Abstract
The objective of this study is to design sustained-release tablets using matrix technology, which can well control the release of highly water-soluble drugs with good system robustness and simple preparation process. Taking venlafaxine hydrochloride (VH) as a drug model, the feasibility of using chitosan (CS), carbomer (CBM) combination system to achieve this goal was studied. Formulation and process variables influencing drug release from CS–CBM matrix tablets were investigated. It was found that CS–CBM combination system weakened the potential influence of CS, CBM material properties and gastric emptying time on drug release profile. Demonstrated by direct observation, differential scanning calorimetry (DSC) and Fourier transform infrared spectroscopy (FTIR), in situ self-assembled polyelectrolyte complex (PEC) film was formed on the tablet surface during gastrointestinal tract transition, which contributed to the tunable and robust control of drug release. The sustained drug release behavior was further demonstrated in vivo in Beagle dogs, with level A in vitro and in vivo correlation (IVIVC) established successfully. In conclusion, CS–CBM matrix tablets are promising system to tune and control the release of highly water-soluble drugs with good system robustness.
Keywords: Venlafaxine hydrochloride, Polyelectrolyte complex, Sustained-release, Robustness, Pharmacokinetic
Graphical abstract
Chitosan–carbomer matrix system is beneficial to tune and control drug release with good system robustness. The in vitro release method can be used as a tool for in vivo bioavailability predication, with level A in vitro and in vivo correlation (IVIVC) established successfully.
1. Introduction
At present, the widely studied oral sustained-release tablets are mainly film coated tablets, osmotic pump controlled release tablets and matrix sustained-release tablets. Compared to film coated tablets and osmotic tablets, which have complex preparation process and high equipment requirements, manufacture of matrix sustained-release tablets can be easily scaled up with good robustness. Regarding matrix materials, hydrophilic polymers are frequently used, such as HPMC [1], alginate [2], carbomer [3], and xanthan gum (XG) [4]. However, when a single polymer is used as the matrix, drug release profile might be greatly influenced by the nature of the polymeric material. Therefore, abundant studies are devoted to hydrophilic materials combination system in order to achieve tunable drug release profiles with good robustness. The well-studied combination systems include combined system of nonionic hydrophilic polymers (e.g. HPMC-PVP [5]), nonionic and anionic polymers (e.g. CMC-Na-PEO [6]) and cationic and anionic polymers [7], [8]. Still, how to effectively control the release of highly hydrophilic drug substance by using matrix based drug delivery system is a great challenge.
Our previous study demonstrated that combination of cationic and anionic polymers as the matrix of tablets can form in situ polyelectrolyte complex (PEC) film on tablet surface upon administration, which can decrease matrix erosion rate therefore achieving better control of drug release [9], [10], [11], [12], [13]. Chitosan (CS), a cationic polysaccharide produced by deacetylation of chitin extracted from the external shell of marine crustaceans, has been widely applied as the cationic polymer due to its good safety and biocompatible properties [14], [15]. Amine groups of chitosan are protonated rapidly in acidic media while in water or neutral media, chitosan is practically insoluble without blocking effect [10]. Therefore, combination of chitosan with other anionic polymers is an effective technology to obtain sustained drug release [9], [10], [11]. Carbomer (CBM), an anionic polymer, has many advantages as a candidate of extended-release tablet matrix including a good gel-forming ability and mucoadhesive property [16]. It contains 56%–58% of carboxylic groups with pKa value of 6.0 ± 0.5. The high percentage of carboxylic acid groups allows the polymer to be swellable in a neutral or an alkaline environment. By comparing different anionic polymers, it was noted that chitosan–carbomer physical mixture system had good swelling behavior with weak erosion [9]. Therefore, chitosan–carbomer combination system might have the potential to sustain the release of highly water-soluble drugs for longer time period with tunable release profile and improved system robustness.
Thus, taking highly water-soluble drug, venlafaxine hydrochloride (VH), as a drug model, which is a selective serotonin and norepinephrine reuptake inhibitor (SNRI) for depression treatment [17], this hypothesis was tested. The tablets were prepared by direct compression method by using chitosan–carbomer physical mixture as the matrix. Influence of different formulation and process parameters on drug release profile was investigated. Mechanism for the sustained drug release was elucidated. Moreover, in vitro-in vivo correlation was studied.
2. Materials and methods
2.1. Materials
Venlafaxine hydrochloride (VH) was purchased from Huaxin Pharmaceutical Co., Ltd (Guilin, Guangxi, China); ornidazole was obtained from Jiudian Pharmaceutical Co., Ltd (Changsha, Hunan, China). Chitosan (50 kDa, 100 kDa, 400 kDa) was purchased from Jinan Haidebei Marine Bioengineering Co., Ltd. (China) with a degree of deacetylation of 86.5%; microcrystalline cellulose (Avicel PH-101) was kindly provided as a gift by FMC Biopolymer (Philadelphia, Pennsylvania, USA). Carbomer (Carbopol 971P NF, Carbopol 974P NF, Carbopol 71G) was obtained from the Lubrizol Corporation (Wickliffe, Ohio, USA). Magnesium stearate was kindly provided by Anhui Shanhe Pharmaceutical Excipients Co., Ltd. (Huainan, Anhui, China). All other chemicals were of analytical grade.
