Abstract
Background
The aim of this study was to compare the results of the standard once-weekly Ponseti casting technique to an accelerated twice-weekly regimen in our population cohort.
Methods
A prospective randomized controlled study was conducted with a total of 100 consecutive patients (158 feet) being enrolled for the study. Fifty patients were randomized to each group and followed up for at least one year.
Results
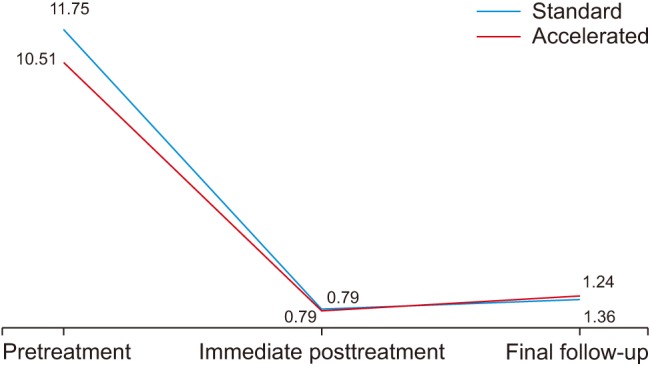
Initial mean Pirani score was 4.67 ± 0.73 in the standard group and 4.35 ± 0.76 in the accelerated group, and the score decreased to 0.34 ± 0.38 and 0.35 ± 0.31, respectively. Initial mean Dimeglio score was 11.75 ± 2.75 in the standard group and 10.51 ± 2.57 in the accelerated group, and the score decreased to 0.79 ± 0.77 and 0.79 ± 0.71, respectively, immediately after casting. The average number of casts required to correct all the deformities was 6.3 ± 1.2 in the standard group and 6.1 ± 1.4 in the accelerated group (p = 0.45). Average time spent in cast was 58.2 ± 8.3 days in the standard group and 39.5 ± 5.2 days in the accelerated group (p < 0.001). Percutaneous Achilles tendon tenotomy was done in 86.42% in the standard group and in 84.41% in the accelerated group (p = 0.72). Final results were assessed by using a modified functional rating scoring system: 55.55% clubfeet had excellent results and 44.45% had good results in the standard group, whereas 66.23% clubfeet had excellent results and 33.77% had good results in the accelerated group. None amongst the two groups had fair or poor results.
Conclusions
These results suggest that the accelerated Ponseti technique significantly reduces the correction time without affecting the final results and that it is as safe and effective as the traditional Ponseti technique.
Keywords: Foot deformities, Clubfoot, Plaster casts, Ponseti
Congenital clubfoot, or congenital talipes equinovarus (CTEV), is one of the most common congenital deformities.1) It most likely represents congenital dysplasia of all musculoskeletal tissues (musculotendinous, ligamentous, osteoarticular, and neurovascular structures) distal to the knee. This conclusion is based on multiple investigators' observations of a myriad of different abnormal anatomic findings and on the functional outcome of patients who were believed to have received optimal non-operative or operative treatment but nevertheless subsequently always had some degree of impairment.2) Congenital clubfoot is a complex three-dimensional deformity consisting of four components: cavus, adductus, varus, and equinus.
The incidence of congenital clubfoot is approximately 1.2 per 1,000 live births.3) If a clubfoot is allowed to remain deformed, many other late adaptive changes occur in the bones. These changes depend on the severity of soft-tissue contractures and the effects of walking. In untreated adults, some joints may spontaneously fuse or degenerative changes secondary to the contractures may develop.
On the basis of a proper understanding of the pathoanatomy from stillborn fetuses with clubfeet and of functional anatomy from radiography of normal feet and of clubfeet, Ignacio Ponseti developed and refined a uniform treatment for clubfeet in the late 1940s.4) Although Ponseti's clubfoot treatment has been around for many years, it is only in the recent past that his method has been given due consideration with a review of the long-term results of patients treated by him.5) The standard regimen of the Ponseti casting technique involves weekly change of cast after an initial period of manipulation. However, more recently, this arbitrary interval between two consecutive casts has been called into question. Studies have shown that the accelerated Ponseti protocol has as similar safety and efficacy as the standard protocol. In the accelerated Ponseti technique, casting is done after five days, twice weekly or thrice weekly.6)
An earlier study by Elgohary and Abulsaad7) showed that the accelerated Ponseti technique significantly reduces the correction time without affecting the final results while being as safe and effective as the traditional Ponseti, but they had excluded patients with a pretreatment Pirani score of less than 4. A decrease in the overall duration of treatment could offer multiple potential benefits leading to better compliance. The aim of our study was to compare the results of the standard Ponseti regimen to those of the accelerated Ponseti regimen in our population cohort.
