Abstract
Background
Many different surgical techniques have been described for the internal fixation of extracapsular hip fractures.
Objectives
To compare different aspects of surgical technique used in operations for internal fixation of extracapsular hip fractures in adults.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (January 2008), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2008, Issue 1), MEDLINE, EMBASE, CINAHL, Current Controlled Trials, orthopaedic journals, conference proceedings and reference lists of articles. Date of last search was January 2008. No language restriction was applied.
Selection criteria
All randomised and quasi‐randomised trials investigating operative techniques used in operations for the treatment of extracapsular hip fractures in adults.
Data collection and analysis
Two review authors independently selected trials, assessed trial quality and extracted data. Wherever appropriate, data were pooled.
Main results
Predominantly older people with trochanteric fractures were treated in the 11 included trials.
One trial (65 participants undergoing fixation with a fixed nail‐plate) found no statistically significant differences between osteotomy versus anatomical reduction. Four trials, involving 465 participants undergoing fixation with a sliding hip screw (SHS), compared osteotomy versus anatomical reduction. Osteotomy was associated with an increased operative blood loss and length of surgery. There were no statistically significant differences for mortality, morbidity or measures of anatomical deformity.
Two trials (138 participants) compared SHS fixation of a trochanteric hip fracture augmented with cement against a standard fixation. There were no reoperations even for the four cases of fixation failure in the cement group. The cement group had significantly better quality of life scores at six months. One trial (200 participants) comparing compression versus no compression of a trochanteric fracture in conjunction with SHS fixation found no significant differences between the two groups. One trial (120 participants) found a tendency to improved outcomes with a hydroxyapatite coated lag screw, but none reached statistical significance. One trial (19 participants) reported reduced temperatures when using a modified reaming method. Another trial (50 participants) found reduced bone marrow intravascular embolism, detected by oesophageal ultrasound, when a Gamma nail was inserted with a distal pressure venting hole in the femur.
Authors' conclusions
There is inadequate evidence to support the use of osteotomy for internal fixation of a trochanteric hip fracture. Similarly, there is insufficient evidence to support the use of the other techniques examined in the trials included in this review.
Plain language summary
Surgical techniques for fixing extracapsular hip fractures in adults
Roughly half of all hip fractures are outside the hip joint capsule (extracapsular proximal femoral fractures). Many of these will be fixed or stabilised using metal implants which are a combination of screws, rods and plates attached to the thigh bone. Various techniques such as the selective removal of bone (osteotomy), the pressing together of bone fragments (compression), the addition of bone cement, and methods for insertion of nails such as reaming, are used during surgery. This review included 11 randomised or quasi‐randomised trials. The majority of the participants were female, usually aged around 80 years. There were seven comparisons but the evidence for each of these was insufficient to draw conclusions. Thus, the review found that there was too little evidence from randomised trials to show which, if any, specific surgical techniques used during operations for extracapsular proximal femoral fractures are better.
Background
Hip fracture is the general term for fracture of the proximal (upper) femur. These fractures can be subdivided into intracapsular fractures (those occurring within or proximal to the attachment of the hip joint capsule to the femur) and extracapsular (those occurring outside or distal to the hip joint capsule). Extracapsular hip fractures are defined as those fractures that occur within the area of bone bounded by the attachment of the hip joint capsule and extending down to a level which is five centimetres below the distal (lower) border of the lesser trochanter. Other terms used to describe these fractures include trochanteric, subtrochanteric, pertrochanteric and intertrochanteric fractures. These terms reflect the proximity of these fractures to the greater and lesser trochanters, which are two bony protuberances (bulges) at the upper end of the femur outside the joint capsule. These fractures can be subdivided into 'stable' and 'unstable' fractures (Evans 1949; Jenson 1980). Stable fractures are two part fractures, whilst unstable fractures are comminuted with more than two parts to the fractures.
In centres with appropriate surgical facilities, most intertrochanteric fractures are treated operatively (Handoll 2008). The most common implant used for internal fixation of these fractures is the sliding hip screw (SHS). This implant consists of a screw which is passed up the femoral neck to the femoral head connected to a plate on the femur. The SHS is equivalent to the Compression, Dynamic, Richards or Ambi hip screws. These are considered 'dynamic' implants as they have the capacity for sliding at the plate/screw junction to allow for collapse at the fracture site.
