge eating, global ED psychopathology, shape concern, and weight concern over the course of treatment. These results preliminarily provide support for a treatment mediator and suggest that one way individuals improve through psychotherapy is through the “active therapeutic components” of reductions in interpersonal problems and negative affect. Findings support the notion that it is important to help patients with BED reduce interpersonal problems and negative affect, which leads to amelioration of binge eating and some aspects of BED psychopathology.
The current study is significant as it increases our mechanistic knowledge of BED treatment by identifying a potential treatment mediator. Although decades of research have been devoted to evaluating and establishing the effectiveness of psychological treatments, a paucity of research attention has been given to understanding the mechanisms or targets by which evidence-based treatments for EDs achieve their effects (Kraemer, Wilson, Fairburn, & Agras, 2002). The field’s lack of understanding in this domain is detrimental considering few evidence-based treatments for EDs exist, and even the best treatments with strong research support have limited efficacy. Treatment may be enhanced by better understanding mediators by strengthening the “active elements” of treatment, or treatment targets, and reducing other components not found to be a key mechanism of therapeutic change (Kraemer, 2016); this would likely yield larger treatment effect sizes and help more individuals struggling with an ED to reach recovery or remission (Kraemer et al., 2002), which is especially important given research findings that suggest many of those with an ED struggle with the illness for many years, often even after receiving psychological treatment (Kordy et al., 2002). Results from this paper preliminarily provide support for theoretical model of the interpersonal model of binge eating, as significant mediation associations were found.
Future studies could examine the impact of fostering more potent change in interpersonal problems and negative affect to examine if even more emphasis on these core areas during treatment would result in enhanced patient outcomes or foster higher rates of ED remission and recovery. Notably, CBT for EDs developer Dr. Fairburn and his colleagues produced an improved, transdiagnostic version of the treatment entitled enhanced CBT, or CBT-E (Fairburn et al., 2003; Fairburn, Cooper, Shafran, Bohn, & Hawker, 2008). CBT-E expanded to include additional treatment components that address interpersonal problems as well as low self-esteem, clinical perfectionism, and mood intolerance. Data collection in this study pre-dated CBT-E and, thus, interpersonal problems were only directly addressed in IPT. Future studies should also investigate the interpersonal model of binge eating over the course of CBT-E given this treatment’s added focus on interpersonal problems. Lastly, since IPT and CBT both work similarly well in the short- and long-term (i.e., immediately, 1 year, and even 5 years following treatment; Hilbert et al., 2012; Wilfley et al., 2002) and have at least some similar mechanisms of action, such as this study demonstrated, it would likely be helpful for future research to try to identify treatment moderators, or factors that may help select which treatment works best for whom or under what conditions a treatment works best; it is possible that those who are more aware of their thoughts and enjoy using a cognitive framework may be better suited for CBT, or perhaps those who strongly value social relationships and do not want to directly talk about eating disorder symptoms are better off receiving IPT. In addition to better understanding treatment moderators and mechanisms, it is also important to consider which psychological problems a treatment addresses, as well as it’s disseminability. For instance, IPT is considered a “best buy” treatment because it is feasible to disseminate (Kazdin, Fitzsimmons-Craft, & Wilfley, 2017) and has demonstrated efficacy for a wide range of psychological problems and patient populations, including (but not limited to) depression, eating disorders, anxiety disorders, post-traumatic stress disorder, and the prevention of mood disorders in pregnant and postpartum women (Cuijpers, Donker, Weissman, Ravitz, & Cristea, 2016; U.S. Preventive Services Task Force, 2018).
