Abstract
Background:
As previous epidemiological studies in elite ice hockey have focused on acute time-loss injuries, little is known about the burden of overuse injuries and illnesses in ice hockey.
Purpose:
To report the prevalence and burden of all health problems in male professional ice hockey players in Norway during a single competitive season.
Study Design:
Descriptive epidemiological study.
Methods:
A total of 225 male ice hockey players in the GET League (the premier professional league) in Norway reported all health problems (acute injuries, overuse injuries, and illnesses) during the 2017-2018 competitive season. Players reported all injuries and illnesses for 31 weeks using the Oslo Sports Trauma Research Center Questionnaire on Health Problems.
Results:
At any given time, 40% (95% CI, 37%-43%) of players reported symptoms from an injury or illness, and 20% (95% CI, 19%-22%) experienced health problems with a substantial negative impact on training and performance. Acute injuries represented the greatest incidence, prevalence, and burden (defined as the cross-product of severity and incidence). The most burdensome acute injuries were to the head/face, shoulder/clavicle, knee, and ankle. The most burdensome overuse injuries were to the knee, lumbar spine, and hip/groin.
Conclusion:
This registration captured a greater burden from overuse injuries than traditional injury registration, but acute injuries did represent a major problem. These data provide guidance in the development of prevention programs for both acute and overuse injuries, which should focus on the lumbar spine, hip/groin, and knee.
Keywords: overuse injuries, ice hockey, epidemiology, injury prevention, sporting injuries, elite performance
Ice hockey is associated with a high risk of injuries, as players frequently collide with each other as well as with boards, sticks, pucks, and goals. In collegiate and professional men’s leagues, the reported injury rate ranges from 1.1 to 74.3 injuries per 1000 match hours20 and 1.1 to 18.7 injuries per 1000 athletic exposures.1,2,13,14,21,25 This wide variation reflects the methodological differences between studies. Despite these differences, some findings are consistent. First, the injury risk is substantially higher during games than during training.20,21 Second, the most commonly injured body regions are the head,2,14,20,21,25 shoulder,2,14,25 and knee.1,2,14,21 Overall, injury rates in professional ice hockey12,26 seem to be comparable to those in other team sports such as football11,27 and handball.11,27
One limitation of the current ice hockey literature is that a majority of epidemiological studies have used a time-loss injury definition. Although this may be sufficient to capture traumatic injuries, injury definitions based on time loss only capture a small percentage of overuse injuries.4,8 This is because overuse injuries often have a gradual onset, and players commonly continue to participate despite their occurrence.4,6,8 At an elite level, ice hockey players may be particularly prone to overuse injuries because of high training loads and congested match schedules. However, the true burden of overuse injuries, defined as the cross-product of severity and incidence,5,16 is currently unknown. Similarly, little is known about the risk of illnesses in elite ice hockey. In other sports, overuse injuries and illnesses have recently been shown to represent as much of a health burden as acute injuries.7–9
In this study, we aimed to describe the prevalence and burden of all health problems affecting players in the Norwegian men’s premier professional league (GET League). This information can provide guidance when developing injury prevention interventions. To record all acute injuries, overuse injuries, and illnesses, we distributed the Oslo Sports Trauma Research Center Questionnaire on Health Problems (OSTRC-HP)9 once a week to all players throughout the 2017-2018 competitive season.
Methods
Study Design and Participants
This was a prospective cohort study of male ice hockey players in the GET League during the 2017-2018 season. A total of 225 players (mean age, 24 years [range, 17-41 years]) registered all health problems once a week using a smartphone application. The study was approved by the Norwegian Data Protection Authority (No. 17/00803-4/SBO) and reviewed by the South-Eastern Norway Regional Health Authority (2017/1298), and all athletes provided written informed consent to participate in the study.
