Abstract
Scarcity of donor organs and the increment in patients awaiting a transplant increased the use of organs from expanded criteria donors or donation after circulatory death. Due to the suboptimal outcomes of these donor organs, there is an increased interest in better preservation methods, such as ex vivo machine perfusion or abdominal regional perfusion to improve outcomes. This state-of-the-art review aims to discuss the available types of perfusion techniques, its potential benefits and the available evidence in kidney, liver and pancreas transplantation. Additionally, translational steps from animal models towards clinical studies will be described, as well as its application to clinical practice, with the focus on the Netherlands. Despite the lack of evidence from randomized controlled trials, currently available data suggest especially beneficial effects of normothermic regional perfusion on biliary complications and ischemic cholangiopathy after liver transplantation. For ex vivo machine perfusion in kidney transplantation, hypothermic machine perfusion has proven to be beneficial over static cold storage in a randomized controlled trial, while normothermic machine perfusion is currently under investigation. For ex vivo machine perfusion in liver transplantation, normothermic machine perfusion has proven to reduce discard rates and early allograft dysfunction. In response to clinical studies, hypothermic machine perfusion for deceased donor kidneys has already been implemented as standard of care in the Netherlands.
Keywords: Machine perfusion, Review, Kidney transplantation, Liver transplantation, Pancreas transplantation
Core tip: Scarcity of donor organs and the increment in waitlisted patients increased the use of organs from expanded criteria donors or donation after circulatory death donors. Due to suboptimal outcomes of these organs, there is an increased interest in dynamic preservation, such as ex vivo machine perfusion or abdominal regional perfusion to improve outcomes. This review discusses perfusion types, its potential benefits and the available evidence in kidney, liver and pancreas transplantation. Additionally, translational steps from animal models towards clinical studies will be described as well as its application to clinical practice, with as focus the Netherlands.
INTRODUCTION
The major obstacle in organ transplantation is the imbalance between demand and supply of suitable donor organs. In the Eurotransplant region, a total number of 14773 patients were on the active organ waiting list on 1 January 2018, while only a number of 7918 patients received a transplant from either a living or deceased donor[1,2]. Consequently, approximately 50% of the waitlisted patients did not receive an organ transplant and either remained waitlisted, became unfit for transplant or died while being waitlisted. This accentuates the urgent need to tackle organ shortage. One solution to address this problem is the increased use of suboptimal organs, such as organs from expanded criteria donors (ECD) or donation after circulatory death (DCD). However, DCD donation is not performed in several countries, mainly because of legal restrictions. Besides, ECD and DCD organs have impaired clinical outcomes based on their poor tolerance to ischemia-reperfusion injury[3]. The outcomes of DCD kidney, liver and pancreas transplantation in comparison to donation after brain death (DBD) have been previously described and are summarized in Table 1. DCD kidneys are more prone to delayed graft function (DGF) and primary non function (PNF), while graft survival is similar[4,5]. DCD livers have more frequent biliary complications, such as ischemic cholangiopathy, with corresponding inferior graft and patient survival rates[6]. For pancreas transplants from a DCD donor, the odds of graft thrombosis are 1.67 times higher compared to DBD pancreas transplants[7]. Therefore, increasing the quality of those suboptimal organs is of paramount importance.
Table 1.
Outcomes from meta-analyses or large studies comparing donation after circulatory death to donation after brain death outcomes in abdominal organ transplantation
| DCD | DBD | P value | |
| Kidney[56] | |||
| PNF (%) | 3.2 | 2.6 | 0.06 |
| DGF (%) | 48.5 | 24.9 | < 0.001a |
| 1-yr eGFR1 | 47.4 (35.6-61.2) | 48.7 (37.3-61.1) | 0.69 |
| 5-yr graft survival (%) | 76.8 | 78.1 | 0.60 |
| 5-yr patient survival (%) | 86.5 | 89.4 | < 0.001a |
| Liver[57] | |||
| Biliary complications (%) | 26 | 16 | < 0.001a |
| Ischemic cholangiopathy (%) | 16 | 3 | < 0.001a |
| 3-yr graft survival (%) | 73 | 74 | 0.01a |
| 3-yr patient survival (%) | 82 | 88 | 0.04a |
| Pancreas[7] | |||
| Graft survival | HR 0.98 (0.74-1.31) | Reference value | 0.92 |
| Patient survival | HR 1.31 (0.62-2.78) | Reference value | 0.47 |
| Graft thrombosis | OR 1.67 (1.04-2.67) | Reference value | 0.006a |
Data is presented as median and interquartile range.
Statistically significant. DBD: Donation after brain death; DCD: Donation after circulatory death; DGF: Delayed graft function; eGFR: Estimated glomerular filtration rate; HR: Hazard ratio; OR: Odds ratio; PNF: Primary non function.
The best strategy for organ preservation in an era where the use of ECD and DCD organs continues to increase is still a major topic of discussion. During the past decade, there has been renewed interest in the use of machine perfusion instead of static cold storage (SCS) as a preservation technique. The concept behind machine perfusion is dynamic reconditioning and repair through restoring blood flow of the donor organ by connecting it to a pump with the possibility to add oxygen and therapeutic agents. Besides this benefit of organ repair that may lead to improved organ quality, machine perfusion has the promising possibility to make initially discarded organs transplantable[8-10]. The second benefit is the possibility of pre-transplantation viability assessment of the donor organ "while on the pump" to prevent unnecessary transplantations with an organ that will never function in the recipient[11,12]. The third benefit is the possibility to extend the time until transplantation, for example in order to provide daytime surgery and to allow time for transfer of the donor organ to the recipient hospital.
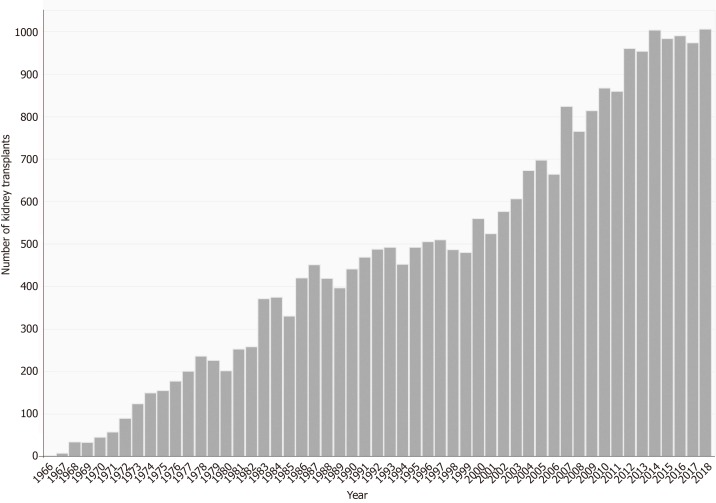
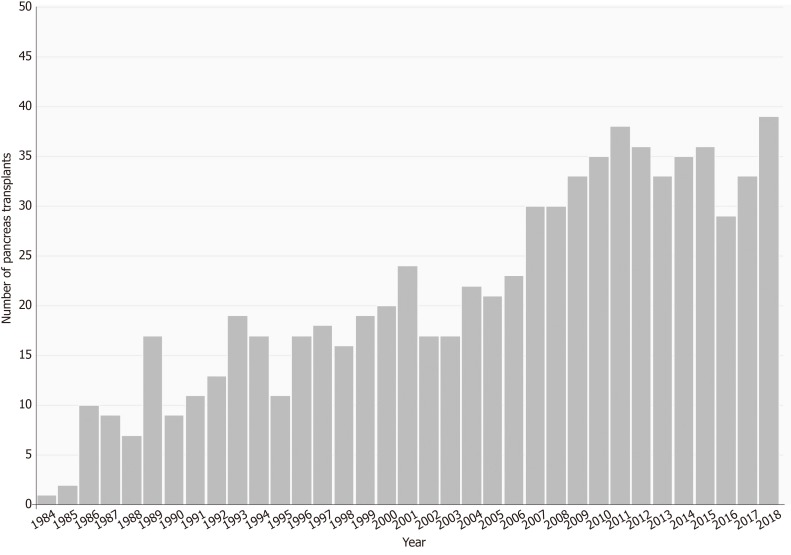
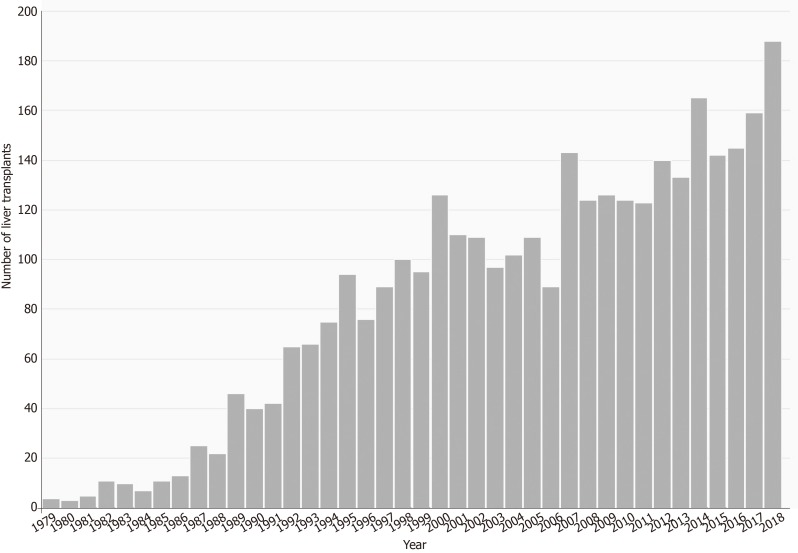
