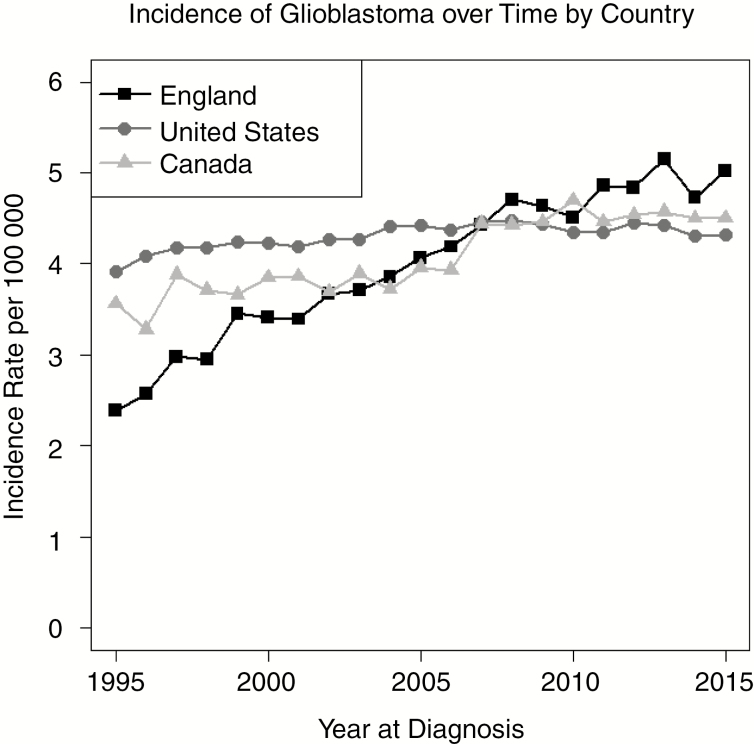
We are commenting on the reported rise in glioblastoma (GB) age-standardized incidence rates across all ages reported by Philips et al.1 To provide comparable incidence rates we show data from England1 complemented by new estimates from Canada and the United States, using data from the Canadian Cancer Registry and the Central Brain Tumor Registry of the United States, respectively. These new incidence rates were calculated for the same time period (1995–2015) and standardized to the same referent population2 as used in estimating the England rates.1 Incidence rates (per 100 000 persons/year) for all 3 countries (International Classification of Diseases for Oncology, third edition, codes 9440/3, 9441/3, and 9442/3) are shown in Fig. 1.
Fig. 1.
Age-standardized incidence rates (per 100 000) for GBs diagnosed between 1995 and 2015 shown by country.
We make the following observations about GB rates by country specifically:
An increase in GB rates is apparent in all 3 countries, but the magnitude of that increase and the patterns over time are different.
In 1995, England had a lower incidence rate (2.39 per 100 000) than Canada (3.56 per 100 000) or the US (3.92 per 100 000).
The crude percent changes in rates between 1995 and 2015 in Canada (26.4%) and the US (10.2%) are moderate compared with that of England (110%).
In 2015, all 3 countries had incidence rates quite close to each other (Canada = 4.50, US = 4.32, England = 5.02).
The differences in the magnitude of these rates cannot be explained by differing age structures in the underlying populations, as the same reference population has been used for the US, Canada, and England estimates included here.2 The similarity in the current rates may reflect a convergence of several data-driven factors that have influenced patterns over time. We know that standardized diagnoses and reporting of all brain tumors have been emphasized in the last 30 years, so improvements in the precision of GB classification and coding in surveillance systems is expected.
Major World Health Organization classification changes for brain tumors (2000, 2007, and 20163) now include molecular markers, and improvements in radiology diagnoses have been significant.4 As such we anticipate that misclassification by histology is more likely in the earlier years reported than the later years. For example, a tumor coded “Glioma NOS” in the 1990s may now be coded as a GB using tumor markers which differentiate these categories.
