Abstract
Kidney transplant provides superior outcomes to dialysis as a treatment for end-stage kidney disease. Therefore, it is essential that kidney transplantation be part of an integrated treatment and management plan for chronic kidney disease (CKD). Developing an effective national program of transplantation is challenging because of the requirement for kidney donors and the need for a multidisciplinary team to provide expert care for both donors and recipients. This article outlines the steps necessary to establish a national kidney transplant program, starting with the requirement for effective legislation that provides the legal framework for transplantation whilst protecting organ donors, their families, recipients, and staff and is an essential requirement to combat organ trafficking. The next steps involve capacity building with the development of a multiskilled workforce, the credentialing of transplant centers, and the reporting of outcomes through national or regional registries. Although it is accepted that most transplant programs will begin with living related kidney donation, it is essential to aspire to and develop a deceased donor program. This requires engagement with multiple stakeholders, especially the patients, the general community, intensivists, and health departments. Development of transplant centers should be undertaken in concert with the development of a dialysis program. Both are essential components of integrated care for CKD and both should be viewed as part of the World Health Organization’s initiative for universal health coverage. Provisions to cover the costs of treatment for patients need to be developed taking into account the state of development of the overall health framework in each country.
Keywords: chronic kidney disease, integrated care, kidney transplantation, sustainable care, universal health care
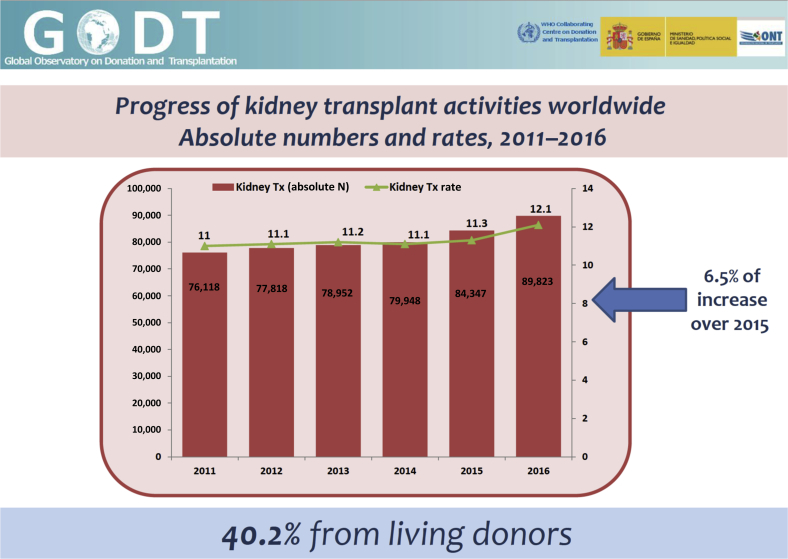
Kidney transplantation remains the preferred treatment for end-stage kidney disease (ESKD). Several large registry-based studies comparing transplanted versus waitlisted patients have demonstrated that kidney transplantation is lifesaving compared with dialysis.1 This is the case for all age groups and for all causes of ESKD. It has also been shown to provide a better quality of life, and, when compared with dialysis, kidney transplantation is cost saving, irrespective of age or comorbidities.2 Although these data have come from developed countries with established deceased donor programs, it is likely to be true for developing countries, as dialysis is very expensive in developing countries, and transplantation with generic immunosuppression will be cheaper after the first 12 months of treatment. According to the ONT-WHO Global Observatory on Donation and Transplantation, there were 89,823 kidney transplants performed worldwide in 2016; 36,109 of these (40.2%) were from living donors.3 Compared with 2015, this was a 7.25% improvement in the total number of kidney transplants and represents an increase in global activity year on year for the past several years (Figure 1).3 However, it is still calculated to be providing less than 10% of global needs.3 Although The Transplantation Society considers it an obligation of health authorities to report their data to the Global Observatory, only 81 of the 192 member states reported their transplant activity for 2016, and the aggregate data from 2011 to 2016 contains data from only 110 member states. Hence, the data reported here are considered to underestimate the overall activity. Nevertheless, it is the most comprehensive available and is useful for developing pragmatic strategies to expand both organ donation and transplantation.
Figure 1.
Global kidney transplant activity from the World Health Organization (WHO)–Spanish Transplant Organization (ONT) Global Observatory on Donation and Transplantation (GODT). Data are provided by national health authorities in WHO member states whenever transplantation (Tx) programs do exist. The figure is based on the aggregate data reported by 100 member states between 2011 and 2016, based on the GODT data, produced by the WHO-ONT collaboration (see Global Observatory on Donation and Transplantation. Organ Donation and Transplantation Activities. 2016. Available at: http://www.transplant-observatory.org/2016-activity-data/. Accessed November 18, 2018.3).
