Abstract
Background
Perioperative patient anxiety in Mohs micrographic surgery (MMS) is associated with increased postoperative pain and decreased satisfaction.
Objective
Determine whether a 3D-printed (3DP) MMS model with standardized education (SE) improves perioperative patient understanding and anxiety.
Methods
An unblinded, randomized controlled trial was conducted, with patients randomized into MMS model plus SE or SE alone groups. Baseline and post-stage understanding and anxiety were evaluated with the Visual Analog Scale (VAS) and State-Trait Anxiety Inventory (STAI). Additionally, patients completed a 6-item knowledge assessment.
Results
Eighty-two patients were enrolled, 42 MMS model and 40 SE group, with similar group mean age, (67.8 years), gender (59.8% male), and previous MMS experience (47.6%). Both groups experienced significant reductions in VAS anxiety and STAI scores and significant increases in VAS understanding. Compared to SE alone, the MMS model group had larger VAS anxiety reduction approaching significance, Δ = −1.31, than SE group, Δ = −.52 (p = .052), 5.59 or 93.25% correct responses vs SE group 5.15 or 85.83% correct response (p<.028).”
Limitations
Overestimations of baseline patient anxiety in our population and 91.1% recruitment of the intended study population limited study power.
Conclusion
A 3DP MMS model with SE may improve patient understanding of MMS and decreases perioperative anxiety.
Keywords: Mohs micrographic surgery, 3D printing, patient anxiety, patient education
Capsule Summary
• Perioperative anxiety in Mohs micrographic surgery (MMS) is associated with poor outcomes and patient dissatisfaction.
• A 3D printed MMS model with standardized education enhanced patient understanding of the procedure and decreased perioperative anxiety. This non-invasive, low-cost strategy may improve patient satisfaction and outcomes in MMS.
Introduction
Performing Mohs micrographic surgery (MMS) under local anesthesia spares patients the risks of general anesthesia but may increase perioperative patient anxiety.1- 3 Factors that may contribute to perioperative patient anxiety include concerns related to skin cancer diagnosis, fear of intraoperative or postoperative pain, procedural complications, and cosmetic result.1-3 Optimizing the patient experience is of utmost importance, as perioperative anxiety in MMS is associated with increased postoperative pain and decreased patient satisfaction.1-2 In this regard, perioperative anxiety is considered a critical component of patient care in MMS, much like pain is often regarded as the sixth vital sign.
In attempts to optimize perioperative anxiety in MMS, pharmacologic and nonpharmacologic interventions have been investigated.4-8 Recently, the use of the peanut butter cup analogy was suggested to improve patient education and decrease anxiety during MMS.9 Analogies remain an important tool in medical education. The 3D-printing technology has enabled the development of widely accessible, fully-customizable models that improve delivery of medical education and learner anxiety.10 The proposed mechanism by which educational models improve anxiety is by decreasing cognitive load associated with the desired material10-11 and thereby making information more understandable to the learner. As verbal counselling is frequently used as the vehicle for delivering medical information, this information can be condensed into a standardized education (SE) protocol and delivered to patients. In our randomized controlled trial, we sought to determine if a 3D-printed (3DP) MMS model in conjunction with a SE protocol was more effective than SE alone in improving patient understanding, presumably by decreasing cognitive load, and thereby serving as a mechanism to reduce perioperative anxiety in MMS.