With legislation in 2003 for the US and in 2007 for Canada4 requiring reporting of all primary brain tumors, an emphasis on complete case ascertainment has resulted. For example, changes to cancer registration procedures may now include new data sources for primary brain tumors. A concurrent emphasis on training for coding of brain tumors and increased standardization of coding guidelines (eg, https://seer.cancer.gov/tools/solidtumor/) may also have improved the accuracy of histology and site categories. While these changes may affect primarily the reporting of non-malignant tumors, an increase in the reporting of malignant primary brain tumors has been observed.5 Thus, it is important to note that since 2007, rates have stayed similar in both the US (−3.4%) and Canada (1.4%).
Our conclusion is that the divergent pattern historically between these countries is most likely due to factors related to improved data collection practices in surveillance systems. Given the similarity in 2015 incidence rates for GB tumors in all 3 countries and documented changes in information gathering, the attribution of any environmental factor as an explanation for past incidence rate patterns is premature. Hypothesis-driven epidemiology study designs are needed to address such questions. We agree with Philips et al1 that accurate data for all countries, including documentation of reporting practices,6 are needed as we work toward understanding emerging patterns of brain tumor incidence rates.
Funding
This work was supported with funding from the Brain Canada Foundation through the Canada Brain Research Fund (with the financial support of Health Canada and the Brain Tumour Foundation of Canada). Funding for the Central Brain Tumor Registry of the United States was provided by the Centers for Disease Control and Prevention (CDC) under contract no. 2016-M-9030, the American Brain Tumor Association, The Sontag Foundation, Novocure, Abbvie, the National Cancer Institute (NCI) under contract no. HHSN261201800176P, the Musella Foundation, the National Brain Tumor Society, the Children’s Brain Tumor Foundation, the Zelda Dorin Tetenbaum Memorial Fund, the Uncle Kory Foundation, as well as private and in kind donations. Contents are solely the responsibility of the authors and do not necessarily reflect the official views of the CDC or the NCI. This research was also supported by funds to the Canadian Research Data Centre Network (CRDCN) from the Social Science and Humanities research Council, the Canadian Institute for Health Research, the Canadian Foundation for Innovation, and Statistics Canada. Although the research and analysis are based on data from Statistics Canada, the opinions expressed do not represent the views of Statistics Canada or the CRDCN.
Conflict of interest statement. The authors have no conflict of interest with respect to this work.
Authorship statement. Conceptualization of content, oversight of analysis, writing and interpretation: FGD. Analysis of data and creation of figure: TRS (Canada) and HRG (US). Writing, review, and interpretation of results: QTO, CK, JSB-S.
References
- 1. Philips A, Henshaw DL, Lamburn G, O’Carroll MJ. Brain tumours: rise in glioblastoma multiforme incidence in England 1995-2015 suggests an adverse environmental or lifestyle factor. J Environ Public Health. 2018;2018:7910754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Eurostat. Revision of the European Standard Population—Report of Eurostat’s Task Force—2013 Edition. https://ec.europa.eu/eurostat/en/web/products-manuals-and-guidelines/-/KS-RA-13-028. Accessed February 27, 2019. [Google Scholar]
- 3. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016;131(6):803–820. [DOI] [PubMed] [Google Scholar]
- 4. Davis F, Nagamuthu C, Ross J, Megyesi J. Current status of brain tumor surveillance in Canada and why it matters. J Registry Manag. 2015;42(4):139–145. [PubMed] [Google Scholar]
- 5. Eckstrand A, Shack L, Pham T, Davis F. The impact of hospital discharge linkage on case ascertainment of brain tumours in the Alberta Cancer Registry, 2010–2015. J Registry Manag. 2018;45(3):109–116. [PubMed] [Google Scholar]
- 6. Barnholtz-Sloan JS. Brain and central nervous system tumor statistics: access to accurate data for all countries is critical. Neuro Oncol. 2019;21(3):291–292. [DOI] [PMC free article] [PubMed] [Google Scholar]