Graphical Abstract
Keywords: Solid dispersion, Molecular modeling, Dissolution process, Ibuprofen
Abstract
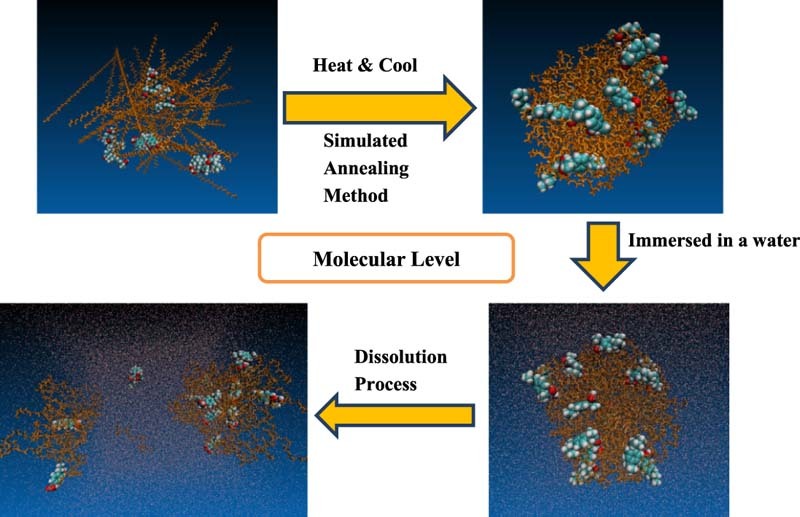
Dissolution molecular mechanism of solid dispersions still remains unclear despite thousands of reports about this technique. The aim of current research was to investigate the molecular dissolution mechanism of solid dispersions by molecular dynamics simulations. The formation of ibuprofen/polymer solid dispersions was modeled by the simulated annealing method. After that, the models of solid dispersions were immersed into the water box with 25–30 Å thicknesses and 50–100 ns MD simulations were performed to all systems. Simulation results showed various dissolution behaviors in different particle sizes and various polymers of solid dispersions. Small-sized particles of solid dispersions dissolved quickly in the water, while the large particles of PEG or PVP-containing solid dispersions gradually swelled in the dissolution process and drug molecules may aggregate together. In the dissolution process, the carboxylic groups of ibuprofen molecules turned its direction from polymer molecules to external water box and then the drug molecules left the polymer coils. At the same time, polymer coils gradually relaxed and became free polymer chains in the solution. In addition, solid dispersion with poloxamer could prevent the precipitate of drug molecules in the dissolution process, which is different from those of PEG or PVP-containing systems. This research provided us clear images of dissolution process of solid dispersions at the molecular level.
1. Introduction
Solubilization of poorly soluble drugs attracts high attentions from formulation scientists in the pharmaceutical industry [1]. Amorphous solid dispersion is one of important drug delivery techniques to enhance the solubility and dissolution rate for crystalline drugs with low solubility [2]. In the system of solid dispersions, the crystalline structure of drugs was changed to amorphous state and resulted in higher bioavailability [3]. The first solid dispersion (SD) was reported by Sekiguchi and Obi in 1961 [4]. Several products with solid dispersion techniques have been commercialized in the pharmaceutical market [5]. In recent two decades, publications in solid dispersion area increase sharply. However, there are still four key problems about solid dispersions to be answered: the solid state structure of solid dispersions; the mechanism of dissolution enhancement; the aging issue during storage period; and the understanding of the in vitro/in vivo correlation [6]. Recent review has raised three possible assumptions of how polymeric amorphous solid dispersions (PASD) dissolve in aqueous solution: (a) PASD nano-clusters dissolve quickly into the solution; (b) the PASD particles gradually dissolve and the drug molecules remain amorphous state in the undissolved particles; (c) the PASD particles gradually dissolve, but the recrystallization of drugs may happen at the surface of the undissolved particles [7]. However, there is still lack of direct and clear evidence for dissolution molecular mechanism of solid dispersions in aqueous environment.
Molecular dynamics (MD) simulation describes the molecular systems by mimicking the behavior of molecules at the atomistic level [8]. Meanwhile, molecular simulation is able to calculate the physical properties of drug/excipient systems without costly experiments [9]. Recent progress about molecular modeling studies for solid dispersions was summarized in Table 1. Our previous study used molecular modeling to investigate the solid state structure of ibuprofen/polymer SD by the simulated annealing method and provided an in silico protocol to the preparation of SD [19]. Three polymers were selected as the carriers, including polyethylene glycol (PEG), poloxamer and polyvinylpyrrolidone (PVP). Simulation results showed linear polymer chains form the random coils under heat and the drug molecules stick on the surface of polymer coils. This research provided more reasonable molecular images of solid dispersions than the existing theory.