The Netherlands has a continuously growing abdominal transplantation program, as shown in Figures 1-3. In the past years, there has been an extensive increase in the DCD program. For kidney transplantation, the amount of DCD organs transplanted within the deceased donor organ transplant program was 39% in 2009, and this increased up to 55% in 2018[13,14]. For the DCD liver transplant program, this was 23% in 2009, which increased up to 39% in 2018[13,14]. For pancreas transplantation, the amount of DCD grafts used increased from 0% in 2009 to 42% in 2018[13,14]. So far, many experimental studies show the potential beneficial effects of machine perfusion in various types of organ transplantation. Many clinical studies have been recently published, translating the earlier experimental work into the clinic. Standard of care concerning organ preservation in the Netherlands already changed in response to earlier published clinical studies. With this state-of-the-art review, we aim to describe the history of machine perfusion in abdominal organ transplantation, as well as the rationale behind different types of perfusion, its potential benefits and its current use in the Netherlands as one of the pioneering countries with regard to translating machine perfusion in standard of care.
Figure 1.
Number of kidney transplantations in the Netherlands per year
Figure 3.
Number of pancreas transplantations in the Netherlands per year.
Figure 2.
Number of liver transplantations in the Netherlands per year.
HISTORY
In the 1960s, machine perfusion became part of clinical practice with its main goal to extend preservation time for cross-matching and transportation of the organ[15]. However, in the late 1980s, Folkert Belzer and James Southard[16-18] developed the University of Wisconsin solution, which improved preservation time significantly when compared to the commonly used EuroCollins solution. Because SCS was a much cheaper and simpler manner of organ preservation without compromising donor organ quality, the interest in machine perfusion decreased[19,20].
In the Netherlands, important research steps concerning preservation techniques started with the usage of hypothermic machine perfusion (HMP) on donor kidneys. In 1978, a study was published showing that kidneys severely damaged by ischemia were found to have a higher percentage of immediate function when preserved with HMP compared to SCS[21]. Five years later, an article was published wherein the clinical outcomes of 75 kidneys transplanted after HMP were compared to 2686 kidneys transplanted after SCS in the Eurotransplant region. Creatinine clearance, PNF and DGF did not differ significantly[22]. These studies raised the hypothesis that only kidneys that have been subjected to prolonged periods of warm ischemia might benefit from HMP in an era of mainly standard criteria donors[22,23]. Later on, when organ shortage forced the more frequent use of ECD donors, various clinical studies were published suggesting that HMP could result in better short-term outcomes, especially in those ECD donors[24-26]. This led to the Machine Perfusion Trial, a randomized controlled trial (RCT) executed in the Eurotransplant region with the University Medical Center Groningen as principal investigator. The results, published in 2009, showed that HMP was associated with a reduced risk of DGF and improved graft survival in the 1st year after transplantation[27].
Research concerning normothermic machine perfusion (NMP) started in the early eighties. Two important animal studies concerning normothermic ex vivo perfusion were carried out, also with the goal to allow longer preservation times[28,29]. The first study was carried out in a dog auto transplant model. Twenty-four dogs were assigned to one of four intervention groups, differing in total preservation time (96 h or 144 h) and HMP alone or interrupted with 4 h of normothermic perfusion on the animal. For both preservation times, the two groups (2 and 4) who also underwent normothermic perfusion had significantly higher creatinine clearance than the HMP only group. This suggested that interruption of HMP by normothermic perfusion improves results, which was later also confirmed in a rabbit study[28,29]. In 2002, Brasile et al[30] investigated graft function in a canine auto-transplant model using kidneys with a prolonged warm ischemia time. He found that all kidneys after NMP had direct function, in contrast to kidneys transplanted after HMP or SCS. NMP became of larger interest due the increased use of ECD organs. The hypothesis was that those organs require careful reconditioning and repair, which may not be optimal in a hypothermic environment where metabolism is suppressed. Together with the growth in the amount of ECD donors, NMP gained interest, with the first in human kidney transplantation after NMP in 2011[31]. Currently, only small clinical studies have been performed concerning NMP. An RCT comparing NMP to SCS in DCD kidney transplantation is currently ongoing in the United Kingdom, with the expected results to be published in 2020/2021 (ISRCTN15821205).
ABDOMINAL REGIONAL PERFUSION
Rationale of ARP
The development of ARP took place in Spain among uncontrolled DCD donors in a successful attempt to increase the donor pool. Abdominal regional perfusion (ARP), depending on the temperature also called normothermic regional perfusion (NRP) or hypothermic regional perfusion (HRP), is an in-vivo dynamic preservation technique that is performed while the organs are still in the donor. After withdrawal of life-sustaining support and circulatory arrest with a following period of no-touch, the donor is transferred to the operating room. In the non-ARP situation, the super-rapid recovery (SRR) technique is used to access all potential donor organs and cannulate the aorta to start cold flushing as quickly as possible, which ends the first warm ischemia time. Then, the donor organs will be inspected on eligibility for transplantation and the organs will be retrieved. In the ARP situation, cannulas will be placed in either the abdominal aorta and caval vein or in the femoral artery and femoral vein. The cannulas are connected to an extracorporeal membrane oxygenation-like device, which uses a pump to recover donor venous blood, oxygenate it and add substrates. Subsequently, the oxygenated blood will be returned to the subdiaphragmatic aorta. The thoracic aorta is clamped to prevent auto-resuscitation, which has been shown to be an effective method[32]. Depending on the law regulations per country, cannulation into the femoral vein and artery is to be performed before cardiac arrest to reduce further warm ischemia time. However, in most countries in Europe, no pre-mortem interventions are allowed by law. Besides the hypothesis that ARP improves organ quality by minimizing warm ischemia time, there are more benefits of this technique. Because the organs are still in the donor body, this creates a more physiological environment for the organs than connected to a pump outside of the body. Also, it is possible to perform viability assessment in the donor. As a third reason, ARP modifies an urgent procedure into an elective organ recovery procedure, which could reduce organ damage and organ losses due to surgical events. Also, NRP is supposed to be more cost-effective than NMP because multiple organs are resuscitated through one procedure.
