Abstract
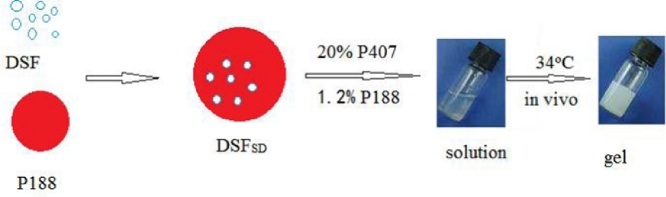
To improve the corneal permeability and water-solubility of disulfiram (DSF), which is an ocular drug for cataract, P188 was selected as a matrix to prepare solid dispersion of DSF (DSFSD) by hot melt method. The DSFSD was characterized by DSC, XRD, and IR, and the results suggested that DSF was amorphous in DSFSD. The DSFSD was added to borate buffer solution (BBS) contained 20% poloxamer P407 and 1.2% poloxamer P188 to form in-situ gel. In vitro and in vivo experiments revealed that DSFSD combined with in-situ gel (DSFSD/in-situ gel) increased the residence time and the amount of DSF penetrated through the corneal. The pharmacodynamics studies exhibited DSFSD/in-situ gel delayed the development of selenium-induced cataract at some content. These results investigated that DSFSD/in-situ gel as a drug delivery system can improve DSF ocular permeability.
Keywords: Disulfiram, Solid dispersion, In-situ gel, Permeability, Anti-cataract
Graphical abstract
Disulfiram solid dispersion was prepared by hot melt method. DSFSD/in-situ gel was also prepared through adjustment of the ratio of P407 to the P188, in-situ gel turned into semisolid at the temperature around eye and then covered the corneal. Which could increase the residence time and the amount of DSF penetrated through the corneal.
1. Introduction
At present, ocular diseases affect around 285 million people whose vision and quality of life were seriously impacted [1], and vision loss posses a chief problem to the aging population worldwide [2]. There are several methods to treat eye diseases. Among them, topical administration is the most popular and acceptable route for the treatment of various eye diseases. However, ocular drug delivery is an enormous challenge because of the various obstacles and protective mechanisms surrounding eyes. For example, blinking, reflex lachrymation, biological barriers and so on [3]. These factors shorten retention time and decrease corneal permeability.
DSF, a prodrug of diethyldithiocarbamate (DDC), had been reported to treat cataract [4], whereas it is poorly water-solubility limited its application. Wang [5] prepared DSF-HP-β-CD inclusion complex to increase the drug solubility in aqueous eye drops and the permeability of DSF into the rabbit eye. Liu [6] prepared octa-arginine modified DSF lipid emulsion to improve its transcorneal capability and treatment effect. Solid dispersion technique is one of popular strategies to improve solubility of poorly water-soluble drug. It has been investigated that solid dispersion can increase ocular [7] and oral bioavailability [8] of disulfiram. In-situ gel is an emergency strategy to prolong the retention time and improving bioavailability in recent years [9].
This study integrated the advantages of in-situ gel and solid dispersion technique to improve the permeability and solubility of DSF. The P407 solution has the temperature thixotropy, which is an ideal material for ocular thermosensitive in-situ gel. Poloxamer 407 and Poloxamer 188 were selected as in-situ gel and solid dispersion matrix, respectively. The physicochemical properties of SD were characterized by DSC, XRD, and IR, the dissolution and corrosion dynamics of in-situ gel were also investigated. Furthermore, in vivo pharmacodynamics and ophthalmic irritation of the in-situ gel were also examined.
2. Materials and methods
2.1. Materials and animals
Disulfiram was purchased from Aladdin (Shanghai, China), poloxamer 407 (P407), poloxamer 188 (P188) (Base, Germany), Sodium selenium (Peking Chemical Works, China). Others reagents were analytical reagent grade.
Eleven-day-old Sprangue-Dawley rat pups (20–25 g) and New Zealand albino rabbits (male, 2.5–3.0 kg) free of any ocular damage were obtained from Shenyang Pharmaceutical University Animal Center (Shenyang, China). All animal studies were conducted in accordance with the Principles of Laboratory Animal Care, and approved by Animal Ethical Committee of Shenyang Pharmaceutical University.
2.2. Preparation of DSF solid dispersion and in-situ gel
The DSF solid dispersion (DSFSD) was prepared by hot melt method, in brief, DSF and poloxamer P188 fine and uniform powder (1:3, 1:5, 1:7, m:m) were heated to 60 °C at vacuum condition in rotary evaporators until melted and changed into the yellowish transparent liquid. Then the liquid was cooled in ice water bath. After that, in-situ gel formulations, 20% poloxamer P407 and 1.2% poloxamer P188 were dissolved in 0.01% BBS of pH 7.4, DSFSD or DSF powder below 50 µm which had been sieved through 300 mesh sieve and benzalkonium chloride were (BKC) added into the solution under stirring, finally, its volume was made up with BBS [10]. In control, DSF suspensions were also prepared. Specifically, DSFSD or DSF powder below 50 µm were uniformly dispersed into 0.01% BBS of pH 7.4 with agitation, after which BKC was added and dissolved by stirring.
