Abstract
Background
Endometriosis is an invalidating gynaecological condition in women of reproductive age, and a frequent cause of infertility. Unfortunately, the condition is characterized by a long interval between onset of symptoms and diagnosis. GPs in the Netherlands are educated to provide basic gynaecological care and serve as gatekeepers for specialist medical care. Therefore, it is of great importance that they recognize signs and symptoms possibly caused by endometriosis to initiate adequate actions.
Objective
The main objective of this study was to identify barriers and facilitators to the timely diagnosis of endometriosis from the GPs’ perspective.
Methods
Semi-structured focus group discussions with GPs were organized throughout the Netherlands. The participants were encouraged to brainstorm about their perspective on daily practice regarding endometriosis and suggestions for interventions to enable early diagnosis and treatment. Analysis was based on grounded theory methodology.
Results
Forty-three GPs participated in six focus groups. Analysis of the transcripts revealed relevant determinants of practice in four main themes: professionals’ experience and competence, patient characteristics, guideline factors and professional collaboration. A lack of knowledge and awareness appeared to result in a low priority for establishing the diagnosis of endometriosis, especially in young women. Infertility, patient engagement and a recent serious case or training facilitated referral.
Conclusion
Several factors in daily primary health care contribute to the diagnostic delay in endometriosis. Future interventions to reduce this delay may be aimed at increasing awareness by means of education, incorporating the subject into national clinical guidelines and improvements in interdisciplinary collaboration.
Keywords: Delayed diagnosis, endometriosis, focus groups, general practice, qualitative research, women’s health
Key Messages.
GPs consider their experience with endometriosis limited.
There is a low sense of urgency for timely diagnosis of endometriosis.
The development of a guideline may support GP awareness and skills.
Background
Endometriosis is a common gynaecological disorder, with a reported prevalence of 2–10% in women of reproductive age (1). It is defined as the presence of ectopic endometrial-like tissue, which induces a chronic, inflammatory reaction (2). The clinical presentation is highly variable, ranging from asymptomatic to invalidating pelvic pain and infertility. Besides classic symptoms such as severe dysmenorrhoea, cyclic pelvic pain and dyspareunia, nonspecific or vague symptoms such as periodic bloating, diarrhoea or constipation, dysuria and fatigue are often presented as well (3, 4). Some women respond well to symptomatic treatment by suppression of the menstrual cycle; however, a substantial number of women require specialist consultation for diagnostics and treatment. Some patients experienced serious complaints that had not been addressed adequately for many years before eventually being diagnosed with endometriosis (5, 6). Diagnostic delay remains an issue of great concern, because it may lead to delayed treatment or suboptimal care with risk of infertility, organ damage, reduced quality of life and loss of work productivity or disability (7, 8). Previous studies have shown that the diagnostic delay in endometriosis is extensive and consists of several components related to both the patient and the doctor (6, 7, 9, 10). The GP plays a pivotal role in identifying patients at an early stage of the disease. Awareness on endometriosis as a possible underlying cause of abdominal complaints facilitates empiric treatment or early referral if needed. In the Netherlands, GP education is based on a structured schedule of theoretical teaching combined with exposure in clinical practice. GPs in training are educated on gynaecological subjects in a short theoretical module in which endometriosis is scarcely addressed. Midwives and non-medical personnel are not involved in the care of gynaecological problems.
To be able to develop targeted interventions aimed at reducing diagnostic delay, it is crucial to be aware of determinants of daily general practice, which may impede or facilitate early recognition of endometriosis. The aim of this study was to explore the barriers and facilitators influencing time to diagnosis of endometriosis from the GPs’ perspective.