EMA is another important future direction that could shed light on how variables change momentarily within the interpersonal model of binge eating framework (or other treatment mediator models) over the course of treatment. Ambwani et al. (2015) found that momentary negative affect was associated with binge eating behavior, but average levels of negative affect over the study period were not, which highlights that momentary data could provide important insight on factors that lead to binge eating that aggregated data potentially masks. EMA could also help researchers understand how treatment influences and changes negative affect, interpersonal problems, and BED symptomatology on a momentary level. Relatedly, Wilson, Fairburn, Agras, Walsh, and Kraemer (2002) advise that studies interested in investigating mediators of treatment must include measures of proposed mechanisms early during treatment and asses these constructs often throughout course, such as on a session-by-session basis. These researchers highlight that past work has assessed putative mediations first at midtreatment in an attempt to explain end-of-treatment outcomes, yet, much of the therapeutic change already has occurred by midtreatment (Wilson et al., 2002). Failure to capture the change in proposed mediator variable while it occurs makes it difficult to differentiate cause from consequence and explain post-treatment effects.
Strengths of this study include the clinical sample with both males and females, and the longitudinal design. Using an interview-based measure of ED symptomatology rather than a self-report measure is also a strength. As previously discussed, a major limitation of the study includes the lack of multiple time points of all study variables throughout the course of treatment which would have allowed for mediation analyses with variables that did not overlap in time, which is the best way to understand true temporal associations (Cole & Maxwell, 2003). However, it is noteworthy that mediation analytic approaches similar to the current study’s analytic plan have been used within the literature (e.g., Altman et al., 2015, Hayes et al., 2016, Holland et al., 2014, Russell et al., 2017; Sauer-Zavala et al., 2017). This study weakness limits the interpretation of results in terms of definitively concluding mediation, as true mediation inherently tests causation which we were unable to examine due to study design. Thus, although the analytic plan in the current study is not conclusive in determining mediation within the interpersonal model of binge eating, the current study’s findings are an important contribution in longitudinally providing support for this theoretical model. Given this limitation, future research should replicate this study and investigate causation of the interpersonal model of binge eating during treatment course by including multiple data collection time points, such as during every session, within the course of treatment in order to have variables that do not overlap in time and capture change in mechanisms as it occurs. It may also be of value for future research to replicate this study using a sample of individuals high in interpersonal problems, as less than half (i.e., 41%) of the current sample met the clinical cutoff (Hansen & Lambert, 1996) for high interpersonal problems.
In conclusion, the current study provided preliminary support that psychotherapy treatment addresses the mechanisms of the interpersonal model of binge eating as theoretically proposed; over the course of treatment, reductions in negative affect were found to mediate changes in interpersonal problems and decreases in the primary outcome of binge eating, as well as the secondary dependent variables including global ED psychopathology, eating concern, and weight concern. Pathways of the interpersonal model of binge eating during treatment course did not significantly differ as a function of treatment condition. This suggests changes in the mechanisms of the model seem to occur in both IPT and CBT, and additional research is needed to better understand whether treatment differences exist for the interpersonal model of binge eating, as well as to further explore the casual mechanisms of this theory.
Highlights:
Results provided preliminary support that interpersonal psychotherapy and cognitive behavioral therapy targeted the mechanisms of the interpersonal model of binge eating as theoretically proposed in terms of the primary dependent variable of binge eating, as well as secondary dependent variables including global eating disorder psychopathology, shape concern, and weight concern.
Results did not indicate support that interpersonal psychotherapy and cognitive behavioral therapy targeted the mechanisms of the interpersonal model of binge eating as theoretically proposed in terms of some secondary dependent variables including restraint or eating concern.
Findings suggest overall preliminary support for the interpersonal model of binge eating for both interpersonal psychotherapy and cognitive behavioral therapy, as moderated mediation analyses did not reveal significant treatment differences.
Acknowledgments
This research was supported by grants R29MH51384, R29MH138403, 5T32HL007456, 1T32HL13035, and K23DK114480 from the National Institute of Health.
Footnotes
Conflict of interest statement: Anna M. Karam, Dawn M. Eichen, PhD, and Ellen E. Fitzsimmons-Craft have no conflicts of interest or commercial relationships related to this paper to report. Denise E. Wilfley has received an educational grant from Shire Pharmaceuticals to develop an interpersonal psychotherapy online training platform.