Fixed nail plates consist of a nail, which is passed up the femoral neck to the femoral head, connected to a plate on the femur. These implants have no capacity for sliding to compensate for collapse at the fracture site and hence are termed 'static' or 'fixed' implants.
The Gamma nail is an intramedullary nail used in the treatment of extracapsular proximal femoral fractures. The implant consists of a sliding lag screw which passes through a short intramedullary nail. The nail is inserted via an entry hole in the greater trochanter and passed distally. Prior to nail insertion the femur has to be reamed to accommodate the nail, with some further reaming for the sliding lag screw.
Many different technical aspects of surgical fixation exist. These include surgical approach to the femur, reduction of the fracture, osteotomy of the femur, reaming of the femur, positioning of the lag screw and compression of the fracture. In addition, there is the use of substances, either inserted at the fracture site or coated on the implant, that are used to enhance the fixation of the fracture. This review update continues to examine only those aspects of surgical fixation of an extracapsular fracture that have been studied within a randomised trial. Trials comparing different implants are considered in other Cochrane reviews of extracapsular hip fractures: extramedullary fixation (Parker 2006b), arthroplasty (Parker 2006a), condylocephalic (e.g. Ender nail) nails (Parker 1998) and cephalocondylic (e.g. Gamma nail) nails (Parker 2008).
Osteotomy of the femur
Prior to fixation of a displaced extracapsular fractures it is routine practice to reduce the fracture before it is fixed. This is generally achieved using traction to the injured limb applied using a fracture table. Either an anatomical or slight over reduction (valgus reduction) is generally used. In addition to fracture reduction, for unstable fractures it has been suggested that an osteotomy around the fracture site alters the fracture configuration to a more stable pattern and thereby reduces the risk of fixation failure. Two different types of osteotomy have been described. Dimon 1967 described a transverse osteotomy at the level of the lesser trochanter: the femur is then displaced medially with the medial cortex of the proximal fragment inserted into the femoral shaft. This is also termed a medial displacement osteotomy. Sarmiento 1970 described a valgus osteotomy, which is an oblique osteotomy from the greater to lesser trochanter. The theoretical benefit of these osteotomies is that they will reduce the degree of collapse that occurs at the fracture site and thereby the risk of fixation failure.
Compression of the fracture
Compression of the fracture site has been advocated as a method of reducing any gap at the fracture surfaces and thus reducing the time it takes for the fracture to heal and the risk of fixation failure.
Reaming of the femur
Reaming of the femur prior to insertion of the lag screw during SHS fixation of proximal femoral fracture is undertaken with a power drill and triple reamer. The reamers are used to create a cavity within the medullar cavity of the bone into which the fixation device can be placed. The friction caused by this will generate heat which may damage the surrounding bone (Eriksson 1984). Calder 1995a described a modification to the reaming technique where the outer cortex is drilled with the reamer set to its minimum length of 60 millimetres. The reamer is then reset as normal and the bone in the femoral neck and head reamed. This process reduces the amount of time the reamer tip is within the femoral head.
For an intramedullary nail, as well as reaming for the lag screw, the proximal femoral medullary cavity needs to be reamed to accommodate the nail. This is generally undertaken with power reamers. One effect of this reaming is that the bone marrow components are forced into the venous circulation. These emboli can be detected within the circulation by transoesophageal ultrasound as they pass through the right ventricle to the pulmonary circulation, where many of them lodge (Christie 1995). The emboli may lead to the complications of fat embolism namely hypoxia, respiratory failure, circulatory failure, mental confusion and in extreme cases cardiac arrest.
Cement augmentation
The fixation of the fracture with an implant may be supplemented by the addition of bone cement. This is a compound, which is injected as a liquid to the spaces around the fractures surfaces. When it sets it bonds the bone surfaces together. Different types of bone cement are used with one of the main differences being whether the cement is slowly reabsorbed by the body by ingrowth of bone or resists being absorbed. One type of absorbable cement is Norian SRS.
Hydroxyapatite coating of the lag screw
The implant or part of the implant may be coated with a substance such as hydroxyapatite. This substance encourages bone growth around the implant and thereby should enhance the fixation and perhaps reduce the risk of fixation failure. A possible adverse effect is that hydroxyapatite coating may make the implant more difficult to remove.
Objectives
To compare the relative effects (operative details, fracture fixation complications, post‐operative complications, anatomical restoration, final outcome measures) of new or modified techniques that have been used for internal fixation of extracapsular hip fractures in adults.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials examining operative techniques or modifications to implants used for the treatment of extracapsular hip fractures. Quasi‐randomised trials and trials in which the treatment allocation was inadequately concealed were considered for inclusion.
