Abstract
Genome-wide polygenic scores (GPSs) integrate information from many common DNA variants into a single measure of inherited susceptibility, and can identify individuals who are at substantially elevated risk of developing important common diseases.1,2 For coronary artery disease, about 8% of the population can be identified who are at triple the normal risk based on genetic variation alone.1 Among these high polygenic score individuals, adherence to a healthy lifestyle or use of statins may offset increased inherited risk.2,3
Journal Subject Terms: Coronary Artery Disease, Secondary Prevention, Genetics, Genetic, Association Studies, Risk Factors
Keywords: genetic epidemiology, genetics, genome, coronary artery disease
While prior studies have demonstrated that GPSs predict prevalent and new-onset cardiovascular disease events,1,2 the utility of GPSs for risk stratification in a secondary prevention population is uncertain. For example, one prior study that focused on a single common DNA variant in the 9p21 genetic locus strongly associated with new-onset cardiovascular disease noted no such association with events in a secondary prevention cohort.2 Here, we examined the ability of the GPS to predict major adverse cardiovascular events among high-risk vascular disease patients, and assessed whether the GPS can be used to identify a subgroup of individuals who derive benefit from a cholesteryl ester transfer inhibitor.
The ACCELERATE trial recruited 12,092 patients to test whether evacetrapib, a cholesteryl ester transfer protein inhibitor, could reduce the risk of major cardiovascular events compared to placebo among patients with pre-existing vascular disease.3 Within the overall trial, evacetrapib did not alter the rates of incident major adverse cardiovascular events – hazard ratio 1.01 (95% confidence interval 0.91 to 1.11). A nested case-control cohort of 1437 patients with a major cardiovascular event observed in trial follow up – including death from cardiovascular causes, myocardial infarction, stroke, coronary revascularization, or hospitalization for unstable angina – and 1547 matching controls underwent genotyping as part of a previously described genomics substudy.3 Approval was obtained from local institutional review boards and all patients enrolled in the ACCELERATE trial provided written informed consent.
Here, we present the result of two additional analyses within this nested case-control genomics substudy. First, we determined the association of a GPS with major cardiovascular events. Second, we assessed whether the efficacy of evacetrapib was modified by a GPS.
A previously validated GPS for coronary artery disease, composed of 6.6 million genetic variants, was calculated in each participant.1 This score was based on association statistics derived from a previously published genome-wide association study of up to 60,801 individuals with coronary artery disease and 123,504 control subjects, and optimized using a recently developed algorithm that integrates the cumulative impact of all available variants.14 The GPS for each individual was corrected for genetic background – as quantified by the first five principal component of ancestry – using a residualized linear regression.5 Patients were then classified into GPS quintiles. Conditional logistic regression was used to estimate the association of each GPS quintile with the risk of major cardiovascular events, with adjustment for age, sex and five principal components of ancestry, as performed previously.3
Among 2,984 patients, the mean age was 66 years, 687 patients (23%) were women and 1494 patients (50%) were randomized to receive evacetrapib. The GPS predicted the development of recurrent major cardiovascular events (Figure). Patients in the highest quintile of the GPS were at 60% higher risk of a major cardiovascular event than patients in the lowest quintile (adjusted odds ratio (OR) 1.60; 95% CI 1.35 – 1.89; P<0.0001). Minimal attenuation of this signal was noted after additional adjustment for cardiovascular risk factors (apolipoprotein-B levels, history of myocardial infarction, history of peripheral arterial disease, history of cerebrovascular disease, region, and smoking status), with the highest quintile associated with a 52% higher risk of cardiovascular events when compared with the lowest quintile (OR 1.52; 95% CI 1.28 – 1.80, p<0.0001). There was no evidence of efficacy of evacetrapib as compared to placebo in reduction of major cardiovascular events within the present nested case-control cohort (OR 1.04, CI 0.96, 1.15, p=0.46), with similarly null results noted within each quintile of the GPS (Figure, p-interaction = 0.66). Similarly, when the GPS was modeled as a continuous variable, no evidence of an interaction between the GPS and evacetrapib use was observed (p-interaction = 0.92).