Recruitment and Inclusion Criteria
The GET League consists of 10 professional teams, each comprising 22 to 25 players. The medical staff consists of a physician, a physical therapist, and for some teams, other health professionals. The principal investigator contacted the teams, their management, and medical staff by email and telephone before the season with information about the study. We informed the players about the study during the annual 1-day preseason testing combine, which all teams attended. We included 9 of the 10 teams; 1 team did not have a medical staff when the season started and could not follow up on data collection during the season. In the 9 teams participating, 5 players declined to participate in the study, 6 players did not download the necessary smartphone application, and 1 player dropped out after reporting for 8 weeks. The final study sample consisted of 225 players.
Injury and Illness Data Collection
Injury and illness data were collected using the OSTRC-HP.8,9 All players were required to download a mobile application (SpartaNova), which automatically distributed the OSTRC-HP once a week (every Sunday) from September 17, 2017 to April 15, 2018 (31 weeks). There were 4 teams (n = 100) that were eliminated in the playoffs and stopped registering after March 11, 3 teams (n = 71) ended their season and stopped registering after March 25, while the 2 finalists (n = 54) completed registration for the entire period. If players failed to complete the questionnaire, the application sent an automated reminder every day until a response was received. Additionally, the principal investigator sent SMS reminders to nonresponders after 3 and 5 days. The medical staff involved in the project could access their team’s health information on a web-based dashboard and encouraged players to respond. To encourage participation, the principal investigator visited 8 of the 9 participating teams during November and December 2017 and maintained regular contact with all players and medical staff throughout the registration period.
Oslo Sports Trauma Research Center Questionnaire on Health Problems (OSTRC-HP)
The OSTRC-HP consists of 4 key questions about the athlete’s participation in sports, training volume, performance, and symptoms of health problems during the past 7 days.8,9 The response to each of the 4 questions is allocated a numeric value between 0 and 25, where 0 represents no problems. The numeric values were summed to calculate a severity score from 0 to 100 for each health problem. If the athlete answered with the minimum value for each of the 4 questions (full participation without problems, no reduction in training or performance, and no symptoms), the questionnaire was completed for that week. If athletes reported a health problem, they were asked to define whether it was an illness or an injury. In case of an injury, they were asked to classify whether it was an acute injury (associated with a specific, clearly identifiable traumatic event) or an overuse injury (no specific identifiable event responsible for its occurrence) and register the affected anatomic area. In case of an illness, they were asked to report their main symptoms (by choosing from multiple predefined symptoms). For all types of health problems, athletes were asked to register the number of days of complete time loss from training and competition (total inability to train or compete) and whether the health problem had been reported previously. They were asked to register all health problems, and in cases of multiple problems during the same week, the questionnaire repeated itself. Finally, they were asked to register the number of training sessions and games played in the previous 7 days.
Definition and Classification of Health Problems
We used an “all complaints” definition, recording all health problems irrespective of the need for medical attention or the consequences on sports participation.17,23,28 Health problems were classified as an injury if they affected the musculoskeletal system or were a concussion, and they were classified as an illness if they affected an organ system or represented generalized symptoms. The definition of an acute injury was an injury/trauma with an acute onset. The definition of an overuse injury was an injury caused by repeated microtrauma without a single, identifiable event responsible for the injury.17 Health problems were defined as “substantial problems” if they caused moderate or severe reductions in training volume, moderate or severe reductions in performance, or a complete inability to participate in ice hockey.8,9 Burden was defined as the cross-product of severity and incidence.5
Prevalence Calculations
Each week, we calculated the following prevalence measures using the methods described by Clarsen et al8: all health problems, substantial health problems, all injuries, substantial injuries, all illnesses, and substantial illnesses. At the end of the study, the mean prevalence and 95% CI were calculated for the entire season.
Incidence and Relative Burden of Acute Injury, Overuse Injury, and Illness
After reviewing each athlete’s questionnaire responses for the entire season, we compiled a list of cases that included the following information: type of health problem, location (for injuries) or main system affected (for illnesses), number of weeks reported, cumulative time-loss days, and cumulative severity score. We also categorized the severity of each case based on its cumulative time loss as slight (0 days), mild (1-7 days), moderate (8-28 days), or severe (>28 days). The incidence of each type of health problem was expressed as the number of cases per player per year (52 weeks).