Materials and methods
Focus groups with GPs were performed between January 2016 and March 2017. Participants were recruited by contacting group practices listed by the Dutch College of General Practitioners by email. Purposive sampling of group practices was performed based on geographical spread, on rural or urban area and on the employment of a GP specialized in urogynaecology. To be able to gain information from different levels of experience, we aimed to include a specialized GP in multiple focus groups and to organize one focus group exclusively with GPs in training. We continued to organize focus groups until data saturation was achieved, which was defined as no additional information was gathered during subsequent focus groups, followed by one additional focus group for confirmation of data saturation. Of the approximately 5000 GP practices in the Netherlands, 29 were invited to participate in the study, based on the earlier-mentioned criteria. Only groups of collaborating GPs were invited, and focus groups took place in their own medical office. No incentives were provided for participation. We expected that the interaction and sharing of experiences in focus groups would generate more relevant information compared to individual interviews. The semi-structured approach allowed the participants to talk freely with structured guidance from the moderator, using a topic guide (supplementary material). The topic guide was based on the literature and experience of the authors (all female), working in the fields of reproductive medicine, primary care, qualitative research, and implementation research. It was a dynamic document, on which topics were added when new items were identified during the focus groups. All focus groups were directed by one experienced moderator (W.N.) with a backup for taking notes and process monitoring (M.Z.). The moderators were not personally or professionally related to the participants. The GPs signed an informed consent form before participating. Anonymity and confidentiality were ensured
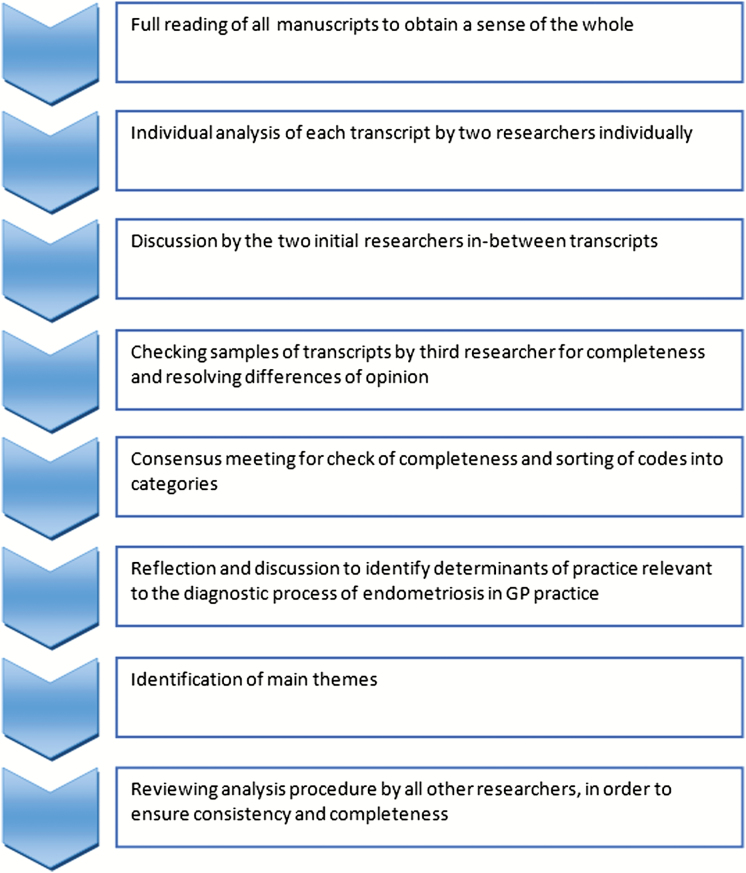
The focus groups were audio-recorded and fully transcribed. The qualitative research software package ATLAS-ti (v7.1) was used to assist in data analysis. Grounded theory methodology was applied for data analysis, which was performed in tandem with the focus groups (11, 12). A summary of the analysis process is shown in Figure 1. Study reporting was based on the COREQ criteria (13). We have provided a quantification to indicate whether the results have been obtained from few (1–3), some (4–10), many (11–21) or most (22 or more) participants.
Figure 1.
Procedure of content analysis.
Results
GPs from 29 group practices were sent an invitation letter by email. Three of these were willing to participate themselves; however, they failed to convince their associated colleagues to join and therefore rejected the invitation. One GP refused because endometriosis was covered in a local education program and 19 did not reply to the email. In total, 43 GPs participated in six focus groups in both urban and rural areas throughout the country. One focus group was held exclusively with GPs in training (n = 12), all from different practices. The other five focus groups were held with all GPs from one group practice each. Three of the participating GPs had completed an additional postgraduate training course for GPs specializing in urogynaecology; they participated in the focus group in their own practice. The duration of the focus groups was between 46 and 89 minutes. Descriptive data of participants are demonstrated in Table 1. Analysis of the focus groups generated four main themes based on the grouping of the most frequent codes and categories, with regard to barriers and facilitators to a timely delay in diagnosing endometriosis: professional experience and competence, patient characteristics, guideline factors and professional collaboration (Table 2).
Table 1.