Methods
Trial Design
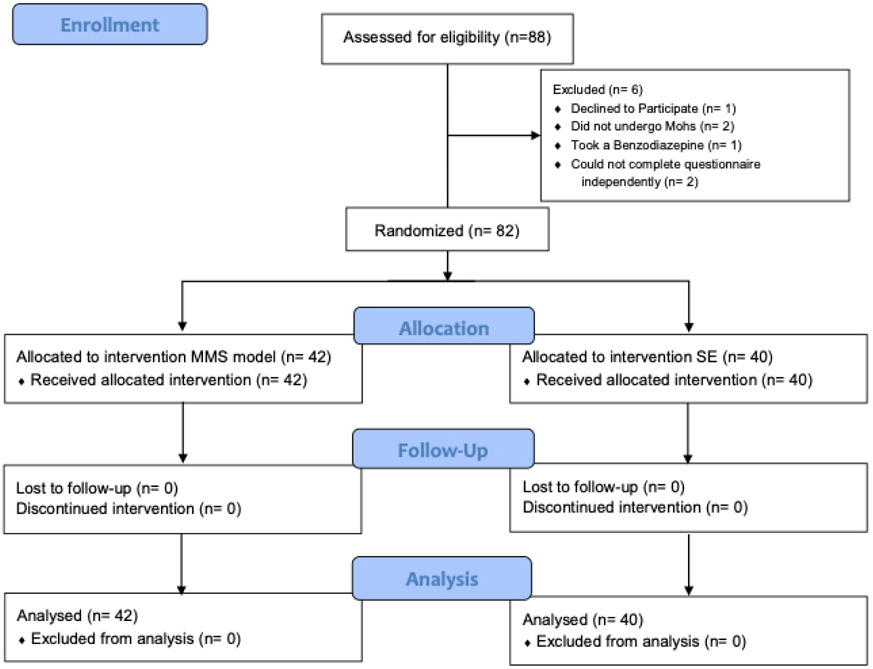
A single-center randomized controlled trial was completed from March 27, 2018 through June 28, 2018 at an outpatient dermatology office affiliated with an urban, academic medical center. A total of 88 patients were assessed for eligibility and randomized 1:1 to the 3D-printed (3DP) MMS model or standardized education (SE) groups. Six patients declined participation or met exclusion criteria prior to baseline testing. Eighty-two patients completed the experimental protocol, 42 in the MMS model group vs 40 in the SE group, and were included in final analysis (Figure 1).
Figure 1:
Participant Recruitment and Randomization
This study received approval by the Case Comprehensive Cancer Center Institutional Review Board, University Hospitals Cleveland Medical Center Institutional Review Board and was registered to clinicaltrials.gov, ID . Informed consent was obtained from patients prior to initiation of the study protocol, and all patient data remained de-identified.
Participants
All patients between the ages of 18-90 and undergoing MMS for removal of non-melanoma skin cancer were eligible. Patients were excluded if they were unable to complete study questionnaires independently, did