Clinical outcomes after ARP
Kidney: Literature concerning kidney transplantation after ARP is scarce, and most of the literature focuses on NRP instead of HRP. Table 2 contains the core clinical studies describing clinical outcomes of kidney transplantation after ARP. A few studies also compared ARP outcomes to either DBD outcomes or outcomes after retrieval with the SRR technique. Farney et al[33] compared 25 kidney transplants after HRP to kidney transplants retrieved with the SRR technique. They concluded that kidney transplants after HRP had lower rates of DGF and shorter hospitalization. Lee et al[34] investigated 31 kidney transplant outcomes after HRP and compared those to outcomes after DBD or living donor kidney transplant. He showed a higher rate of DGF in comparison to DBD but similar incidence of acute rejection and 5-year graft and patient survival rates. Valero et al[35] described in situ perfusion with HRP and NRP. They concluded a lower incidence of DGF and PNF after NRP when compared to in situ perfusion or total body cooling[35]. Miñambres et al[36] investigated 37 kidney transplantations after NRP and compared their clinical outcomes to DBD kidney transplant outcomes. They showed that graft survival was similar to graft survival of a DBD kidney with 5% PNF and 27% DGF[36]. Also, Magliocca et al[37] compared the outcomes after NRP with DBD outcomes. They concluded no statistically significant differences in DGF, PNF and rejection. In conclusion, HRP could possibly reduce the incidence of DGF and hospitalization duration after kidney transplantation when compared with the SRR technique. Graft survival after NRP resembles DBD graft survival, which has been shown to be similar to DCD kidney graft survival using the SRR technique[5]. However, NRP may reduce the incidence of DGF and PNF.
Table 2.
Clinical studies published about kidney transplant outcomes after abdominal regional perfusion
|
Graft survival, % |
Patient survival, % |
||||||||||
| Study | n | DCD type | Rejection, % | DGF, % | PNF, % | 1 | 3 | 5 | 1 | 3 | 5 |
| HRP | |||||||||||
| Valero et al[35], 2000 | 8 | II | - | 75 | 0 | - | - | - | - | - | - |
| Koyama et al[58], 2002 | 46 | III/IV | - | 87 | 6.5 | 88.3 | - | - | - | - | - |
| Lee et al[34], 2005 | 31 | II/III/IV | 35.5 | 41.9 | 0 | 100 | - | 88.4 | 100 | - | 100 |
| Sánchez-Fructuoso et al[59], 2006 | 320 | I/II | 4.4 | 60.9 | 4.4 | 87.4 | - | 82.1 | 95 | - | 90 |
| Farney et al[33], 2011 | 25 | III | 16 | 21 | 0 | 88 | 88 | - | - | - | - |
| NRP | |||||||||||
| Valero et al[35], 2000 | 8 | II | - | 12.5 | 0 | - | - | - | - | - | - |
| Magliocca et al[37], 2005 | 24 | III | 0 | 8.3 | 0 | - | - | - | - | - | - |
| Reznik et al[60], 2011 | 20 | II | 10 | 70 | 10 | - | - | - | - | - | - |
| Hessheimer et al[61], 2015 | 158 | II | - | 65 | 9 | 88 | - | - | - | - | - |
| Oniscu et al[42], 2014 | 32 | III | - | 40 | 6 | 87.5 | - | - | 96.8 | - | - |
| Butler et al[43], 2014 | 141 | III | - | 18.2 | 9.1 | - | - | - | - | - | - |
| Rojas-Peña et al[62], 2014 | 292 | III | - | 31 | 3.5 | - | - | - | - | - | - |
| Demiselle et al[63], 2016 | 19 | II | - | 53 | 5.3 | 94 | - | - | 100 | - | - |
| Miñambres et al[36], 2017 | 37 | III | - | 27 | 5 | 91.8 | - | - | - | - | - |
Fourteen kidneys were transplanted in 11 recipients. Therefore, clinical outcomes are calculated in the 11 recipients;
Outcomes were only mentioned from their own center. DCD: Donation after circulatory death; DGF: Delayed graft function; HRP: Hypothermic regional perfusion; NRP: Normothermic regional perfusion; PNF: Primary non function.
Liver: Only incidental cases have been described concerning liver transplantation after HRP[33,38,39]. The outcomes of those transplants are not discussed separately. The results from liver transplantation after NRP are summarized in Table 3. One study by Hessheimer et al[40] compared 95 controlled DCD liver transplant outcomes after NRP to the outcomes of liver transplantation after retrieval with the SRR technique. They showed a significant decrease in favor of the NRP group for graft loss (NRP: 12%, SRR: 24%), biliary complications (NRP: 8%, SRR: 31%), ischemic cholangiopathy (NRP: 2%, SRR: 13%) and retransplantation rates (NRP: 5%, SRR: 9%). Miñambres et al[36] and Fondevila et al[41] described NRP-DCD liver transplant outcomes in comparison to DBD outcomes. They concluded that graft and patient survival after NRP-DCD liver transplantation is comparable to DBD liver transplantation. In conclusion, NRP decreases the incidence of biliary complications, ischemic cholangiopathy, graft loss and retransplantation rates when compared to the SRR technique. Graft and patient survival rates are comparable to those after DBD liver transplantation.
Table 3.
Clinical studies published about liver transplant outcomes after normothermic regional perfusion
|
Graft survival, % |
Patient survival, % |
|||||||||||
| Study | n | DCD type | Rejection, % | BC, % | IC, % | PNF, % | 1 | 3 | 5 | 1 | 3 | 5 |
| Otero et al[64], 2004 | 14 | II | 22 | - | 28 | 28 | 43 | - | - | 71 | - | - |
| Fondevila et al[41], 2007 | 10 | II | - | 10 | - | 10 | 50 | - | - | 70 | - | - |
| Jiménez-Galanes et al[65], 2009 | 20 | II | - | - | 5 | 10 | 80 | - | - | 85 | - | - |
| Fondevila et al[66], 2012 | 34 | II | - | 12 | 8 | 4.3 | - | - | - | - | - | - |
| Oniscu et al[42], 2014 | 11 | III | - | 18.2 | 0 | 9.1 | 87.5 | - | - | 96.8 | - | - |
| Butler et al[43], 2014 | 3 | III | - | - | 0 | - | - | - | - | - | - | - |
| Rojas-Peña et al[62], 2014 | 13 | III | - | - | 14.3 | 14.3 | 85.7 | - | - | - | - | - |
| Hessheimer et al[61], 2015 | 42 | II | - | - | 10 | 73 | - | - | - | - | - | |
| De Carlis et al[67], 2016 | 7 | II/III | 14.3 | 14.3 | 0 | 0 | - | - | - | - | - | - |
| Miñambres et al[36], 2017 | 11 | III | - | 0 | 0 | 9.1 | 90.9 | - | - | - | - | - |
| Hessheimer et al[40], 2019 | 95 | III | - | 8 | 2 | 2 | 88 | 88 | - | 93 | 93 | - |
BC: Biliary complications; DCD: Donation after circulatory death; IC: Ischemic cholangiopathy; NRP: Normothermic regional perfusion; PNF: Primary non function.
Pancreas: There is scarcity of studies about pancreas transplant outcomes after the use of ARP. Two aforementioned studies for kidney and liver transplant outcomes after NRP also described some anecdotal cases of pancreas transplant outcomes after NRP. Oniscu et al[42] described two combined kidney-pancreas transplants and one islet transplant after NRP, all with primary function. Miñambres et al[36] described one combined kidney-pancreas transplant after NRP, also with primary function. Butler et al[43] described two pancreas transplants after 120 minutes of NRP, both with primary function.
Current practice in the Netherlands
In October 2018, the first liver transplantation after NRP was successfully performed in Erasmus Medical Center, Rotterdam, The Netherlands. This transplantation was part of the NRP project, a collaboration between organ retrieval team West (consisting of Leiden University Medical Center and Erasmus Medical Center) and subsidized by the Ministry of Health, Welfare and Sport. The goal of this project is to increase the number of transplantable organs and to improve organ quality. NRP can be carried out in every potential DCD donor, but within the Dutch project it is currently only carried out within DCD type III donors. Different protocols exist in the literature for pump parameters during NRP. In the Dutch NRP project, a pump flow of 2-3 L per minute is pursued with a temperature starting at 33 °C that is slowly increased to 37 °C. For oxygen, a mix between air and oxygen is used with the aim to reach a PaO2 of 110-150 mmHg. Loss of volume is supplemented by adding red blood cells concentrate, albumin and Ringer’s lactate. The circuit is primed with heparin to prevent the blood from clotting. Bicarbonate is added in case of acidosis to keep the pH within a physiologic range. For the liver, the following issues are considered to determine suitability for transplantation: (1) Aspartate aminotransferase (ALAT) less than 4 times the upper limit at the end of NRP; (2) ALAT reaches its plateau phase between first and second hour; (3) Lactate below 5 mmol/L at the end of NRP; (4) Glucose doubles at the end of NRP in comparison to the start of NRP and (5) Glucose is above 10 mmol/L at the end of NRP. After 2 years, results of this project will be analyzed to see whether this technique should be implemented nationwide in the Netherlands.