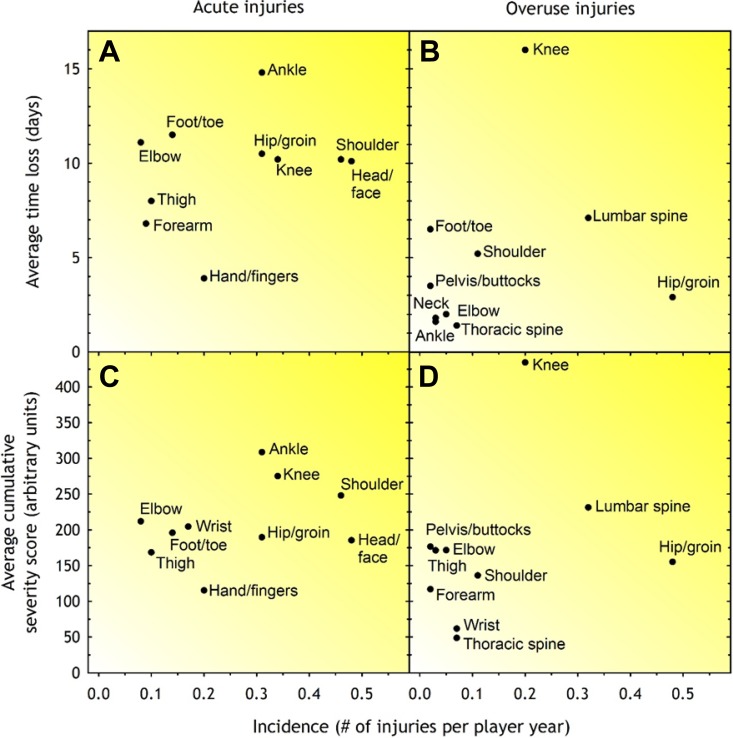
To reflect the relative burden of acute injuries, overuse injuries, and illnesses as a proportion of the total health burden, we summed the severity scores for each health problem type and divided the result by the cumulative severity score for all health problems.5 We also created risk matrices based on the severity and incidence of injuries in the 10 most affected anatomic regions.5 This was performed separately for acute and overuse injuries using 2 measures of severity: (1) the mean number of time-loss days per case and (2) the mean severity score per case.
Results
Response Rate to Weekly Questionnaires
During the 31-week study period, we distributed 6061 questionnaires and received 5353 responses (mean weekly response rate, 88% [range, 80%-98%]). The response rate ranged from 78% to 94% between teams.
Number, Incidence, and Severity of Health Problems
Overall, players reported 323 acute injuries, 152 overuse injuries, and 209 illnesses. This translated to 3.1 new acute injuries, 1.5 new overuse injuries, and 2.0 new illnesses per athlete per year (Table 1). The mean time loss was 39 days per athlete per year (95% CI, 38-41 days): 27 days for acute injuries (95% CI, 26-29 days), 8 days for overuse injuries (95% CI, 7-8 days), and 5 days for illnesses (95% CI, 4-5 days).
Table 1.
Incidence, Total Time Loss, and Cumulative Severity Score of Acute Injuries, Overuse Injuries, and Illnesses
| Incidence, Cases/Athlete/y | Total Time Loss, d | Cumulative Severity Score | |
|---|---|---|---|
| Acute injury (n = 323) | 3.1 | 2783 | 62,235 |
| Overuse injury (n = 152) | 1.5 | 775 | 29,432 |
| Illness (n = 209) | 2.0 | 477 | 14,686 |
| Total (n = 684) | 6.8 | 4035 | 106,353 |
The most frequent acute injury locations were the head/face, shoulder/clavicle, knee, and ankle; the most frequent overuse injury locations were the hip/groin, lumbar spine, and knee. The number and severity of acute injuries, overuse injuries, and illnesses are summarized by region and organ system in Table 2.
Table 2.