not undergo MMS, or administered anxiolytic medication during the perioperative period. Patients self-reported age, gender and prior history of MMS. All procedures for were performed by the same female surgeon, M.M., in the University Hospitals Cleveland Medical Center Department of Dermatology.
Interventions
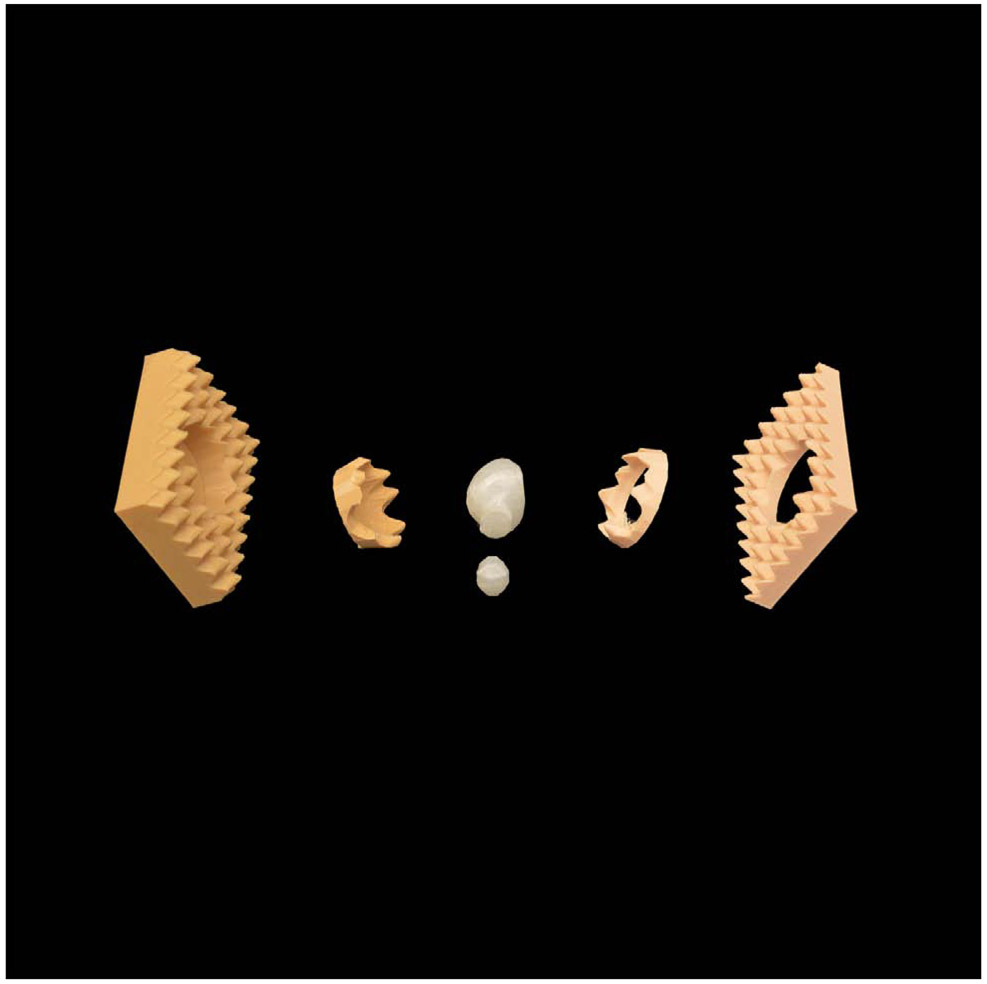
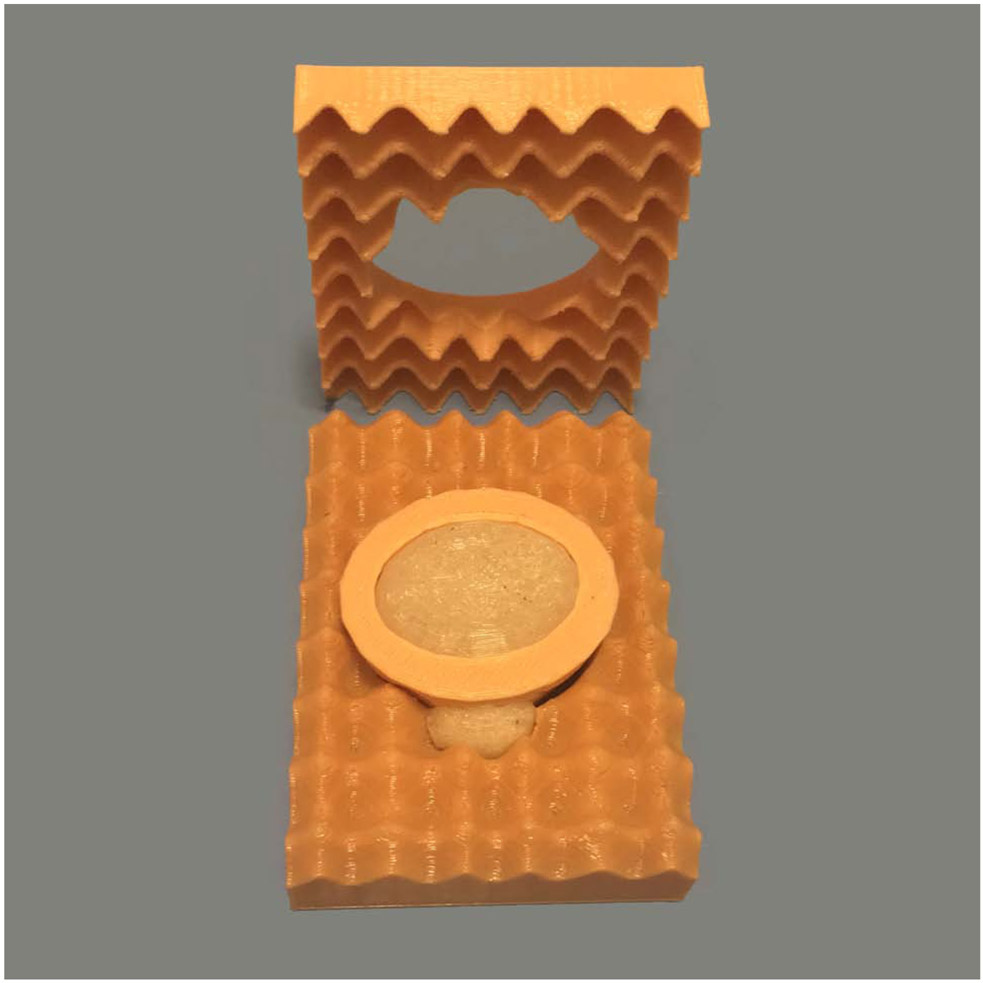
Patients in both groups were educated by a male, M.B., or female, A.H., member of the research team. Participants randomized to the SE group received verbal counselling about MMS from a standardized script written by M.B., under supervision of M.M. Research members were instructed to present information from the script, defer procedural questions to the medical team, and allotted 5 minutes to complete the SE educational protocol. Participants randomized to the MMS model group received verbal counselling about MMS from the SE script with addition of physical demonstration using a 3DP MMS model (Figure 2). This 3DP MMS model contained two skin layers for simplification, a layer of removed tissue, and residual tumor embedded in the bottom layer of skin. The same instructions and constraints for the SE group, were applied to the MMS model group.