2.3. Characterization of solid dispersion
2.3.1. X-ray diffraction (XRD)
The XRD patterns of DSF powder, P188 powder, DSFSD or physical mixture of DSF and P188(1:5, m:m) were measured on a D/max-r A (PANALYII CALB.V, Netherlands) equipped with Cu Kα radiation source at 30 mA and 45 kV and using diffraction angles between 5° and 50°. Aliquots of samples were placed and smoothed evenly over a round cupper disc, which was then placed in the diffractometer for measurement.
2.3.2. Thermal analysis
Differential scanning calorimetry (DSC) curves were obtained using a Mettler DSC 30S (Mettler Toledo, Switzerland). The temperature scale of DSC was calibrated to the melting temperatures of In and Zn, and empty aluminium pans was used as a reference to establish the baseline. About 3 mg of DSF powder, P188 powder, DSFSD (hot melt method) or physical mixture of DSF and P188 (1:5, m:m) were placed in sealed aluminum pan, before heating under a nitrogen flow (50 ml/min) at a heating rate of 10 °C/min from 20 °C to 90 °C.
Thermogravimetric analysis (TGA) was used to determine the amount of water in the samples. The measurement were performed with a TA Instrument Hi-Res TGA 2950 (TA Instruments, New Castle, DE, USA) and data station TA2100. The samples (2–5 mg) were heated in alumina crucible at a temperature range of 50–600 °C with a heating rate of 10 °C/min under nitrogen atmosphere.
2.3.3. Fourier transform infrared spectroscopy analysis (FTIR)
FTIR analysis of DSF powder, P188 powder, DSFSD or physical mixture of DSF and P188 (1:5, m:m) was performed using a FTIR spectrometer (Avatar 360, Nicolet, USA); Data were collected over a spectral region from 400 cm−1 to 4000 cm−1 with a resolution of 4 cm−1.
2.4. In vitro corneal permeation evaluation
Corneal penetration of DSF in-situ gel was investigated using fresh excised rabbit corneal on Franz diffusing cells. The corneal was excised and washed with artificial aqueous humor which consisted of 136.2 mmol/l NaCl, 5.3 mmol/l KCl, 5.5 mmol/l Glucose, 1.7 mmol/l CaCl2 and 1.0 mmol/l K2PO4 in 10 mmol/l HEPES buffer (pH7.4). 2.5 ml 2-[4-(2-Hydroxyethyl)−1-piperazinyl] ethanesulfonic acid HEPES buffer solution was added to reception cell for simulating the condition of eye, while 2 ml sample solution and 0.5 ml simulated tear fluid (STF) (consisted of 2.18 g NaHCO3, 6.78 g NaCl, 0.084 g CaCl2•2H2O, 1.38 g KCl, quantment with 1 L distilled water were added to the donor chamber. The temperature was kept at (34 ± 0.5) °C. 200 µl receptor phase was removed at predetermined time intervals, equal volumes of fresh dissolution medium were replaced, added internal standard solution, centrifugated and conserved in 4 °C. The samples were determined by HPLC and each sample was tested in triplicate.
The cumulative penetration amount of DDC at each interval was calculated as following equations:
where V0 refers to the volume of the receiver cell (2.5 ml); V is the sampling volume (0.25 ml); Cn is the drug concentration in the receiver compartment at scheduled intervals; Ci is the drug concentration in the receiver compartment before determination, A is the effective penetrating region area (0.78 cm2).
The apparent permeability coefficient (Papp) and steady-state flux (Jss) were calculated according to following equations:
where the term ΔQ/Δt represents the slope of the linear plots of cumulative drug permeation amount in the recipient cell; C0 is the initial concentration of drug in the donor cell.
2.5. Dissolution studies
2.5.1. Dissolution of DSFSD in sink condition
The cumulative dissolution release of DSF powder, physical mixture and DSFSD were measured by paddle method according to Chinese pharmacopoeia (2015 edition). 900 ml distilled water with 2% sodium dodecyl sulfate (SDS) was as dissolution medium at (34 ± 0.5) °C with stirring rate 100 rpm. The DSF powder below 50 µm, physical mixture and DSFSD was put into the dissolution vess at the beginning of the study. 2 ml samples were withdrawn and filtered through 0.8 µm and replaced with equal volumes of fresh dissolution medium at 5, 15, 30, 45 and 60 min. The concentration of DSF in each medium was measured by HPLC. Each sample was analyzed in triplicate.
2.5.2. The drug release of DSFSD in STF
The drug release of DSFSD in STF was evaluated in shaker bed with constant-temperature bath. The 0.1% DSFSD sample solution or equivalent amount DSF eye drop was added to STF. The volume ratio of drug solution to STF was 1:7, which could simulate the condition of topical administration. Both of the samples were gently shaking at (34 ± 0.5) °C with 100 rmp. 100 µl samples were withdrawn at 5, 15, 30, 45, 60, 120 and 180 min and filtered through 0.8 µm microspore film. The DSF concentration was assayed by HPLC.