METHODS
This study is a prospective, single-blind, randomized controlled study conducted in our hospital between May 2015 and December 2016. A minimum 1-year follow-up was completed by December 2017. After obtaining permission from the college ethical committee, we enrolled a total of 100 patients for the study and followed up for a minimum of 1 year. Written informed consent was obtained from the parents or guardians of the children. Randomization was done at the patient level with both feet being treated by using the same method in bilateral cases and an opaque sealed envelope method was used. Exclusion criteria were as follows: age more than 6 months, neurogenic or syndromic CTEV, and previously operated or relapsed CTEV.
All patients were treated in our clubfoot clinic and a detailed history was sought from attendants, with particular reference to the age, sex, exposure of the mother to radiation or drugs during pregnancy, type of delivery, place of delivery, birth order, birth asphyxia, family history, other deformities or diseases, and any previous intervention. Initial Pirani8) and Dimeglio9) scoring was done. Radiographs of the foot were taken (anteroposterior view and lateral view in stress dorsiflexion) to calculate the talocalcaneal angle, talus-first metatarsal angle, and tibiocalcaneal angle.10)
Steps were the same in both the standard and accelerated Ponseti techniques11,12,13) except for the duration of cast immobilization. The cast was changed twice weekly in the accelerated group and once weekly in the standard group. The two phases in the management were as follows: (1) treatment phase: consisted of weekly gentle manipulation and casting in the standard group and twice weekly in the accelerated group. Manipulation was done for 1 minute in each group. (2) Maintenance phase: consisted of bracing with a foot abduction orthosis after removal of the final cast.
All the deformities of clubfoot were corrected simultaneously except the equinus deformity, which was corrected in the final cast. The final cast was applied for three weeks with the foot in more than 15° of dorsiflexion and 70° of abduction, if tendoachilles tenotomy had been performed, or for 2 weeks otherwise. The radiographs of the foot were taken to calculate talocalcaneal angle, talus-first metatarsal angle, and tibiocalcaneal angle after the final cast was removed.
The foot abduction brace was used thereafter for 23 hours a day for 3 months and then during night time and nap time. The first follow-up was at 1 week to check for compliance of bracing, then monthly till 3 months and then every 3 months till final assessment at 1 year. At the end of 12-month follow-up, the Pirani and Dimeglio scores were checked along with the modified functional rating system (FRS) score (Table 1).14,15) Results were labeled as excellent, good, fair, and poor on the basis of the modified FRS score.
Table 1. Modified Functional Rating System Score to Evaluate Functional Outcomes (Maximum Score = 100).
| Variable | Score |
|---|---|
| Ankle dorsiflexion | |
| Above neutral | 20 |
| To neutral (+ 5°) | 10 |
| Less than neutral | 0 |
| Subtalar motion | |
| > 15℃ | 10 |
| < 15° | 5 |
| 0°–5° | 0 |
| Heel position with maximal passive ankle dorsiflexion | |
| 0° Varus or valgus | 15 |
| 0°–5° Varus | 10 |
| Varus 6°–10° | 5 |
| Varus > 10° | 0 |
| Forefoot appearance | |
| > 5° Abduction | 15 |
| Neutral | 10 |
| > 5° Adduction | 0 |
| Medial crease | |
| Absent | 10 |
| Present | 0 |
| Cavus | |
| < 5 mm | 10 |
| > 5 mm | 0 |
| Radiological measurement | |
| Talocalcaneal index | |
| > 40° | 10 |
| < 40° | 0 |
| Talar-first metatarsal angle | |
| < 10° | 10 |
| > 10° | 0 |
Statistical Methods
Data analysis was performed by using IBM SPSS ver. 25.0 (IBM Corp., Armonk, NY, USA). Metric data are described as mean and median; nonmetric or categorical data are described as frequency and frequency percentage. Intergroup comparison of metric variables was done by the Student t-test and that of nonmetric variables was done by chi-square test. Furthermore, the intragroup variance was measured by paired t-test and repeated measures analysis of variance was done by F-test. All the inferences were drawn at 0.05 level of significance.