Table 1.
Recent progress of molecular modeling in solid dispersions.
| Drugs | Polymers | Simulation methods | References |
|---|---|---|---|
| Lafutidine (LAFT) | Soluplus, PEG 400, Lutrol F127, Lutrol F68 | Molecular dynamics (MD) simulation; Gaussian program in Schrodinger, Maestro software program | [10] |
| Artemisinin | PEG, PVP | Molecular dynamics (MD) simulation; Materials Studio 6.0; COMPASS force field; | [11] |
| Carbamazepine | Poloxamer 188 | Molecular dynamics (MD) simulation; XenoView software; PCFF force field parameters and charges; | [3] |
| Posaconazole | Soluplus, PEG 400, Lutrol F127, Lutrol F68, TPGS | Molecular dynamics (MD) simulation; Gaussian program in Schrodinger, Maestro software program; | [12] |
| Curcumin | MPEG-PCL | Molecular dynamics (MD) simulation; HyperChem software (HyperChem Professional 80); CHARMM27 force field; Simulating anneal method; | [13] |
| Paclitaxel | PEG, PCL, MPEG-PCL | Molecular dynamics (MD) simulation and molecular docking; HyperChem software (HyperChem Professional 80); CHARMM27 force field; simulating anneal method; AutoDock Vina | [14] |
| Propranolol HCl, diphenhydramine HCl, paracetamol, ibuprofen, dichlofenac Na, hydrocortisone | Eudragit L100, Eudragit EPO, Eudragit L100-55, Kollidon VA64 | Computational model based on quantum mechanical (QM) calculations; GaussView software; Gaussian 09 program; | [15] |
| Lumefantrine | Soluplus, Kollidone VA64, Plasdone S630 | Molecular dynamics (MD) simulation; Gaussian program in Schrodinger; Maestro software program; | [16] |
| Indomethacin (IMC) | PVP | Molecular dynamics (MD) simulation; AMBER software; AMBER-ff03 forcefield; Gaussian 03 program; | [17] |
| Cetirizine HCl, verapamil HCl, | Eudragit L100 and L100-55 | Molecular dynamics (MD) simulation; Gaussian 09 program in Schrodinger; | [18] |
Following our previous study [19], the aim of our study was to further investigate the dissolution molecular mechanism of SD by MD approach. Ibuprofen (IBU), an anti-inflammatory drug for moderating pain and fever, was still chosen as the model drug, and PEG, PVP and poloxamer were selected as the polymeric carriers.
2. Material and simulation details
2.1. Model establishing
The model of the selected polymer and drug molecules were built by Discovery Studio Visualizer 3.1 (http://accelrys.com/products/discovery-studio/). The molecular structures of the polymers (PEG, PVP, poloxamer 188) were same as our previous publication [19]. The model of PEG contains 20 repeating units of ethylene oxide. The PVP model contains nine repeating units of vinylpyrrolidone. The model of poloxamer was composed of a central chain with three repeating units of propylene oxide, flanked by two chains with 8 repeating units of ethylene oxide. Ibuprofen was used as a model drug. The structure of ibuprofen lattice was downloaded from Cambridge Structural Database and crystal structure of racemate and enantiomer (S)-(+)-ibuprofen was selected [20]. These SD models with the Packmol program were further optimized from previous manual-built models in our previous publication [19]. Packmol program [21] (http://www.ime.unicamp.br/~martinez/packmol/) was used to obtain random distribution of polymers with a tolerance distance of 3.0 Å in a limited boundary box. The details of all systems were shown in Table 2.
Table 2.