Baseline characteristics of the GPs participating in the focus groups between January 2016 and March 2017
| FG 1 | FG 2 | FG 3 | FG 4 | FG 5 | FG 6 | |
|---|---|---|---|---|---|---|
| Number of participants | 8 | 8 | 7 | 3 | 12 | 5 |
| Gender | ||||||
| Male | 2 | 4 | 1 | 1 | 1 | 1 |
| Female | 6 | 4 | 6 | 2 | 11 | 4 |
| Specialty training in Women’s Health | 1 | 1 | 1 | 0 | 0 | 0 |
| Type of practice | ||||||
| Urban | 0 | 8 | 1 | 3 | 1 | 3 |
| Rural | 8 | 0 | 6 | 0 | 0 | 1 |
| Mixed/variable | 0 | 0 | 0 | 0 | 11 | 1 |
| Years in profession | ||||||
| GP in training | 1 | 0 | 0 | 0 | 11 | 2 |
| < 5 years | 1 | 1 | 3 | 1 | 0 | 1 |
| 5–20 years | 4 | 5 | 3 | 1 | 0 | 1 |
| > 20 years | 2 | 2 | 1 | 1 | 1# | 1 |
| Full-time equivalent* | ||||||
| Fulltime | 0 | 0 | 0 | 0 | 3 | |
| Part-time | 8 | 8 | 7 | 3 | 2 |
*GPs in training excluded.
#Participating mentor of GPs in training.
Table 2.
Barriers and facilitators in the diagnostic process of endometriosis according to the GPs participating in the focus groups between January 2016 and March 2017
| Professional experience and competence | Patient characteristics | Guideline factors | Collaboration |
|---|---|---|---|
| Barriers | |||
| Low sense of urgency for timely diagnosis | Not returning to the GP when initiated treatment fails | Lack of GP guideline | Lack of understanding gynaecologists’ diagnostic/treatment options |
| Limited experience with endometriosis | Young women less likely considered for pathologic condition | Low frequency of reporting on endometriosis in correspondence letters | |
| Limited knowledge and skills related to endometriosis | Lack of knowledge in other medical specialists | ||
| Insufficient training and literature | |||
| Facilitators | |||
| Reluctance for referral because lack of gain perceived | Faster referral in case of infertility | Reporting of endometriosis as incidental finding may increase awareness | |
| Recent case or training enhances awareness | Patient engagement promotes referral | ||
| Non-Western European background more easily referred |
Professional experience and competence
Many participants reported limitations in knowledge about endometriosis. They realized that their training in endometriosis is limited, both in clinical traineeships and educational programs. A few GPs stated they do not know where to find easily accessible literature. Almost all GPs were unaware of the prevalence rate of endometriosis and considered it a rare condition.
“Well, you have to think of it in the first place. You have to know the condition before it even occurs to you. And if you don’t think of it, you will not find the information you need.” [FG2, GP1, male]
When GPs are consulted by women with dysmenorrhoea or other complaints related to the menstrual cycle, they find it difficult to differentiate between physiological discomfort and pathological conditions like endometriosis. Moreover, consultations for abdominal complaints pose the difficulty of a wide differential diagnosis, which is mostly pointed to defecation and dietary patterns instead of a possible concurrence of complaints with the menstrual cycle.
“When I got the invitation [for the interview] I thought I hardly ever see endometriosis. But it’s like when you buy a new car; all of a sudden you see a lot of them… Last week I got the results of a woman who had a laparoscopy because of endometriosis. A young adult who suffered from severe abdominal pain for many years. I thought she had a problem with her intestines, referred her to the gastroenterologist…”[FG4, GP2, female]
The quality of the history taking may define the nature and extent of the physical examination. This can lead to omitting a gynaecological examination if symptoms are not addressed correctly. A prior serious case in their practice or recent training appeared to facilitate awareness of endometriosis. Although some of the respondents were familiar with typical signs of endometriosis in basic gynaecological examinations, like the characteristic blue nodules in the posterior fornix, most GPs stated they consider their own knowledge and skills insufficient for diagnosing endometriosis.
“If you are more aware of the condition you can ask more detailed questions, and then you can have a suspicion.”[FG2, GP1, male]
Even when the GPs consider endometriosis, referral for further diagnostics is not always beneficial in their opinion. The GPs felt that definite diagnosis may induce a burden of disease or “stigma” to some women. Especially for young or adolescent women, for whom the GPs considered a gynaecological examination too invasive given the low probability of a pathological condition in their opinion, the willingness to refer to a gynaecologist was low.