References
- Altman M, Holland JC, Lundeen D, Kolko RP, Stein RI, Saelens BE, … Epstein LH (2015). Reduction in Food Away from Home Is Associated with Improved Child Relative Weight and Body Composition Outcomes and This Relation Is Mediated by Changes in Diet Quality. Journal of the Academy of Nutrition and Dietetics. 115, 1400–1407. 10.1016/j.jand.2015.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ambwani S, Roche MJ, Minnick AM, & Pincus AL (2015). Negative affect, interpersonal perception, and binge eating behavior: An experience sampling study. International Journal of Eating Disorders, 48, 715–726. 10.1002/eat.22410 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5). Washington, DC: American Psychiatric Pub. [Google Scholar]
- Ansell EB, Grilo CM, & White MA (2012). Examining the interpersonal model of binge eating and loss of control over eating in women. International Journal of Eating Disorders, 45, 43–50. 10.1002/eat.20897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of personality and social psychology, 51, 1173–1182. 10.1037/0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- Berg KC, Cao L, Crosby RD, Engel SG, Peterson CB, Crow SJ, … & Wonderlich SA (2017). Negative affect and binge eating: Reconciling differences between two analytic approaches in ecological momentary assessment research. International Journal of Eating Disorders, 50, 1222–1230. 10.1002/eat.22770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KC, Peterson CB, Frazier P, & Crow SJ (2012). Psychometric evaluation of the Eating Disorder Examination and Eating Disorder Examination-Questionnaire: A systematic review of the literature. International Journal of Eating Disorders, 45, 428–438. doi: 10.1002/eat.20931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blomquist KK, Ansell EB, White MA, Masheb RM, & Grilo CM (2012). Interpersonal problems and developmental trajectories of binge eating disorder. Comprehensive Psychiatry, 53, 1088–1095. 10.1016/j.comppsych.2012.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckelew SP, Burk JP, Brownlee-Duffeck M, Frank RG, & DeGood D (1988). Cognitive and somatic aspects of depression among a rehabilitation sample: Reliability and validity of SCL-90-R research subscales. Rehabilitation Psychology, 33, 67–75. doi: 10.1037/h0091679 [DOI] [Google Scholar]
- Cole DA, & Maxwell SE (2003). Testing mediational models with longitudinal data: questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology, 112, 558–577. doi: 10.1037/0021-843X.112.4.558 [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Donker T, Weissman MM, Ravitz P, & Cristea IA (2016). Interpersonal psychotherapy for mental health problems: A comprehensive meta-analysis. American Journal of Psychiatry, 173, 680–687. 10.1176/appi.ajp.2015.15091141 [DOI] [PubMed] [Google Scholar]
- Derogatis LR, & Cleary PA (1977). Confirmation of the dimensional structure of the SCL-90: a study in construct validation. Journal of Clinical Psychology, 33, 981–989. [DOI] [Google Scholar]
- Derogatis LR, Rickels K, & Rock AF (1976). The SCL-90 and the MMPI: a step in the validation of a new self-report scale. The British Journal of Psychiatry, 128, 280–289. 10.1192/bjp.128.3.280 [DOI] [PubMed] [Google Scholar]
- Duchesne M, de Oliveira Falcone EM, de Freitas SR, d’Augustin JF, Marinho V, & Appolinario JC (2012). Assessment of interpersonal skills in obese women with binge eating disorder. Journal of Health Psychology, 17, 1065–1075. doi: 10.1177/1359105311432326 [DOI] [PubMed] [Google Scholar]
- Elliott CA, Tanofsky-Kraff M, Shomaker LB, Columbo KM, Wolkoff LE, Ranzenhofer LM, & Yanovski JA (2010). An examination of the interpersonal model of loss of control eating in children and adolescents. Behaviour Research and Therapy, 48, 424–428. 10.1016/j.brat.2009.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, & Cooper Z (1993). The Eating Disorder Examination (12th Edition). In Fairburn CG & Wilson GT (Eds.), Binge Eating: Nature, Assessment, and Treatment.(pp. 317–360). New York, NY: Guilford Press. [Google Scholar]