EX VIVO MACHINE PERFUSION
Rationale of ex vivo machine perfusion
Whereas the goal of preserving an organ on SCS is slowing down deterioration of the donor organ, the goal of ex vivo machine perfusion is sustaining organ viability, organ repair and organ preconditioning. This all takes place in the period between procurement and transplantation of the donor organ with the main goal to optimize outcomes of the graft when transplanted in the recipient. In comparison to ARP, ex vivo machine perfusion takes place after organ retrieval, and it may also be used in case of a DBD donor organ. During ex vivo machine perfusion, the donor organ is connected to an often pressure-controlled perfusion device that pumps perfusate solution continuously through the organ vasculature. Ex vivo machine perfusion can be performed at different temperatures: Hypothermia, normothermia and subnormothermia. In comparison to SCS, HMP may be a more efficient way of cooling of the donor organ while metabolic and toxic waste products are washed out. During NMP, the temperature is within physiologic range, which increases metabolic activity and allows for active repair and reconditioning. Therefore, NMP may be more beneficial in donor organs that require reconditioning, such as ECD organs.
As normothermia leads to metabolic activity, an oxygenated perfusate is essential. Therefore, a blood-based perfusate is often used, containing washed and leukocyte-depleted red blood cells. Another option is to use an acellular perfusion solution containing a hemoglobin-based oxygen carrier. No studies have investigated which of the two is preferred. In practice, the blood-based perfusate is more popular, probably because this option is less expensive. For NMP, additional substances are added to provide the best circumstances for active repair. The composition and number of additives in the perfusate differs. In general, antibiotics, vitamins, prostaglandins, bicarbonate and heparin to prevent thrombosis are added. Currently, there is no evidence favoring one perfusate solution over another. For HMP, kidney perfusion solution-1 is used as the standard solution for clinical machine perfusion, without additional substances.
Clinical outcomes of ex vivo machine perfusion
Kidney: In abdominal organ transplantation, most clinical research concerning ex vivo machine perfusion is carried out in kidney transplants. Currently ongoing RCTs or clinical trials involving discarded kidneys are mentioned in Table 4. There is conclusive evidence for the benefits of HMP over SCS. In 2009, the aforementioned Machine Perfusion Trial of the Consortium for Organ Preservation in Europe (COPE) was published, showing that non oxygenated HMP offers a graft survival benefit in comparison to SCS and a decrease in DGF in all deceased donor kidneys[27]. Subsequently, the COPE-COMPARE trial was initiated, investigating the possible beneficial effects of adding oxygen to HMP. The preliminary results as presented on the American Transplant Conference 2019 showed that oxygenated HMP shows a significant benefit for graft survival and 1-year graft function, which is possibly mediated through a lower risk of BPAR[44]. The results from other studies, as mentioned in the Table 4, have not been published yet.
Table 4.
Currently ongoing clinical trials concerning ex vivo machine perfusion in kidney transplantation
| Name of study | Registration number | Design | PI | n | Primary outcome | Intervention | Included donors | Results |
| Unknown | ISRCTN91315246 | Non-randomized | Cambridge | 90 | Graft function | 1 h NMP | Discarded kidneys | November 2019 |
| COPE-POMP | ISRCTN63852508 | RCT | COPE Essen | 262 | Graft survival 1y | Short period HMP vs SCS only | ECD-DBD | July 2019 |
| COPE-COMPARE | ISRCTN32967929 | RCT | COPE Leuven | 162 | Kidney graft function 1 y | HMP with oxygen vs HMP without oxygen | DCD III | ↓ risk BPAR ↑ 1-y eGFR[44] |
| PIO | NCT03031067 | Case control | Bologna | 20 | Graft function | 2 h HMP vs SCS | ECD -DBD | February 2018 |
| PREDICTION | NCT02055950 | Case control | Bergamo | 60 | Kidney function | HMP vs SCS | ECD-DBD | Augustus 2018 |
| Unknown | NCT03837197 | RCT | Bologna | 260 | DGF | 2 h oxygenated HMP vs SCS | ECD-DBD | December 2021 |
| IMPULSION | NCT01170910 | RCT | Lyon | 162 | DGF | 6-8 h HMP vs SCS | ECD | August 2016 |
| Machine perfusion trial | ISRCTN83876362 | RCT | COPE Groningen | 654 | DGF | Non-oxygenated HMP vs SCS | DCD III and DBD | ↓ risk of DGF (OR 0.57) ↓ risk of graft failure (HR 0.52) ↑ allograft survival (94 vs 90%, P = 0.04)[27] |
| Unknown | ISRCTN15821205 | RCT | Cambridge | 400 | DGF | 1 h pre-transplant NMP vs SCS | DCD III and IV | January 2021 |
BPAR: Biopsy proven acute rejection; COPE: Consortium for Organ Preservation in Europe; DBD: Donation after brain death; DCD: Donation after circulatory death; DGF: Delayed graft function; ECD: Expanded criteria donor; eGFR: Estimated glomerular filtration rate; HMP: Hypothermic machine perfusion; HR: Hazard ratio; NMP: Normothermic machine perfusion; OR: Odds ratio; PI: Principal investigator; RCT: Randomized controlled trial; SCS: Static cold storage.
In contrast to HMP, clinical studies concerning the use of NMP in kidney transplantation are still in its infancy. This is possibly because NMP may be more hazardous because potential failure of NMP leads to harmful additional warm ischemia time. In 2011, the first human kidney transplant after ex vivo NMP was performed in the United Kingdom with good post-transplant outcomes[31]. Currently, there is no evidence from RCTs yet that NMP may be beneficial. However, experimental studies have already shown the benefits of NMP over HMP[45]. A phase II, multi-center RCT is currently recruiting to assess the efficacy of 1 h ex vivo NMP compared to SCS only in DCD III and IV kidney transplantation (ISRCTN15821205). However, this RCT does not answer the question whether the addition of NMP has beneficial effects in comparison to HMP only. Another study from the Cambridge group is assessing the use of NMP in discarded kidneys, with the primary aim to make them transplantable.
Liver: Currently, there are many ongoing clinical trials for liver ex vivo machine perfusion. Table 5 summarizes all ongoing RCTs and non-randomized trials in discarded livers. Oxygenated HMP, better known as HOPE in the liver transplantation field, is currently under investigation together with RCTs investigating dual hypothermic oxygenated machine perfusion (DHOPE). The results from these RCTs are expected to follow in 2020. A case control study from the Groningen group in 10 patients found a higher graft survival, a two-fold lower peak ALAT and bilirubin in livers treated with DHOPE[46].
Table 5.