Figure 2. 3D printed MMS model expanded view.
(A) Assembly of the 3D printed MMS model shown. Complete 6-piece model costs $4.00 in plastic material and can be printed in ≤ 3 hours. Left) Expanded view of the 6 components used in the model. (B) An overhead view as presented to patient demonstrating tumor extending beyond the surgical margins.
Outcomes
Patients underwent baseline testing prior to assigned intervention, either SE or MMS model, and post-testing following completion of the first MMS stage. The primary outcome was reduction of patient anxiety, which was determined using two well-validated anxiety measures, the Visual Analog Scale (VAS) and State Trait Anxiety Inventory (STAI).4,6,12 The VAS is a 10 cm line, with 11 evenly spaced intervals that ranged from “No Anxiety” to “Extreme Anxiety.” Patient’s marked their anxiety level from-0 to 10 and values between intervals were round to the nearest .5 between values as described in the experimental protocol.
The STAI12 combines two twenty-question assessments; Form Y-1 measuring patient’s state or dynamic anxiety and Form Y-2 measuring patient’s trait or static anxiety. State anxiety inventory items had preassigned values ranging from 1-4, where 1 represented “not at all”, 2 “somewhat”, 3 “moderately so” and 4 “very much so”. Trait anxiety inventory items had preassigned values ranging from 1-4, where 1 represented “almost never”, 2 “sometimes”, 3 “often” and 4 “almost always”. Total scores for each inventory ranged from 20 to 80, with increasing scores associated with higher levels of anxiety. Data for trait anxiety were only collected at baseline, to ensure similar characteristics amongst groups. After consent, patients completed the VAS and both STAI questionnaires and during post-testing patients completed only the VAS and STAI state anxiety questionnaire.
Secondary outcomes included patient understanding and satisfaction. As no standardized measure of patient understanding exists for MMS, subjective and objective measures were used to analyze patient understanding. To assess patient’s perception of their knowledge, a VAS entitled “My Current Comfort Level with My Understanding of the Mohs Procedure” that ranged from “Not at All Comfortable” to “Extremely Comfortable” was completed, with values ranging from 0 – 10 at .5 intervals, similar to VAS anxiety scores. To assess objective knowledge, a 6-item test with multiple choice questions was created by investigators and included information discussed in the standardized script. Patients filled out the VAS assessing understanding at baseline and post-testing and the 6-item test at completion of post-testing. To gauge patient satisfaction, a 3-item Likert scale questionnaire was distributed to patients after completion of the protocol. This scale included questions regarding satisfaction with their explanation of the MMS procedure, if the explanation used could be improved, and if they recommended other patients be provided a similar explanation of MMS.
Sample size
Our sample size, determined prior to initiation of the experiment was 90, with 45 participants in each group. This calculation was based on a previous study,4 in which STAI state mean scores were approximately 38.7 at baseline, assuming that following intervention we would be able to detect a 6-point difference on the STAI state anxiety form between the MMS model and SE group, with a power of 80% and a 5% rate of type I error.
Randomization
Based on a coin-flip randomization, patients who underwent Mohs on Tuesdays were randomized to the MMS model group and Thursdays were randomized to the SE group. Tuesday and Thursday patients were from the same patient pool, presented to the same clinic location, and all procedures were completed by the same surgeon, M.M.