2.2. Preparation of matrix tablets
In this study, direct compression method was used to prepare the tablets, which contain the model drug, cationic polymer (CS) and anionic polymer (CBM) as the matrices, microcrystalline cellulose as the filler and magnesium stearate as the lubricant. Briefly, the drug and excipients used were passed through an 80-mesh sieve before mixing. In order to keep the volume and surface area of the tablets constant, the final weight of each tablet was maintained at 310 mg unless otherwise specified. 75 mg drug, the specified amounts of polymers, as indicated in different section, and 10 mg microcrystalline cellulose were blended for 15 min using a pestle and mortar. Afterwards, 0.3% (w/w) magnesium stearate was added and mixed for another 2 min. Tablets were prepared using a single-punch tableting machine (DP30A; Beijing Gylongli Science & Technology Co., Ltd., Beijing, China) equipped with a 10 mm diameter flat-faced punch. Hardness of all the tablets was adjusted to 40–80 N using tablet hardness tester (YPJ-200B; Shanghai Huanghai Instruments Co., Ltd., Shanghai, China).
2.3. In vitro release studies
All drug release tests were carried out using a drug dissolution apparatus (ZRD6-B; Shanghai Huanghai Instruments, Shanghai, China) with the basket method (ChP 2015), rotating at 100 r/min at 37.0 ± 0.5 °C. Unless specially indicated, in vitro release experiments were conducted in simulated gastric fluid (SGF) followed by simulated intestinal fluid (SIF). Specifically, tablets were submerged into 500 ml of 0.1 mol/l HCl solution (SGF, pH 1.2) for 2 h, then the tablets were transferred to 500 ml of phosphate buffer (SIF, PBS, pH 6.8, 0.05 mol/l) for additional 22 h.
This method was used to simulate the situation of a tablet's transit through the gastrointestinal tract [18]. Aliquots of 10 ml were withdrawn at different time intervals (1, 2, 3, 4, 6, 8, 10, 12 and 24 h) and were replaced with equal amounts of fresh release medium. The samples were filtered through a 0.8 mm membrane filter and thereafter analyzed using UV-visible spectrophotometer (UV-2000; UNIC Instrument Corporation, Shanghai, China) at 273 nm.
Drug release studies were carried out in triplicate for each formulation tested and standard deviations were calculated. The difference in dissolution profiles was compared using similarity factor (f2). The similarity factor was calculated using Eq. (1):
| (1) |
where n is the number of time points, Rt is the dissolution value of the reference at time t, and Tt is the dissolution value of the test at time t. The release profiles were significantly different if f2 < 50 [19]. Only one measurement should be considered after 85% dissolution of both the two contrastive formulations.
In addition, the release rate of the drug in the two release media was calculated respectively. The slope of the release curve in 0–2 h was designated as k1.2, and the slope of the followed time points was designated as k6.8.
2.4. Differential scanning calorimetry (DSC)
DSC studies were used to analyze composition of the film formed on the tablet surface, which provided the basis for elucidating the drug release mechanism. Thermal studies were performed using a Mettler Toledo model 30TC 15 equipped with the STARe System (Mettler, Zurich, Switzerland). The samples (2–4 mg) were scanned in sealed aluminum pans under nitrogen atmosphere. DSC thermograms were studied over a temperature range of 25–300 °C at a constant rate of 10 °C/min.
2.5. Fourier transform infrared (FTIR) spectrometry
The infrared absorption spectra of the in situ formed films were analyzed using a FTIR spectrophotometer (IFS-55; Bruker Co., Ltd., Faellanden, Zurich, Switzerland). The tablets were prepared by compressing the samples with potassium bromide. The peak variation of adsorption between 400 and 4000 cm−1 was detected.
2.6. In vivo pharmacokinetic study
Healthy Beagle dogs (15 ± 3 kg) were provided by the Experimental Animal Division of Shenyang Military Region General Hospital and the experiment was carried out in accordance with the Principle of Laboratory Animal Care. Shenyang Pharmaceutical University Animal Ethical Committee approved the protocol for this study. Three Beagle dogs fasted for 12 h before the experiment were used in this study and VH sustained-release tablets were taken with 50 ml water. 5 ml blood samples were withdrawn from femoral vein of anterior limb at different time intervals (1, 2, 4, 6, 8, 10, 12, 16, 24, 36 and 48 h) and were centrifuged at 4000 r/min for 10 min to separate the upper plasma. Plasma samples were treated by protein precipitation and liquid–liquid extraction methods. Briefly, 500 µl plasma samples were placed in a 5 ml Eppendorf tube, and mixed with 100 l of internal standard solution (ornidazole), 200 µl of 1 mol/l NaOH solution and 3 ml of absolute ether. Thereafter, the sample was centrifuged at 10000 r/min for 10 min to isolate the supernatant and transferred in a 5 ml Eppendorf tube. Then, the supernatant was mixed with 200 µl 0.1 mol/l HCl solution and centrifuged at 10000 r/min for 10 min. After removing the organic phase, the water phase was dried in 55 °C water bath under N2 atmosphere and then the residues were dissolved in 100 µl of the mobile phase. The final solution was quantified by HPLC (Agient1100; Agilent Technologies Inc., USA).