Severity of Time Loss of Acute Injuries, Overuse Injuries, and Illnesses by Region and Organ System
| Cases, n | Total Time Loss, d | ||||
|---|---|---|---|---|---|
| Slight (0 d) | Mild (1-7 d) | Moderate (8-28 d) | Severe (>28 d) | ||
| Acute injury | |||||
| Head/face | 15 | 16 | 13 | 4 | 486 |
| Neck | 6 | 5 | 2 | 0 | 40 |
| Chest/ribs | 2 | 4 | 2 | 0 | 32 |
| Thoracic spine | 3 | 2 | 0 | 0 | 5 |
| Shoulder/clavicle | 18 | 14 | 9 | 5 | 470 |
| Upper arm | 2 | 0 | 0 | 0 | 0 |
| Elbow | 4 | 3 | 0 | 1 | 89 |
| Forearm | 4 | 4 | 0 | 1 | 61 |
| Wrist | 6 | 10 | 1 | 0 | 57 |
| Hand/fingers | 13 | 4 | 2 | 1 | 78 |
| Abdomen | 0 | 4 | 0 | 0 | 12 |
| Lumbar spine | 9 | 6 | 2 | 0 | 50 |
| Pelvis/buttocks | 2 | 0 | 0 | 0 | 0 |
| Hip/groin | 11 | 8 | 9 | 3 | 326 |
| Thigh | 3 | 4 | 2 | 1 | 80 |
| Knee | 12 | 11 | 7 | 4 | 347 |
| Lower leg | 1 | 2 | 1 | 0 | 12 |
| Ankle | 10 | 10 | 6 | 5 | 458 |
| Foot/toes | 7 | 2 | 2 | 3 | 161 |
| Overuse injury | |||||
| Head/face | 2 | 1 | 0 | 0 | 2 |
| Neck | 2 | 1 | 0 | 0 | 5 |
| Thoracic spine | 5 | 2 | 0 | 0 | 10 |
| Shoulder/clavicle | 9 | 1 | 0 | 1 | 57 |
| Elbow | 3 | 1 | 1 | 0 | 10 |
| Forearm | 1 | 1 | 0 | 0 | 2 |
| Wrist | 5 | 2 | 0 | 0 | 3 |
| Hand/fingers | 3 | 0 | 0 | 0 | 0 |
| Abdomen | 1 | 0 | 0 | 0 | 0 |
| Lumbar spine | 21 | 7 | 3 | 1 | 227 |
| Pelvis/buttocks | 0 | 2 | 0 | 0 | 7 |
| Hip/groin | 25 | 17 | 5 | 1 | 139 |
| Thigh | 2 | 1 | 0 | 0 | 3 |
| Knee | 9 | 5 | 3 | 3 | 320 |
| Ankle | 2 | 1 | 0 | 0 | 5 |
| Foot/toes | 1 | 0 | 1 | 0 | 13 |
| Illness | |||||
| Respiratory | 98 | 47 | 5 | 1 | 280 |
| Gastrointestinal | 9 | 18 | 0 | 0 | 51 |
| Neurological | 1 | 3 | 0 | 0 | 16 |
| Other illness | 7 | 16 | 3 | 1 | 121 |
| Total | 334 | 235 | 79 | 36 | 4035 |
Prevalence of Health Problems
The mean prevalence of health issues, as well as their range and 95% CI, is summarized in Table 3. We did not identify any trends in prevalence; it remained relatively stable throughout the 31-week registration period.
Table 3.
Weekly Prevalence of All Health Problems and Substantial Health Problems (in Percentages)
| Mean | 95% CI | Range | |
|---|---|---|---|
| All health problems | 40 | 37-43 | 26-55 |
| Injuries | 35 | 33-37 | 25-46 |
| Acute injuries | 21 | 19-23 | 12-34 |
| Overuse injuries | 15 | 14-16 | 9-24 |
| Illnesses | 6 | 5-7 | 2-11 |
| Substantial health problems | 20 | 19-22 | 14-28 |
| Injuries | 18 | 17-19 | 13-24 |
| Acute injuries | 13 | 12-14 | 7-21 |
| Overuse injuries | 6 | 5-6 | 2-11 |
| Illnesses | 3 | 2-3 | 0-6 |
Player Availability
On average, 87% of players were fully available to play during the season (range, 81%-94%), 13% had modified participation (range, 6%-19%), and 7% were unavailable because of health problems (range, 0%-14%).