Statistical Analysis
All data analysis was completed in GraphPad Prism 7 and SAS 9.14 software. The association of between categorical variables including patient gender, history of previous MMS, the 6-item knowledge assessment and 3-item Likert satisfaction survey were analyzed using Chi-Square tests. The difference of continuous variables including patients age, baseline and post-test VAS and STAI scores between treatment groups (MMS vs. SE) was examined using T-test and the difference of pre (baseline) and post-test VAS and STAI scores within each treatment group was analyzed using paired T-test after checking normality. Wilcoxon rank-sum test or Wilcoxon signed-rank test was used instead if normality was violated. P-value was not adjusted for multiple tests across different endpoints. All tests were 2-sided and p-value < 0.05 was considered statistically significant.
Results
The mean age of patients enrolled was 67.8 years [SD +/− 12.1 years], 59.8% of the patients enrolled were male, and 52.4% of the patients had not previously undergone MMS. No baseline differences existed between group demographics, anxiety, or subjective understanding, summarized in Table 1. Subgroup analysis completed demonstrated no significant differences existed based on which research team member completed the protocol. The MMS model group had a decreased VAS anxiety scores from 3.00 to 1.7 (Δ = −1.3, p < .0001) and the STAI state anxiety scores from 32.7 to 27.8 (Δ = −4.9, p < .0001), while the SE group had decreased VAS anxiety from 2.5 to 2.0 (Δ = −.5, p < .04) and STAI state anxiety from 33 to 29.7 (Δ = −3.3, p < .03). Larger reductions in anxiety were observed in the MMS model group but only the VAS for anxiety approached statistical significance (p = .052), demonstrated in Figure 3 and Table 2. When subgroup analysis was completed for the VAS for anxiety and STAI, a significant difference was observed for reduction in anxiety in the experimental group across both measures, VAS anxiety from 3.0 to 1.5 (p<.01) and STAI state anxiety from 36 to 29.22 (p<.01), which was not observed in the control group, VAS anxiety from 3.0 to 2.45 and STAI state anxiety from 32.7 to 30.3. Both groups had significant improvements in VAS for understanding scores: 6.17 to 8.63 (Δ = 2.56, p < .0001) for the MMS group and 7.21 to 9.04 (Δ = 1.83, p < .0001) for the SE group. Differences in subjective understanding were not statistically significant between the groups. For the 6-item knowledge assessment, the MMS model group averaged significantly higher scores than the SE group, MMS model 5.59 or 93.25% correct responses vs SE group 5.15 or 85.83% correct response (p<.028). Finally, overall satisfaction was significantly higher on the 3-item Likert scale assessment in the MMS group (p < .03).
Table 1. Patient characteristics in randomized volunteer groups.
There were no significant differences between the control and experimental groups. Parenthetic data represents percentages or standard deviation as shown.
| Characteristic | Control | Experimental | Total | p-value |
|---|---|---|---|---|
| Total Patients | 40 (48.88%) | 42 (51.12%) | 82 | |
| Mean Age (SD) | 67.83 (12.89) | 67.83 (11.34) | 67.83 (12.10) | .92 |
| Patient Gender | ||||
| Male | 25 (62.5%) | 24 (57.14%) | 49 (59.76%) | .62 |
| Female | 15 (37.5%) | 18 (42.86%) | 33 (40.24%) | |
| Number of patients who previously underwent MMS | ||||
| Mohs Experience | 19 (47.5%) | 20 (47.62%) | 39 (47.56%) | .99 |
| No Mohs Experience | 21 (52.5%) | 22 (52.38%) | 43 (52.44%) | |
| Baseline STAI Y-2 “Trait Anxiety” (SD) | 31.1 (8.85) | 29.8 (7.53) | 30.5 (8.28) | 0.65 |
Figure 3. Patient reported Anxiety by Visual Analog Scale (VAS) demonstrated greater improvement in the experimental vs. control group.