“Moderator: For example a young girl, 16 years old, who comes to your office with complaints about her menstruation, would you tell her, you consider endometriosis when you prescribe her the pill? GP3: I wouldn’t even think of it. GP2: No, me neither. I would think it just bothers her more than others. Or she just wants the pill, that’s fine. GP3: Or PMS. Just try taking the pill. I would never say to anyone ‘well you might have endometriosis, try this’. GP2: No way.”[FG4, GP2, female and GP3, male]
Many of the participating GPs routinely prescribed the contraceptive pill in a cyclic manner instead of continuously. They were not aware of the possibility of organ damage like infertility or chronic pain syndromes resulting from late diagnosis and treatment, nor the advice to fully suppress menstruation by hormonal therapy in case of endometriosis.
“GP1: But if you think of it and you start the pill you aren’t doing anything wrong. GP8: Well they will have menstruations even on the pill, but would it be better to take it continuously rather than the usual way? I actually don’t know about that. Should you advise women with endometriosis to take the pill continuously? GP3: I don’t know for sure...”[FG1, GP1, male; GP3, female, postgraduate training; GP8, male]
Patient characteristics
It appeared that several patient characteristics influenced clinical strategies. GPs were more reluctant in referring patients with dysmenorrhoea as compared to patients with infertility. The GPs were more willing to refer to a gynaecologist if family planning came up during the consultation. The suggestion that timely diagnosis and treatment of endometriosis may prevent future infertility increased their sense of urgency. One GP suggested that a note with considerations about possible endometriosis in the patient’s file may be helpful as a reminder if the woman presents some years later with persisting complaints or desire for pregnancy.
Women who frequently visit the GP’s office with a wide spectrum of complaints and who perceive a high burden of those complaints were more often considered as somatizing and less frequently referred.
The GPs were more willing to refer women who are assertive during the consultation as compared to more passive women. They were more likely to consider endometriosis in women who brought information they found on the internet to the consultation. GPs considered additional diagnostic testing or referral if their own treatment strategy was not successful. However, they noticed that many women do not return to their office when symptoms persist, which makes it more difficult to identify those with treatment failure.
“There was this lady who had a wide range of complaints, very diffuse. And to be honest, she came up with the diagnosis [endometriosis] herself. Actually, I didn’t much agree with her. But then the gynaecologist did a laparoscopy and it appeared to be endometriosis after all.”[FG2, GP2, male]
A few GPs stated that women with a different ethnic background were more likely to get a fast referral, because of communication difficulties, different presentation of pain and the assumption that these women more frequently expect or demand a referral.
“Well I think I refer migrants easily, because I find the conversation more difficult. Communication about pain, how to handle it or how to address it. I somatise more easily, faster referral. They always present their symptoms more dramatically as well, and maybe they value diagnostic tests more than others.” [FG4, GP3, male]
Guideline factors
The lack of a national guideline for GPs concerning endometriosis or abdominal pain was mentioned in five of six focus groups. The participants suggested a clinical guideline, written in their own language and developed by and for both GPs and gynaecologists. This joint guideline should ideally provide the GPs with a summary of the most recent relevant literature as well as clear instructions about which therapy they can start themselves, when referral is advised and which actions may be undertaken by the gynaecologists.
“GP1: One thing I do miss is the fact that none of our GP guidelines mention endometriosis. GP2: While apparently it has a high prevalence... GP1: Exactly.” [FG3, GP1, female and GP2, female]
“Maybe a joint guideline would help. So you will have something to pull up when you think of it. It would provide you with considerations and advice regarding diagnostics and treatment.” [FG3, GP6, male]
Collaboration
The GPs unanimously preferred more collaboration with gynaecologists about indications and instructions for empirical or first-line treatment and timing of referral. In all six focus groups, the GPs stated that they were reluctant in referring patients for further diagnostic testing on endometriosis. They questioned the added value of establishing a definite diagnosis and fear the inappropriate use of invasive techniques since the treatment regimens appeared the same to them whether the diagnosis was confirmed or not. The participants suggested that improvements in the quality of correspondence after a woman is referred may increase awareness of endometriosis and motivation for early referral. They stated that reporting on considerations about endometriosis by the gynaecologists may help in a better understanding and motivates them to consider endometriosis more easily in future consultations. Besides this, they advised gynaecologists and other medical specialists to report on endometriosis as an incidental finding or secondary diagnosis, for instance when spots are visualized at laparoscopy for another indication or when diagnosed in the workup of infertility.
“I think it would help if we got a lot of correspondence letters from the fertility specialists in which endometriosis is mentioned as a secondary diagnosis. That would keep us alert about the condition.”[FG2, GP6, female]
The GPs experienced that other medical specialists like urologists, surgeons or gastroenterologists also have a lack of knowledge about endometriosis. They suggested improving knowledge in these specialists, as well as collaboration between gynaecologists and other medical specialists.