The single and double compartment models were fitted to the plasma concentration-time curve of the VH formulation using DAS2.0 experimental pharmacokinetic computer program. And single compartment model can better describe the in vivo pharmacokinetics of the formulation. The formula is as follows (Eq. (2)):
| (2) |
where Fa is in vivo absorption percentage in different time; Ct is the plasma drug concentration at different time points; Ke is the elimination rate constant; AUC(0–t) is area under the curve from 0 to t.
2.7. Statistical analysis
Results were depicted as mean ± SD from at least three measurements. The level of significance was α = 0.05. A P-value < 0.05 was considered statistically significant.
3. Results and discussion
3.1. Effect of CS and CBM in combination on in vitro drug release
First of all, by fixing the amount of polymer (225 mg) in each formulation constant, influence of CS (400 kDa), CBM (974P) and CS–CBM (CS–CBM = 1:1, w/w) physical mixture on in vitro drug release was characterized. As shown in Fig. 1, when CS or CBM was used as the single matrix, sustained drug release could only be maintained for 12 h. Serious burst release was observed in single CBM based tablets, with 42% drug release in 2 h. In the first 4 h, drug release from CS based system was comparable with that from CS–CBM combination system. Thereafter, drug release from CS based system was faster. It was noted that the sustained-release behavior of CS–CBM combination system was prolonged to 24 h. Although CS in SGF and CBM in SIF had strong swelling capacity to form gel, they were insufficient to control the release of highly water-soluble drugs. This study showed that CS and CBM in combination as matrix carrier could surmount the limitation of single polymers. The related sustained-release mechanism will be elucidated in the followed part.
Fig. 1.
Release profiles of VH from CS and CBM single polymer, and CS–CBM physical mixture based matrix tablets in SGF (2 h) followed by SIF.
3.2. Effect of CS molecular weight on in vitro drug release
Polymers with different molecular weight have different gelation degree, which is crucial to drug release because it affects the ability of release medium to pass through the gel layer during swelling process. Therefore, by fixing CS–CBM = 1:1 (w/w) and CBM (974P) type constant, the effect of CS molecular weight (50 kDa, 100 kDa, 400 kDa) on drug release behavior was evaluated. As shown in Fig. 2A, no statistical difference in release profile was found between CS50kDa and CS100kDa groups, however, much slower release was observed in CS400kDa group, especially in the initial first 4 h. To elucidate drug release behavior quantitatively, not only total drug release rate, but also drug release rate in pH 1.2 and pH 6.8 medium was calculated and listed in Table 1. It was found that in pH 1.2 medium, drug release rate from CS400kDa group was significantly lower than that from CS50kDa and CS100kDa groups. This can probably be attributed to the fact that the erosion rate of low molecular weight CS was faster than that of high molecular weight CS under acid condition [10]. However, in pH 6.8 medium, the molecular weight of CS had no significant effect on drug release, indicated by their comparable drug release rate (k6.8). Therefore, taking low burst release into consideration, CS400kDa was selected for the followed studies.
Fig. 2.
Dissolutions profiles of VH from matrix based sustained-release tablets with: (A) different CS molecular weight; (B) different types of CBM; (C) different matrix/drug ratio; (D) different CS–CBM ratio.
Table 1.
Mathematical modeling and drug release kinetics.