The details of solid dispersion systems in the simulation process.
| SD system no. | Weight ratio | Molar ratio | Numbers of ibuprofen | Numbers of polymer chains | Numbers of water molecules (water box) | Total atom number in the systems | Initial gyration radius |
|---|---|---|---|---|---|---|---|
| IBU/PEG | 1:5 | 4:5 | 4 | 5 | 29,529 (30 Å) | 89,434 | 13.37 Å |
| IBU/PVP | 1:10 | 4:8 | 4 | 8 | 30,894 (30 Å) | 94,012 | 13.75 Å |
| IBU/POL | 1:10 | 4:10 | 4 | 10 | 36,036 (30 Å) | 109,690 | 14.81 Å |
| IBU/PEG-2 | 1:5 | 16:20 | 16 | 20 | 22,579 (25 Å) | 71,125 | 15.37 Å |
| IBU/PVP-2 | 1:10 | 16:32 | 16 | 32 | 32,480 (25 Å) | 103,120 | 18.82 Å |
| IBU/POL-2 | 1:10 | 16:40 | 16 | 40 | 30,771 (25 Å) | 98,641 | 19.12 Å |
2.2. Preparation process modeling of solid dispersions by the simulated annealing method
The molecular dynamics (MD) simulations utilized the AMBER14 software package with the general AMBER force field (gaff) for all carriers and drugs. The models of all systems were built using the LEAP module in AmberTools 1.5. The simulated annealing method was similar to our previous publication [19]. After minimization, 2 ns annealing simulation was performed. Firstly, the system was gradually heated from 0 to 500 K in 200 ps, and then kept at a temperature of 500 K for 1000 ps to equilibrate the systems. Next, the system was quickly cooled down from 500 to 300 K in 100 ps and finally the systems were kept at a temperature of 300 K for 700 ps for equilibration.
2.3. Dissolution process modeling of solid dispersions by MD simulations
After the simulated annealing process, the solid dispersion system was immersed in a water box with a solvation shell of 25 or 30 Å thickness using TIP3P model for water with the general AMBER force field (gaff) and the ff14SB force field. In the minimization procedure, the structures of drugs and polymers were subjected to 2000 steps of steepest descent minimization followed by 2000 steps of conjugate gradient minimization. The whole system was subjected to 2000 steps of conjugate gradient minimization followed by 3000 steps of conjugate gradient minimization. After minimization, the system was heated at 300 K while keeping the structure of the solid dispersion fixed with weak restraints. The non-bonded cutoff distance was 8.0 Å. Then, 50 or 100 ns MD simulation at 300 K was performed in the solvated system to simulate the dissolution process of the solid dispersion. The Langevin Dynamics was used to control the temperature using a collision frequency of 1.0 ps−1. In these simulations, the parameter iwrap = 1 of MD input files were used to wrap all molecules into a primary box. Constant pressure periodic boundary with an average pressure of 1 atm was also applied. Initial Gyration Radius gave the reference of the particle size for different SD systems after simulated anneal process.
3. Results and discussion
During simulated annealing process, the polymer chains formed random coils, the crystal structure of ibuprofen was broken and the drug molecules were stuck or inserted to the surface of the polymer coils to form an amorphous solid dispersion, the drugs molecules were molecularly dispersed in the SDs matrix. SD system of ibuprofen with polymers (e.g. PEG, poloxamer and PVP) also showed similar results. Various SD systems with polymers in different lengths and different weight ratios gained similar results (data not shown). The temperature change during the simulated annealing process was shown in Fig. 1. It was not surprising that these results were similar to our previous report.
Fig. 1.
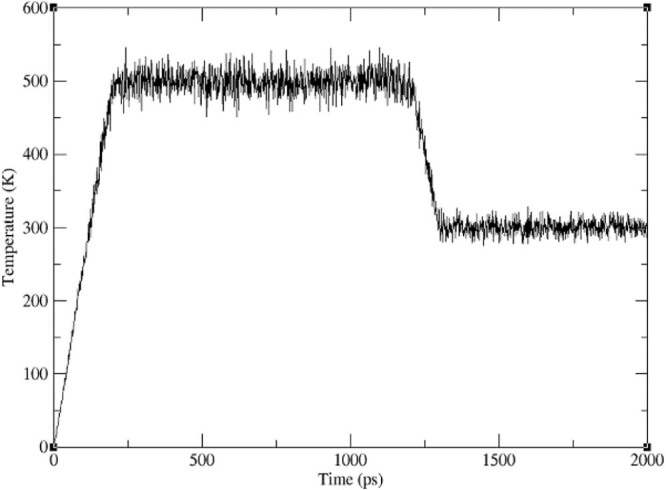
Temperature change vs time for the systems in the simulated annealing method.