Figure.
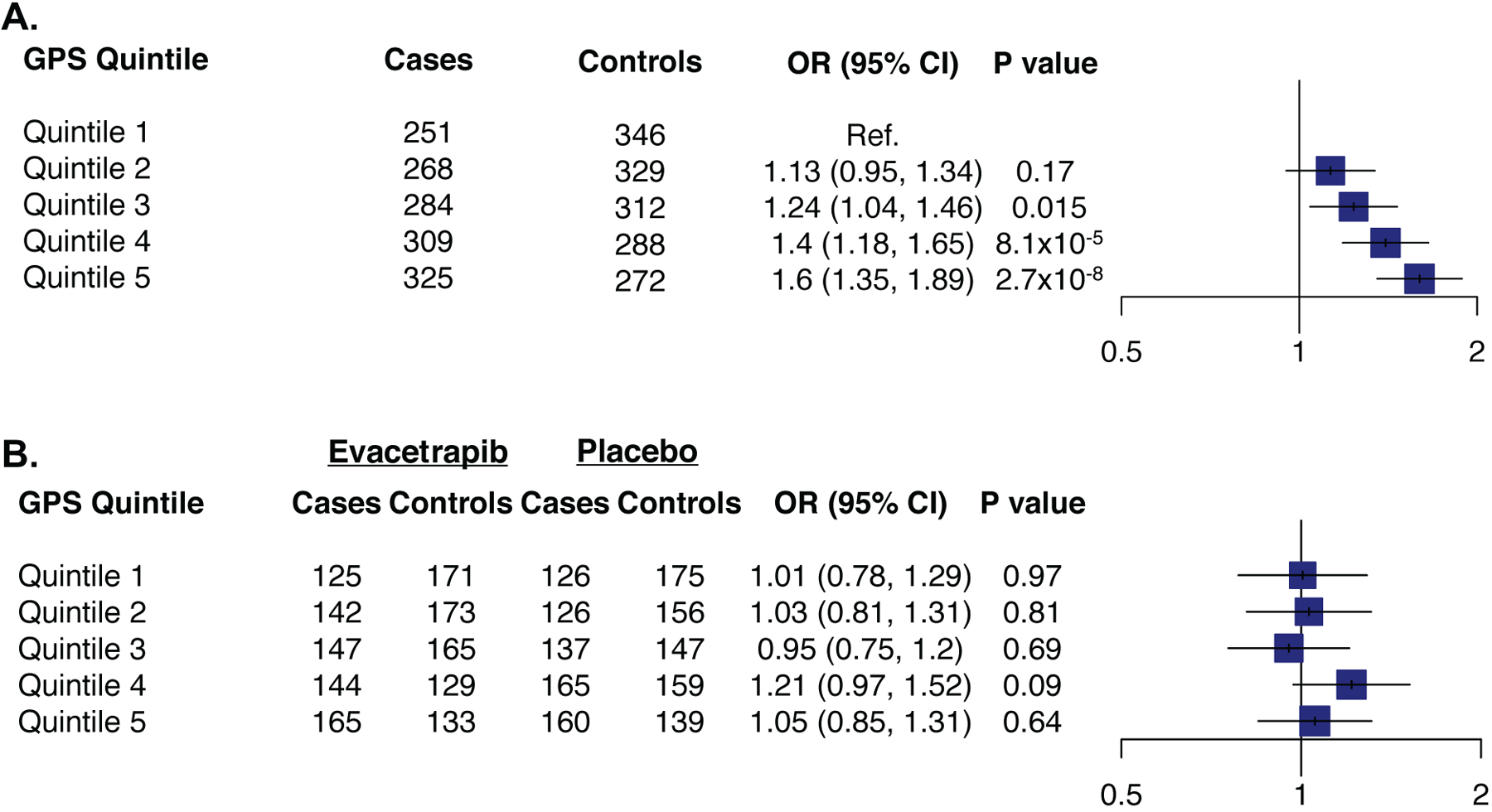
A. Association of genome-wide polygenic score (GPS) quintile with major adverse cardiovascular events in patients with high risk vascular disease. B. Association of evacetrapib use with major cardiovascular events by quintile of the genome-wide polygenic score (GPS). Estimates were derived using conditional logistic regression with adjustment for age, sex and the first five principal components of ancestry. OR, odds ratio; 95% CI, 95% confidence interval.