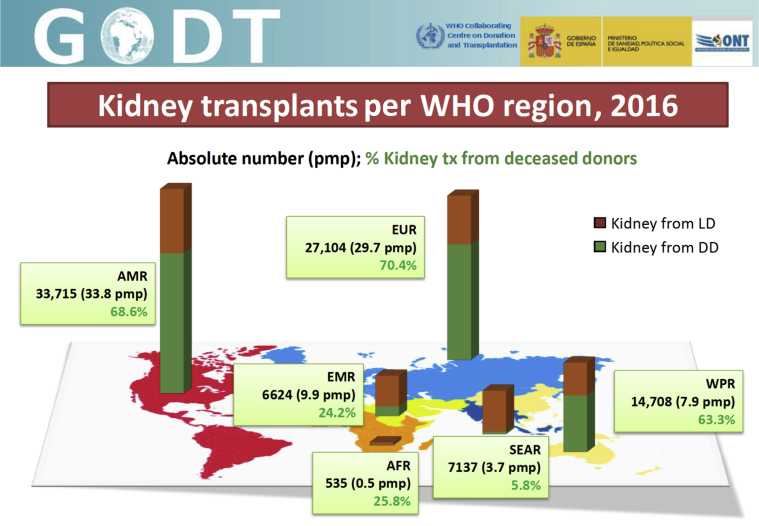
There are wide disparities in access to—and use of—transplantation. Kidney transplants are being performed in at least 100 of the 196 countries.3 Living donor kidney transplants were performed in 98 countries and transplants from deceased donors performed in 76. Figure 2 shows the distribution of kidney transplants by World Health Organization (WHO) region.3 In particular, Africa has a very low transplant rate, with only 535 kidney transplants performed (0.5 per million population [pmp]) in 2016 in a very variable distribution, as many countries have no transplantation programs.3 The majority of kidney transplants were performed in South Africa, Tunisia, and—to a lesser extent—in the Sudan. The majority of transplants occur in high-income countries (HIC) and these regions generally have higher rates of deceased donation, with deceased donors being more common than live donors in the Americas, Europe, and Western Pacific. By contrast, deceased donation rates are exceptionally low in South East Asia, making only 5.8% of all kidney transplants, although this is an increase on 2015 data. By contrast, in North America, 33,715 (32.8 pmp) kidney transplants were performed, and 10,519 were from live donors (31.2%); in Europe, there were 27,104 kidney transplants (29.7 pmp), and 29.6% were live donor transplants.
Figure 2.
The number of reported deceased and live donor (LD) transplants in 2016 from each of the World Health Organization (WHO) regions. Data are provided by national health authorities in WHO member states whenever transplantation (tx) programs do exist. Rates are estimated using the regional population as the denominator. Data are based on the Global Observatory on Donation and Transplantation (GODT) data, produced by the WHO-ONT collaboration (see Global Observatory on Donation and Transplantation. Organ Donation and Transplantation Activities. 2016. Available at: http://www.transplant-observatory.org/2016-activity-data/. Accessed November 18, 2018.3). AFR, African Region; AMR, Americas Region; DD, deceased donors; EMR, Eastern-Mediterranean Region; EUR, European Region; ONT, Spanish Transplant Organization; pmp, per million population; SEAR, South-East-Asia Region; WPR, Western-Pacific Region.
Basic Requirements for Effective Transplantation
The issue that separates transplantation from most other medical therapies is that the source of the product is a human donor. Their rights and well-being must be protected, as must that of the medical professionals involved. Hence, transplantation cannot occur without relevant legislation and regulatory oversight. From this follows a list of health ministry, hospital, and medical professional responsibilities, which must all be in place for a successful national program of kidney transplantation.
A broad summary of the regulatory requirements follows:
-
•
Legality of organ donation (both living and deceased) underpinned by legislation. All countries should introduce such legislation, as it will help facilitate the introduction and expansion of transplantation. To our knowledge, the majority of African nations have no legislation on organ donation and/or transplantation. According to a recent publication, legislation pertaining to organ donation and transplantation is limited to South Africa, Tunisia, Nigeria, Ghana, Kenya, and Cameroon.4
-
•
Development of regulations based on legislation.