Burden of Health Problems
Using the total number of time-loss days as the basis for injury severity when calculating relative burden (Table 1), acute injuries represented 69% of the total burden of health problems, with overuse injuries and illnesses representing 19% and 12%, respectively. Using cumulative severity scores as the basis for injury severity, acute injuries represented 59% of the total burden of health problems, with overuse injuries and illnesses accounting for 28% and 14%, respectively.
Figure 1 illustrates the relationship between severity and incidence for the 10 anatomic regions most affected by acute and overuse injuries. The regions representing the highest burden of acute injuries were the head/face, shoulder/clavicle, knee, and ankle. For overuse injuries, the regions representing the highest burden were the knee, lumbar spine, and hip/groin.
Figure 1.
Risk matrix illustrating the relationship between severity (consequence) and incidence (likelihood) of the most commonly reported types of injuries in Norwegian ice hockey (GET League). For each injury in all matrices, the incidence is shown as cases per athlete per year. Shading illustrates the relative importance of each of the injury types; the darker the color, the greater the injury burden, and the greater the priority should be given to prevention. (A, B) A time-loss injury definition is used, and (C, D) an all-complaints injury definition is used.
Discussion
This is the first study to record all injuries and illnesses, including those that did not lead to time loss, in male professional ice hockey players. We used methods designed to capture the full impact of health problems on sports participation and performance, which allowed us to compare the relative burden of acute injuries, overuse injuries, and illnesses in this group.8,9,22 Previous studies using the same methodology in other sports have revealed a “hidden problem” posed by overuse injuries. However, in the current study, we found that irrespective of how we calculated injury severity, acute injuries still clearly represented the greatest burden. Acute injuries accounted for more than twice the burden of overuse injuries and 4 times that of illnesses. Compared with this, previous studies8,9 using the same methodology in other sports have documented that overuse injuries represent a greater relative burden.
In our study, the mean weekly prevalence of health problems reported was 40%; half of this percentage represented a substantial health problem. On average, 7% were unavailable to participate because of health problems, indicating that a significant number of players were playing while injured or sick. Large discrepancies in the definition of an injury, various surveillance techniques, and different methods for calculating incidence and prevalence make comparisons with other ice hockey studies difficult. Compared with other studies using the same methodology in other sports, the prevalence was similar to that observed by Clarsen et al9 (average weekly prevalence of health problems of 36% and of substantial health problems of 15%) and Moseid et al22 (43% and 25%, respectively) but greater than that of Pluim et al24 (21% and 15%, respectively). However, an important difference between these studies is the participation profiles: Clarsen et al9 monitored adult Olympic athletes from mixed sports, Pluim et al24 monitored 11- to 14-year-old elite tennis players, and Moseid et al22 monitored a mixed group of 15- to 16-year-old youth athletes attending sports academy high schools.
We found that the mean weekly prevalence of all acute injuries was 21% and that the mean weekly prevalence of substantial acute injuries was 13%. Our findings suggest that ice hockey teams and organizations should prioritize the prevention of acute injuries. The greatest burden from acute injuries was caused by injuries to the ankle, shoulder/clavicle, head/face, and knee. This is largely consistent with previous epidemiological studies1,2,14,20,21,25 from ice hockey. However, direct comparisons are hampered by differences in anatomic categorization methods between studies. Notably, as illustrated in Figure 1, differences in the injury definition had little effect on the incidence, severity, or burden of acute injuries, as most of these satisfied both an “all complaints” and a “time loss” definition.