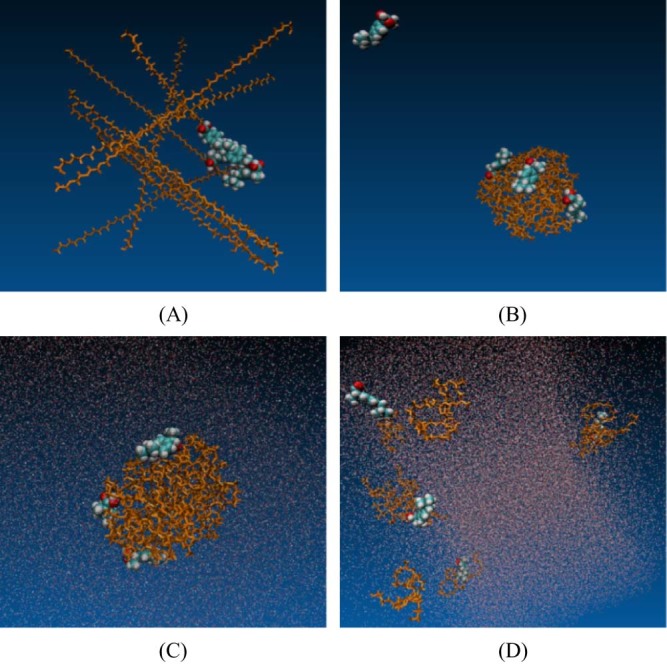
3.1. Simulation results of small particle systems
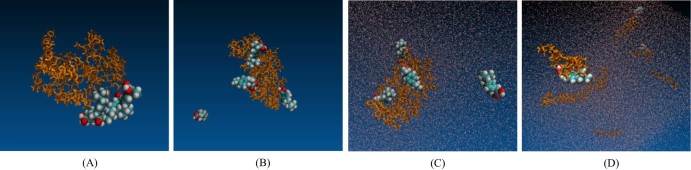
Fig. 2, Fig. 3 and Fig. 4 indicated the dissolution process of small particles of solid dispersions with three polymers. In the dissolution process, the carboxylic group of ibuprofen molecules turned its direction from polymer molecules to external water molecules and ibuprofen molecules slowly left the surface of the polymer coils. At the same time, all three polymer coils including PEG, POL and PVP became quickly relaxed and the polymer chains were released in the solution, which was in agreement with the assumption (a) [7]. Due to the less numbers of the polymer chain, the interaction between the chain–chain and chain–drug was weaker compare to larger particle system. When the particle was immersed in the aqueous condition, the polymer matrix had easily disentangled the random coils. At the same time, the water molecules quickly permeated into the carrier matrix, while the polymer and drug molecules rapidly dispersed and diffused into the water.
Fig. 2.
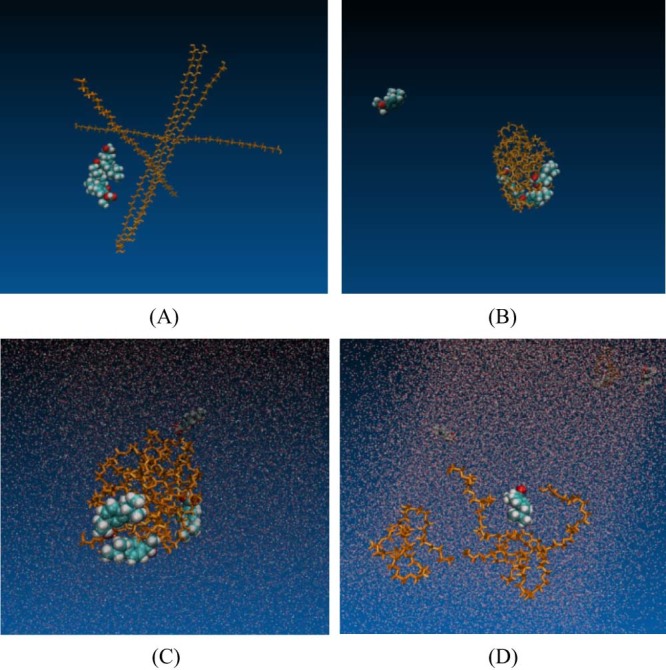
Simulation process of IBU-PEG small particle system (drug-polymer unit ratio 4:5, weight ratio 1:5). (A) Initial model of ibuprofen crystal and PEG system, (B) the solid dispersion system after simulated annealing process, (C) solid dispersion in aqueous phase at 0 ns, (D) solid dispersion in aqueous phase after 50 ns.
Fig. 3.
Simulation process of IBU-POL small particle system (drug-polymer unit ratio was 4:10, weight ratio 1:10). (A) Starting model of ibuprofen crystal and POL system, (B) the solid dispersion system after simulated annealing process, (C) solid dispersion in aqueous phase, (D) solid dispersion in aqueous phase after 50 ns.