-
•
Oversight of organ donation and transplantation by health departments and development of an agency to oversee organ donation to ensure transparency and safety. Kidney transplantation is a complex multidisciplinary activity, even for live-donor kidney transplant programs. This is best developed with involvement of the national health department, even if there is only a single center within a country. The complexity of the degree of centralized regulation will vary according to level of economic development and the number and nature of the transplant programs that exist. However, a system of national regulation of transplant program(s) is essential to ensure equity, safety, ethical adherence to legislation, and to monitor clinical standards and outcomes. Historically, countries with emerging transplant programs begin with live-donor transplantation. Successful live donor programs can be established with substantially fewer resources than a comprehensive transplant program with both deceased and living-donor transplantation. However, even a small transplant program requires a team approach. Transplant recipients require lifelong care on immunosuppression, and there needs to be well-defined shared responsibilities between the transplanting center and the caring physician who may live many kilometers away. Health authorities are best placed to plan the expansion from a single transplant program to the development of multiple programs and to ensure that the whole population is served.
-
•
Credentialing of kidney transplant centers to ensure appropriate standards. As most emerging transplant programs begin with live donation, there is an obligation to ensure that the transplant center has the skills and expertise to carry this out safely and effectively. In addition, it is essential to ensure that transplant outcomes meet appropriate standards. The complexity of this process will vary according to the relative level of development of the health care system in any given country and the types of transplantation being undertaken. However, it is a fundamental requirement for all transplant programs. The reporting of outcomes both short-term and long-term, for both the donor and the recipient, would be a basic minimum requirement.
-
•
All national kidney transplant programs should ultimately aspire to development of a deceased organ donor program. The challenges of this should not be underestimated, even in developed economies. It requires an integrated approach to ESKD care with well-established referral patterns from nephology centers, cooperation and involvement of intensive-care unit (ICU) and high-dependency unit (HDU) specialists as well as organ procurement teams and human leukocyte antigen (HLA) laboratories that are ideally available 24 hours a day. It also requires the support and involvement of the general community. The development of a just and transparent allocation system is an essential component of this system in which allocation priorities are consistent with community expectations and not swayed by considerations of financial gain or patients’ social status.
-
•
Development of national registries and auditing of agencies and transplant centers. Reporting of results is an essential component of a successful transplant program. With the establishment of a single transplant center in a country, outcomes will initially be monitored by that center. However, all countries should establish a national registry of transplantation in which basic outcomes are reported at the earliest opportunity.
-
•
Funding mechanism to establish and maintain a national kidney transplant program. Development of a successful transplant program, especially a program that has deceased organ donation, relies on equity of access. Kidney transplantation is an expensive procedure, and patients require lifelong monitoring and immunosuppression. In many respects, post-transplant care is equally or more important than the surgery and can lead to catastrophic health expenditure if the costs of immunosuppression are not covered or subsidized in some way. Hence, a national insurance scheme or funding mechanism is required to develop an effective national transplant program.
Minimal Infrastructure Requirements and Specialist Personnel
It is acknowledged that the level of infrastructure and the number of specialized personnel involved in a kidney transplant program depends on many factors. Important aspects to consider in developing this are the following:
-
•
developmental status and income of the country
-
•
sophistication of the health care system
-
•
existing dialysis programs
-
•
anticipated transplant activity, and
-
•
access to specialized personnel.
In newly developed programs, many of the positions will be filled by specialists who have an interest in kidney transplantation rather than it being a full-time occupation. Regardless, these specialized personnel need to be identified and involved in the early stages of development so that expertise in all aspects of transplantation can be developed as the experience of the unit increases. Because of the multidisciplinary nature of transplantation, ideally, this should be performed in a tertiary care hospital. For appropriate selection of donor recipient pairs, access to an HLA laboratory is essential. In centers that perform live-donor transplantation only, a national HLA laboratory is not essential, provided there is access to a reliable regional laboratory. As national programs grow, an HLA laboratory will be required, and this should be planned for from the earliest stages. This can be supported by a clinical partnership with a regional or international transplant center with extensive existing experience. Access to supportive dialysis in the kidney transplantation center is critical to act as a bridge to transplantation for many patients and to provide support in the situation of delayed transplant function. After transplantation, patients require long-term immunosuppression. This will require drug monitoring, supervision by a physician trained in transplantation, and involvement of a hospital pharmacist. As a consequence of long-term immunosuppression, transplant recipients are at increased risk of opportunistic infections, and infection is a major cause of death in kidney transplant patients, especially in developing countries with high rates of endemic infections such as tuberculosis. Clinicians with expertise in infectious disease and access to reliable microbiology laboratory services are essential components of an integrated transplant program. This may be supported by regional services initially with the aim of developing appropriate local infrastructure as the program evolves. Monitoring the kidney transplant long-term and the ability to diagnose the cause of acute graft loss accurately requires the involvement of a skilled histopathologist. As with other specialized services, this can be supported by a partnership with a regional center or established transplant center elsewhere. However, a process for providing timely reports for treatment decisions is essential. Optimally, a local pathologist should be involved with the intention of developing appropriate local expertise within the transplant center in due course.