2.5.3. The corrosion of DSF in-situ gel preparations
Membraneless dissolution model was selected for exploring corrosion and dissolution of in-situ gel. 2 g in-situ gel preparations was placed in the preweighted tube and preheated for 10 min at (34 ± 0.5) °C to make the in-situ gel gelatinize. Then, 1 ml STF with the temperature of 34 °C as corrosion medium was injected into the tube which was subsequently shook for 20 min in shaker bed with temperature of (34 ± 0.5) °C. The all free flow medium was poured out and weighed. The new medium was added and repeated the above procedure every 20 min until the remaining of the gel was less than 20%. The concentration of DSF in the medium were assayed by HPLC.
2.6. Precorneal retention time
The samples containing fluorochrome were prepared according to the above procedures of preparing DSFSD/in-situ gel and DSF suspensions except that 30% DSF in original formulation was replaced with Rhodamine B. The in-situ gel and suspensions both contained 300 µg/ml of Rhodamine B. After rabbits were completely narcotized, 10 µl of samples and normal saline were dropped to right eye and left eye, respectively. The anesthetized rabbit was laid into the restraining boxes. Eyes and around area were detected by the In vivo Imaging System (Carestream image station system FX Pro Carestream Health, Inc, USA) equipped with light filters with an excitation wavelength and emission wavelength of 530 nm and 600 nm, respectively. The capturing was performed by the time course of 5, 10, 15, 20 and 30 min after dropping samples into the eye of rabbit [11].
2.7. Stimulating study
2.7.1. Determination of corneal hydration levels
In the test of permeability of drug through the isolated-cornea, only transparent area of isolated-cornea was saved by cutting the around sclera after permeability test, a bit of STF was applied to wash clean corneal, then wiped away apparent moisture and recorded its weight as Wb, then, dried over night under 60 °C with phosphorus pentoxide and recorded its weight as Wa.
The corneal hydration levels (H%) can be calculated by the following equation:
2.7.2. Eye irritation assay
Adult male New Zealand albino rabbits (2.5–3.0 kg) were used to inspect the irritation of preparations. 40 µl in-situ gel was dropped in one eye, meanwhile 40 µl normal saline (NS) was dropped in another eye as a control. Subsequently, eyes were passively closed for 5–10 s. The same administration was taken four times per day in a 7-day period. The irritation was assayed by preparing and examining eyes pathological sections.
2.8. In vivo anti-cataract effect
The Eleven-day-old Sprague-Dawley rat pups were divided into five groups: the blank control (normal saline), cataract model control, DSF suspensions, DSFSD suspensions and DSFSD/in-situ gel groups to research the anti-cataract effect after administration. The test cycle was 7 days, 4 times daily, 24 h after the first administration. During the cycle, the eyeballs of rats were exposed outside the eyelid, and the lenses were observed by slit lamp microscope everyday.
Except blank group, pups of other groups were made to cataract model through received subcutaneous injection with sodium selenium saline solution (19 µmol/kg). To test the development of cataract, 0.5% w/v tropicamide and 2.5% phenylephrine was used to dilate pupils, and then taking slit images every day by using a photo slit lamp microscope (EAS-1000, Nidek, Aichi, Japan) equipped with a CCD camera. The area of lens opacity, expressed as pixels, was analyzed by an image analysis software connected to EAS-1000 then recorded the opacity width (wo) and transparency width (wt) in the microscope, the calculation formula is
3. Results and discussion
3.1. Characterization of solid dispersion
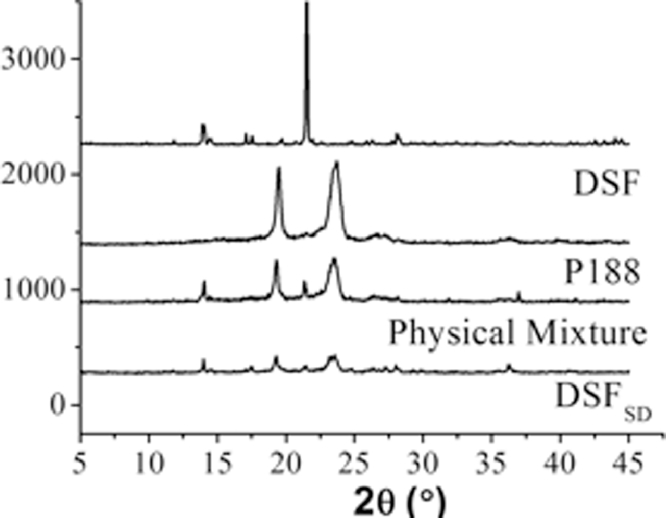
3.1.1. XRD
The XRD patterns for the he DSF, P188 controls as well as the physical mixture and DSFSD were shown in Fig. 1. For pure DSF powder, the diffraction pattern has sharp intensive peaks at around 21.5°, which suggested that it is crystalline in nature; while the P188 are less crystalline in nature, with some broad peaks spaced throughout their diffraction pattern. Comparing the physical mixture and DSFSD demonstrates that the physical mixture and DSFSD have sharp peaks associated with DSF and broad peaks associated with P188, however, the weaker intensity in the physical mixture may be resulted from the dilution effect by P188 compared to pure DSF, and the sharp DSF peaks are of a lower intensity in the DSFSD than those in physical mixture, which would imply that parts of the drug in the DSFSD were microcrystalline structures compared to the physical mixture [8].