RESULTS
A total of 100 patients were included in the study (158 feet). Of those, 58 patients had bilateral involvement, 23 had right-side involvement and 19 had left-side involvement. In the standard group, 31 (62%) had bilateral involvement, nine (18%) had right-side involvement, and 10 (20%) had left-side involvement; in the accelerated group, 27 (54%) had bilateral involvement, 14 (28%) had right-side involvement, and nine (18%) had left-side involvement. The mean age in the standard group was 29.2 days (range, 2 to 165 days) and that in the accelerated group was 18.2 days (range, 1 to 175 days). Most of our patients were male: 36 in the standard group and 34 in the accelerated group. Family history of CTEV was present in 9% of total cases.
The average pretreatment, immediate posttreatment, and final follow-up Pirani and Dimeglio scores are given in Figs. 1 and 2. There was no statistically significant difference in the number of casts needed for full correction between the standard group (6.3 ± 1.2) and the accelerated group (6.1 ± 1.4; p = 0.45). The average duration of casting needed for correction was 58.2 ± 8.3 days (range, 42 to 77 days) in the standard group and 39.5 ± 5.2 days (range, 32 to 56 days) in the accelerated group (p < 0.001). In the standard group, 70 of 81 clubfeet (86.42%) needed a percutaneous tendoachilles tenotomy while in the accelerated group, 65 of 77 clubfeet (84.41%) needed one. The mean age at tenotomy was 41.02 days in the standard group and 18.18 days in the accelerated group.
Fig. 1. The mean Pirani score at the pretreatment, immediate posttreatment, and final follow-up.
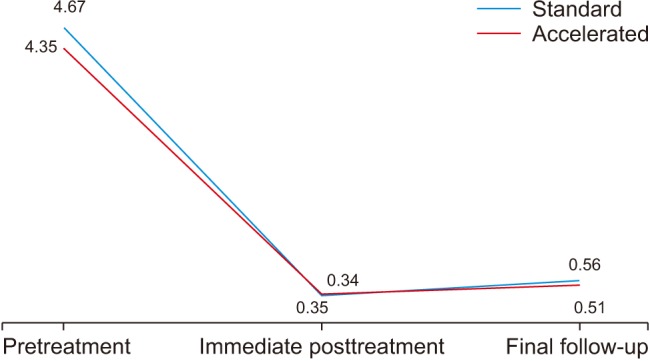
Fig. 2. The mean Dimeglio score at the pretreatment, immediate posttreatment, and final follow-up.
The anteroposterior talocalcaneal angle increased from 17.22° ± 6.3° pretreatment to 33.93° ± 8.9° immediate posttreatment (p < 0.05) in the standard group and from 17.4° ± 6.5° to 36.54° ± 8.6° (p < 0.05) in the accelerated group. The mean lateral talocalcaneal angle increased from 18.18° ± 5.7° to 31.01° ± 8.7° (p < 0.05) in the standard group and from 18.66° ±6.8° to 34.35° ± 9.8° (p < 0.05) in the accelerated group. The mean talus-first metatarsal angle changed from 60.33° ± 20.5° to −23.37° ± 9.2° (p < 0.05) in the standard group and from 56.79 ± 19.10 to −23.97 ± 10.90 (p < 0.05) in the accelerated group. The mean tibiocalcaneal angle decreased from 108.95 ± 20.30 to 79.74 ± 10.20 (p < 0.05) in the standard group and from 102 ± 15.50 to 80.4 ± 12.60 (p < 0.05) in the accelerated group. There was no statistically significant difference between the two groups in immediate posttreatment anteroposterior talocalcaneal angle (p = 0.07), lateral talocalcaneal angle (p = 0.06), talus-first metatarsal angle (p = 0.97), and tibiocalcaneal angle (p = 0.95).
Final outcome was assessed by using the modified FRS and categorized into excellent, good, fair, and poor. The mean FRS was 83.81 ± 6.8 in the standard group and 85 ± 6.3 in the accelerated group (p = 0.24). In the standard group, excellent and good results were obtained in 55.55% and 44.45% (45 and 36 out of 71) feet, respectively; and in the accelerated group in 66.23% and 33.77% (51 and 26 out of 77) feet, respectively. There were no patients with fair or poor results (Fig. 3).