Because of the multidisciplinary nature of kidney transplantation and the requirement of highly specialized personnel, transplant centers are usually regionally based. Therefore, there needs to be well-established lines of referral from nephrologists and dialysis centers so that patients have access to pretransplant assessment for suitability and a central resource for ongoing advice on management. A team of surgeons, physicians, and specialized nurses who are well trained in post-transplant management are needed to care for both the donor and recipient.
The expansion of the transplant program to include deceased donor programs requires the involvement of ICU and HDU. Establishing good links with the relevant specialists within the region is needed to develop such a program. Developing and encouraging their support and involvement from the earliest stages is essential to the success of such a program. It requires the establishment of an organ procurement team (for deceased donation).
Gaps in Capacity and Knowledge
To expand global access to organ donation and transplantation it is necessary to identify gaps in capacity. Without a good understanding of the deficiencies in infrastructure and personnel required to develop transplantation in low- and middle-income countries (LMIC), scarce resources will be wasted. Several issues that have been identified as important components of a developing national transplant program are outlined here. Lack of capacity in these areas needs to be explored at a country level to ensure that strategies to fill these gaps are put in place early in the planning of transplant programs.
Legislation and regulation
Clear unambiguous legislation and regulation is the foundation of a successful organ donation and transplantation system, regardless of whether deceased organ donation is occurring or not.5 In addition to protecting staff, it is essential for the protection of donors from exploitation and the elimination of organ trafficking. Since the Madrid Resolution, there has been an increase in the number of countries with appropriate legislation.5 However, in parts of Asia and Africa, this essential component is lacking.4 At this time, it remains unclear how many countries lack appropriate legislation. For those with legislation, it is not clear whether there are clear definitions of death to enable deceased organ donation.
Health financing and insurance
Transplantation is expensive, although not as expensive as dialysis over the long term.2 Nevertheless, it is beyond the capacity of most individuals to cover the costs. Unless there is insurance, out-of-pocket payments can lead to catastrophic health expenditure on all modalities of kidney replacement therapy (KRT).6 An inability to afford the cost of immunosuppressive medication can lead to premature graft loss from rejection. Although costs for transplantation are less than that of dialysis, public funding for transplantation occurs in only 49% of countries.7 Not unexpectedly, public funding of transplantation is highest in HIC and very limited in LIC. As a result, poorer countries with a high burden of disease have little or no access to KRT, including transplantation. However, many developing countries are starting to provide dialysis for ESKD. A number of funding models are used to facilitate public funding of dialysis, including raising dedicated funds through taxation and the use of charity schemes.8,9 Although there is some expansion of dialysis using these models, it remains rudimentary or nonexistent for transplantation.
Health workforce
Kidney transplantation is a highly skilled, multidisciplinary procedure. It requires a specialist workforce with the appropriate qualifications. It extends beyond transplant surgeons and nephrologists; it requires anesthetists, skilled nurses, pharmacists, histopathologists, and scientists to run an HLA laboratory. Although it is possible to start a live-donor kidney transplant program with an appropriately trained surgeon and nephrologist, a national program requires a multiskilled team. Recognition and planning for this from the beginning is essential if the transplant program has expectations of meaningful service delivery. It is essential to have active engagement with the regional and national government departments of health to ensure a sustainable program can be maintained. In addition, the procedure should be undertaken at a tertiary referral hospital and the importance of the immediate and long-term care of the donor needs to be stressed. These requirements emphasize the need for oversight by a national authority who has the responsibility for instituting an integrated national plan for the management of ESKD that encompasses all facets of treatment including prevention, dialysis, and transplantation. It has been identified that in Africa, the Middle East, South East Asia, Central Asia, and Oceania, the number of trained personnel is low and enhancing workforce capacity and expertise will be a prerequisite for developing kidney transplantation services.7
Patient engagement and community education
ESKD is a chronic disease and has severe impact on patients, families, and caregivers. Patients and caregivers are best placed to advocate for improved services with governments and health departments. They need to be involved in the setting of local priorities in care delivery, development of infrastructure, setting of research priorities, and expansion of service. Patient involvement can help garner community support for deceased organ donation and promote transparency in the allocation of scarce resources and acceptance of patients onto waiting lists. Closely aligned with this is community engagement and education. The community needs to understand the concepts of brain and circulatory death and the benefits of organ donation as a sign of community solidarity and a benefit to society. In many societies, it would be essential to involve local religious leaders in the development of patient education and awareness programs to help overcome existing major anxieties and fear of organ donation.