- Fairburn CG, Cooper Z, & Shafran R (2003). Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behaviour research and therapy, 41, 509–528. 10.1016/S0005-7967(02)00088-8 [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R, Bohn K, & Hawker DM (2008). Clinical perfectionism, core low self-esteem and interpersonal problems In Cognitive behavior therapy and eating disorders. (pp. 197–220). New York, NY: Guilford Press. [Google Scholar]
- Fritz MS, & MacKinnon DP (2007). Required sample size to detect the mediated effect. Psychological science, 18, 233–239. 10.1111/j.14679280.2007.01882.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groth-Marnat G (2009). Handbook of psychological assessment, 5th ed Hoboken, NJ: John Wiley & Sons Inc. [Google Scholar]
- Haedt-Matt AA, & Keel PK (2011). Revisiting the affect regulation model of binge eating: a meta-analysis of studies using ecological momentary assessment. Psychological Bulletin, 137, 660–681. doi: 10.1037/a0023660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen NB, & Lambert MJ (1996). Brief report: Assessing clinical significance using the Inventory of Interpersonal Problems. Assessment, 3, 133–136. 10.1177/107319119600300204 [DOI] [Google Scholar]
- Hartmann A, Zeeck A, & Barrett MS (2010). Interpersonal problems in eating disorders. International Journal of Eating Disorders, 43, 619–627. 10.1002/eat.20747 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs, 76, 408–420. 10.1080/03637750903310360 [DOI] [Google Scholar]
- Hayes AF (2013). Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: The Guilford Press. [Google Scholar]
- Hayes AF (2018). Partial, conditional, and moderated moderated mediation: Quantification, inference, and interpretation. Communication Monographs, 85, 4–40. 10.1080/03637751.2017.1352100 [DOI] [Google Scholar]
- Hayes JF, Altman M, Kolko RP, Balantekin KN, Holland JC, Stein RI, … & Epstein LH (2016). Decreasing food fussiness in children with obesity leads to greater weight loss in family-based treatment. Obesity, 24, 2158–2163. 10.1002/oby.21622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbert A, Bishop ME, Stein RI, Tanofsky-Kraff M, Swenson AK, Welch RR, & Wilfley DE (2012). Long-term efficacy of psychological treatments for binge eating disorder. The British Journal of Psychiatry, 200, 232–237. 10.1192/bjp.bp.110.089664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland JC, Kolko RP, Stein RI, Welch RR, Perri MG, Schechtman KB, … Wilfley DE (2014). Modifications in parent feeding practices and child diet during family-based behavioral treatment improve child zBMI. Obesity, 22, E119–E126. doi: 10.1002/oby.20708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz LM, Rosenberg SE, Baer BA, Ureño G, & Villaseñor VS (1988). Inventory of interpersonal problems: psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology, 56, 885–892. doi: 10.1037/0022-006X.56.6.885. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry, 61, 348–358. 10.1016/j.biopsych.2006.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanova IV, Tasca GA, Hammond N, Balfour L, Ritchie K, Koszycki D, & Bissada H (2015). Negative affect mediates the relationship between interpersonal problems and binge-eating disorder symptoms and psychopathology in a clinical sample: A test of the interpersonal model. European Eating Disorders Review, 23, 133–138. 10.1002/erv.2344 [DOI] [PubMed] [Google Scholar]