Fig. 4.
Simulation process of IBU-PVP small particle system (drug-polymer unit ratio was 4:8, weight ratio 1:10). (A) Starting model of ibuprofen crystal and PVP system, (B) the solid dispersion system after simulated annealing process, (C) solid dispersion in aqueous phase, (D) solid dispersion in aqueous phase after 50 ns.
3.2. Simulation results of large particle systems
Fig. 5, Fig. 6 and Fig. 7 indicated the dissolution process of large particles of solid dispersion with three polymers. In the dissolution process, more and more ibuprofen molecules in the large particles were gradually released from solid dispersion systems and the polymer coils increased the relaxed state with the time. However, large SD particles with different polymers presented various dissolution behaviors, which was different from small SD particles. The larger particle system of IBU-PEG and IBU-PVP showed the aggregation of drug molecules at the later stage of dissolution process, which may result in further recrystallization and low dissolution rate. In the preparation process of solid dispersions, it is clearly shown that the drug molecules were randomly dispersed on the surface of amorphous polymer coils by the simulated annealing method. However, the drug aggregation in the dissolution process indicated that the solid dispersion systems with PEG or PVP may have the recrystallization problem in the GI tract and then lead to the bioavailability issue. Previous studies investigated the reprecipitation inhibitory effect of three polymers (PEG 6000, PVP K30 and Eudragit) for patchouli alcohol supersaturated solutions [22]. The results showed that the inhibitory effect of PEG 6000 and PVP K30 was less effective than that of Eudragit.
Fig. 5.
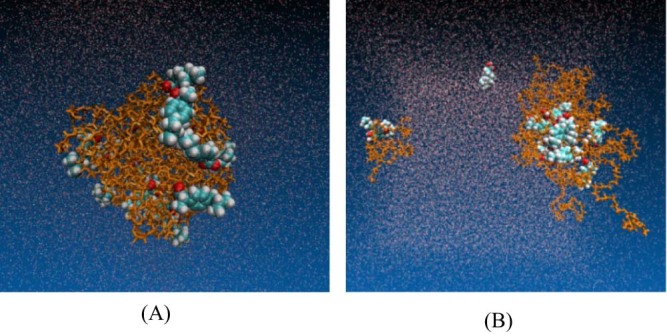
Simulated dissolution process of IBU-PEG large particle system (drug-polymer unit ratio was 16:20, weight ratio was 1:5). (A) IBU-PEG SD system in aqueous phase, (B) IBU-PEG SD system in aqueous phase after 100 ns.
Fig. 6.
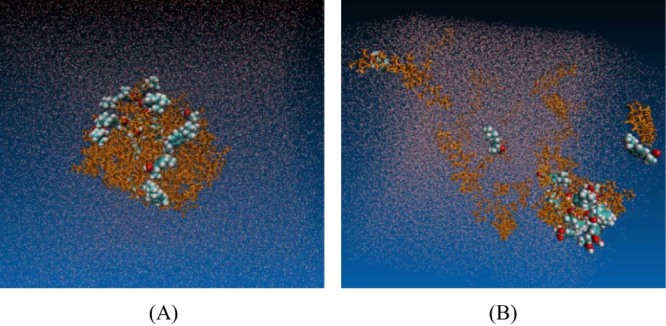
Simulated dissolution process of IBU-PVP large particle system (drug-polymer unit ratio was 16:32, weight ratio was 1:10). (A) IBU-PVP SD system in aqueous phase, (B) IBU-PVP SD system in aqueous phase after 100 ns.
Fig. 7.
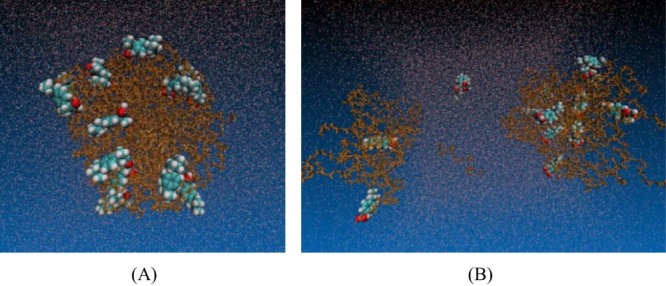
Simulated dissolution process of IBU-POL large particle system (drug-polymer unit ratio was 16:40, weight ratio was 1:10). (A) IBU-POL SD system in aqueous phase, (B) IBU-POL SD system in aqueous phase after 100 ns.