Registries
Ultimately, health care delivery, workforce planning, and evaluation of outcomes are essential components of a coordinated national program for ESKD care.10 These require the development of comprehensive and reliable registries. Although these components are prevalent in Australia, New Zealand, Canada, USA, most of Western Europe, and an increasing number of Latin American countries, they are very limited or absent in other parts of the globe. Large portions of the population in Africa, Asia, and parts of Eastern Europe are lacking national registries. Countries such as South Korea, Thailand, and Japan are exceptions. The establishment of a registry requires a national infrastructure but does not need to be government supported and could be a professional initiative. Generic software, such as that developed by the Collaborative Transplant Registry at the University of Heidelberg, is available to interested parties free of charge, provided there is the collective will to implement it.11
Promotion of deceased donation
Deceased donation is difficult to develop in LIC and in many HIC and MIC as well. In addition to the substantial medical infrastructure required, there are social, legal, and religious hurdles that must be overcome. Development of deceased organ donation can be divided into legal requirements, community engagement, and engagement with the medical community.
Development of ethical standards
There are several regional and international instruments that outline the ethical issues and standards surrounding organ donation and transplantation.8,12, 13, 14, 15 The major features are as follows:
Consent for organ donation and transplantation
The legal and ethical requirement for consent for donation and transplantation is an essential mechanism for the protection of donors and transplant recipients.16 In addition to the routine steps involved in obtaining valid consent to surgical and medical interventions, procedural elements designed to safeguard the voluntariness of donation and promote informed decision making may be required for donation and transplantation. These may include specific strategies to identify and address signs of potential coercion or manipulation of potential donors, such as risk factors associated with organ trafficking.
Care of the living kidney donor
As living donors assume significant risks and burdens to help others through transplantation, minimizing those risks and burdens through provision of optimal care is a key responsibility of health professionals. Care begins during the process of screening potential living donors and must continue throughout their lifetimes to address any long-term consequences of donation. Care must be comprehensive of both medical and psychosocial care. There should be an independent and robust process for certification of suitability of the potential living kidney donor to remove the risk of coercion and inappropriate financial incentives.
Trafficking in human organs in all its forms and trafficking in persons for organ removal must be prohibited and criminalized
Consistent with the position of the WHO and the Declaration of Istanbul Custodian Group,17 countries around the world have legally prohibited—and, in many cases, criminalized—organ trafficking and trafficking in persons for organ removal. These practices, in which the human body becomes a source of financial gain, exploit the vulnerable, and cause long-lasting harm to those forced to sell kidneys and to their communities. Trafficking in organs undermines public trust in organ donation and health care systems and jeopardizes efforts to establish sustainable and equitable systems of donation and transplantation.
Financial neutrality of organ donation
Although profiting from organ donation is antithetical to the values of donation and transplantation systems, so too is financial injury to those who donate their organs. The principle of financial neutrality in donation holds that donors should not be left worse off financially as a result of donation and encourages efforts to prevent and cover the costs associated with living donation.18 Addressing costs in this way not only prevents harm to donors and their families but also removes potential financial barriers to donation.
Overarching Objectives
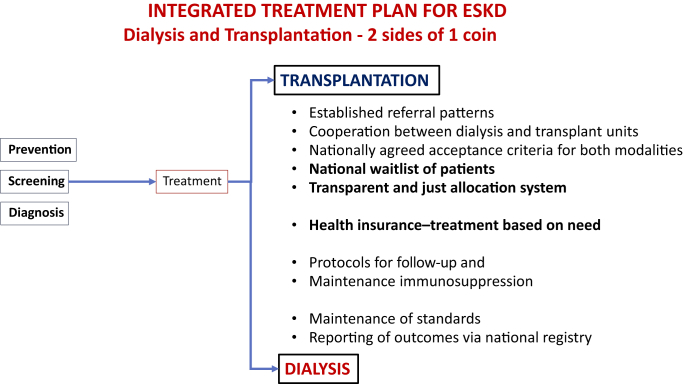
The prime objective is to integrate kidney transplantation services into every national program of ESKD treatment (Figure 3). A policy focused solely on dialysis will be costly and result in patients seeking transplantation in an unregulated environment, creating a market for organ trafficking. For HIC, a realistic national objective is 50% of ESKD treatment delivered by transplantation. At present, only 12 countries have achieved this objective.19 All these countries have national health care schemes and strong deceased kidney donor programs.