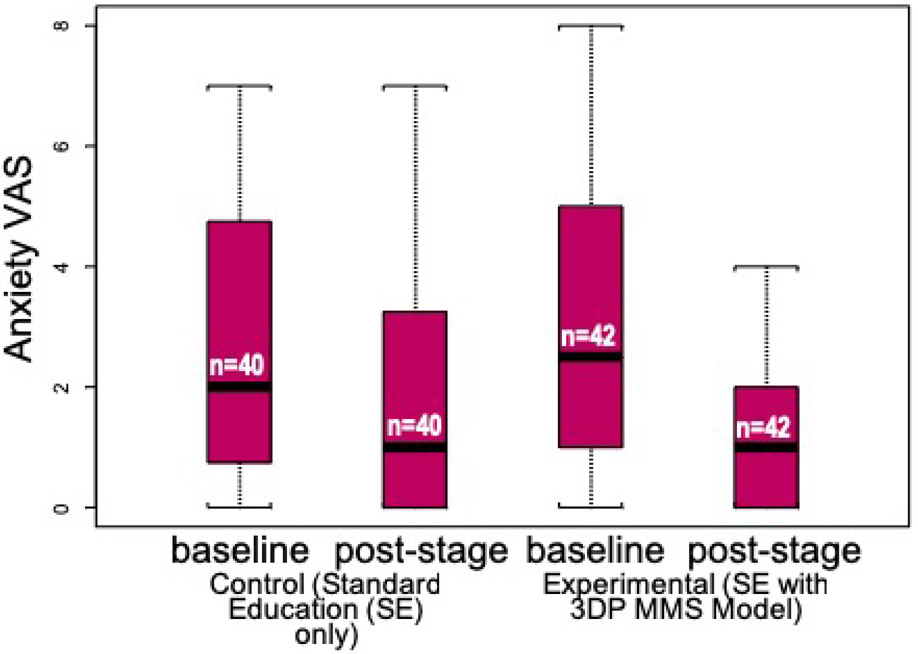
A greater magnitude of improvement was observed for patient volunteers randomized to the group which used a 3DP model during counseling vs. the group randomized to standard of care with handout only as summarized in a boxplot. Bolded black bar = median, red box = 25th to 75th percentiles, brackets encompass entire range and dot-dash whisker line highlights outliers. When comparing the improvement in anxiety (post-stage minus baseline) between experimental and control groups, p=0.052 in a Student’s T-test.
Table 2. Summary of primary and secondary outcomes.
Significant benefit was observed from use of 3DP model regarding anxiety and understanding. Parenthetic data represents standard deviation, or percentages where indicated.
| Outcome | Control | Experimental | p-value |
|---|---|---|---|
| Baseline VAS: Anxiety (SD) | 2.48 (1.99) | 3.00 (2.36) | 0.38 |
| Post-Stage VAS: Anxiety | 1.95 (2.12) | 1.69 (2.03) | 0.61 |
| P-value Compared to baseline | 0.038 | <.0001 | |
| Δ Anxiety VAS (Post-Stage minus Baseline) | −.53 (1.54) | −1.31 (2) | 0.052 |
| Baseline STAI Y-1 “State Anxiety” | 33.0 (10.79) | 32.7 (8.80) | 0.93 |
| Post-Stage STAI Y-1 “State Anxiety” | 29.7 (9.61) | 27.8 (8.16) | 0.54 |
| P-value Compared to baseline | 0.03 | <.0001 | |
| Δ Anxiety “State Anxiety” (Post-Stage minus Baseline) | −3.3 (9.37) | −4.95 (6.95) | 0.352 |
| Baseline VAS: Understanding | 7.21 (2.63) | 6.17 (2.96) | 0.11 |
| Post-Stage VAS: Understanding | 9.04 (1.24) | 8.63 (1.53) | 0.31 |
| P-Value Compared to baseline | <.0001 | <.0001 | |
| Δ Understanding VAS (Post-Stage minus Baseline) | 1.83 (2.34) | 2.46 (2.22) | 0.208 |
| Correct Quiz Responses | 206 (85.83%) | 235 (93.25%) | .007 |
| Incorrect Quiz Responses | 34 (14.17%) | 17 (6.75%) | |
Discussion
Optimal management of perioperative anxiety in MMS remains an increasingly important element of patient care. In our randomized controlled trial, we found that preoperative counseling with a 3DP MMS model, along with standardized verbal counseling, provided patients greater objective understanding of the procedure and was associated with reductions in patient VAS anxiety that approached statistical significance (p = 0.052). Several studies have assessed pharmacologic and non-pharmacologic interventions to alleviate perioperative patient anxiety in MMS. These studies have demonstrated anxiolytic effects of midazolam and personalized patient music in MMS. Ravitskiy et al. found a significant decrease in patient VAS anxiety at 60 minutes following a one-time dose of 10 mg midazolam syrup compared to placebo alone. Although this therapy was effective at 60 minutes, anxiolytic effects of therapy were nonsignificant after 120 minutes.5 Vachiramon et al. found that patients who listened to personalized music during MMS had a significant decrease in VAS anxiety and STAI state anxiety compared to those who did not.4 Compared to our results, these trials had similar patient demographics, including patient age and prior MMS experience. One limitation of both of these studies was that the proposed intervention was compared to placebo or no-intervention alone, whereas our patients were provided the same verbal information during counseling with the standardized script protocol.