| CS (kDa) | CBM | M/D (w/w) | CS–CBM (w/w) | k (%/h) | k1.2 (%/h) | k6.8 (%/h) |
|---|---|---|---|---|---|---|
| 50 | 3.78 | 18.10 | 3.68 | |||
| 100 | 3.84 | 18.31 | 3.96 | |||
| 400 | 3.72 | 14.85 | 3.57 | |||
| 974P | 3.72 | 14.85 | 3.57 | |||
| 971P | 3.68 | 14.68 | 3.80 | |||
| 71G | 3.26 | 15.70 | 2.70 | |||
| 2 | 5.94 | 25.60 | 2.82 | |||
| 5/2 | 5.08 | 18.48 | 3.08 | |||
| 3 | 3.72 | 14.85 | 3.57 | |||
| 4 | 3.16 | 14.95 | 2.29 | |||
| 1:5 | 4.19 | 21.55 | 4.25 | |||
| 1:3 | 4.02 | 21.73 | 3.74 | |||
| 1:2 | 3.38 | 16.02 | 3.21 | |||
| 1:1 | 3.72 | 14.85 | 3.57 | |||
| 2:1 | 4.09 | 15.76 | 4.04 | |||
| 3:1 | 4.04 | 13.45 | 4.46 | |||
| 5:1 | 4.16 | 13.88 | 4.80 |
3.3. Effect of CBM type on in vitro drug release
Polymers with different properties might affect the swelling and erosion behavior of matrix tablets and further change the dissolution path of drugs [20]. CBM is a kind of acrylic cross-linked polymer, which can be divided into different types according to its cross-linking degree and particle size, including CBM 974P, 971P and 71G. CBM 974P is a highly cross-linked powdery polymer. CBM 971P is a slightly cross-linked powdery polymer. CBM 71G has the same structure as that of CBM 971P but it is a granular polymer. Therefore, by fixing CS–CBM = 1:1 (w/w) and CS molecular weight 400 kDa constant, the effect of CBM type (974P, 971P and 71G) on drug release behavior was evaluated. Fig. 2B showed that no statistical difference in drug release was found in CBM 974P, 971P based system in the investigated 24 h (f2 = 90), with cumulative release rate of 88% and 90% after 24 h, respectively. Similarly, as shown in Table 1, there was no significant difference in k1.2 (%/h) and k6.8 (%/h) values between the 974P and 971P groups (P > 0.05). Thus, when using CS–CBM physical mixture as tablet matrices, the release difference of highly cross-linked 974P and slightly cross-linked 971P disappeared. It was noted that CBM type has no influence on drug burst release in the first 2 h. However, compared to CBM 974P and 971P group, slower drug release was observed from CBM 71G based system from 4 h on with incomplete drug release after 24 h (P < 0.05). Similarly, drug release rate k6.8 (%/h) from 71G was significantly lower than that of 971P and 974P system (Table 1). This can be explained by the fact that, compared with powdery CBM 974P and 971P, the granular CBM 71G could better maintain integrity of the matrix and thus prolong drug release [3]. Taking complete drug release at 24 h into consideration, CBM 974P was selected for the followed studies.
3.4. Effect of matrix/drug ratio on in vitro drug release
In hydrophilic matrix tablets, the amount of drug and matrix in the tablet may affect release of the drug [21]. Therefore, by fixing CS (400 kDa)/CBM (974P) = 1:1 (w/w), influence of matrix drug ratio on drug release profile was investigated at matrix/drug (M/D) = 2:1, 2.5:1, 3:1 and 4:1, w/w respectively. As shown in Fig. 2C, the amount of CS–CBM used in the matrix had a significant effect on drug release characteristics. When the matrix drug ratio increased from 2:1 to 2.5:1, the release was significantly retarded (f2 = 39 < 50). However, further increasing matrix/drug ratio from 2.5:1 to 3:1, no significant difference in release profile was found (f2 = 58 > 50). Especially, for M/D = 3:1 or 4:1 formulations, the dissolution curves were almost coincident (f2 = 94 > 50), with low burst release. Considering the principle of minimizing tablet weight under the same sustained-release condition, M/D = 3:1 was identified for the follow-up study.
3.5. Effect of CS–CBM ratio on in vitro drug release
By keeping matrix/drug (M/D) at 3:1, influence of CS (400 kDa)–CBM (974P) ratio on drug release profile was investigated from 1:5 to 5:1. As shown in Fig. 2D, tunable VH release can be achieved by changing CS (400 kDa)–CBM (974P) ratio. When CS–CBM ratio was at 1:5 or 1:3, VH was released faster from the matrix, with high burst release (43% released in 2 h). Significantly retarded drug release was observed at CS–CBM ratio 1:2 and 1:1, but with incomplete drug release at 24 h. In contrast, as shown in Fig. 2D and Table 1, increasing the ratio of CS in the matrix could not only decrease burst release in SGF, indicated by the decreased k1.2 (%/h), but also increase drug release rate k6.8 (%/h) in SIF, and complete drug release at 24 h was observed for CS–CBM ratio 3:1 and 5:1 formulations.
It was noted that when CS–CBM ratio changed from 1:5 to 3:1, k1.2 (%/h) reduced from 21.55%/h to 13.88%/h in the first 2 h. This can probably be attributed by the gelling property of CS, therefore leading to more sustained drug release; while the value of k6.8 (%/h) decreased from CS–CBM ratio 1:5 to 1:2 and then increased from the ratio of 1:2 to 5:1. This phenomenon can be explained by the fact that, when CS–CBM ratio increased from 1:5 to 1:2, more ionized CBM could form PEC with ionized CS based on electrostatic interaction, leading to better control of drug release. However, further increasing CS–CBM ratio from 1:2 to 5:1, the ratio of nonionized CS may increase in SGF. Since CS has limited solubility in SIF, instead, it may lead to tablet disintegration at higher ratio [22], which explained the increased k6.8 (%/h) value at higher CS–CBM ratio 5:1.
Based on the present study, it seems that CS–CBM ratio in the range of 3:1–5:1 is quite effective in decreasing the burst release of VH and brings complete drug release at the later stage from the matrix based tablets. Therefore, by adjusting the ratio of CS–CBM, various release rates of highly soluble VH could be achieved, indicating that CS–CBM matrix system could be used to obtain tunable drug release profiles.
3.6. Formation of in situ self-assembled PEC film
It was noted that drug release from different ratio of CS–CBM system was significantly different from that of single CS and CBM system (Fig. 1), implying a novel drug release mechanism might be involved.