3.3. Discussion of two dissolution behaviors in large particle systems
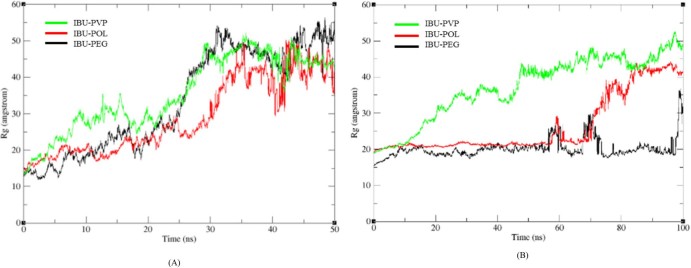
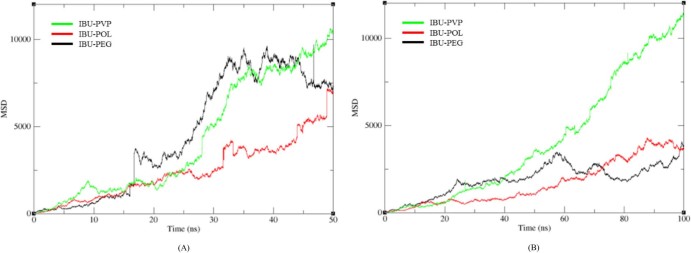
PEGs are semi-crystalline polymers of ethylene oxide and widely used in solid dispersions. However, it is quite interesting that PEG promotes crystallization for some compounds (e.g. ibuprofen, fenofibrate), which is different from other polymers for crystallization hindrance [23]. For PVP, recent research with ATR (Attenuated Total Reflection)–FTIR (Fourier-Transform-Infrared) spectroscopic imaging indicated that too fast dissolution of PVP/Aprepitant solid dispersion could negatively influence the bioavailability due to high local super-saturation and consequent recrystallization [24]. The good water affinity of PVP solid dispersions makes the polymer fast dissolving, which leads to phase separation and local recrystallization of the drug molecules [25]. Fig. 8B also showed that the gyration radius of IBU-PVP system increased much faster than another two systems after 20 ns, which also indicated that the PVP system dissolved more quickly than PEG and POL systems. Moreover, Fig. 9B showed that the overall mean square displacement plot of PVP was clearly increased sharply compared to PEG and POL systems, which also indicated that the displacement of the whole atoms in PVP system moved faster. The simulation results gave a clear molecular image of the aggregation and/or recrystallization process in solid dispersion systems with PEG or PVP.
Fig. 8.
The mass-weighted radius of gyration of SD system in different size scale, with fluctuation as a function of time. (A) Small particle size system, (B) larger particle size system.
Fig. 9.
The overall mean square displacement plot of SD system in different size scale, with fluctuation as a function of time. (A) Small particle size system, (B) larger particle size system.
For large particles with poloxamer, the drug and polymer molecules of poloxamer SD particles were gradually released and the drug remains amorphous form in the undissolved particles in 100 ns simulations, which is different from the systems with PEG and PVP. The possible reason is that amphiphilic property of poloxamer, as a nonionic surfactant, could effectively hinder the aggregation of drug molecules in the dissolution process. This result was also observed in the experimental studies. For example, solubility and dissolution rate of nifedipine/poloxamer solid dispersion were better than those of the systems with PEGs or cyclodextrin complex [26]. Furthermore, the increasing amount of Soluplus in the Aprepitant-Soluplus-PVP ternary solid dispersion systems could effectively delay the onset of recrystallization due to the amphiphilic nature of Soluplus [27]. Another experimental study indicated that hypromellose acetate succinate (HPMCAS) with the amphiphilic nature showed better stabilization of solid dispersions than that of hypromellose systems [28]. Thus, we can see that the amphiphilic polymer (e.g. poloxamer, Soluplus or HPMCAS) could effectively prevent the recrystallization in the dissolution process and may enhance the bioavailability of poorly soluble drugs in solid dispersions.
3.4. Combination of our simulation results and the three dissolution assumptions
Our simulation results indicated that the dissolution process of small SD particles agrees with the hypothesis (a), while large SD particles agreed with the hypotheses (b) and (c) [7]. The hypothesis (a) assumed that the drug and polymer molecules rapidly dissolved and dispersed in the aqueous solution. However, large SD particles with different polymers showed different dissolution behaviors. In the dissolution process, the drug molecules in the large particles with PEG or PVP easily shift and aggregate together, which was in consistence with the hypothesis (c) of drug recrystallization in the dissolution process [24], [25], [29]. The large SD particles with poloxamer could effectively hinder the aggregation of drug molecules in the dissolution process, indicated in hypothesis (b). Therefore, our simulations could effectively mimic the dissolution process of solid dispersion.