In this study, we demonstrate that a GPS predicts risk of major adverse cardiovascular events among patients with high-risk vascular disease. However, this GPS did not modify the effect of evacetrapib on risk of secondary cardiovascular events. Although the GPS predicted risk of major cardiovascular events within a secondary prevention context, the magnitude of the association of the GPS was reduced compared to prior reported associations of polygenic scores with initial cardiovascular events. For example, the top quintile of a GPS was associated with a 2.55-fold increased risk of incident coronary artery disease, in contrast to the 1.6-fold increased risk observed in this study.1 Whether a GPS trained specifically to predict cardiovascular risk among those with already manifest disease can further improve predictive power warrants further study.
Prior analyses have demonstrated that statins provide greater benefit among individuals at high polygenic risk of coronary artery disease than those at low polygenic risk, giving rise to the hypothesis that similar heterogeneity of effect might be observed for evacetrapib.6 However, no evidence of heterogeneity of effect of evacetrapib on cardiovascular events was observed across quintiles of the GPS. Importantly, this null result was observed despite a greater number of events in those with the highest GPS quintile – 325 in the present study versus 155 in the previous analysis of the West of Scotland Coronary Prevention Study.6 In contrast to a GPS, previous analyses have provided preliminary evidence that a common genetic variant near the ADCY9 gene may identify a subset of individuals who derive benefit from the cholesteryl ester transfer protein inhibitor, dalcetrapib.7 However, subsequent analyses of the ACCELERATE and REVEAL clinical trials using evacetrapib and anacetrapib, respectively, failed to replicate this observation.3,8 This hypothesis is being tested prospectively in the Effect of Dalcetrapib vs Placebo on CV Risk in a Genetically Defined Population With a Recent ACS (dalGene, clinicaltrials.gov ) clinical trial.
Low event rates in contemporary cardiovascular outcomes have led to important cost considerations that limit the field’s ability to test therapeutic hypotheses. This analysis suggests that widespread availability of a GPS might allow for identification and enrollment of individuals of a genetically enriched clinical trial population with a significantly higher event rate, thus allowing for decreased sample size and cost.
Supplementary Material
Acknowledgments:
We thank the patients who consented to participate in the ACCELERATE trial. Eli Lilly & Co. was the sponsor of this study. We also thank Wendra M. Foster for assisting in internal approval processes, ICD review, and coordinating with CRO for sample shipments, genotyping and secure data transfer.
Sources of Funding: This project was is supported by an institutional grant from the Broad Institute of MIT and Harvard (BroadIgnite), grant 1K08HG010155 from the National Human Genome Research Institute, a Hassenfeld Scholar Award from Massachusetts General Hospital, and a sponsored research agreement from IBM Research (to S.K. and A.V.K.)