Figure 3.
An outline of a management plan for end-stage kidney disease (ESKD) that incorporates both dialysis and transplantation.
Although kidney transplantation has been associated with predominantly HIC, increasingly it is being established in LMIC. In fact, it has been implemented successfully in some of the poorest of countries, provided there is broad commitment from medical practitioners and health authorities.20 The minimum requirement would be the presence of legislation governing organ donation and transplantation, a committed team of health practitioners who have established protocols for donor assessment and follow-up and recipient care and ongoing management. It should be undertaken in the public sector to promote transparency, limit organ trafficking, and provide opportunities for sections of the community to gain access to treatment. Both the International Society of Nephrology (ISN) and The Transplant Society (TTS) have developed programs to promote kidney transplantation within LMIC. The 2 societies have joined together to establish the ISN-TTS Sister Transplant Centers Program (http://stc.theisn.org) to create new kidney transplant centers and develop existing kidney transplant programs in emerging economies. The strength of the program is that it links an emerging program in a resource-low country with an established center that is well resourced.
For LMIC, an objective relative to their level of development and sophistication of their health system needs to be considered. An argument can be made that countries with nascent ESKD programs should aspire to a 100% transplant rate, as time on dialysis will be limited by lack of infrastructure and expense. Hence, most or all patients accepted for dialysis should be transitioned to transplantation. However, current data show that the reverse is true. Nearly all newly established ESKD programs start with dialysis and have no transplantation. In countries with established live-donor programs, a reasonable objective would be that 30% of patients with ESKD be assessed for—and offered the option of—transplantation. An aspirational goal would be that every country has the objective of a minimum of 20% of ESKD treatment being transplantation. For the global nephrological and transplant community, 30% of all patients with ESKD worldwide should be offered transplantation. There is a substantial subset of patients with ESKD who have substantial comorbidity that will contraindicate kidney transplantation. Two important performance indicators would be the proportion of the dialysis population that was evaluated for transplantation and the proportion of patients receiving treatment for ESKD who are managed with transplantation.
Development of strategies to assist countries to achieve these objectives will vary according to the income level of the country and the degree of development of their health care system. Regardless of development status, all countries need to develop a national program in which diagnosis, prevention, pre–end-stage treatment, dialysis, and kidney transplantation form an integrated service. This integrated service needs to be offered to the whole community, not only those who can afford to pay. Hence, factors such as health insurance coverage, cost of immunosuppression, and providing adequate care throughout all regions of the country need to be considered.
It is important to emphasize that all transplant programs must follow the principles of the Declaration of Istanbul and be compliant with the WHO Guiding Principles on Human Cell, Tissue and Organ Transplantation and the Madrid Resolution on Organ Donation and Transplantation.12,14
Possible templates for the development of new or nascent transplant programs are outlined here.
Establish a new transplant program in a country in which transplantation is currently unavailable
This should focus on living related donor (LRD) transplantation in the first instance. Experience has shown that development of a LRD program is easier and more feasible than development of deceased organ donation, which requires more planning, a greater infrastructure, and engagement with the whole community. Successful establishment of a LRD transplant program will help build the necessary capacity to develop deceased donation and provide a springboard to educate the community of the benefits of kidney transplantation. Specific points required to start a LRD transplant program include development of surgical and medical expertise, involvement of other specialties such as infectious disease, HLA laboratory, and engagement with dialysis programs. This can be facilitated by a training partnership with an experienced transplant center within the region or wider transplant community. Once a successful LRD program is established, it can be expanded using strategies such as paired kidney exchange. Ultimately, there will be patients without a suitable LRD, and this will provide pressure to develop deceased organ donation. All countries with successful LRD programs face pressure to develop deceased organ donation. This can be challenging, especially in countries where there are educational, social, and religious barriers to organ donation. Planning for deceased donation should start at the time of the establishment of the LRD program but will take several years to develop. Measuring and reporting outcomes is an important requirement of any transplant program and should be established early in the process.