Of particular interest may be the large burden represented by acute ankle injuries. Based on information from team medical staff, this can be partly explained by 5 players with “high” ankle sprains involving the anterior tibiofibular ligament, who all took >28 days to return to sport. As ankle flexion is restricted by the hockey skate, this may increase the risk of a “pure” external rotation mechanism, which loads the syndesmosis. A similar pattern has been observed in alpine skiing,15 in which ankle flexion/extension is also restricted by the boot.
Contact between players has been shown to be the most frequent cause of a concussion.10,18 Full or half protection can reduce the severity of head injuries,3 but there is no concluding evidence showing that protective equipment or rule changes can reduce the incidence of concussions. Wennberg30 found significantly fewer collisions of all types in elite hockey games played on international-sized ice surfaces compared with games played on North American–sized rinks, suggesting that playing ice hockey on bigger ice surfaces can reduce the number of acute injuries.
We found that the mean weekly prevalence of overuse injuries was 15%. However, as few overuse injuries affected performance or participation, the prevalence of substantial overuse injuries was only 6%. This rate is lower than in previous studies8,9,22 using the same methodology in other sports. However, it should be noted that the 3 regions most commonly affected by overuse injuries, the lumbar spine, hip/groin, and knee, still represent a burden comparable to the main problem areas for acute injuries. Therefore, ice hockey teams and organizations should also prioritize the prevention of overuse injuries, focusing on these 3 areas, with targeted prevention strengthening programs.29 There have been 2 previous studies13,20 that registered non–time-loss injuries in ice hockey, but as they did not subcategorize into acute and overuse injuries, it is difficult to compare their findings to ours.
The total number of reported illnesses, especially respiratory infections, was comparable to similarly aged Norwegians in the general population.19 However, our findings did not show that symptoms of illnesses had a substantial impact on health, training, or performance. McKay et al21 found 0.7 time-loss illnesses per 1000 athletic exposures in their report from 6 seasons in the National Hockey League, the only previous large-scale study to report on illnesses in ice hockey.
Methodological Considerations
One of the main strengths of the study is the high response rate, although the need for multiple software upgrades may have affected the rates negatively. An additional strength is its full-season duration and relatively large sample size. We also used sensitive injury surveillance methods that capture all health problems.
This study also has several limitations. We did not separate match from training injuries, nor do we have data on exposure. This would have strengthened our data on acute injuries. Additionally, we did not collect data at the beginning of the preseason, so we do not know how many players began the season with lingering injuries or illness. The data were collected from the players, and the extent to which injuries were underreported could not be measured. Conversely, it is also possible that players who are underperforming may have a tendency to report more health problems, but our study was not designed to capture this. The weekly reports by the athletes were subjective, and the reporting threshold may differ between players. However, recall bias and underreporting of health problems could also have affected the results; daily reports could reduce this bias but, on the other hand, challenge the compliance of the participants.
The recording of specific diagnoses has been achieved in previous studies9,24 using similar methods. Every time that an athlete reported a health problem, medical staff/personnel registered a specific diagnosis. This requires close monitoring of reported cases by team medical staff, which was not possible in all clubs in our study. Health-related problems are expected in professional ice hockey. The wide definition used, based on “all complaints,” leads to the registration of minor and transient problems (eg, muscle soreness or unspecific symptoms).8 This is a source of systematic bias, overestimating the prevalence of sports-related health problems. The “substantial health problem” definition (problems leading to reduced performance and/or participation) might be a more appropriate estimate of the impact of injuries and illnesses in ice hockey.
Conclusion
At any given time, 40% of male professional ice hockey players reported symptoms of an injury or illness, and 20% of all players reported health problems that substantially affected their training or performance. We used a surveillance method designed to capture the full extent of all health problems, including illnesses and overuse injuries. Nevertheless, our data showed that acute injuries represented the major health problem. Traditional injury surveillance methods, based on time loss, may therefore be sufficient for the registration of injuries in ice hockey. However, our registration did capture a greater burden from overuse injuries than traditional injury registration methods. These data provide guidance in the development of prevention programs for both acute and overuse injuries, which should focus on the lumbar spine, hip/groin, and knee.