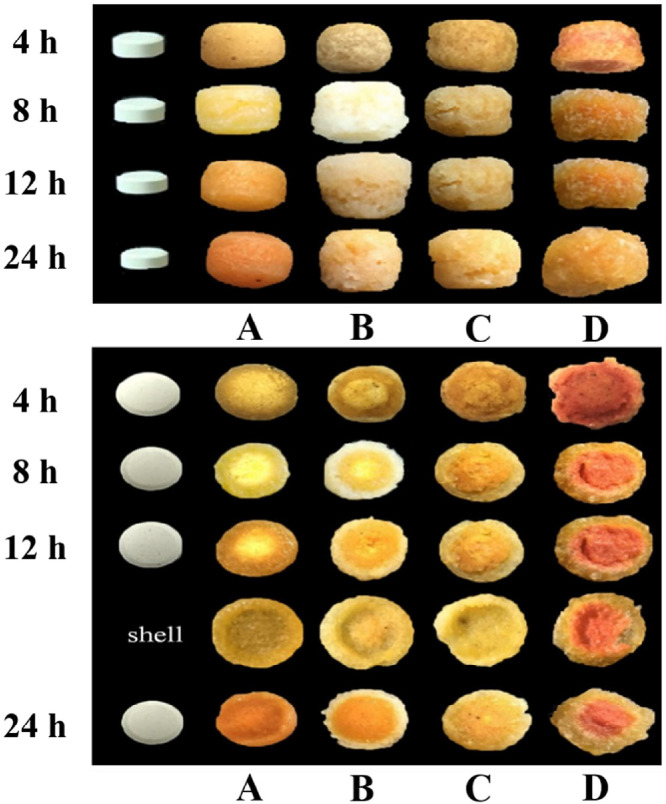
To elucidate this phenomenon, first of all, by adding 5% methyl orange in the tablets as indicator, influence of CS–CBM ratio (5:1, 3:1, 1:1, 1:3) on surface and cross section morphology change of the tablets during dissolution were taken for direct observation. It was noted that a film was formed on tablet surface within 4 h and smoothness of the film was CS–CBM ratio dependent (Fig. 3). Cross section photographs further demonstrated the formation of obvious core-shell structure during release process. And the formed shell can be easily separated from the internal core (Fig. 3 shell). When CS–CBM ratio was 5:1, the film was relatively smooth. In contrast, when CS–CBM ratio was 3:1, more pores were observed on the film, while for CS–CBM ratio 1:1 tablets, additional cracks were found on the rough surface. Especially, when CS–CBM was 1:3, the film was close to gel state, therefore limiting retarding effect for drug release. These results are in good agreement with the drug release profiles presented in Fig. 2D.
Fig. 3.
The surface and the cross section photographs of the tablets: (A) CS–CBM = 5:1; (B) CS–CBM = 3:1; (C) CS–CBM = 1:1; (D) CS–CBM = 1:3; shell: the formed film after 12 h.
According to our preliminary studies [10], [11], [12], [23], film was formed on the surface of tablets in gastrointestinal environment and originated from polyelectrolyte complex (PEC) film formation contributed to the chitosan–anionic polymers electrostatic interaction. Based on the structure properties of CS and CBM, it was assumed that polyelectrolyte complex (PEC) film might be formed on the tablet surface, which promoted better control of drug release. To demonstrate this point, the composition and physicochemical properties of the shell were further characterized by DSC and FTIR, and compared with that of CS, CBM and CS–CBM physical mixture.
As shown in Fig. 4, DSC studies indicated that CS (Fig. 4A) showed an exothermic peak at 280 °C due to its degradation and CBM (Fig. 4B) showed an endothermic degradation peak beginning at 200 °C [24]. Physical mixtures of CS–CBM (Fig. 4C) showed the exothermic peak of CS at 280 °C and the degradation peak of CBM at 200 °C, indicating that there was no interaction between CS and CBM in their physical mixture. In contrast, the characteristic peaks of CS and CBM disappeared in the thermogram of the tablet shell (outer layer, Fig. 4D), indicating the formation of new substance. This might suggest that the table shell originated from the chitosan–carbomer PEC, which was formed by electrostatic interaction between CS and CBM [23].
Fig. 4.
DSC curves of (A) CS, (B) CBM; (C) the physical mixture of CS–CBM at ratio 1:1, (D) the outer layer film of CS–CBM based tablets with CS–CBM ratio 1:1.
In addition to DSC, FTIR was used to analyze the shell structure. In the spectrum of CS (Fig. 5A), the band situated at 1639 cm−1 was assigned to the õ (C = O) of the amide group (amide I band) presented in the acetylated units of CS. In the spectrum of CBM (Fig. 5B), the band at 1713 cm−1 was due to C = O stretching vibration of carboxylic groups [25]. No apparent new peak was obtained from the spectrum of CS and CBM physical mixture (Fig. 5C). However, compared to the physical mixture, a new characteristic peak at 1610 cm−1 was observed in the outer layer film sample, and other characteristic peaks became weaker or even disappeared in the spectrum (Fig. 5D), indicating that NH3+ in CS structure was cross-linked with COO− in CBM chain [26].