Fig. 3. Final results as per the modified functional system.
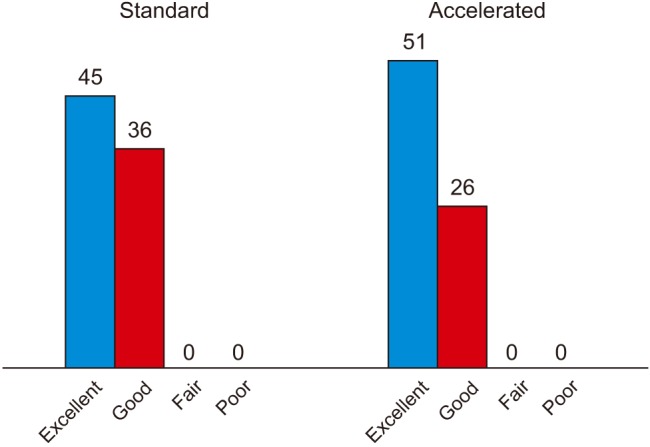
Table 2 lists the complications that we encountered during the treatment of clubfeet and the management of these complications. Only equinus deformity recurred among our patients. In the standard group, it recurred in two patients (three feet); in the accelerated group, in one patient (two feet). All of these patients were managed by percutaneous heel cord tenotomy and casting. All of these patients had not had an initial tendoachilles tenotomy done. We also did an intragroup comparison (post-hoc analysis) of treatment scores over the study period in each group, the results of which are presented in Tables 3 and 4: there were statistically significant differences in Pirani and Dimeglio scores between pretreatment, immediate posttreatment, and final follow-up. Table 5 summarizes the results of this study.
Table 2. Complications during Treatment and Their Management.
| Complication | No. of patients | Management of complication | |
|---|---|---|---|
| Standard group | Accelerated group | ||
| Rash around groin and thigh | 5 | 7 | Not applicable |
| Tight cast with swelling of feet | 2 | 3 | Removal of cast followed by reapplication after swelling subsided |
| Cast slippage | 3 | 2 | Reapplication of cast |
| Excessive irritability in brace | 5 | 4 | Reassurance to parents |
| Both-bone leg fracture | 0 | 1 | Cast continued for 2 more weeks |
| Sore due to brace | 2 | 1 | Change of brace |
| Minor saw injury | 2 | 2 | Wound dressing and cast continuation |
Table 3. Intra Group Comparison (Post-Hoc Analysis) of Treatment Scores (Mean ± SD) over the Study Period in the Accelerated Group.
| Variable | N | Mauchly's W | Pretreatment (a) | Immediate posttreatment (b) | Final follow-up (c) | p-value | |||
|---|---|---|---|---|---|---|---|---|---|
| ab | ac | bc | abc | ||||||
| Pirani | |||||||||
| Right | 41 | 0.452 | 4.4 ± 0.8 | 0.4 ± 0.3 | 0.5 ± 0.3 | < 0.001 | < 0.001 | 0.006 | < 0.001 |
| Left | 36 | 0.401 | 4.3 ± 0.7 | 0.3 ± 0.3 | 0.5 ± 0.3 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Dimeglio | |||||||||
| Right | 41 | 0.192 | 10.6 ± 2.7 | 0.9 ± 0.8 | 1.4 ± 0.7 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Left | 36 | 0.229 | 10.4 ± 2.4 | 0.7 ± 0.7 | 1.3 ± 0.5 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Modified FRS | |||||||||
| Right | 85.5 ± 6.7 | ||||||||
| Left | 85 ± 6.0 | ||||||||
Values are presented as mean ± standard deviation.
SD: standard deviation, FRS: functional rating system.