- Ivanova IV, Tasca GA, Proulx G, & Bissasda H (2016). Contribution of Interpersonal Problems to Eating Disorder Psychopathology via Negative Affect in Treatment-seeking Men and Women: Testing the Validity of the Interpersonal Model in an Understudied Population. Clinical Psychology & Psychotherapy. 24, 952–964. 10.1002/cpp.2060. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Fitzsimmons CEE, & Wilfley DE (2017). Addressing critical gaps in the treatment of eating disorders. International Journal of Eating Disorders, 50, 170–189. doi: 10.1002/eat.22670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenardy J, Arnow B, & Agras WS (1996). The aversiveness of specific emotional states associated with binge-eating in obese subjects. Australian and New Zealand Journal of Psychiatry, 30, 839–844. 10.3109/00048679609065053 [DOI] [PubMed] [Google Scholar]
- Klerman GL, Weissman MM, Rounsaville BJ, & Chevron ES (1984). Interpersonal psychotherapy of depression. New York, NY: Basic Books, Inc. [Google Scholar]
- Kordy H, Krämer B, Palmer RL, Papezova H, Pellet J, Richard M, … & Action COST (2002). Remission, recovery, relapse, and recurrence in eating disorders: conceptualization and illustration of a validation strategy. Journal of Clinical Psychology, 58, 833–846. 10.1002/jclp.2013 [DOI] [PubMed] [Google Scholar]
- Kraemer HC (2016). Messages for clinicians: moderators and mediators of treatment outcome in randomized clinical trials. American Journal of Psychiatry, 173, 672–679. 10.1007/978-981-287-087-2_71-1 [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, & Agras WS (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of general psychiatry, 59, 877–883. 10.1001/archpsyc.59.10.877 [DOI] [PubMed] [Google Scholar]
- Lo Coco G, Sutton R, Tasca GA, Salerno L, Oieni V, & Compare A (2016). Does the Interpersonal Model Generalize to Obesity Without Binge Eating?. European Eating Disorders Review, 24, 391–398. 10.1002/erv.2459 [DOI] [PubMed] [Google Scholar]
- MacKinnon DP (2008). Longitudinal mediation analysis In MacKinnon DP (Ed.), Introduction to statistical mediation analysis (pp. 193–236). New York, NY: Lawrence Erlbaum Associates. [Google Scholar]
- Masheb RM, & Grilo CM (2006). Emotional overeating and its associations with eating disorder psychopathology among overweight patients with binge eating disorder. International Journal of Eating Disorders, 39, 141–146. 10.1002/eat.20221 [DOI] [PubMed] [Google Scholar]
- Maxwell SE, & Cole DA (2007). Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods, 12, 23–44. doi: 10.1037/1082-989X.12.1.23 [DOI] [PubMed] [Google Scholar]
- Maxwell SE, Cole DA, & Mitchell MA (2011). Bias in cross-sectional analyses of longitudinal mediation: Partial and complete mediation under an autoregressive model. Multivariate Behavioral Research, 46, 816–841. doi: 10.1080/00273171.2011.606716 [DOI] [PubMed] [Google Scholar]
- Ranzenhofer LM, Engel SG, Crosby RD, Anderson M, Vannucci A, Cohen LA, … & Tanofsky-Kraff M (2014). Using ecological momentary assessment to examine interpersonal and affective predictors of loss of control eating in adolescent girls. International Journal of Eating Disorders, 47, 748–757. 10.1002/eat.22333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell SL, Haynos AF, Crow SJ, & Fruzzetti AE (2017). An experimental analysis of the affect regulation model of binge eating. Appetite, 110, 44–50. 10.1016/j.appet.2016.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauer-Zavala S, Boswell JF, Bentley KH, Thompson-Hollands J, Farchione TJ, & Barlow DH (2018). Expectancies, working alliance, and outcome in transdiagnostic and single diagnosis treatment for anxiety disorders: An investigation of mediation. Cognitive Therapy and Research, 42, 135–145. 10.1007/s10608-017-9855-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shank LM, Crosby RD, Grammer AC, Shomaker LB, Vannucci A, Burke NL, … & Yanovski JA (2017). Examination of the interpersonal model of loss of control eating in the laboratory. Comprehensive psychiatry, 76, 36–44. 10.1016/j.comppsych.2017.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E (2002). Risk and maintenance factors for eating pathology: a meta-analytic review. Psychological Bulletin, 128, 825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- Stice E, & Agras WS (1999). Subtyping bulimic women along dietary restraint and negative affect dimensions. Journal of Consulting and Clinical Psychology, 67, 460–469. doi: 10.1037/0022-006X.67.4.460 [DOI] [PubMed] [Google Scholar]