Disclosures: CAE reports personal fees from Navitor Pharma and Novartis. Dr Lincoff reports grants from Eli Lilly during the conduct of the study; grants from Astra Zeneca, CSL, AbbVie, and Esperion outside the sumbmitted work; and personal fees from Novo Nordisk outside the submitted work. Dr Nicholls reports grants from Eli Lilly during the conduct of the study; grants from AstraZeneca, Amgen, Anthera, Eli Lilly, Novartis, Cerenis, The Medicines Company, Resverlogix, InfraReDx, Roche, Sanofi-Regeneron, and LipoScience outisde the submitted work; and personal fees from AstraZeneca, Eli Lilly, Anthera, Omthera, Merck, Takeda, Resverlogix, Sanofi-Regeneron, CSL Behring, Esperion, and Boehringer Ingelheim outside the submitted work. Dr Nissen reports grants and nonfinancial support from Eli Lilly during the conduct of the study. Drs Bhatnagar, Pillai, Riesmeyer and Ruotolo are employees of Eli Lilly. No other disclosures were reported. S.K. is an employee of Verve Therapeutics, and holds equity in Verve Therapeutics, Maze Therapeutics, Catabasis, and San Therapeutics. He is a member of the scientific advisory boards for Regeneron Genetics Center and Corvidia Therapeutics; he has served as a consultant for Acceleron, Eli Lilly, Novartis, Merck, Novo Nordisk, Novo Ventures, Ionis, Alnylam, Aegerion, Haug Partners, Noble Insights, Leerink Partners, Bayer Healthcare, Illumina, Color Genomics, MedGenome, Quest, and Medscape; he reports patents related to a method of identifying and treating a person having a predisposition to or afflicted with cardiometabolic disease (20180010185) and a genetics risk predictor (20190017119). A.V.K. has served as a consultant or received honoraria from Color Genomics, Illumina, and Navitor Pharmaceuticals, received grant support from the Novartis Institute for Biomedical Research and IBM Research, and reports a patent related to a genetic risk predictor (20190017119).
Non-standard abbreviations:
- GPS
genome-wide polygenic score
References:
- 1.Khera AV, Chaffin M, Aragam KG, Haas ME, Roselli C, Choi SH, Natarajan P, Lander ES, Lubitz SA, Ellinor PT, Kathiresan S. Genome-wide polygenic scores for common diseases identify individuals with risk equivalent to monogenic mutations. Nat Genet. 2018;50:1219–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel RS, Schmidt AF, Tragante V, McCubrey RO, Holmes MV, Howe LJ, Direk K, Åkerblom A, Leander K, Virani SS, et al. Association of Chromosome 9p21 With Subsequent Coronary Heart Disease Events. Circ Genom Precis Med. 2019;12:e002471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nissen SE, Pillai SG, Nicholls SJ, Wolski K, Riesmeyer JS, Weerakkody GJ, Foster WM, McErlean E, Li L, Bhatnagar P, et al. ADCY9 Genetic Variants and Cardiovascular Outcomes With Evacetrapib in Patients With High-Risk Vascular Disease: A Nested Case-Control Study. JAMA Cardiol. 2018;3:401–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vilhjálmsson BJ, Yang J, Finucane HK, Gusev A, Lindström S, Ripke S, Genovese G, Loh P-R, Bhatia G, Do R, et al. Modeling Linkage Disequilibrium Increases Accuracy of Polygenic Risk Scores. Am J Hum Genet. 2015;97:576–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khera AV, Chaffin M, Zekavat SM, Collins RL, Roselli C, Natarajan P, Lichtman JH, D’Onofrio G, Mattera J, Dreyer R, et al. Whole-Genome Sequencing to Characterize Monogenic and Polygenic Contributions in Patients Hospitalized With Early-Onset Myocardial Infarction. Circulation. 2019;139:1593–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Natarajan P, Young R, Stitziel NO, Padmanabhan S, Baber U, Mehran R, Sartori S, Fuster V, Reilly DF, Butterworth A, et al. Polygenic Risk Score Identifies Subgroup With Higher Burden of Atherosclerosis and Greater Relative Benefit From Statin Therapy in the Primary Prevention Setting. Circulation. 2017;135:2091–2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tardif J-C, Rhainds D, Brodeur M, Feroz Zada Y, Fouodjio R, Provost S, Boulé M, Alem S, Grégoire JC, L’Allier PL, et al. Genotype-Dependent Effects of Dalcetrapib on Cholesterol Efflux and Inflammation: Concordance With Clinical Outcomes. Circ Cardiovasc Genet. 2016;9:340–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hopewell JC, Ibrahim M, Hill M, Shaw PM, Braunwald E, Blaustein RO, Bowman L, Landray MJ, Sabatine MS, Collins R, HPS3/TIMI55 - REVEAL Collaborative Group. Impact of ADCY9 Genotype on Response to Anacetrapib. Circulation. 2019;377:1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