Fig. 1.
XRD patterns of DSF, P188, physical mixture and DSFSD.
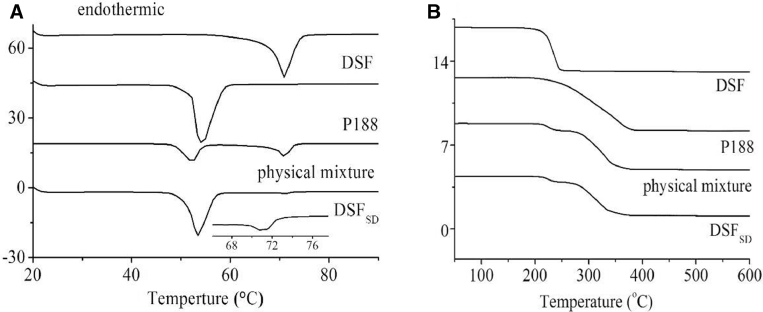
3.1.2. DSC
The DSC profiles of the DSF powder, P188, physical mixture and DSFSD were presented in Fig. 2A. DSF powder has a distinct endothermic peak at about 70.88 °C which was indicated its crystalline state [12]. The thermogram of the physical mixture has a DSF melting peak but weaker peak in the DSFSD thermogram, which corroborates the XRD findings that the DSF in the physical mixture maintained its crystallinity, while fewer DSF in the DSFSD retained some of its crystalline nature. The TGA results of the DSF powder, P188, physical mixture and DSFSD were shown in Fig. 2B. TGA was used to determine the amount of water in the DSFSD because that water content which can also influence the sample thermal transition. There were not obviously weight loss up to 100 °C about the evaporation of volatile materials and moisture in sample. This might be due to the fact that there was no solvents taken part in the preparation process of DSFSD.
Fig. 2.
Thermol analysis of (A) DSC thermograms of DSF, P188, physical mixture and DSFSD; (B) TGA results of DSF, P188, physical mixture and DSFSD.
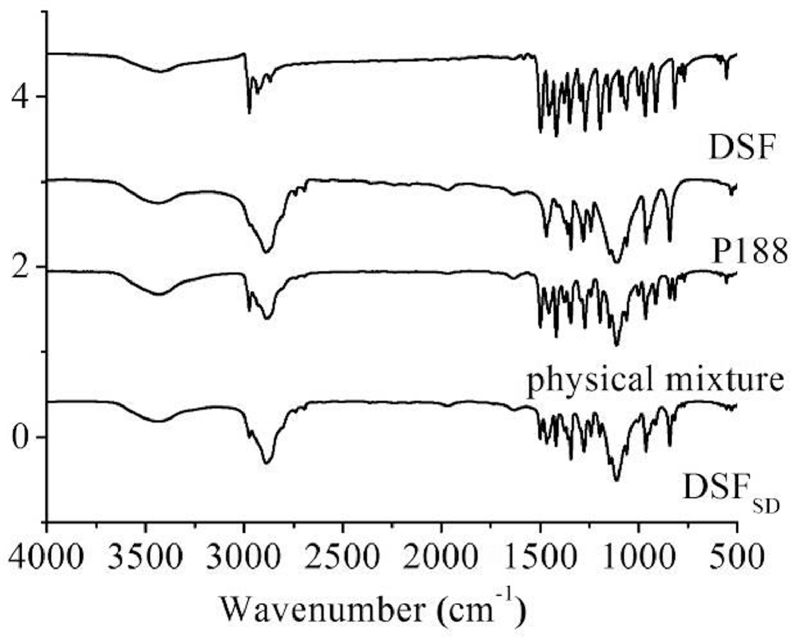
3.1.3. IR
Fig. 3 shows the IR spectra the DSF, P188, physical mixture and DSFSD. The DSF spectrum exhibited characteristic peaks at 2974 cm−1 (C—H stretching vibration band), 1497 cm−1 (N—C = S band), 555 cm−1 (S-S band) and 1273 cm−1 (C-S band). In the IR spectrum of DSFSD, the characteristic bands of C—H were slightly shifted after transformed to DSFSD compared to DSF bulk drug. These changes indicated that there are some molecular interactions, such as hydrogen bond, between DSF and P188 in the formation of DSFSD. However, the fingerprint region of the DSFSD also has all the characteristic peaks for relevant to DSF confirming that its chemical structure did not change during the preparation of the DSFSD and stayed its original chemical form within P188 in the region from 4000 cm−1 to 500 cm−1 .
Fig. 3.
IR spectrograms of DSF, P188, physical mixture and DSFSD.