Table 4. Intra Group Comparison (Post-Hoc Analysis) of Treatment Scores (Mean ± SD) over the Study Period in the Standard Group.
| Variable | N | Mauchly's W | Pretreatment (a) | Immediate posttreatment (b) | Final follow-up (c) | p-value | |||
|---|---|---|---|---|---|---|---|---|---|
| ab | ac | bc | abc | ||||||
| Pirani | |||||||||
| Right | 40 | 0.549 | 4.5 ± 0.8 | 0.3 ± 0.4 | 0.6 ± 0.3 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Left | 41 | 0.761 | 4.8 ± 0.7 | 0.4 ± 0.4 | 0.6 ± 0.3 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Dimeglio | |||||||||
| Right | 40 | 0.125 | 11.4 ± 2.9 | 0.8 ± 0.8 | 1.4 ± 0.9 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Left | 41 | 0.161 | 12.1 ± 2.6 | 0.8 ± 0.8 | 1.1 ± 1.0 | < 0.001 | < 0.001 | 0.007 | < 0.001 |
| Modified FRS | |||||||||
| Right | 83.8 ± 6.8 | ||||||||
| Left | 83.4 ± 6.7 | ||||||||
Values are presented as mean ± standard deviation.
SD: standard deviation, FRS: functional rating system.
Table 5. Summary of Results.
| Variable | Accelerated (n = 50) | Standard (n = 50) | p-value |
|---|---|---|---|
| Initial tenotomy done: right | 0.925 | ||
| No | 6 (14.6) | 6 (15.4) | |
| Yes | 35 (85.4) | 33 (84.6) | |
| Initial tenotomy done: left | 0.547 | ||
| No | 6 (16.7) | 5 (11.9) | |
| Yes | 30 (83.3) | 37 (88.1) | |
| Final result: right | 0.529 | ||
| Excellent | 27 (64.3) | 23 (57.5) | |
| Good | 15 (35.7) | 17 (42.5) | |
| Final result: left | 0.185 | ||
| Excellent | 24 (68.6) | 22 (53.7) | |
| Good | 11 (31.4) | 19 (46.3) | |
| No. of casts required | 6.1 ± 1.4 | 6.3 ± 1.2 | 0.481 |
| Time spent in cast till last cast (day) | 18.2 ± 4.7 | 41 ± 8.1 | < 0.001 |
| Time spent in cast (day) | 39.5 ± 5.2 | 58.2 ± 8.3 | < 0.001 |
Values are presented as number (%) or mean ± standard deviation.
DISCUSSION
At present, the Ponseti method is the most commonly used modality for management of CTEV.16) The traditional Ponseti technique of weekly manipulation and casting is inexpensive, has a relatively short learning curve, and has yielded excellent results in both in short- and long-term studies.17) Although Giesberts et al.18) have published a review article showing that accelerated protocols have a similar efficacy and safety profile as the traditional protocols, no ideal casting interval has been suggested. Our aim was to establish the effectiveness of a twice-weekly accelerated protocol vis-à-vis the standard protocol in our population cohort.
The overall male to female ratio in our study was 2.3 (2.57 in the standard group and 2.12 in the accelerated group). Although many studies have demonstrated this sexual dimorphism, the exact cause is still not known. A polygenic threshold model with Carter effect has been proposed as the likely mechanism.15) While in our study 9% of the patients had a positive family history, this is much less than 22% and 25% reported by Terrazas-Lafargue and Morcuende19) and Dobbs and Gurnett,20) respectively. Bilateral involvement (58%) was more common in our study than that in the study by Elshenawy et al.21) The initial Pirani score was 4.67 in the standard group and 4.35 in the accelerated group, lower than that in studies by Elgohary and Abulsaad7) and Harnett et al,22) reflecting a less severe initial deformity. The immediate posttreatment score was 0.34 in the standard group and 0.35 in the accelerated group; Elgohary and Abulsaad7) reported immediate posttreatment scores of 0.49 and 0.52. The average decrease in the Pirani score in our study was 4.32 in the standard group and 4 in the accelerated group, whereas it was 4 and 4.5, respectively, in the study by Harnett et al.22) The Pirani score at final follow-up was 0.56 in the standard group and 0.50 in the accelerated group, whereas Elgohary and Abulsaad7) reported a score of 0.49 and 0.52 in respective group. The initial Dimeglio score was 11.75 in the standard group and 10.51 in the accelerated group, the mean immediate posttreatment score was 0.79 in both groups, and at final follow-up, it was 1.25 and 1.36, respectively.