Fig. 5.
FTIR spectra of (A) CS, (B) CBM; (C) the physical mixture of CS–CBM at ratio 1:1; (D) the outer layer film of CS–CBM based tablets with CS–CBM at ratio 1:1.
Based on the above results, it was demonstrated that PEC film was indeed formed on the tablet surface during the transition in gastrointestinal tract. In SGF, the amino group of CS chain on tablet surface was fully protonated to form NH3+ since the pKa of CS is 6.5 [14]. After being transferred into SIF, CBM began to hydrate and dissociate to form COO− and large amount of protonated CS still existed. Electrostatic reaction occurred between COO− and NH3+ and in situ self-assemble PEC film was formed [10], [27]. Therefore, drug release from CS–CBM system was regulated via combined action of in situ formed polyelectrolyte complex film coating and internal hydrophilic gel system, which was consistent with former studies [10].
3.7. Effect of dissolution media pH on in vitro drug release
Since PEC film can only be formed under gastrointestinal transition, to further demonstrate that the formed PEC film played an important role in regulating drug release, influence of in vitro release medium pH on drug release from CS–CBM matrix (CS (400 kDa): CBM (974P): VH = 5:1:2, w:w:w) based tablets were investigated. As shown in Fig. 6A, despite the fact that VH is a highly water-soluble drug with pH-independent solubility, the release profiles of VH from the three studied media (i.e., SGF, SIF and SGF followed by SIF) were varied after 4 h, which was regarded as the starting point for PEC formation [10]. The fastest drug release was found in SGF, followed by SIF and the sustained drug release up to 24 h can only be achieved in SGF followed by SIF system, indicating that the self-assemble PEC film formed in SGF followed by SIF after 4 h could slow drug release.
Fig. 6.
Influence of (A) pH variation; (B) the contact time with SGF on drug release from VH extended release tablets based on CS–CBM = 5:1.
3.8. Effect of gastric fluid contact time on in vitro drug release
The above study indicated that PEC film can only be formed during gastrointestinal tract transition. Therefore, it was assumed that the contact time between matrix tablets and gastric fluid might affect the ionization degree of CS, further influencing the PEC film formation and its permeability. Thus, influence of gastric fluid contact time on drug release from CS–CBM matrix (CS (400 kDa): CBM (974P): VH = 5:1:2, w:w:w) based tablets was investigated in SGF (0.5 h, 1 h, 2 h) followed by SIF (23.5 h, 23 h, 22 h) conditions. As shown in Fig. 6B and Table 2, tablet contact time with gastric fluid had no statistical influence on k6.8 (%/h), similarly, no significant difference in drug release profile was found (f2 > 50). This study indicated that 0.5 h contact with gastric fluid was sufficient to form PEC film upon transit in the intestinal fluid, implying the difference in patient gastric emptying time has marginal influence on drug release profile, which is an advantage for consistent therapeutic efficacy.
Table 2.
Mathematical modeling and drug release kinetics.
| pH | SGF Contact time (h) | k (%/h) | k1.2 (%/h) | k6.8 (%/h) |
|---|---|---|---|---|
| 1.2 | 7.97 | 13.37 | 6.80 | |
| 6.8 | 3.88 | 12.99 | 5.60 | |
| 1.2–6.8 | 4.16 | 13.88 | 4.80 | |
| 0.5 | 4.02 | 29.06 | 4.45 | |
| 1 | 4.00 | 18.64 | 4.47 | |
| 2 | 4.16 | 13.88 | 4.80 |
3.9. In vivo pharmacokinetic study
To further demonstrate that the in vitro sustained-release behavior can also be achieved in vivo, the CS–CBM matrix based tablets (CS (400 kDa): CBM (974P): VH = 5:1:2, w:w:w), which had lower burst release and complete drug release, was selected for in vivo study. The mean plasma drug concentration-time profile of the test tablets and corresponding pharmacokinetics parameters are shown in Fig. 7A and Table 3. Tmax of the tablets was about 12 h and the drug was completely eliminated in the blood for more than 48 h. This phenomenon showed that the designed formulation could also achieve good sustained-release effect in vivo.
Fig. 7.
(A) Mean plasma drug concentration-time profile in Beagle dogs (n = 3); (B) in vivo and in vitro correlation profile.
Table 3.
Pharmacokinetics parameters of the test tablets in Beagle dogs (n = 3).
| Parameters | Test |
|---|---|
| Cmax (µg/ml) | 0.641 ± 0.023 |
| Tmax (h) | 12 |
| Ke | 0.084 ± 0.011 |
| t1/2 (h) | 8.33 ± 1.12 |
| AUC(0-t) (µg⋅h/ml) | 12.23 ± 0.62 |
| AUC(0-∞) (µg⋅h/ml) | 14.40 ± 1.34 |
| MRT (h) | 18.29 ± 0.28 |
For sustained-release preparations, the establishment of an in vitro and in vivo correlation (IVIVC) has important implications in quality control and regulatory compliance. And with preferable IVIVC, the in vitro release results could be used as indicators of in vivo bioavailability [28]. Taking in vivo absorption percentage (Fa), calculated via Wagner–Nelson method, as the independent variable and in vitro cumulative release ratio (Fd) at corresponding time as dependent variable, as shown in Fig. 7B, a level A linear correlation between Fa and Fd was established (Fa = 1.092Fd–8.800 (r = 0.975)). Therefore, in vitro drug release data could be used as the indicator of in vivo bioavailability.