3.2. Corneal permeability
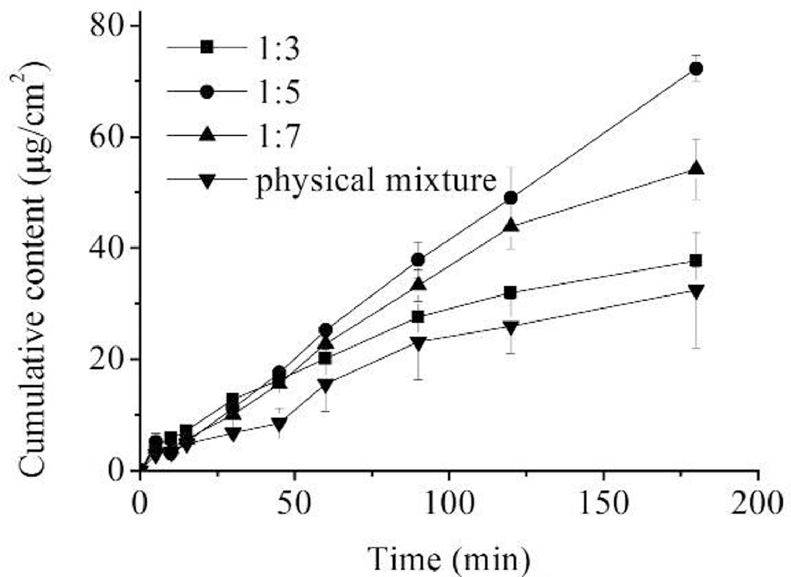
Fig. 4 showed the transcorneal permeation curves of the formulations with different the ratios of DSF to P188, and the corresponding transcorneal penetration parameters are listed in Table 1. As shown, the Papp order of formulations was Papp of formulation 1:5 > Papp of formulation 1:7 > Papp of formulation 1:3 > Papp of DSF, and the highest Papp of 1:5 formulation was 2.31-fold higher than that of DSF eye drops. The complex structure of the corneal might contribute to the results. The corneal has five layers: the epithelium, Bowman layer, substrate layer, Descemet membrane and inner cortex [13]. The formulation needs hydrophilic group to go through the substrate layer, meanwhile, hydrophobic portion is also needed to ensure the drug can across the epithelium and inner cortex. Thus, the ratio of the DSF to P188 plays an important role in transcorneal permeability and DSFSD makes significant contributions to the drug penetrating through the corneal.
Fig. 4.
DDC cumulative amount of formulation 1:3, 1:5, 1:7 and DSF.
Table 1.
In vitro drug transcorneal penetration results of DSFSD with different formulations.
| Samples | Q (µg/cm2) | Papp (cm−2.s−1) | Jss (µg/cm2.s1) |
|---|---|---|---|
| 1:3 | 37.30 | 7.05 × 10−6 | 7.05 × 10−3 |
| 1:5 | 72.27 | 9.40 × 10−6 | 9.40 × 10−3 |
| 1:7 | 54.18 | 8.76 × 10−6 | 8.76 × 10−3 |
| DSF | 31.30 | 5.14 × 10−6 | 5.14 × 10−3 |
3.3. Release of DSFSD
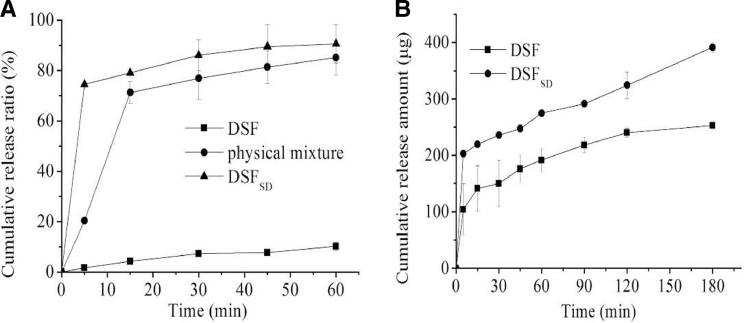
3.3.1. Sink conditions
The results of the release behavior under sink conditions were displayed in Fig. 5A. The 2% SDS aqueous solution was chosen as dissolution medium to get sink condition. The cumulative release from pure DSF powders and physical mixture were, respectively, about 10% and 60% within 1 h. However, the cumulative release from DSFSD was markedly increased up to 90%. The obvious difference among them could be resulted from that the DSF was high-dispersion state in DSFSD and its water solubility was also improved compared with the crystalline state.
Fig. 5.
(A) In vitro cumulative release for the pure drug DSF, physical mixture, DSFSD in sink conditioned release; (B) In vitro cumulative release for the pure drug DSF and DSFSD in STF.
3.3.2. Artificial ophthalmic condition
The investigation was undertaken to reveal whether the SD can improve the dissolution of DSF under artificial ophthalmic condition. As shown in Fig. 5B, the drug cumulative release of DSFSD is 2-fold and 1.5-fold that of DSF powder within 5 min and 30 min, respectively. The results suggested that the SD technique can improve the DSF dissolution under the artificial ophthalmic condition and DSFSD would be used as ophthalmic delivery system to increase the uptake of DSF.