Two prior studies have investigated the role of patient education for reduction of anxiety in MMS. Sobanko et al. conducted a trial to determine if a preoperative educational telephone call one week prior to surgery compared to no call would decrease perioperative patient anxiety in MMS and found no difference.6 A limitation may have been that the intervention was too temporally distant from surgery to have the desired anxiolytic effect. Additionally, Hawkins et al. found decreased perioperative anxiety with explanatory video modules in MMS.7 These results must be interpreted with caution, however, as anxiety data were only provided for two of the four total experimental groups and comparison data were unavailable.
A key strength of our trial includes the standardized script protocol used in both groups, thereby allowing us to assess the impact of standardized verbal education alone versus the additional benefit of the 3D MMS model. Other strengths include the use of 2 well-validated markers of patient anxiety, the VAS and STAI, as well as similar baseline characteristics in both groups.4,6,12 Despite these strengths, there are limitations to report. The first is that our trial was powered to detect differences in STAI scores with 45 patients in each group, but the goal enrollee number was not reached. Despite this limitation, we recruited 91.1% of our intended population, 93.3% of the MMS model group and 88.9% of the SE group. Completion of recruitment would unlikely have significantly impacted our primary outcome. Administrative delays, unfortunately, prevented completion of recruitment. Completion of recruitment, may in part explain group differences of .5 points at baseline for VAS for anxiety and 1.0 points for VAS for Understanding points. Similar, small differences, in baseline VAS anxiety have been observed in previous studies and the clinical significance of this is unknown.4 Second, anticipated baseline patient anxiety may be overestimated in our patient population based on previous studies.4 Our power calculation was based on the Vachiramon et al. trial, in which patients had higher baseline STAI anxiety, 38.7 in their experimental group vs. 32.7 in our MMS model group. Possible explanations for decreased anxiety in our study population include increased access to educational resources between diagnosis and MMS, increased awareness of the procedure, or education status of the patient population.
Additional limitations include the lack of a well-validated instrument to measure patient understanding. Our previous pilot data,13 suggested that VAS can be used for evaluating patient perception of their understanding, similar to the VAS for anxiety. In order to compare patient perception of their understanding and objective understanding, we developed a 6-item knowledge assessment to measure patient understanding. Patients did not have statistically significant differences in VAS for understanding, however, the application of this knowledge was significantly greater in the experimental group. This suggests patients educated with a 3DP MMS model have increased short-term understanding of MMS than patients educated with verbal education alone. We hypothesize that the mechanism for this is a reduction in cognitive load, of the provided material. Whether this has an impact on long-term learning, willingness to adhere to recommended follow up skin examinations, or future MMS procedures remains to be investigated.
Conclusion
In conclusion, patient education using a 3DP MMS model along with standardized education preoperatively increases patient understanding and decreases perioperative anxiety, compared to standardized education alone. As preoperative anxiety during MMS has been associated with increased pain and lower patient satisfaction, there is an increasing need to address perioperative anxiety. Here, we propose a low-cost, non-invasive tool, which can be used in combination with other non-invasive treatments, such as music, to decrease perioperative patient anxiety in MMS. Our 3DP MMS model may decrease cognitive load, allowing patients to gain a greater understanding of a complex procedure and improving the counseling experience. Future investigation may address the long-term impact of this useful tool and if similar interventions are applicable to other dermatologic and non-dermatologic procedures.
Acknowledgments
Source of Funding: National Institute of Health, Training Grant T32 AR007569
Abbreviations:
- MMS
Mohs micrographic surgery
- VAS
Visual Analog Scale
- STAI
State-Trait Anxiety Inventory
- 3DP
3D Printed
- SE
Standardized Education
Footnotes
Conflict of Interest: The authors have no conflict of interest to declare. Additionally, this work has not been published or presented previously.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Study Location: University Hospitals Cleveland Medical Center Department of Dermatology
Trial Registration Information: 3D Printed Models in Mohs Micrographic Surgery, , URL: https://clinicaltrials.gov/ct2/show/NCT03461965?cond=3D+print&draw=4&rank=22.