The mean number of casts required was 6.32 in the standard group and 6.14 in the accelerated group. In the study by Elgohary and Abulsaad,7) the number was 4.88 and 5.16, respectively, and in the study by Harnett et al,22) 4 and 4, respectively. In our study, percutaneous heel cord tenotomy was done in 86.42% in the standard group and in 84.41% in the accelerated group. The rates of tendoachilles tenotomy have been variably reported as <50% to 100% in various studies.23,24) In our study, the average time spent in cast was 58.52 days in the standard group and 39.38 days in the accelerated group. However, when we excluded the last cast, which was of variable duration depending on whether a tenotomy had been done or not, the average time spent in cast (before correction of equinus) was 41.02 days in the standard group and 18.18 days in the accelerated group (p < 0.001). Elgohary and Abulsaad7) reported the average time spent in cast before correction of equinus was 33.36 days in the standard group and 18.13 days in the accelerated group, while Xu25) reported 35.35 days and 20.61 days, respectively.
In our study, five of the total 158 feet had a recurrence: three feet (3.7%, two patients) in the standard group and two feet (2.6%, one patient) in the accelerated group. While Harnett et al.22) reported no recurrences at about 6 months' follow-up, Elgohary and Abulsaad7) reported a recurrence of 14.7% and 15.6 % in the two groups at a minimum 1-year follow-up (range, 12 to 48 months). The recurrence was in the form of equinus deformity in these patients and all of them did not have an initial heel cord tenotomy. The cause of recurrence in our study may be attributed to not performing an initial tenotomy. We encountered one tibial fracture in the first patient in the accelerated group at the time of brace application. Although the cause of this fracture was unidentified, the fracture healed after two more weeks of cast immobilization. Gerlach et al.26) in a 2009 study, reported two iatrogenic fractures of tibia in patients with clubfoot managed with the Ponseti technique. In one case, the distal tibial fracture was incidentally seen after clubfoot correction; in the other case, the tibial fracture was seen 24 hours after the brace application.
The Ponseti method continues to be the best approach for correction of typical congenital clubfeet. But, changing casts twice weekly greatly reduces the time patients spend in cast immobilization. In addition, in developing countries where time to clinics necessitates time away from home, work, and family, the adoption of accelerated technique can reduce costs for families and help to improve patient compliance. However, the final outcome did not show any significant difference between the two methods. The only problem we could find with the accelerated Ponseti method was that we had to dedicate two days to clubfoot clinic rather than a single day. The limitation of the study was the relatively short follow-up; a longer follow-up may reveal other significant differences between the two methods.
ACKNOWLEDGEMENTS
We thank Tariq Wani, MSc, Biostatistician, King Fahad Medical City (KFMC), for his help in preparing this manuscript.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Ponseti IV. Congenital clubfoot: fundamentals of treatment. New York, NY: Oxford University Press; 1996. p. 9. [Google Scholar]
- 2.Herring JA. Tachdjian's pediatric orthopaedics: from the Texas Scottish Rite Hospital for Children. 5th ed. Philadelphia, PA: Saunders; 2014. p. 913. [Google Scholar]
- 3.Globalclubfoot.com [Internet] Oxford: Global Clubfoot Initiative; c2019. [cited 2019 Dec 22]. Available from: http://globalclubfoot.com/countries/india. [Google Scholar]
- 4.Ponseti IV, Smoley EN. Congenital club foot: the results of treatment. Clin Orthop Relat Res. 1963;45:261–344. doi: 10.1007/s11999-009-0720-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper DM, Dietz FR. Treatment of idiopathic clubfoot: a thirty-year follow-up note. J Bone Joint Surg Am. 1995;77(10):1477–1489. doi: 10.2106/00004623-199510000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Gray K, Pacey V, Gibbons P, Little D, Burns J. Interventions for congenital talipes equinovarus (clubfoot) Cochrane Database Syst Rev. 2014;(8):CD008602. doi: 10.1002/14651858.CD008602.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elgohary HS, Abulsaad M. Traditional and accelerated Ponseti technique: a comparative study. Eur J Orthop Surg Traumatol. 2015;25(5):949–953. doi: 10.1007/s00590-015-1594-5. [DOI] [PubMed] [Google Scholar]