4. Conclusion
This research investigated the dissolution process of solid dispersion particles at molecular level. The results agreed with recent hypotheses of different dissolution mechanism of solid dispersions [7]. Our research will provide useful clues for future formulation development of solid dispersions.
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Acknowledgment
University of Macau research grants (MYRG2016-00038-ICMS-QRCM and MYRG2016-00040-ICMS-QRCM) are gratefully acknowledged for providing financial support.
Footnotes
Peer review under responsibility of Shenyang Pharmaceutical University.
References
- 1.Vasconcelos T., Sarmento B., Costa P. Solid dispersions as strategy to improve oral bioavailability of poor water soluble drugs. Drug Discov Today. 2007;12:1068–1075. doi: 10.1016/j.drudis.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 2.Lakshman J.P., Cao Y., Kowalski J. Application of melt extrusion in the development of a physically and chemically stable high-energy amorphous solid dispersion of a poorly water-soluble drug. Mol Pharm. 2008;5:994–1002. doi: 10.1021/mp8001073. [DOI] [PubMed] [Google Scholar]
- 3.Medarević D.P., Kachrimanis K., Mitrić M. Dissolution rate enhancement and physicochemical characterization of carbamazepine-poloxamer solid dispersions. Pharm Dev Technol. 2016;21:268–276. doi: 10.3109/10837450.2014.996899. [DOI] [PubMed] [Google Scholar]
- 4.Sekiguchi K., Obi N. Studies on absorption of eutectic mixture. I. A comparison of the behavior of eutectic mixture of sulfathiazole and that of ordinary sulfathiazole in man. Chem Pharm Bull. 1961;9:866–872. [Google Scholar]
- 5.Mitra A., Li L., Marsac P. Impact of polymer type on bioperformance and physical stability of hot melt extruded formulations of a poorly water soluble drug. Int J Pharm. 2016;505:107–114. doi: 10.1016/j.ijpharm.2016.03.036. [DOI] [PubMed] [Google Scholar]
- 6.Craig D.Q. The mechanisms of drug release from solid dispersions in water-soluble polymers. Int J Pharm. 2002;231:131–144. doi: 10.1016/s0378-5173(01)00891-2. [DOI] [PubMed] [Google Scholar]
- 7.Baghel S., Cathcart H., O'Reilly N.J. Polymeric amorphous solid dispersions: a review of amorphization, crystallization, stabilization, solid-state characterization, and aqueous solubilization of biopharmaceutical classification system class II drugs. J Pharm Sci. 2016;105:2527–2544. doi: 10.1016/j.xphs.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 8.Leach A.R. 2nd ed. Prentice Hall; 2001. Molecular modelling: principles and applications; pp. 1–25. Chapter 1. [Google Scholar]
- 9.Maus M., Wagner K.G., Kornherr A. Molecular dynamics simulations for drug dosage form development: thermal and solubility characteristics for hot-melt extrusion. Mol Simul. 2008;34:1197–1207. [Google Scholar]
- 10.Fule R., Amin P. Development and evaluation of lafutidine solid dispersion via hot melt extrusion: investigating drug-polymer miscibility with advanced characterisation. Asian J Pharm Sci. 2014;9:92–106. doi: 10.1155/2014/146781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shahzad Y., Sohail S., Arshad M.S. Development of solid dispersions of artemisinin for transdermal delivery. Int J Pharm. 2013;457:197–205. doi: 10.1016/j.ijpharm.2013.09.027. [DOI] [PubMed] [Google Scholar]
- 12.Fule R., Amin P. Hot melt extruded amorphous solid dispersion of posaconazole with improved bioavailability: investigating drug-polymer miscibility with advanced characterisation. Biomed Res Int. 2014 doi: 10.1155/2014/146781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gong C., Deng S., Wu Q. Improving antiangiogenesis and anti-tumor activity of curcumin by biodegradable polymeric micelles. Biomaterials. 2013;34:1413–1432. doi: 10.1016/j.biomaterials.2012.10.068. [DOI] [PubMed] [Google Scholar]