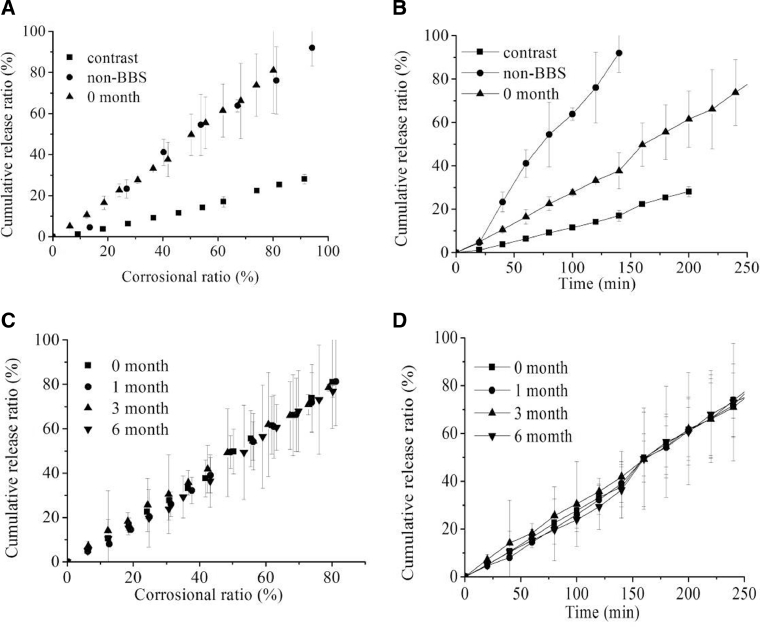
3.3.3. Corrosion dynamics and stability
Fig. 6A and Table 2 showed the cumulative release versus corrosional ratio curves of contrast, DSFSD/in-situ gel with non-BBS and DSFSD/in-situ gel with BBS in 0 month. The curves of the DSFSD/in-situ gel with and without BBS have a slope of about 1 while the slope of the bulk drug release curve is only 0.3, which indicated that the in-situ gel corrosion was the rate-limiting step of drug release of DSFSD/in-situ gel. Additionally, it can be speculated that the drug dispersity was extremely high and the drug loading was uniform in in-situ gel. The drug release of control group that was DSF in-situ gel was affected not only by in-situ gel corrosion but also by DSF dissolution. Fig. 6B showed that the anti-corrosion ability of in-situ gel with BBS is better than the non-BBS group and contrast group. More stronger the anti-corrosion ability, more longer corneal residence time. These results suggested that in-situ gel with BBS may enhance the anti-corrosion ability and extend the corneal retention time of DSF.
Fig. 6.
(A) Corrosional curves and (B) Cumulative release curves of contrast, non-BBS, BBS at initial time; (C) Corrosional stability and (D) Cumulative release stability of DSFSD/in-situ gel in 0, 1, 3, 6 month.
Table 2.
Results of the corrosion test.
| Samples | Time (min) | Corrosional ratio (%) | Cumulative release percent (%) | Slope |
|---|---|---|---|---|
| Contrast | 200 | 91.5 | 28.1 | 0.3316 |
| Non-BBS | 140 | 94.2 | 92.1 | 1.0339 |
| BBS | 260 | 80.1 | 81.0 | 1.0306 |
Fig. 6C and D displayed that the drug release had no obviously change within 6 months. These results suggested that the physical stability of DSFSD/in-situ gel was well.
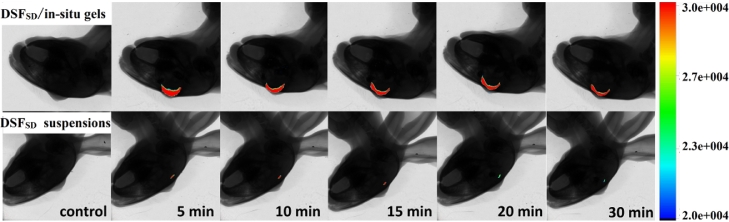
3.4. Precorneal retention study
The fluorescence imaging (shown in Fig. 7) revealed whether in-situ gel can prolong the drug pre-corneal residence time in vivo. Rhodamine B was selected as model drug for that it has fluorescence absorption while DSF has no fluorescence absorption. For the eye drops, fluorescence intensity declined rapidly and almost vanished within 15 min. In case of in-situ gel formulation, fluorescence intensity was prolonged and maintained for 30 min. Suspensions was quickly diluted and removed by lachrymal fluid after instillation, while in-situ gel turned into semisolid at the temperature around eye and then covered the corneal. The study illustrated that in-situ gel can extend the drug residence time and finally might improve therapeutic effect that was certified in the pharmacodynamics study.
Fig. 7.
Fluorescence imaging of Rhodamine B on precorneal at different time of (A) DSFSD in-situ gels group and (B) DSFSD suspensions group.