Currently ongoing clinical trials concerning ex vivo machine perfusion in liver transplantation
| Name of study | Design | PI | n | Primary outcome | Intervention | Included donors | Results | |
| DHOPE DCD | NCT02584283 | RCT | Groningen | 156 | % NAS | 2 h end-ischemic DHOPE | DCD III | October 2019 |
| HOPE | NCT01317342 | RCT | Zürich | 170 | Postoperative complications | 1-2 h HOPE | DBD | July 2019 |
| HOPE ECD-DBD | NCT03124641 | RCT | Aachen | 46 | Peak ALT | 1-2 h HOPE | ECD-DBD | June 2019 |
| DHOPE-COR-NMP | NTR5972 | Non-randomized | Groningen | 16 | Graft survival | DHOPE, gradually rewarming, NMP | Discarded livers (DCD and DBD) | 11 livers transplanted 100% patient/graft survival, 9.1% ischemic cholangiopathy[48] |
| PIO | NCT03031067 | Case control | Bologna | 20 | Graft function | 2 h HOPE | ECD livers | February 2018 |
| VITTAL | NCT02740608 | Non-randomized | Birmingham | 22 | Patient survival | 4 h NMP | Discarded livers (DCD and DBD) | March 2020 |
| Liver WP2 | ISRCTN39731134 | RCT | Oxford COPE | 220 | Peak AST | Minimally 4 h NMP | All deceased donors | 49.4% ↓ peak AST[47] |
| CORNET | ISRCTN94691167 | RCT | Essen | 40 | Peak AST | 1,5 h COR until 20 degrees (dual perfusion) | ECD | February 2021 |
| DHOPE | NTR4493 | Case control | Groningen | 10 | Graft survival 6 mo | At least 2 h of DHOPE | DCD III | ↑ graft survival (P = 0.052) ↓peak ALT (P = 0.006) ↓bilirubin (P = 0.044)[46] |
| Unknown | NCT03837197 | RCT | Bologna | 260 | Early allograft dysfunction | Minimally 1 hour of HOPE | ECD-DBD | December 2021 |
ALT: Alanine aminotransferase; AST: Aspartate transaminase; COR: Controlled oxygenated rewarming; COPE: Consortium for Organ Preservation in Europe; DBD: Donation after brain death; DCD: Donation after circulatory death; DHOPE: Dual hypothermic oxygenated perfusion; DCD: Donation after circulatory death; ECD: Expanded criteria donor; HOPE: Hypothermic oxygenated perfusion; NAS: Non-anastomotic strictures; NMP: Normothermic machine perfusion; PI: Principal investigator; RCT: Randomized controlled trial
There is conclusive evidence for NMP over SCS in donor livers. In 2018, a RCT among all deceased liver donors was published comparing SCS to NMP with a minimal duration of 4 h[47]. This study showed a 49.4% reduced peak ASAT during the first 7 d post-transplant in both DCD and DBD livers[47]. Early allograft dysfunction was 74% lower than in the SCS arm. Discard rates were higher in the SCS group (24.1% vs 11.7%)[47]. However, there were no differences in biliary complications, ischemic cholangiopathy, incidence of PNF or graft and patient survival at 1 year[47]. A recently published study in discarded livers combined the use of DHOPE with subsequently controlled oxygenated rewarming and NMP[48]. From the 16 livers perfused according to the protocol, 11 were considered transplantable, which was decided based on pre-defined viability criteria. The authors conclude that the attributable percentage of transplantable livers in their center was increased 20% by using the DHOPE-COR-NMP protocol. This would have a major impact on the amount of transplantable livers if applied worldwide.
Pancreas: Machine perfusion of pancreas grafts is still in its infancy because of lower incidence of pancreas transplants. Besides, machine perfusion may increase edema of the pancreas due to its low-flow state. The use of machine perfusion in the pancreas is currently still in the pre-clinical experimental phase. Studies in the earlier years have favored SCS over HMP in preservation failure and post-transplant survival rates[49-51]. However, in more recent studies, results have been superior in machine perfusion[52]. No large data are yet available concerning the use of machine perfusion in pancreas transplantation.
Viability assessment
One of the benefits of machine perfusion is the possibility of viability assessment. However, rules concerning viability assessment are not set in stone. It still remains highly difficult, as often no highly predictive cut-offs of liver or kidney markers have been identified that could lead to either acceptance or rejection of the donor organ. Especially for HMP, viability assessment is largely unexplored.
Kidney: For NMP, Hosgood et al[8] developed a quality assessment score based on macroscopic perfusion, renal blood flow and urine output during NMP. The total amount of urine produced during NMP has proven to be significantly less in kidneys deemed unsuitable for transplantation[8]. It is unknown whether parameters during perfusion, such as flow and intrarenal resistance, may predict post-transplant outcomes.
Liver: For HOPE, fluometric analysis of released mitochondrial flavoproteins was shown to have a high predictive value of liver graft function after transplantation with an area under the curve of 0.926 for 90-day graft loss[53]. During NMP, liver viability can be assessed using a combination of transaminase release, glucose metabolism, lactate clearance and maintenance of acid-base balance[54]. Evaluation of bile pH may predict post-transplant biliary complications, such as ischemic cholangiopathy[54]. No correlation has been found for hepatic artery/portal vein resistance and hepatocellular damage[54]. Also, there was no difference in hepatic artery/portal vein resistance between non-transplanted livers and transplanted livers and transplanted and non-transplanted livers[48]. Liver enzymes, lactate and bile production has shown not to be sufficient for prediction of liver graft failure in the recipient[54]. The following criteria have been described as being associated with successful transplantation of a normothermically perfused liver[54]: (1) Maximum bile pH > 7.5; (2) Bile glucose concentration ≤ 3 mmol/L or ≥ 10 mmol less than perfusate glucose; (3) Able to maintain perfusate pH > 7.2 without >30 mmol bicarbonate supplementation; (4) Falling glucose beyond 2 hours or perfusate glucose under 10 mmol/L which, on challenge with 2.5 g glucose, does subsequently fall; (5) Peak lactate fall ≥ 4.4 mmol/L per kilogram per hour; and (6) ALAT < 6000 iU/L at 2 h.
Current practice in the Netherlands
After publication of the results of the Machine Perfusion Trial in deceased donor kidneys, a committee was established in the Netherlands to implement this technique as standard of care. As a result, since January 2016, the Netherlands is the first country where HMP is standard of care for all deceased donor kidneys. Several studies, both experimental and clinical, are carried out in the Netherlands concerning the possible additional benefits of NMP in donor kidneys. In March 2018, the first kidney transplantation after NMP in the Netherlands was performed successfully in Erasmus Medical Center in Rotterdam. It was the start of a pilot study, the POSEIDON study, to assess the feasibility of kidney transplantation after NMP in the Eurotransplant Senior program. Because of the poor results of kidney transplantation in this program, the hypothesis was that those patients may benefit the most from an effort to improve organ quality by NMP[55]. The results from the NMP patients will be compared to a historical cohort of Eurotransplant Senior Program patients that have been treated with HMP. The study finished its inclusion, and the results are expected in the beginning of 2020. Furthermore, various experimental studies are currently carried out in discarded human kidneys and porcine kidneys concerning the best perfusion parameters to use when performing NMP. One of them is the PROPER study, a collaboration between Erasmus Medical Center, Leiden Medical Center and Groningen Medical Center, with the goal to improve discarded kidneys to make them transplantable. For liver ex vivo machine perfusion, the aforementioned DHOPE, DHOPE-DCD and DHOPE-COR-NMP studies are led by Groningen Medical Center. Various experimental studies on discarded livers or animal livers are currently carried out, and the results of those are about to follow.
CONCLUSION
Since the renewed interest in machine perfusion, major steps have been made by translating experimental research into clinical studies. For NRP, there is no evidence from RCTs yet. The currently available evidence suggests especially beneficial effects for improving outcomes of liver transplantation by reducing the incidence of biliary complications and ischemic cholangiopathy. For ex vivo machine perfusion in kidney transplantation, HMP has proven to be beneficial over SCS in an RCT, while NMP is currently under investigation. For ex vivo machine perfusion in liver transplantation, NMP has proven to reduce discard rates and early allograft dysfunction. Multiple RCTs, such as the DHOPE, are ongoing from which the results are awaited. In response to clinical studies, NRP and HMP for deceased donor kidneys have already been implemented as standard of care in the Netherlands.
Footnotes
Conflict-of-interest statement: No potential conflicts of interest.
Manuscript source: Invited manuscript
Peer-review started: July 31, 2019
First decision: August 20, 2019
Article in press: December 19, 2019
Specialty type: Transplantation
Country of origin: Netherlands
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gheith O, Taheri S S-Editor: Ma RY L-Editor: Filipodia E-Editor: Xing YX
Contributor Information
Elsaline Rijkse, Division of HPB and Transplant Surgery, Department of Surgery, Erasmus MC University Medical Center, Rotterdam 3015 GD, Netherlands.
Jan NM IJzermans, Division of HPB and Transplant Surgery, Department of Surgery, Erasmus MC University Medical Center, Rotterdam 3015 GD, Netherlands.
Robert C Minnee, Division of HPB and Transplant Surgery, Department of Surgery, Erasmus MC University Medical Center, Rotterdam 3015 GD, Netherlands. r.minnee@erasmusmc.nl.