Acknowledgment
The authors thank all the athletes for their participation as well as the clubs and medical staff involved.
Footnotes
Final revision submitted November 26, 2019; accepted December 03, 2019.
One or more of the authors declared the following potential conflict of interest or source of funding: Funding for this project was received from Stiftelsen Fondet til fremme av idrettsmedisin og idrettsfysioterapi i Norge. The Oslo Sports Trauma Research Center has been established at the Norwegian School of Sport Sciences through generous grants from the Royal Norwegian Ministry of Culture, the South-Eastern Norway Regional Health Authority, the International Olympic Committee, the Norwegian Olympic and Paralympic Committee and Confederation of Sports, and Norsk Tipping. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Norwegian Data Protection Authority (No. 17/00803-4/SBO).
References
- 1. Agel J, Dompier TP, Dick R, Marshall SW. Descriptive epidemiology of collegiate men’s ice hockey injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):241–248. [PMC free article] [PubMed] [Google Scholar]
- 2. Agel J, Harvey EJ. A 7-year review of men’s and women’s ice hockey injuries in the NCAA. Can J Surg. 2010;53(5):319–323. [PMC free article] [PubMed] [Google Scholar]
- 3. Asplund C, Bettcher S, Borchers J. Facial protection and head injuries in ice hockey: a systematic review. Br J Sports Med. 2009;43(13):993–999. [DOI] [PubMed] [Google Scholar]
- 4. Bahr R. No injuries, but plenty of pain? On the methodology for recording overuse symptoms in sports. Br J Sports Med. 2009;43(13):966–972. [DOI] [PubMed] [Google Scholar]
- 5. Bahr R, Clarsen B, Ekstrand J. Why we should focus on the burden of injuries and illnesses, not just their incidence. Br J Sports Med. 2018;52(16):1018–1021. [DOI] [PubMed] [Google Scholar]
- 6. Clarsen B, Bahr R. Matching the choice of injury/illness definition to study setting, purpose and design: one size does not fit all! Br J Sports Med. 2014;48(7):510–512. [DOI] [PubMed] [Google Scholar]
- 7. Clarsen B, Bahr R, Heymans MW, et al. The prevalence and impact of overuse injuries in five Norwegian sports: application of a new surveillance method. Scand J Med Sci Sports. 2015;25(3):323–330. [DOI] [PubMed] [Google Scholar]
- 8. Clarsen B, Myklebust G, Bahr R. Development and validation of a new method for the registration of overuse injuries in sports injury epidemiology: the Oslo Sports Trauma Research Centre (OSTRC) overuse injury questionnaire. Br J Sports Med. 2013;47(8):495–502. [DOI] [PubMed] [Google Scholar]
- 9. Clarsen B, Ronsen O, Myklebust G, Florenes TW, Bahr R. The Oslo Sports Trauma Research Center Questionnaire on Health Problems: a new approach to prospective monitoring of illness and injury in elite athletes. Br J Sports Med. 2014;48(9):754–760. [DOI] [PubMed] [Google Scholar]
- 10. Donaldson L, Asbridge M, Cusimano MD. Bodychecking rules and concussion in elite hockey. PLoS One. 2013;8(7):e69122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Engebretsen L, Soligard T, Steffen K, et al. Sports injuries and illnesses during the London Summer Olympic Games 2012. Br J Sports Med. 2013;47(7):407–414. [DOI] [PubMed] [Google Scholar]
- 12. Engebretsen L, Steffen K, Alonso JM, et al. Sports injuries and illnesses during the Winter Olympic Games 2010. Br J Sports Med. 2010;44(11):772–780. [DOI] [PubMed] [Google Scholar]
- 13. Ferrara MS, Schurr KT. Intercollegiate ice hockey injuries: a causal analysis. Clin J Sport Med. 1999;9(1):30–33. [PubMed] [Google Scholar]
- 14. Flik K, Lyman S, Marx RG. American collegiate men’s ice hockey: an analysis of injuries. Am J Sports Med. 2005;33(2):183–187. [DOI] [PubMed] [Google Scholar]
- 15. Fritschy D. [A rare injury of the ankle in competition skiiers]. Schweiz Z Med Traumatol. 1994;1:13–16. [PubMed] [Google Scholar]
- 16. Fuller CW. Injury risk (burden), risk matrices and risk contours in team sports: a review of principles, practices and problems. Sports Med. 2018;48(7):1597–1606. [DOI] [PubMed] [Google Scholar]
- 17. Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Clin J Sport Med. 2006;16(2):97–106. [DOI] [PubMed] [Google Scholar]
- 18. Hutchison MG, Comper P, Meeuwisse WH, Echemendia RJ. A systematic video analysis of National Hockey League (NHL) concussions, part I: who, when, where and what? Br J Sports Med. 2015;49(8):547–551. [DOI] [PubMed] [Google Scholar]
- 19. Institute for Health Metrics and Evaluation. Global Health Data Exchange. Available at: http://www.healthdata.org/. Accessed May 6, 2019.