- 14.Gong C., Xie Y., Wu Q. Improving anti-tumor activity with polymeric micelles entrapping paclitaxel in pulmonary carcinoma. Nanoscale. 2012;4:6004–6017. doi: 10.1039/c2nr31517c. [DOI] [PubMed] [Google Scholar]
- 15.Maniruzzaman M., Pang J., Morgan D.J. Molecular modeling as a predictive tool for the development of solid dispersions. Mol Pharm. 2015;12:1040–1049. doi: 10.1021/mp500510m. [DOI] [PubMed] [Google Scholar]
- 16.Fule R., Meer T., Sav A. Solubility and dissolution rate enhancement of lumefantrine using hot melt extrusion technology with physicochemical characterisation. J Pharm Investig. 2013;43:305–321. [Google Scholar]
- 17.Xiang T.X., Anderson B.D. Molecular dynamics simulation of amorphous indomethacin–poly (vinylpyrrolidone) glasses: solubility and hydrogen bonding interactions. J Pharm Sci. 2013;102:876–891. doi: 10.1002/jps.23353. [DOI] [PubMed] [Google Scholar]
- 18.Maniruzzaman M., Snowden M.J., Bradley M.S. Studies of intermolecular interactions in solid dispersions using advanced surface chemical analysis. RSC Adv. 2015;5:84936. [Google Scholar]
- 19.Ouyang D. Investigating the molecular structures of solid dispersions by the simulated annealing method. Chem Phys Lett. 2012;554:177–184. [Google Scholar]
- 20.Hansen L.K., Perlovich G.L., Bauer-Brandl A. Redetermination and H-atom refinement of (S)-(+)-ibuprofen. Acta Crystallogr Sect E Struct Rep Online. 2003;59:o1357–o1358. [Google Scholar]
- 21.Martínez L., Andrade R., Birgin E.G. PACKMOL: a package for building initial configurations for molecular dynamics simulations. J Comput Chem. 2009;30:2157–2164. doi: 10.1002/jcc.21224. [DOI] [PubMed] [Google Scholar]
- 22.Chen Y.L., Liao J.B., Liang Y.Z. Characterization of solid dispersions of Patchouli alcohol with different polymers: effects on the inhibition of reprecipitation and the improvement of dissolution rate. Drug Dev Ind Pharm. 2015;41:436–444. doi: 10.3109/03639045.2013.877482. [DOI] [PubMed] [Google Scholar]
- 23.Zhu Q., Harris M.T., Taylor L.S. Modification of crystallization behavior in drug/polyethylene glycol solid dispersions. Mol Pharm. 2012;9:546–553. doi: 10.1021/mp200546p. [DOI] [PubMed] [Google Scholar]
- 24.Punčochová K., Ewing A.V., Gajdošová M. Identifying the mechanisms of drug release from amorphous solid dispersions using MRI and ATR-FTIR spectroscopic imaging. Int J Pharm. 2015;483:256–267. doi: 10.1016/j.ijpharm.2015.02.035. [DOI] [PubMed] [Google Scholar]
- 25.Punčochová K., Vukosavljevic B., Hanuš J. Non-invasive insight into the release mechanisms of a poorly soluble drug from amorphous solid dispersions by confocal Raman microscopy. Eur J Pharm Biopharm. 2016;101:119–125. doi: 10.1016/j.ejpb.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 26.Chutimaworapan S., Ritthidej G.C., Yonemochi E. Effect of water-soluble carriers on dissolution characteristics of nifedipine solid dispersions. Drug Dev Ind Pharm. 2000;26:1141–1150. doi: 10.1081/ddc-100100985. [DOI] [PubMed] [Google Scholar]
- 27.Punčochová K., Ewing A.V., Gajdošová M. The combined use of imaging approaches to assess drug release from multicomponent solid dispersions. Pharm Res. 2017;34:990–1001. doi: 10.1007/s11095-016-2018-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.DiNunzio J.C., Hughey J.R., Brough C. Production of advanced solid dispersions for enhanced bioavailability of itraconazole using KinetiSol Dispersing. Drug Dev Ind Pharm. 2010;36:1064–1078. doi: 10.3109/03639041003652973. [DOI] [PubMed] [Google Scholar]
- 29.Qian F., Wang J., Hartley R. Solution behavior of PVP-VA and HPMC-AS-based amorphous solid dispersions and their bioavailability implications. Pharm Res. 2012;29:2766–2776. doi: 10.1007/s11095-012-0695-7. [DOI] [PubMed] [Google Scholar]