References
- 1.Eurotransplant. 3002P_All ET_all organs. Available from: http://statistics.eurotransplant.org/reportloader.php?report=56816-6141-6113&format=html&download=0.
- 2.Eurotransplant. 2052P_All ET_all organs. Available from: http://statistics.eurotransplant.org/reportloader.php?report=55913-6141-6113&format=html&download=0.
- 3.Xu J, Sayed BA, Casas-Ferreira AM, Srinivasan P, Heaton N, Rela M, Ma Y, Fuggle S, Legido-Quigley C, Jassem W. The Impact of Ischemia/Reperfusion Injury on Liver Allografts from Deceased after Cardiac Death versus Deceased after Brain Death Donors. PLoS One. 2016;11:e0148815. doi: 10.1371/journal.pone.0148815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen G, Wang C, Ko DS, Qiu J, Yuan X, Han M, Wang C, He X, Chen L. Comparison of outcomes of kidney transplantation from donation after brain death, donation after circulatory death, and donation after brain death followed by circulatory death donors. Clin Transplant. 2017;31 doi: 10.1111/ctr.13110. [DOI] [PubMed] [Google Scholar]
- 5.Schaapherder A, Wijermars LGM, de Vries DK, de Vries APJ, Bemelman FJ, van de Wetering J, van Zuilen AD, Christiaans MHL, Hilbrands LH, Baas MC, Nurmohamed AS, Berger SP, Alwayn IP, Bastiaannet E, Lindeman JHN. Equivalent Long-term Transplantation Outcomes for Kidneys Donated After Brain Death and Cardiac Death: Conclusions From a Nationwide Evaluation. EClinicalMedicine. 2018;4-5:25–31. doi: 10.1016/j.eclinm.2018.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jay CL, Lyuksemburg V, Ladner DP, Wang E, Caicedo JC, Holl JL, Abecassis MM, Skaro AI. Ischemic cholangiopathy after controlled donation after cardiac death liver transplantation: a meta-analysis. Ann Surg. 2011;253:259–264. doi: 10.1097/SLA.0b013e318204e658. [DOI] [PubMed] [Google Scholar]
- 7.Shahrestani S, Webster AC, Lam VW, Yuen L, Ryan B, Pleass HC, Hawthorne WJ. Outcomes From Pancreatic Transplantation in Donation After Cardiac Death: A Systematic Review and Meta-Analysis. Transplantation. 2017;101:122–130. doi: 10.1097/TP.0000000000001084. [DOI] [PubMed] [Google Scholar]
- 8.Hosgood SA, Thompson E, Moore T, Wilson CH, Nicholson ML. Normothermic machine perfusion for the assessment and transplantation of declined human kidneys from donation after circulatory death donors. Br J Surg. 2018;105:388–394. doi: 10.1002/bjs.10733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barlow AD, Hamed MO, Mallon DH, Brais RJ, Gribble FM, Scott MA, Howat WJ, Bradley JA, Bolton EM, Pettigrew GJ, Hosgood SA, Nicholson ML, Saeb-Parsy K. Use of Ex Vivo Normothermic Perfusion for Quality Assessment of Discarded Human Donor Pancreases. Am J Transplant. 2015;15:2475–2482. doi: 10.1111/ajt.13303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mergental H, Perera MT, Laing RW, Muiesan P, Isaac JR, Smith A, Stephenson BT, Cilliers H, Neil DA, Hübscher SG, Afford SC, Mirza DF. Transplantation of Declined Liver Allografts Following Normothermic Ex-Situ Evaluation. Am J Transplant. 2016;16:3235–3245. doi: 10.1111/ajt.13875. [DOI] [PubMed] [Google Scholar]
- 11.Hosgood SA, Barlow AD, Hunter JP, Nicholson ML. Ex vivo normothermic perfusion for quality assessment of marginal donor kidney transplants. Br J Surg. 2015;102:1433–1440. doi: 10.1002/bjs.9894. [DOI] [PubMed] [Google Scholar]
- 12.Mergental H, Stephenson BTF, Laing RW, Kirkham AJ, Neil DAH, Wallace LL, Boteon YL, Widmer J, Bhogal RH, Perera MTPR, Smith A, Reynolds GM, Yap C, Hübscher SG, Mirza DF, Afford SC. Development of Clinical Criteria for Functional Assessment to Predict Primary Nonfunction of High-Risk Livers Using Normothermic Machine Perfusion. Liver Transpl. 2018;24:1453–1469. doi: 10.1002/lt.25291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eurotransplant. 1172P_Netherlands. Available from: http://statistics.eurotransplant.org/reportloader.php?report=55474-6008&format=html&download=0.
- 14.Eurotransplant. 2212P_Netherlands. Available from: http://statistics.eurotransplant.org/reportloader.php?report=56077-6008&format=html&download=0.
- 15.Marecki H, Bozorgzadeh A, Porte RJ, Leuvenink HG, Uygun K, Martins PN. Liver ex situ machine perfusion preservation: A review of the methodology and results of large animal studies and clinical trials. Liver Transpl. 2017;23:679–695. doi: 10.1002/lt.24751. [DOI] [PubMed] [Google Scholar]
- 16.Ploeg RJ, Goossens D, McAnulty JF, Southard JH, Belzer FO. Successful 72-hour cold storage of dog kidneys with UW solution. Transplantation. 1988;46:191–196. doi: 10.1097/00007890-198808000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Kalayoglu M, Sollinger HW, Stratta RJ, D'Alessandro AM, Hoffmann RM, Pirsch JD, Belzer FO. Extended preservation of the liver for clinical transplantation. Lancet. 1988;1:617–619. doi: 10.1016/s0140-6736(88)91416-x. [DOI] [PubMed] [Google Scholar]
- 18.Todo S, Nery J, Yanaga K, Podesta L, Gordon RD, Starzl TE. Extended preservation of human liver grafts with UW solution. JAMA. 1989;261:711–714. [PMC free article] [PubMed] [Google Scholar]
- 19.Barry JM, Metcalfe JB, Farnsworth MA, Bennett WM, Hodges CV. Comparison of intracellular flushing and cold storage to machine perfusion for human kidney preservation. J Urol. 1980;123:14–16. doi: 10.1016/s0022-5347(17)55751-1. [DOI] [PubMed] [Google Scholar]
- 20.Opelz G, Terasaki PI. Advantage of cold storage over machine perfusion for preservation of cadaver kidneys. Transplantation. 1982;33:64–68. doi: 10.1097/00007890-198201000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Slooff MJ, van der Wijk J, Rijkmans BG, Kootstra G. Machine perfusion versus cold storage for preservation of kidneys before transplantation. Arch Chir Neerl. 1978;30:83–90. [PubMed] [Google Scholar]
- 22.van der Vliet JA, Vroemen JP, Cohen B, Lansbergen Q, Kootstra G. Preservation of cadaveric kidneys. Cold storage or machine perfusion? Arch Surg. 1983;118:1166–1168. doi: 10.1001/archsurg.1983.01390100040010. [DOI] [PubMed] [Google Scholar]
- 23.Daemen JH, de Vries B, Oomen AP, DeMeester J, Kootstra G. Effect of machine perfusion preservation on delayed graft function in non-heart-beating donor kidneys--early results. Transpl Int. 1997;10:317–322. doi: 10.1007/s001470050063. [DOI] [PubMed] [Google Scholar]
- 24.Wight J, Chilcott J, Holmes M, Brewer N. The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors. Health Technol Assess. 2003;7:1–94. doi: 10.3310/hta7250. [DOI] [PubMed] [Google Scholar]
- 25.Wight JP, Chilcott JB, Holmes MW, Brewer N. Pulsatile machine perfusion vs. cold storage of kidneys for transplantation: a rapid and systematic review. Clin Transplant. 2003;17:293–307. doi: 10.1034/j.1399-0012.2003.00077.x. [DOI] [PubMed] [Google Scholar]