References
- 1.Granot M, Ferber SG. The roles of pain catastrophizing and anxiety in the prediction of postoperative pain intensity: a prospective study. Clin J Pain 2000;21(5):439–45. doi: 10.1111/papr.12060. [DOI] [PubMed] [Google Scholar]
- 2.Chen AF, Landy DC, Kumetz E, Smith G, Weiss E, Saleeby ER. Prediction of postoperative pain after Mohs micrographic surgery with 2 validated pain anxiety scales. Dermatologic Surgery. 2015;41:40–7. doi: 10.1097/DSS.0000000000000224. [DOI] [PubMed] [Google Scholar]
- 3.Kossintseva ICA, Zloty D. Determinants and Timeline of Perioperative Anxiety in Mohs Surgery. Dermatologic Surgery. 2017;43(8):1029–1035.10, 2017. doi: 10.1097/DSS.0000000000001152. [DOI] [PubMed] [Google Scholar]
- 4.Vachiramon V, Sobanko JF, Rattanaumpawan P, Miller CJ. Music Reduces Patient Anxiety During Mohs Surgery: An Open-Label Randomized Controlled Trial. Dermatologic Surgery. 2013;39(2):298–305. doi: 10.1111/dsu.12047. [DOI] [PubMed] [Google Scholar]
- 5.Ravitskiy L, Phillips PK, Roenigk RK, et al. The use of oral midazolam for perioperative anxiolysis of healthy patients undergoing Mohs surgery: conclusions from randomized controlled and prospective studies. Journal of the American Academy Dermatology. 2011;64:310–22. doi: 10.1016/j.jaad.2010.02.038. [DOI] [PubMed] [Google Scholar]
- 6.Sobanko JF, Da Silva D, Chiesa Fuxench ZC, Modi B, Shin TM, Etzkorn JR, et al. Preoperative telephone consultation does not decrease patient anxiety before Mohs micrographic surgery. J Am Acad Dermatol. 2017;76(3):519–526. doi: 10.1016/j.jaad.2016.09.027. [DOI] [PubMed] [Google Scholar]
- 7.Hawkins SD, Koch SB, Williford PM, Feldman SR, Pearce DJ. Web App– and Text Message–Based Patient Education in Mohs Micrographic Surgery—A Randomized Controlled Trial. Dermatol Surg. 2018;44(7):924–932. Doi: 10.1097/DSS.0000000000001489. [DOI] [PubMed] [Google Scholar]
- 8.Alam M, Roongpisuthipong W, Kim NA, Goyal A, Swary JH, et al. Utility of recorded guided imagery and relaxing music in reducing patient pain and anxiety, and surgeon anxiety, during cutaneous surgical procedures: A single-blinded randomized controlled trial. J Am Acad Dermatol. 2016;75(4):585–589. doi: 10.1016/j.jaad.2016.02.1143 [DOI] [PubMed] [Google Scholar]
- 9.Lee E, Wolverton JE, Somani A-K. A Simple, Effective Analogy to Elucidate the Mohs Micrographic Surgery Procedure—The Peanut Butter Cup. JAMA Dermatology. 2017;153(8):743. doi: 10.1001/jamadermatol.2017.0614. [DOI] [PubMed] [Google Scholar]
- 10.Lim KH, Loo ZY, Goldie SJ, Adams JW and McMenamin PG Use of 3D printed models in medical education: A randomized control trial comparing 3D prints versus cadaveric materials for learning external cardiac anatomy. American Association of Anatomists, 2016; 9 (3) 213–221. doi: 10.1002/ase.1573 [DOI] [PubMed] [Google Scholar]
- 11.Leppink J, van den Heuvel A. The evolution of cognitive load theory and its application to medical education. Perspectives on Medical Education. 2015;4(3):119–127. doi: 10.1007/s40037-015-0192-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Speilberger C State-Trait Anxiety Inventory for adults, self evaluation questionnaire STAI form Y-1 and Y-2. Mind Garden: Redwood City; 1977. [Google Scholar]
- 13.Biro M, Mann M, and Popkin D. The use of 3D Printed Models to Optimize Patient Education in Mohs Micrographic Surgery. Poster presented at: 2017 Ohio Dermatological Association Annual Conference; September, 2017; Columbus, Ohio. [Google Scholar]