Discussion
This study has yielded rich information about barriers and facilitators in general practice regarding the diagnostic process of endometriosis.
The most important finding is the fact that symptoms that may be characteristic for endometriosis are not easily recognized. Moreover, GPs appear to have a low sense of urgency about confirming the diagnosis of endometriosis even if they consider it as a possible explanation for these symptoms. The GPs are rather reluctant in referring women to a gynaecologist for further diagnostics on endometriosis, especially if these women are of young age. These barriers to a timely referral and diagnosis possibly result from limitations in knowledge and awareness amongst GPs. Facilitating factors are infertility as reason for the consultation, patient engagement, and a recent serious case or training. The GPs stated that improvement in collaboration with gynaecologists is necessary. For example; in developing a joint national clinical guideline, improvement in correspondence letters and additional training for GPs. This may enhance awareness on endometriosis, including understanding of the importance of adequate treatment and when referral for advanced diagnostic testing or specialist treatment is required.
The importance of findings derived from qualitative research has been increasingly appreciated (11, 14). However, careful consideration on study methodology is of great importance to secure study validity (13, 15, 16). To extract all relevant information in an objective manner, we conducted a data-based analysis style by two independent researchers, and all steps of data analysis were discussed with several members of the research team. The variety of the research team is one of the strengths of this study. Moreover, we selected participants with different levels of experience to obtain a complete set of barriers and facilitators. The setting of focus groups with all colleagues from a group practice reduced the likelihood of including only participants with a special interest in the matter and therefore underreporting of barriers in daily practice. Although less than 0.5% of GPs in the Netherlands completed a specialty training in women’s health, we intended to include group practices with a contracted specialized GP to make sure different levels of experience and exposure were represented in the study population.
Some limitations of this study should be discussed. Selection bias may have occurred because of the sampling procedure. However, the involvement of all GPs from the participating group practices, the geographical spread and the variety in level of experience increases the generalizability of our findings. Nevertheless, countries with a different health care setting may bring about other barriers and facilitators to a timely diagnosis of endometriosis. Furthermore, the determinants identified in this study may not be comprehensive, and future research activities directed at the diagnostic process can complement our findings.
To date, studies reflecting the GPs’ perspective on endometriosis care are scarce. There are some retrospective studies about the diagnostic process in general practice based on primary care records reporting similar findings with regard to the role of the GP in the diagnostic delay of endometriosis. One study extracted information from primary care records in the UK demonstrating that repeated consultations and negative diagnostic tests contributed to a median delay of 9.0 years between first consultation and diagnosis (17). Another British study identified a predictive value of linking features of consecutive consultations over time to a subsequent diagnosis of endometriosis (18). This finding may help in the development of diagnostic support systems in general practice. Prevalence rates concerning endometriosis differ according to the type of study population, with higher estimated prevalence rates seen in clinical studies as compared to community-based or database estimates (1, 3, 18-21). Although population-based studies may appear to reflect the actual prevalence rate in general practice, they are likely to be hampered by incomplete coding in medical records or databases and missed diagnosis in symptomatic women. It is important for GPs to be aware of the possibility of an underlying condition like endometriosis in consultations concerning abdominal pain, dysmenorrhoea or other symptoms related to the menstrual cycle, preventing unnecessary medicalization at the same time. A clinical guideline, covering first-line diagnostic and treatment strategies for women with abdominal or menstrual symptoms, including indications for referral may be useful in daily practice.
Conclusion
The quality of the diagnostic process of endometriosis in GPs is hampered by a limitation in knowledge and awareness, the lack of appropriate guidelines and insufficient collaboration between GPs and gynaecologists. These factors contribute to an extensive diagnostic delay. The present study was designed to explore determinants of practice regarding the diagnostic process of endometriosis in GPs in the Netherlands using a qualitative approach. Our principal aim was to identify possible barriers and facilitators rather than quantifying their relative importance. We recommend future research directed at prioritizing the individual barriers and facilitators, to be able to develop a multifaceted intervention strategy aimed at reducing diagnostic delay in endometriosis.
Acknowledgements
We thank the GPs who participated in the focus groups and Brigette Johnston for reviewing the grammar of the manuscript.
Declaration
Funding: none.
Ethical approval: The study protocol did not require full institutional review board approval (Reference number 2016-2629).
Conflict of interest: None.