- 26.Schold JD, Kaplan B, Howard RJ, Reed AI, Foley DP, Meier-Kriesche HU. Are we frozen in time? Analysis of the utilization and efficacy of pulsatile perfusion in renal transplantation. Am J Transplant. 2005;5:1681–1688. doi: 10.1111/j.1600-6143.2005.00910.x. [DOI] [PubMed] [Google Scholar]
- 27.Moers C, Smits JM, Maathuis MH, Treckmann J, van Gelder F, Napieralski BP, van Kasterop-Kutz M, van der Heide JJ, Squifflet JP, van Heurn E, Kirste GR, Rahmel A, Leuvenink HG, Paul A, Pirenne J, Ploeg RJ. Machine perfusion or cold storage in deceased-donor kidney transplantation. N Engl J Med. 2009;360:7–19. doi: 10.1056/NEJMoa0802289. [DOI] [PubMed] [Google Scholar]
- 28.Rijkmans BG, Van der Wijk J, Donker AJ, Slooff MJ, Kootstra G. Functional studies in 6 days successful preserved canine kidneys. J Urol. 1982;127:163–166. doi: 10.1016/s0022-5347(17)53653-8. [DOI] [PubMed] [Google Scholar]
- 29.van der Wijk J, Slooff MJ, Rijkmans BG, Kootstra G. Successful 96- and 144-hour experimental kidney preservation: a combination of standard machine preservation and newly developed normothermic ex vivo perfusion. Cryobiology. 1980;17:473–477. doi: 10.1016/0011-2240(80)90057-7. [DOI] [PubMed] [Google Scholar]
- 30.Brasile L, Stubenitsky BM, Booster MH, Lindell S, Araneda D, Buck C, Bradfield J, Haisch CE, Kootstra G. Overcoming severe renal ischemia: the role of ex vivo warm perfusion. Transplantation. 2002;73:897–901. doi: 10.1097/00007890-200203270-00011. [DOI] [PubMed] [Google Scholar]
- 31.Hosgood SA, Nicholson ML. First in man renal transplantation after ex vivo normothermic perfusion. Transplantation. 2011;92:735–738. doi: 10.1097/TP.0b013e31822d4e04. [DOI] [PubMed] [Google Scholar]
- 32.Shapey IM, Summers A, Augustine T, van Dellen D. Systematic review to assess the possibility of return of cerebral and cardiac activity after normothermic regional perfusion for donors after circulatory death. Br J Surg. 2019;106:174–180. doi: 10.1002/bjs.11046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Farney AC, Hines MH, al-Geizawi S, Rogers J, Stratta RJ. Lessons learned from a single center's experience with 134 donation after cardiac death donor kidney transplants. J Am Coll Surg. 2011;212:440–51; discussion 451-453. doi: 10.1016/j.jamcollsurg.2010.12.033. [DOI] [PubMed] [Google Scholar]
- 34.Lee CY, Tsai MK, Ko WJ, Chang CJ, Hu RH, Chueh SC, Lai MK, Lee PH. Expanding the donor pool: use of renal transplants from non-heart-beating donors supported with extracorporeal membrane oxygenation. Clin Transplant. 2005;19:383–390. doi: 10.1111/j.1399-0012.2005.00358.x. [DOI] [PubMed] [Google Scholar]
- 35.Valero R, Cabrer C, Oppenheimer F, Trias E, Sánchez-Ibáñez J, De Cabo FM, Navarro A, Paredes D, Alcaraz A, Gutiérrez R, Manyalich M. Normothermic recirculation reduces primary graft dysfunction of kidneys obtained from non-heart-beating donors. Transpl Int. 2000;13:303–310. doi: 10.1007/s001470050706. [DOI] [PubMed] [Google Scholar]
- 36.Miñambres E, Suberviola B, Dominguez-Gil B, Rodrigo E, Ruiz-San Millan JC, Rodríguez-San Juan JC, Ballesteros MA. Improving the Outcomes of Organs Obtained From Controlled Donation After Circulatory Death Donors Using Abdominal Normothermic Regional Perfusion. Am J Transplant. 2017;17:2165–2172. doi: 10.1111/ajt.14214. [DOI] [PubMed] [Google Scholar]
- 37.Magliocca JF, Magee JC, Rowe SA, Gravel MT, Chenault RH 2nd, Merion RM, Punch JD, Bartlett RH, Hemmila MR. Extracorporeal support for organ donation after cardiac death effectively expands the donor pool. J Trauma. 2005;58:1095–101; discussion 1101-2. doi: 10.1097/01.ta.0000169949.82778.df. [DOI] [PubMed] [Google Scholar]
- 38.Suárez F, Otero A, Solla M, Arnal F, Lorenzo MJ, Marini M, Vázquez-Iglesias JL, Gómez M. Biliary complications after liver transplantation from maastricht category-2 non-heart-beating donors. Transplantation. 2008;85:9–14. doi: 10.1097/01.tp.0000297945.83430.ce. [DOI] [PubMed] [Google Scholar]
- 39.Wang CC, Wang SH, Lin CC, Liu YW, Yong CC, Yang CH, Huang KC, Lin TS, Jawan B, Cheng YF, Eng HL, Concejero AM, Chen CL. Liver transplantation from an uncontrolled non-heart-beating donor maintained on extracorporeal membrane oxygenation. Transplant Proc. 2005;37:4331–4333. doi: 10.1016/j.transproceed.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 40.Hessheimer AJ, Coll E, Torres F, Ruíz P, Gastaca M, Rivas JI, Gómez M, Sánchez B, Santoyo J, Ramírez P, Parrilla P, Marín LM, Gómez-Bravo MÁ, García-Valdecasas JC, López-Monclús J, Boscá A, López-Andújar R, Fundora-Suárez J, Villar J, García-Sesma Á, Jiménez C, Rodríguez-Laíz G, Lladó L, Rodríguez JC, Barrera M, Charco R, López-Baena JÁ, Briceño J, Pardo F, Blanco G, Pacheco D, Domínguez-Gil B, Sánchez Turrión V, Fondevila C. Normothermic regional perfusion vs. super-rapid recovery in controlled donation after circulatory death liver transplantation. J Hepatol. 2019;70:658–665. doi: 10.1016/j.jhep.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 41.Fondevila C, Hessheimer AJ, Ruiz A, Calatayud D, Ferrer J, Charco R, Fuster J, Navasa M, Rimola A, Taurá P, Ginés P, Manyalich M, García-Valdecasas JC. Liver transplant using donors after unexpected cardiac death: novel preservation protocol and acceptance criteria. Am J Transplant. 2007;7:1849–1855. doi: 10.1111/j.1600-6143.2007.01846.x. [DOI] [PubMed] [Google Scholar]
- 42.Oniscu GC, Randle LV, Muiesan P, Butler AJ, Currie IS, Perera MT, Forsythe JL, Watson CJ. In situ normothermic regional perfusion for controlled donation after circulatory death--the United Kingdom experience. Am J Transplant. 2014;14:2846–2854. doi: 10.1111/ajt.12927. [DOI] [PubMed] [Google Scholar]
- 43.Butler AJ, Randle LV, Watson CJ. Normothermic regional perfusion for donation after circulatory death without prior heparinization. Transplantation. 2014;97:1272–1278. doi: 10.1097/TP.0000000000000082. [DOI] [PubMed] [Google Scholar]
- 44.2019 American Transplant Congress Abstracts. Am J Transplant. 2019;19 Suppl 3:5–1167. doi: 10.1111/ajt.15404. [DOI] [PubMed] [Google Scholar]
- 45.Hameed AM, Pleass HC, Wong G, Hawthorne WJ. Maximizing kidneys for transplantation using machine perfusion: from the past to the future: A comprehensive systematic review and meta-analysis. Medicine (Baltimore) 2016;95:e5083. doi: 10.1097/MD.0000000000005083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van Rijn R, Karimian N, Matton APM, Burlage LC, Westerkamp AC, van den Berg AP, de Kleine RHJ, de Boer MT, Lisman T, Porte RJ. Dual hypothermic oxygenated machine perfusion in liver transplants donated after circulatory death. Br J Surg. 2017;104:907–917. doi: 10.1002/bjs.10515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nasralla D, Coussios CC, Mergental H, Akhtar MZ, Butler AJ, Ceresa CDL, Chiocchia V, Dutton SJ, García-Valdecasas JC, Heaton N, Imber C, Jassem W, Jochmans I, Karani J, Knight SR, Kocabayoglu P, Malagò M, Mirza D, Morris PJ, Pallan A, Paul A, Pavel M, Perera MTPR, Pirenne J, Ravikumar R, Russell L, Upponi S, Watson CJE, Weissenbacher A, Ploeg RJ, Friend PJ Consortium for Organ Preservation in Europe. A randomized trial of normothermic preservation in liver transplantation. Nature. 2018;557:50–56. doi: 10.1038/s41586-018-0047-9. [DOI] [PubMed] [Google Scholar]