3.5. Stimulating study
After the test of permeability of drug through the isolated-corneal, the corneal hydration levels of DSFSD/in-situ gel and DSF bulk drug were calculated, they were 78.9 ± 1.7% and 81.7 ± 2.7%, respectively, both were in the normal range of corneal hydration levels 76%−83% [14]. In addition, no inflammation, red swelling or increased tear production were observed during the stimulating study. This result showed that DSFSD exhibited good biocompatibility.
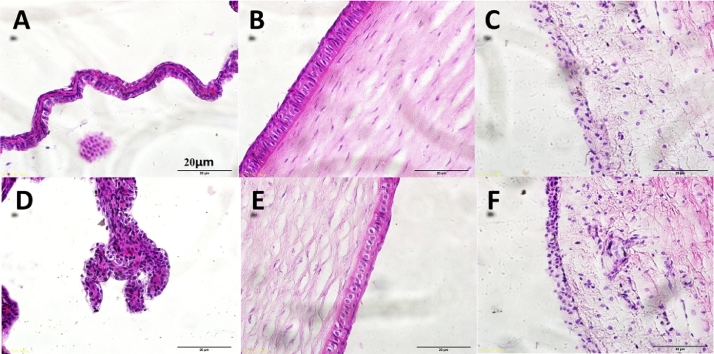
The result of stimulating study was shown in Fig. 8. The three tissues cornea, conjunctiva, and iris histopathological microscope images exhibited that DSFSD/in-situ gel group (D-F) have no obvious difference compared with the control group (A-C), which suggests that topical DSFSD/in-situ gel to rabbit eyes did not produce any ocular toxicity or irritation of the external ocular tissues.
Fig. 8.
Histopathology microscopy of the ocular tissues including the conjunctiva (A and D), the corneal (B and E) and the iris (C and F) after treatment for 7 days, (A–C) normal saline as control, (D–F) DSFSD/ in situ gel.
3.6. Pharmacodynamics study
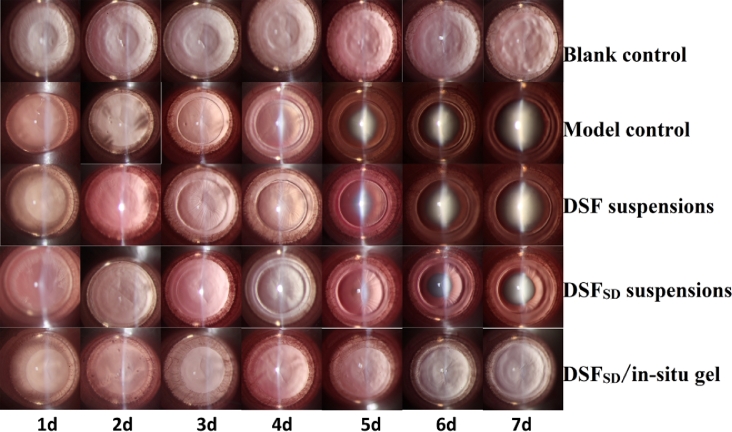
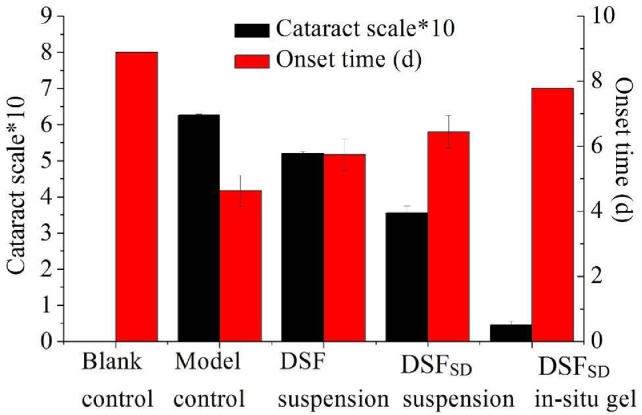
The slit images of the five groups are showed in Fig. 9. DSFSD in-situ gel group, 7 days after administration, lenses of the blank group and DSFSD/in-situ gel group still remained clear, which indicated that the DSFSD/in-situ gel had an effect on inhibiting the formation of selenium cataract. Meanwhile, with regard to the model group the DSF suspensions group had a faster development of cataract between the 4th and the 5th day, and 7 days later, the rats became to be cataract completely. In comparison, DSFSD suspensions had a rapid development of cataract delayed one day and the lens opacity was not as serious as the DSF suspensions group. Concerning the DSFSD/in-situ gel group, no opacity was observed and the lenses remained clear during the 7th day in the experiment. The results of cataract scale which was calculated by the formula shown in Fig. 10 exhibited similar results that the cataract scale of DSFSD/in-situ gel group was weaker than other group. Pharmacodynamics study revealing that DSFSD/in-situ gel had the potency to delay the development of selenium-induced cataract.
Fig. 9.
Imagine of anti-cataract effect in different groups including blank control group, model control group, DSF suspensions group, DSFSD suspensions and DSFSD/in-situ gel group.
Fig. 10.
Calculation cataract scale in different groups including blank control group, model control group, DSF suspension group, DSFSD suspension and DSFSD/in-situ gel group.