- Stice E, Gau JM, Rohde P, & Shaw H (2017). Risk factors that predict future onset of each DSM–5 eating disorder: Predictive specificity in high-risk adolescent females. Journal of Abnormal Psychology, 126, 38–51. https://doiorg.libproxy.wustl.edu/10.1037/abn0000219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan HS (1953). The interpersonal theory of psychiatry. New York, NY: WW Norton & Co. [Google Scholar]
- Svaldi J, Dorn C, & Trentowska M (2011). Effectiveness for interpersonal problem-solving is reduced in women with binge eating disorder. European Eating Disorders Review, 19, 331–341. 10.1002/erv.1050 [DOI] [PubMed] [Google Scholar]
- Tasca GA, Balfour L, Presniak MD, & Bissada H (2012). Outcomes of specific interpersonal problems for binge eating disorder: Comparing group psychodynamic interpersonal psychotherapy and group cognitive behavioral therapy. International Journal of Group Psychotherapy, 62, 197–218. 10.1521/ijgp.2012.62.2.197 [DOI] [PubMed] [Google Scholar]
- Ung EM, Erichsen CB, Poulsen S, Lau ME, Simonsen S, & Davidsen AH (2017). The association between interpersonal problems and treatment outcome in patients with eating disorders. Journal of eating disorders, 5, 53–62. doi: 10.1186/s40337-017-0179-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force (2018). Draft Recommendation Statement: Perinatal Depression: Preventive Interventions. August 2018. Retrieved from: https://www.uspreventiveservicestaskforce.org/Page/Document/draft-recommendation-statement/perinatal-depression-preventive-interventions
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063–1070. doi: 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Watson D, & Tellegen A (1985). Toward a consensual structure of mood. Psychological Bulletin, 98, 219–235. doi: 10.1037/0033-2909.98.2.219 [DOI] [PubMed] [Google Scholar]
- Whisman MA, Dementyeva A, Baucom DH, & Bulik CM (2012). Marital functioning and binge eating disorder in married women. International Journal of Eating Disorders, 45, 385–389. 10.1002/eat.20935 [DOI] [PubMed] [Google Scholar]
- Wilfley DE, Agras WS, Telch CF, Rossiter EM, Schneider JA, Cole AG, … & Raeburn SD (1993). Group cognitive-behavioral therapy and group interpersonal psychotherapy for the nonpurging bulimic individual: a controlled comparison. Journal of Consulting and Clinical Psychology, 61, 296–305. doi: 10.1037/0022-006X.61.2.296 [DOI] [PubMed] [Google Scholar]
- Wilfley DE, MacKenzie RK, Welch RR, Ayres VE, & Weissman MM (2000). Interpersonal Psychotherapy for Group. New York, NY: Basic Books. [Google Scholar]
- Wilfley DE, Welch RR, Stein RI, Spurrell EB, Cohen LR, Saelens BE, … & Matt GE (2002). A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Archives of General Psychiatry, 59, 713–721. 10.1001/archpsyc.59.8.713 [DOI] [PubMed] [Google Scholar]
- Wilson GT, Fairburn CC, Agras WS, Walsh BT, & Kraemer H (2002). Cognitive behavioral therapy for bulimia nervosa: Time course and mechanisms of change. Journal of consulting and clinical psychology, 70, 267–274. doi: 10.1037/0022-006X.70.2.267 [DOI] [PubMed] [Google Scholar]
- Woodward LE, Murrell SA, & Bettler RJ (2005). Stability, reliability, and norms for the Inventory of Interpersonal Problems. Psychotherapy Research, 15, 272–286. doi: 10.1080/10503300512331334977 [DOI] [PubMed] [Google Scholar]