Established LRD transplant programs that need to develop a deceased donor program
Apart from community education, there are workforce issues surrounding the development of a deceased donor program. There need to be trained donor surgeons who are available around the clock, engagement with ICU/HDU specialists, and training of donor coordinators. Deceased organ donation requires quick turnaround of HLA testing and tissue typing. This will require a national laboratory that is on call. Deceased donor protocols also need to be developed for organ retrieval, equitable organ allocation, organ preservation, evaluation of brain death, and seeking of consent from relatives. All of these require trained staff.
Establishing a network of transplant centers in a country with a single center
Depending on the size of the country it is likely that multiple centers will be needed. Coordinating this at a national level will ensure better use of scarce resources and expertise. Expansion of deceased donation will require engagement of the whole community, and this means that there is equitable access to transplantation, regardless of where they are located.
Using transplantation to enhance the overall capacity of the health care system
Development of transplantation within LMIC has positive spinoffs for the whole health care system. Because of its multidisciplinary nature, it will enhance the capacity of the health care system to deliver complex medical procedures beyond transplantation. It enhances expertise in the medical care of patients with complex cases, the management of immunosuppression, and training of a skilled nursing and allied health workforce. In addition, it leads to improvement in laboratory medicine, pathology, and drug monitoring. All these features enhance the capacity of the health care system and have benefits for other areas of specialized medicine.
Disclosure
Publication of this article was supported by the International Society of Nephrology.
PJOC reports consulting fees from Vitaeris and Commonwealth Serum Laboratories (CSL), Qihan Biotech, and eGenesis; equity ownership/stock options of Qihan Biotech; and grant support from the National Health and Medical Research Council, the Juvenile Diabetes Research Foundation, and CSL. TMC reports consulting or paid advisory board fees from Astellas Pharma and Novartis. RC-DG reports travel support from Drogueria INTI, current grant support from the International Society of Nephrology Sister Renal Center Program and has a grant under negotiation with the International Society of Nephrology Sister Renal Center Program, for Level A. SJD reports grant support from Baxter Health Care (Clinical Evidence Council and Extramural Research Grants). KK-Z reports consulting fees from Abbott, Abbvie, Alexion, Amgen, Astra-Zeneca, Aveo, Chugai, DaVita, Fresenius Medical Care, Genentech, Haymarket Media, Hospira, Kabi, Keryx, Novartis, Pfizer, Relypsa, Resverlogix, Sandoz, Sanofi, Shire, Vifor, UpToDate, and ZS-Pharma; lecture fees from Abbott, Abbvie, Alexion, Amgen, Astra-Zeneca, Aveo, Chugai, DaVita, Fresenius Medical Care, Genentech, Haymarket Media, Hospira, Kabi, Keryx, Novartis, Pfizer, Relypsa, Resverlogix, Sandoz, Sanofi, Shire, Vifor, UpToDate, and ZS-Pharma; grant support from the National Institutes of Health and National Institute of Diabetes and Digestive and Kidney Diseases; and philanthropy grants and divisional and departmental funds; and has served as an expert witness for GranuFlo (Fresenius Medical Care, DaVita). PNH reports grant support from Chiesi Pharmaceuticals. All the other authors declared no competing interests.
Acknowledgments
This manuscript emerged as an individual product of the International Society of Nephrology’s 2nd Global Kidney Health Summit held in Sharjah, United Arab Emirates, in March 2018, and portions of the material in this document have been published in the full report from the Summit (Harris DCH, Davies SJ, Finkelstein FO, et al. Increasing access to integrated ESKD care as part of universal health coverage. Kidney Int. 2019;95:S1–S3321). In addition to the International Society of Nephrology, support of the Summit was provided through unrestricted grants from Baxter and BBraun.
Footnotes
The views expressed in this commentary are solely the responsibility of the authors and they do not necessarily reflect the views, decisions, or policies of the institutions with which they are affiliated.