4. Conclusion
The present study demonstrated that CS–CBM combination system can be used as the matrix to design sustained-release tablets using simple preparation technology, which can well control the release of highly water-soluble drugs with good system robustness. It was found that CS–CBM combination system weakened the potential influence of CS, CBM material properties and gastric emptying time on drug release profile. Demonstrated by direct observation, differential scanning calorimetry and Fourier transform infrared spectroscopy, in situ self-assembled polyelectrolyte complex film was formed on the tablet surface in simulated gastrointestinal fluid, which contributed to the tunable and robust control of drug release. The sustained drug release behavior was further demonstrated in vivo in Beagle dogs, with level A in vitro and in vivo correlation (IVIVC) established successfully, indicating the in vitro release method established in this paper can be used as a tool for in vivo bioavailability predication. In conclusion, chitosan–carbomer matrix tablets are promising system to tune and control the release of highly water-soluble drugs with good system robustness.
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Acknowledgments
This work was supported by the Distinguished Professor Project of Liaoning Province (2015).
References
- 1.Colombo P., Bettini R., Peppas N.A. Observation of swelling process and diffusion front position during swelling in hydroxypropyl methyl cellulose (HPMC) matrices containing a soluble drug. J Control Release. 1999;61:83–91. doi: 10.1016/s0168-3659(99)00104-2. [DOI] [PubMed] [Google Scholar]
- 2.Ching A.L., Liew C.V., Chan L.W., Heng P.W.S. Modifying matrix micro-environmental pH to achieve sustained drug release from highly laminating alginate matrices. Eur J Pharm Sci. 2008;33:361–370. doi: 10.1016/j.ejps.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Parojcic J., Duric Z., Jovanovic M., Ibric S. An investigation into the factors influencing drug release from hydrophilic matrix tablets based on novel carbomer polymers. Drug Deliv. 2004;11:59–65. doi: 10.1080/10717540490265379. [DOI] [PubMed] [Google Scholar]
- 4.Talukdar M.M., Kinget R. Swelling and drug release behaviour of xanthan gum matrix tablets. Int J Pharm. 1995;120:63–72. [Google Scholar]
- 5.Hardy I.J., Windberg-Baarup A., Neri C., Byway P.V., Booth S.W., Fitzpatrick S. Modulation of drug release kinetics from hydroxypropyl methyl cellulose matrix tablets using polyvinyl pyrrolidone. Int J Pharm. 2007;337:246–253. doi: 10.1016/j.ijpharm.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 6.Palmer D., Levina M., Douroumis D., Maniruzzaman M., Morgan D.J., Thomas P.F. Mechanism of synergistic interactions and its influence on drug release from extended release matrices manufactured using binary mixtures of polyethylene oxide and sodium carboxymethylcellulose. Colloids Surf B Biointerfaces. 2013;104:174–180. doi: 10.1016/j.colsurfb.2012.11.025. [DOI] [PubMed] [Google Scholar]
- 7.Tapia C., Costa E., Moris M., Sapag-Hagar J., Valenzuela F., Basualto C. Study of the influence of the pH media dissolution, degree of polymerization, and degree of swelling of the polymers on the mechanism of release of diltiazem from matrices based on mixtures of chitosan/alginate. Drug Dev Ind Pharm. 2002;28:217–224. doi: 10.1081/ddc-120002455. [DOI] [PubMed] [Google Scholar]
- 8.Tapia C., Escobar Z., Costa E. Comparative studies on polyelectrolyte complexes and mixtures of chitosan–alginate and chitosan–carrageenan as prolonged diltiazem clorhydrate release systems. Eur J Pharm Biopharm. 2004;57:65–75. doi: 10.1016/s0939-6411(03)00153-x. [DOI] [PubMed] [Google Scholar]
- 9.Li L., Wang L., Li J. Insights into the mechanisms of chitosan–anionic polymers-based matrix tablets for extended drug release. Int J Pharm. 2014;476:253–265. doi: 10.1016/j.ijpharm.2014.09.057. [DOI] [PubMed] [Google Scholar]
- 10.Zhang T., Mao S., Sun W. Design and in vitro evaluation of a film-controlled dosage form self-converted from monolithic tablet in gastrointestinal environment. J Pharm Sci. 2010;99:4678–4690. doi: 10.1002/jps.22163. [DOI] [PubMed] [Google Scholar]
- 11.Shao Y., Li L., Gu X., Wang L., Mao S. Evaluation of chitosan–anionic polymers based tablets for extended-release of highly water-soluble drugs. Asian J Pharm Sci. 2015;10:24–30. [Google Scholar]