- 8.Pirani S. Clubfoot scoring. In: Staheli L, editor. Clubfoot: Ponseti management. 3rd ed. Seattle, WA: Global-HELP; 2009. p. 27. [Google Scholar]
- 9.Dimeglio A, Bensahel H, Souchet P, Mazeau P, Bonnet F. Classification of clubfoot. J Pediatr Orthop B. 1995;4(2):129–136. doi: 10.1097/01202412-199504020-00002. [DOI] [PubMed] [Google Scholar]
- 10.Simons GW. A standardized method for the radiographic evaluation of clubfeet. Clin Orthop Relat Res. 1978;(135):107–118. [PubMed] [Google Scholar]
- 11.Lohan I. Treatment of congenital clubfoot using the Ponseti method: workshop manual. 2nd Ed. Seattle, WA: Global-HELP; 2009. pp. 18–36. [Google Scholar]
- 12.Herring JA. Congenital talipes equinovarus (clubfoot) in Tachdjian's pediatric orthopedics. 5th ed. Philadelphia, PA: Saunders; 2014. p. 921. [Google Scholar]
- 13.Evans D. Relapsed club foot. J Bone Joint Surg Br. 1961;43(4):722–733. [Google Scholar]
- 14.Ponseti IV. Congenital clubfoot: fundamentals of treatment. New York, NY: Oxford University Press; 1996. pp. 61–81. [Google Scholar]
- 15.Cummings RJ, Davidson RS, Armstrong PF, Lehman WB. Congenital clubfoot. J Bone Joint Surg Am. 2002;84(2):290–308. doi: 10.2106/00004623-200202000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Carroll NC. Clubfoot in the twentieth century: where we were and where we may be going in the twenty-first century. J Pediatr Orthop B. 2012;21(1):1–6. doi: 10.1097/BPB.0b013e32834a99f2. [DOI] [PubMed] [Google Scholar]
- 17.Scher DM. The Ponseti method for treatment of congenital club foot. Curr Opin Pediatr. 2006;18(1):22–25. doi: 10.1097/01.mop.0000192520.48411.fa. [DOI] [PubMed] [Google Scholar]
- 18.Giesberts RB, van der Steen MC, Maathuis PG, Besselaar AT, Hekman EE, Verkerke GJ. Influence of cast change interval in the Ponseti method: a systematic review. PLoS One. 2018;13(6):e0199540. doi: 10.1371/journal.pone.0199540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Terrazas-Lafargue G, Morcuende JA. Effect of cast removal timing in the correction of idiopathic clubfoot by the Ponseti method. Iowa Orthop J. 2007;27:24–27. [PMC free article] [PubMed] [Google Scholar]
- 20.Dobbs MB, Gurnett CA. Update on clubfoot: etiology and treatment. Clin Orthop Relat Res. 2009;467(5):1146–1153. doi: 10.1007/s11999-009-0734-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elshenawy EM, Hassanen EY, Ramadam AI, Ibrahim MM. The Mansoura experience in the treatment of idiopathic clubfoot deformity using the Ponseti technique. Acta Orthop Belg. 2008;74(5):659–666. [PubMed] [Google Scholar]
- 22.Harnett P, Freeman R, Harrison WJ, Brown LC, Beckles V. An accelerated Ponseti versus the standard Ponseti method: a prospective randomised controlled trial. J Bone Joint Surg Br. 2011;93(3):404–408. doi: 10.1302/0301-620X.93B3.24450. [DOI] [PubMed] [Google Scholar]
- 23.Morcuende JA, Abbasi D, Dolan LA, Ponseti IV. Results of an accelerated Ponseti protocol for clubfoot. J Pediatr Orthop. 2005;25(5):623–626. doi: 10.1097/01.bpo.0000162015.44865.5e. [DOI] [PubMed] [Google Scholar]
- 24.Kampa R, Binks K, Dunkley M, Coates C. Multidisciplinary management of clubfeet using the Ponseti method in a district general hospital setting. J Child Orthop. 2008;2(6):463–467. doi: 10.1007/s11832-008-0134-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xu RJ. A modified Ponseti method for the treatment of idiopathic clubfoot: a preliminary report. J Pediatr Orthop. 2011;31(3):317–319. doi: 10.1097/BPO.0b013e31820f7358. [DOI] [PubMed] [Google Scholar]
- 26.Gerlach DJ, Gurnett CA, Limpaphayom N, et al. Early results of the Ponseti method for the treatment of clubfoot associated with myelomeningocele. J Bone Joint Surg Am. 2009;91(6):1350–1359. doi: 10.2106/JBJS.H.00837. [DOI] [PubMed] [Google Scholar]