References
- 1.Tonelli M., Wiebe N., Knoll G. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11:2093–2109. doi: 10.1111/j.1600-6143.2011.03686.x. [DOI] [PubMed] [Google Scholar]
- 2.Wong G., Howard K., Chapman J.R. Comparative survival and economic benefits of deceased donor kidney transplantation and dialysis in people with varying ages and co-morbidities. PLoS One. 2012;7 doi: 10.1371/journal.pone.0029591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Global Observatory on Donation and Transplantation Organ Donation and Transplantation Activities. 2016. http://www.transplant-observatory.org/2016-activity-data/ Available at:
- 4.Muller E. Transplantation in Africa: an overview. Clin Nephrol. 2016;86:90–95. doi: 10.5414/CNP86S125. [DOI] [PubMed] [Google Scholar]
- 5.The Madrid resolution on organ donation and transplantation: national responsibility in meeting the needs of patients, guided by the WHO principles. Transplantation. 2011;91(suppl 11):S29–S31. doi: 10.1097/01.tp.0000399131.74618.a5. [DOI] [PubMed] [Google Scholar]
- 6.Jha V., Martin D.E., Bargman J.M. Ethical issues in dialysis therapy. Lancet. 2017;389:1851–1856. doi: 10.1016/S0140-6736(16)32408-4. [DOI] [PubMed] [Google Scholar]
- 7.Bello A.K., Levin A., Tonelli M. Assessment of global kidney health care status. JAMA. 2017;317:1864–1881. doi: 10.1001/jama.2017.4046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bello A.K., Alrukhaimi M., Ashuntantang G.E. Global overview of health systems oversight and financing for kidney care. Kidney Int Suppl. 2018;8:41–51. doi: 10.1016/j.kisu.2017.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramirez S.P., Hsu S.I., Nandakumar M. Funding ESRD care through charity: the paradigm of the National Kidney Foundation of Singapore. Semin Nephrol. 2001;21:411–418. doi: 10.1053/snep.2001.23776. [DOI] [PubMed] [Google Scholar]
- 10.Gonzalez-Bedat M.C., Rosa-Diez G.J., Fernandez-Cean J.M. National kidney dialysis and transplant registries in Latin America: how to implement and improve them. Rev Panam Salud Publica. 2015;38:254–260. [PubMed] [Google Scholar]
- 11.Opelz G., Dohler B., Ruhenstroth A. The collaborative transplant study registry. Transplant Rev. 2013;27:43–45. doi: 10.1016/j.trre.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization WHO guiding principles on human cell, tissue and organ transplantation. Transplantation. 2010;90:229–233. doi: 10.1097/TP.0b013e3181ec29f0. [DOI] [PubMed] [Google Scholar]
- 13.Chapman J., Delmonico F., Groth C. Commentary: the World Health Assembly resolution on human organ and tissue transplantation. Transplantation. 2010;90:236–237. doi: 10.1097/TP.0b013e3181ebc0ea. [DOI] [PubMed] [Google Scholar]
- 14.Steering Committee of the Istanbul Summit Organ trafficking and transplant tourism and commercialism: the Declaration of Istanbul. Lancet. 2008;372:5–6. doi: 10.1016/S0140-6736(08)60967-8. [DOI] [PubMed] [Google Scholar]
- 15.Council of Europe Convention against trafficking in human organs 2015. Santiago de Compostela, 25.III.2015: Council of Europe Treaty Series-No. 216.
- 16.Martin D.E., Van Assche K., Dominguez-Gil B. Strengthening global efforts to combat organ trafficking and transplant tourism: implications of the 2018 edition of the Declaration of Istanbul. Transplant Direct. 2019;5:e433. doi: 10.1097/TXD.0000000000000872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muller E., Dominguez-Gil B., Martin D. The Declaration of Istanbul on organ trafficking and transplant tourism (2018 Edition) introduction. Transplantation. 2019;103:217. doi: 10.1097/TP.0000000000002541. [DOI] [PubMed] [Google Scholar]
- 18.Delmonico F.L., Martin D., Dominguez-Gil B. Living and deceased organ donation should be financially neutral acts. Am J Transplant. 2015;15:1187–1191. doi: 10.1111/ajt.13232. [DOI] [PubMed] [Google Scholar]
- 19.Robinson B.M., Akizawa T., Jager K.J. Factors affecting outcomes in patients reaching end-stage kidney disease worldwide: differences in access to renal replacement therapy, modality use, and haemodialysis practices. Lancet. 2016;388:294–306. doi: 10.1016/S0140-6736(16)30448-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zafer M.N., Wong G., Aziz T. Living donor risk model for predicting kidney allograft and patient survival in an emerging economy. Nephrology. 2018;23:279–286. doi: 10.1111/nep.12983. [DOI] [PubMed] [Google Scholar]
- 21.Harris D.C.H., Davies S.J., Finkelstein F.O. Increasing access to integrated ESKD care as part of universal health coverage. Kidney Int. 2019;95:S1–S33. doi: 10.1016/j.kint.2018.12.005. [DOI] [PubMed] [Google Scholar]