- 12.Li L., Wang L., Shao Y. Elucidation of release characteristics of highly soluble drug trimetazidine hydrochloride from chitosan-carrageenan matrix tablets. J Pharm Sci. 2013;102:2644–2654. doi: 10.1002/jps.23632. [DOI] [PubMed] [Google Scholar]
- 13.Li L., Li J., Si S. Effect of formulation variables on in vitro release of a water-soluble drug from chitosan–sodium alginate matrix tablets. Asian J Pharm Sci. 2015;10:314–321. [Google Scholar]
- 14.Mao S., Shuai X., Unger F., Wittmar M., Xie X., Kissel T. Synthesis, characterization and cytotoxicity of poly(ethylene glycol)-graft-trimethyl chitosan block copolymers. Biomaterials. 2005;26:6343–6356. doi: 10.1016/j.biomaterials.2005.03.036. [DOI] [PubMed] [Google Scholar]
- 15.Rosca C., Popa M.I., Lisa G., Chitanu G.C. Interaction of chitosan with natural or synthetic anionic polyelectrolytes. 1. The chitosan–carboxymethylcellulose complex. Carbohydr Polym. 2005;62:35–41. [Google Scholar]
- 16.Park S.H., Chun M.K., Choi H.K. Preparation of an extended-release matrix tablet using chitosan/Carbopol interpolymer complex. Int J Pharm. 2008;347:39–44. doi: 10.1016/j.ijpharm.2007.06.024. [DOI] [PubMed] [Google Scholar]
- 17.Peng Y., Li J., Li J., Fei Y., Dong J., Pan W. Optimization of thermosensitive chitosan hydrogels for the sustained delivery of venlafaxine hydrochloride. Int J Pharm. 2013;441:482–490. doi: 10.1016/j.ijpharm.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 18.Wang Y.J., Assaad E., Ispas-Szabo P., Mateescu M.A., Zhu X.X. NMR imaging of chitosan and carboxymethyl starch tablets: swelling and hydration of the polyelectrolyte complex. Int J Pharm. 2011;4198:215–221. doi: 10.1016/j.ijpharm.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 19.Shah V.P., Tsong Y., Sathe P., Liu J.P. In vitro dissolution profile comparison-statistics and analysis of the similarity factor, f2. Pharm Res. 1998;15:889–896. doi: 10.1023/a:1011976615750. [DOI] [PubMed] [Google Scholar]
- 20.Liew C.V., Chan L.W., Ching A.L., Heng P.W.S. Evaluation of sodium alginate as drug release modifier in matrix tablets. Int J Pharm. 2006;309:25–37. doi: 10.1016/j.ijpharm.2005.10.040. [DOI] [PubMed] [Google Scholar]
- 21.Siepmann J., Peppas N.A. Hydrophilic matrices for controlled drug delivery: an improved mathematical model to predict the resulting drug release kinetics (the “sequential layer” model) Pharm Res. 2000;17:1290–1298. doi: 10.1023/a:1026455822595. [DOI] [PubMed] [Google Scholar]
- 22.Huanbutta K., Cheewatanakornkool K., Terada K., Nunthanid J., Sriamornsak P. Impact of salt form and molecular weight of chitosan on swelling and drug release from chitosan matrix tablets. Carbohydr Polym. 2013;97:26–33. doi: 10.1016/j.carbpol.2013.04.073. [DOI] [PubMed] [Google Scholar]
- 23.Li L., Wang L., Shao Y., Ni R., Zhang T., Mao S. Drug release characteristics from chitosan–alginate matrix tablets based on the theory of self-assembled film. Int J Pharm. 2013;450:197–207. doi: 10.1016/j.ijpharm.2013.04.052. [DOI] [PubMed] [Google Scholar]
- 24.Zoppi A., Linck Y.G., Monti G.A., Genovese D.B., Jimenez Kairuz Á.F., Manzo R.H. Studies of pilocarpine:carbomer intermolecular interactions. Int J Pharm. 2012;427:252–259. doi: 10.1016/j.ijpharm.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 25.de la Torre P.M., Enobakhare Y., Torrado G., Torrado S. Release of amoxicillin from polyionic complexes of chitosan and poly(acrylic acid). Study of polymer/polymer and polymer/drug interactions within the network structure. Biomaterials. 2003;24:1499–1506. doi: 10.1016/s0142-9612(02)00512-4. [DOI] [PubMed] [Google Scholar]
- 26.Chavasit V., Torres J.A. Chitosan-poly(acrylic acid): mechanism of complex formation and potential industrial applications. Biotechnol Prog. 1990;6:2–6. doi: 10.1021/bp00001a001. [DOI] [PubMed] [Google Scholar]
- 27.Hamman J.H. Chitosan based polyelectrolyte complexes as potential carrier materials in drug delivery systems. Mar Drugs. 2010;8:1305–1322. doi: 10.3390/md8041305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang L., Feng R., Gao J., Xi Y., Huang G. Generic sustained release tablets of trimetazidine hydrochloride: preparation and in vitro–in vivo correlation studies. Asian J Pharm Sci. 2016;11:417–426. [Google Scholar]