- 20. Kuzuhara K, Shimamoto H, Mase Y. Ice hockey injuries in a Japanese elite team: a 3-year prospective study. J Athl Train. 2009;44(2):208–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McKay CD, Tufts RJ, Shaffer B, Meeuwisse WH. The epidemiology of professional ice hockey injuries: a prospective report of six NHL seasons. Br J Sports Med. 2014;48(1):57–62. [DOI] [PubMed] [Google Scholar]
- 22. Moseid CH, Myklebust G, Fagerland MW, Clarsen B, Bahr R. The prevalence and severity of health problems in youth elite sports: a 6-month prospective cohort study of 320 athletes. Scand J Med Sci Sports. 2018;28(4):1412–1423. [DOI] [PubMed] [Google Scholar]
- 23. Mountjoy M, Junge A, Alonso JM, et al. Consensus statement on the methodology of injury and illness surveillance in FINA (aquatic sports). Br J Sports Med. 2016;50(10):590–596. [DOI] [PubMed] [Google Scholar]
- 24. Pluim BM, Loeffen FG, Clarsen B, Bahr R, Verhagen EA. A one-season prospective study of injuries and illness in elite junior tennis. Scand J Med Sci Sports. 2016;26(5):564–571. [DOI] [PubMed] [Google Scholar]
- 25. Rishiraj N, Lloyd-Smith R, Lorenz T, Niven B, Michel M. University men’s ice hockey: rates and risk of injuries over 6-years. J Sports Med Phys Fitness. 2009;49(2):159–166. [PubMed] [Google Scholar]
- 26. Soligard T, Steffen K, Palmer-Green D, et al. Sports injuries and illnesses in the Sochi 2014 Olympic Winter Games. Br J Sports Med. 2015;49(7):441–447. [DOI] [PubMed] [Google Scholar]
- 27. Soligard T, Steffen K, Palmer D, et al. Sports injury and illness incidence in the Rio de Janeiro 2016 Olympic Summer Games: a prospective study of 11274 athletes from 207 countries. Br J Sports Med. 2017;51(17):1265–1271. [DOI] [PubMed] [Google Scholar]
- 28. Timpka T, Alonso JM, Jacobsson J, et al. Injury and illness definitions and data collection procedures for use in epidemiological studies in athletics (track and field): consensus statement. Br J Sports Med. 2014;48(7):483–490. [DOI] [PubMed] [Google Scholar]
- 29. Tyler TF, Nicholas SJ, Campbell RJ, McHugh MP. The association of hip strength and flexibility with the incidence of adductor muscle strains in professional ice hockey players. Am J Sports Med. 2001;29(2):124–128. [DOI] [PubMed] [Google Scholar]
- 30. Wennberg R. Collision frequency in elite hockey on North American versus international size rinks. Can J Neurol Sci. 2004;31(3):373–377. [DOI] [PubMed] [Google Scholar]