References
- 1. Eskenazi B, Warner ML. Epidemiology of endometriosis. Obstet Gynecol Clin North Am 1997; 24: 235–58. [DOI] [PubMed] [Google Scholar]
- 2. Kennedy S, Bergqvist A, Chapron C et al. ; ESHRE Special Interest Group for Endometriosis and Endometrium Guideline Development Group ESHRE guideline for the diagnosis and treatment of endometriosis. Hum Reprod 2005; 20: 2698–704. [DOI] [PubMed] [Google Scholar]
- 3. Bellelis P, Dias JA Jr., Podgaec S, Gonzales M, Baracat EC, Abrao MS. Epidemiological and clinical aspects of pelvic endometriosis-a case series. Rev Assoc Med Bras (1992). 2010;56(4):467–71. [DOI] [PubMed] [Google Scholar]
- 4. Davis GD, Thillet E, Lindemann J. Clinical characteristics of adolescent endometriosis. J Adolesc Health 1993; 14: 362–8. [DOI] [PubMed] [Google Scholar]
- 5. Denny E, Mann CH. Endometriosis and the primary care consultation. Eur J Obstet Gynecol Reprod Biol 2008; 139: 111–5. [DOI] [PubMed] [Google Scholar]
- 6. Ballard K, Lowton K, Wright J. What’s the delay? A qualitative study of women’s experiences of reaching a diagnosis of endometriosis. Fertil Steril 2006; 86: 1296–301. [DOI] [PubMed] [Google Scholar]
- 7. Nnoaham KE, Hummelshoj L, Webster P et al. ; World Endometriosis Research Foundation Global Study of Women’s Health consortium Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril 2011; 96: 366–73.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. De Graaff AA, D’Hooghe TM, Dunselman GA, Dirksen CD, Hummelshoj L, Simoens S; WERF EndoCost Consortium The significant effect of endometriosis on physical, mental and social wellbeing: results from an international cross-sectional survey. Hum Reprod 2013; 28: 2677–85. [DOI] [PubMed] [Google Scholar]
- 9. Hudelist G, Fritzer N, Thomas A et al. . Diagnostic delay for endometriosis in Austria and Germany: causes and possible consequences. Hum Reprod 2012; 27: 3412–6. [DOI] [PubMed] [Google Scholar]
- 10. Staal AH, van der Zanden M, Nap AW. Diagnostic delay of endometriosis in the Netherlands. Gynecol Obstet Invest 2016; 81: 321–4. [DOI] [PubMed] [Google Scholar]
- 11. Glaser BG, Strauss AL.. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine Publishing Company, 1967. [Google Scholar]
- 12. Strauss A, Corbin J. Grounded theory methodology: an overview. In: Denzin NK, Lincoln YS, (eds). Handbook of Qualitative Research. Thousand Oaks, CA: SAGE Publications, 1994, pp. 273–85. [Google Scholar]
- 13. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19: 349–57. [DOI] [PubMed] [Google Scholar]
- 14. Malterud K. The art and science of clinical knowledge: evidence beyond measures and numbers. Lancet 2001; 358: 397–400. [DOI] [PubMed] [Google Scholar]
- 15. Malterud K. Qualitative research: standards, challenges, and guidelines. Lancet 2001; 358: 483–8. [DOI] [PubMed] [Google Scholar]
- 16. Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ (Clinical research ed). 2000; 320(7226): 50–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pugsley Z, Ballard K. Management of endometriosis in general practice: the pathway to diagnosis. Br J Gen Pract. 2007; 57(539): 470–6. [PMC free article] [PubMed] [Google Scholar]
- 18. Burton C, Iversen L, Bhattacharya S, Ayansina D, Saraswat L, Sleeman D. Pointers to earlier diagnosis of endometriosis: a nested case-control study using primary care electronic health records. Br J Gen Pract 2017; 67: e816–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Eisenberg VH, Weil C, Chodick G, Shalev V. Epidemiology of endometriosis: a large population-based database study from a healthcare provider with 2 million members. BJOG 2018; 125: 55–62. [DOI] [PubMed] [Google Scholar]
- 20. Husby GK, Haugen RS, Moen MH. Diagnostic delay in women with pain and endometriosis. Acta Obstet Gynecol Scand 2003; 82: 649–53. [DOI] [PubMed] [Google Scholar]
- 21. Meuleman C, Vandenabeele B, Fieuws S, Spiessens C, Timmerman D, D’Hooghe T. High prevalence of endometriosis in infertile women with normal ovulation and normospermic partners. Fertil Steril 2009; 92: 68–74. [DOI] [PubMed] [Google Scholar]