- 48.van Leeuwen OB, de Vries Y, Fujiyoshi M, Nijsten MWN, Ubbink R, Pelgrim GJ, Werner MJM, Reyntjens KMEM, van den Berg AP, de Boer MT, de Kleine RHJ, Lisman T, de Meijer VE, Porte RJ. Transplantation of High-risk Donor Livers After Ex Situ Resuscitation and Assessment Using Combined Hypo- and Normothermic Machine Perfusion: A Prospective Clinical Trial. Ann Surg. 2019 doi: 10.1097/SLA.0000000000003540. [DOI] [PubMed] [Google Scholar]
- 49.Brynger H. Twenty-four-hour preservation of the duct-ligated canine pancreatic allograft. Eur Surg Res. 1975;7:341–354. doi: 10.1159/000127819. [DOI] [PubMed] [Google Scholar]
- 50.Florack G, Sutherland DE, Heil J, Squifflet JP, Najarian JS. Preservation of canine segmental pancreatic autografts: cold storage versus pulsatile machine perfusion. J Surg Res. 1983;34:493–504. doi: 10.1016/0022-4804(83)90101-4. [DOI] [PubMed] [Google Scholar]
- 51.Toledo-Pereyra LH, Valjee KD, Chee M, Lillehei RC. Preservation of the pancreas for transplantation. Surg Gynecol Obstet. 1979;148:57–61. [PubMed] [Google Scholar]
- 52.Leemkuil M, Lier G, Engelse MA, Ploeg RJ, de Koning EJP, 't Hart NA, Krikke C, Leuvenink HGD. Hypothermic Oxygenated Machine Perfusion of the Human Donor Pancreas. Transplant Direct. 2018;4:e388. doi: 10.1097/TXD.0000000000000829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dutkowski P, Muller X, Schlegel A, Kron P, Eshmuminov D, Würdinger M, Meierhofer D, Clavien P-A. PS-168-Novel real time prediction of liver graft function during hypothermic oxygenated machine perfusion prior to liver transplantation. Journal of Hepatology. 2019;70:e104–e105. doi: 10.1097/SLA.0000000000003513. [DOI] [PubMed] [Google Scholar]
- 54.Watson CJE, Kosmoliaptsis V, Pley C, Randle L, Fear C, Crick K, Gimson AE, Allison M, Upponi S, Brais R, Jochmans I, Butler AJ. Observations on the ex situ perfusion of livers for transplantation. Am J Transplant. 2018;18:2005–2020. doi: 10.1111/ajt.14687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Peters-Sengers H, Berger SP, Heemskerk MB, Al Arashi D, Homan van der Heide JJ, Hemke AC, Ten Berge IJ, Idu MM, Betjes MG, van Zuilen AD, Hilbrands LB, de Vries AP, Nurmohamed AS, Christiaans MH, Ernest van Heurn LW, de Fijter JW, Bemelman FJ. Stretching the Limits of Renal Transplantation in Elderly Recipients of Grafts from Elderly Deceased Donors. J Am Soc Nephrol. 2017;28:621–631. doi: 10.1681/ASN.2015080879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Summers DM, Watson CJ, Pettigrew GJ, Johnson RJ, Collett D, Neuberger JM, Bradley JA. Kidney donation after circulatory death (DCD): state of the art. Kidney Int. 2015;88:241–249. doi: 10.1038/ki.2015.88. [DOI] [PubMed] [Google Scholar]
- 57.O'Neill S, Roebuck A, Khoo E, Wigmore SJ, Harrison EM. A meta-analysis and meta-regression of outcomes including biliary complications in donation after cardiac death liver transplantation. Transpl Int. 2014;27:1159–1174. doi: 10.1111/tri.12403. [DOI] [PubMed] [Google Scholar]
- 58.Koyama I, Shinozuka N, Miyazawa M, Watanabe T. Total body cooling using cardiopulmonary bypass for procurement from non-heart-beating donors. Transplant Proc. 2002;34:2602–2603. doi: 10.1016/s0041-1345(02)03441-3. [DOI] [PubMed] [Google Scholar]
- 59.Sánchez-Fructuoso AI, Marques M, Prats D, Conesa J, Calvo N, Pérez-Contín MJ, Blazquez J, Fernández C, Corral E, Del Río F, Núñez JR, Barrientos A. Victims of cardiac arrest occurring outside the hospital: A source of transplantable kidneys. Ann Intern Med. 2006;145:157–164. doi: 10.7326/0003-4819-145-3-200608010-00003. [DOI] [PubMed] [Google Scholar]
- 60.Reznik O, Skvortsov A, Loginov I, Ananyev A, Bagnenko S, Moysyuk Y. Kidney from uncontrolled donors after cardiac death with one hour warm ischemic time: resuscitation by extracorporal normothermic abdominal perfusion "in situ" by leukocytes-free oxygenated blood. Clin Transplant. 2011;25:511–516. doi: 10.1111/j.1399-0012.2010.01333.x. [DOI] [PubMed] [Google Scholar]
- 61.Hessheimer AJ, Billault C, Barrou B, Fondevila C. Hypothermic or normothermic abdominal regional perfusion in high-risk donors with extended warm ischemia times: impact on outcomes? Transpl Int. 2015;28:700–707. doi: 10.1111/tri.12344. [DOI] [PubMed] [Google Scholar]
- 62.Rojas-Peña A, Sall LE, Gravel MT, Cooley EG, Pelletier SJ, Bartlett RH, Punch JD. Donation after circulatory determination of death: the university of michigan experience with extracorporeal support. Transplantation. 2014;98:328–334. doi: 10.1097/TP.0000000000000070. [DOI] [PubMed] [Google Scholar]
- 63.Demiselle J, Augusto JF, Videcoq M, Legeard E, Dubé L, Templier F, Renaudin K, Sayegh J, Karam G, Blancho G, Dantal J. Transplantation of kidneys from uncontrolled donation after circulatory determination of death: comparison with brain death donors with or without extended criteria and impact of normothermic regional perfusion. Transpl Int. 2016;29:432–442. doi: 10.1111/tri.12722. [DOI] [PubMed] [Google Scholar]
- 64.Otero A, Gómez-Gutiérrez M, Suárez F, Arnal F, Fernández-García A, Aguirrezabalaga J, García-Buitrón J, Alvarez J, Máñez R. Liver transplantation from maastricht category 2 non-heart-beating donors: a source to increase the donor pool? Transplant Proc. 2004;36:747–750. doi: 10.1016/j.transproceed.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 65.Jiménez-Galanes S, Meneu-Diaz MJ, Elola-Olaso AM, Pérez-Saborido B, Yiliam FS, Calvo AG, Usera MA, González MC, González JC, González EM. Liver transplantation using uncontrolled non-heart-beating donors under normothermic extracorporeal membrane oxygenation. Liver Transpl. 2009;15:1110–1118. doi: 10.1002/lt.21867. [DOI] [PubMed] [Google Scholar]
- 66.Fondevila C, Hessheimer AJ, Flores E, Ruiz A, Mestres N, Calatayud D, Paredes D, Rodríguez C, Fuster J, Navasa M, Rimola A, Taurá P, García-Valdecasas JC. Applicability and results of Maastricht type 2 donation after cardiac death liver transplantation. Am J Transplant. 2012;12:162–170. doi: 10.1111/j.1600-6143.2011.03834.x. [DOI] [PubMed] [Google Scholar]
- 67.De Carlis R, Di Sandro S, Lauterio A, Ferla F, Dell'Acqua A, Zanierato M, De Carlis L. Successful donation after cardiac death liver transplants with prolonged warm ischemia time using normothermic regional perfusion. Liver Transpl. 2017;23:166–173. doi: 10.1002/lt.24666. [DOI] [PubMed] [Google Scholar]