4. Conclusion
In this study, the DSFSD in-situ gel was designed as an ocular drug delivery system. In vitro, the in-situ gel exhibited low-irritating properties, and the corneal penetration assessment revealed that it could enhance the transcorneal permeation of DSF. In vivo, the pharmcodynamics study showed anti-cataract effect. From the overall study, it was clarified that the in-situ gel loaded DSFSD represents a potential tool that can improve DSF ophthalmic bioavailability at some extent.
Acknowledgments
Conflict of interest
No conflict of interest exits in the manuscript, and the article is approved by all authors.
Acknowledgments
This work was supported by Liaoning Provincial Key Laboratory of Drug Preparation Design and Evaluation of Liaoning Provincial Education Department (LZ2014045).
Footnotes
Peer review under responsibility of Shenyang Pharmaceutical University.
References
- 1.Delplace V, Payne S, Shoichet M. Delivery strategies for treatment of age-related ocular diseases: From a biological understanding to biomaterial solution. J Control Release. 2015;219:652–668. doi: 10.1016/j.jconrel.2015.09.065. [DOI] [PubMed] [Google Scholar]
- 2.Kim YC, Chiang B, Wu X, Prausnitz MR. Ocular delivery of macromolecules. J Control Release. 2014;190:172–181. doi: 10.1016/j.jconrel.2014.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ludwig A. The use of mucoadhesive polymers in ocular drug delivery. Adv Drug Deliv Rev. 2005;57(11):1595–1639. doi: 10.1016/j.addr.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Ito Y, Cai H, Koizumi Y, Nakao M, Terao M. Correlation between prevention of cataract development by disulfiram and fates of selenium in selenite-treated rats. Curr Eye Res. 1999;18(4):292–299. doi: 10.1076/ceyr.18.4.292.5356. [DOI] [PubMed] [Google Scholar]
- 5.Wang S, Li D, Ito Y. Bioavailability and anticataract effects of a topical ocular drug delivery system containing disulfiram and hydroxypropyl-beta-cyclodextrin on selenite-treated rats. Curr Eye Res. 2004;29(1):51–58. doi: 10.1080/02713680490513209. [DOI] [PubMed] [Google Scholar]
- 6.Liu C, Lan Q, He W. Octa-arginine modified lipid emulsions as a potential ocular delivery system for disulfiram: A study of the corneal permeation, transcorneal mechanism and anti-cataract effect. Colloids Surf B Biointerfaces. 2017;160:305–314. doi: 10.1016/j.colsurfb.2017.08.037. [DOI] [PubMed] [Google Scholar]
- 7.Nabekura T, Ito Y, Cai H, Terao M, Hori R. Preparation and in vivo ocular absorption studies of disulfiram solid dispersion. Biol Pharm Bull. 2000;23(5):616–620. doi: 10.1248/bpb.23.616. [DOI] [PubMed] [Google Scholar]
- 8.Ramadhani N, Shabir M, McConville C. Preparation and characterisation of Kolliphor(R) P 188 and P 237 solid dispersion oral tablets containing the poorly water soluble drug disulfiram. Int J Pharm. 2014;475(1-2):514–522. doi: 10.1016/j.ijpharm.2014.09.013. [DOI] [PubMed] [Google Scholar]
- 9.Morsi N, Ghorab D, Refai H, Teba H. Ketoroloac tromethamine loaded nanodispersion incorporated into thermosensitive in situ gel for prolonged ocular delivery. Int J Pharm. 2016;506(1-2):57–67. doi: 10.1016/j.ijpharm.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 10.Li J, Zhao H, Okeke C I. Comparison of systemic absorption between ofloxacin ophthalmic in situ gels and ofloxacin conventional ophthalmic solutions administration to rabbit eyes by HPLC-MS/MS. Int J Pharm. 2013;450(1-2):104–113. doi: 10.1016/j.ijpharm.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 11.Li J, Liu D, Tan G, Zhao Z, Yang X, Pan W. comparative study on the efficiency of chitosan-N-acetylcysteine, chitosan oligosaccharides or carboxymethyl chitosan surface modified nanostructured lipid carrier for ophthalmic delivery of curcumin. Carbohydr Polym. 2016;146:435–444. doi: 10.1016/j.carbpol.2016.03.079. [DOI] [PubMed] [Google Scholar]
- 12.Shergill M, Patel M, Khan S, Bashir A, McConville C. Development and characterisation of sustained release solid dispersion oral tablets containing the poorly water soluble drug disulfiram. Int J Pharm. 2016;497(1-2):3–11. doi: 10.1016/j.ijpharm.2015.11.029. [DOI] [PubMed] [Google Scholar]
- 13.Waring GO, 3rd, Bourne WM, Edelhauser HF, Kenyon KR. The corneal endothelium. Normal and pathologic structure and function. Ophthalmology. 1982;89(6):531–590. [PubMed] [Google Scholar]
- 14.Schoenwald RD, Huang HS. Corneal penetration behavior of beta-blocking agents I: Physiochemical factors. J Pharm Sci. 1983;72(11):1266–1272. doi: 10.1002/jps.2600721108. [DOI] [PubMed] [Google Scholar]