Types of participants
Skeletally mature patients with an extracapsular proximal femoral fracture.
Types of interventions
All forms of modification of the surgical technique for the internal fixation of intracapsular fracture compared with treatment with a standard technique (here the control group). Included were methods, including bone substitutes, used to enhance the fixation of the implant within the bone. Systemically‐applied interventions such as the use of bisphosphates were excluded.
Types of outcome measures
All clinically relevant outcome measures as detailed within any of the included studies were considered, including those listed below.
a) Operative details
length of surgery (in minutes)
operative blood loss (in millilitres)
post‐operative blood transfusion (in units)
radiographic screening time (in seconds)
temperature of the femoral head during reaming
extent of bone marrow embolisation as determined by transoesophageal cardiac ultrasound
b) Fracture fixation complications
cut‐out of the implant proximally (penetration of the implant from the proximal femur either into the hip joint or external to the femur).
non‐union of the fracture within the follow‐up period (the definition of non‐union was that used within each individual study).
other surgical complications of fixation (as detailed in each study)
fracture fixation failure rate (sum of the above three)
re‐operation (within the follow‐up period of the study)
superficial wound infection (infection of the wound in which there is no evidence that the infection is deep to the deep fascia layer or extends to the site of the implant)
deep wound infection (infection below the deep fascia layer)
c) Post‐operative complications
pneumonia
deep vein thrombosis
pulmonary embolism
thromboembolic complications (summation of the above two)
any medical complication (as detailed in each individual study)
length of hospital stay (in days)
d) Anatomical restoration
shortening (> 2 cm)
varus deformity of the femoral neck (as detailed in each individual study)
external rotation deformity ( > 20 degrees)
e) Final outcome measures
mortality (within the follow‐up period of the study)
pain (persistent pain at the final follow‐up assessment)
failure to return to living at home
failure to regain mobility
functional activities of daily living
composite function and hip scores
quality of life scores
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (March 2008), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2008, Issue 1), MEDLINE (1966 to January Week 4 2008), EMBASE (1988 to 2008 Week 4) and CINAHL ‐ Cumulative Index to Nursing & Allied Health Literature (1982 to December Week 1 2007). We searched Current Controlled Trials (accessed January 2008) for ongoing and recently completed trials. No language or publication restriction was applied.
The Cochrane Library (Wiley InterScience), MEDLINE (OVID‐WEB), EMBASE (OVID‐WEB) and CINAHL (OVID‐WEB) search strategies are shown in Appendix 1. The MEDLINE search was combined with all three stages of the optimal trial search strategy (Higgins 2006).
Searching other resources
We searched reference lists of articles and our own reference databases. We checked the findings from handsearches of the British Volume of the Journal of Bone and Joint Surgery supplements (1996 to 2006) and abstracts of the American Orthopaedic Trauma Association annual meetings (1996 to 2007) and American Academy of Orthopaedic Surgeons annual meeting (2004 to 2007). We also included handsearch results from the final programmes of SICOT (1996 & 1999) and SICOT/SIROT (2003), EFFORT (2007) and the British Orthopaedic Association Congress (2000, 2001, 2002, 2003, 2005 and 2006). We scrutinised weekly downloads of "Fracture" articles in new issues of 15 journals (Acta Orthop Scand; Am J Orthop; Arch Orthop Trauma Surg; Clin J Sport Med; Clin Orthop; Foot Ankle Int; Injury; J Am Acad Orthop Surg; J Arthroplasty; J Bone Joint Surg Am; J Bone Joint Surg Br; J Foot Ankle Surg; J Orthop Trauma; J Trauma; Orthopedics) from AMEDEO.
Data collection and analysis
Selection of studies
Two review authors independently assessed potentially eligible trials for inclusion. Any disagreement was resolved by discussion.
Data extraction and management
Data for the outcomes listed above were independently extracted by two review authors and any differences resolved by discussion. Where necessary and practical, we contacted trialists for additional data and clarification of trial methods and results.
Assessment of risk of bias in included studies
In this review, risk of bias is implicitly assessed in terms of methodological quality. Each trial was assessed independently, without masking of authors or source, for its quality of methodology by two review authors. All differences were resolved by discussion. In total, 11 aspects of methodology were rated (seeTable 6). Summation of the scores for individual items was discontinued in the update published in Issue 2, 2009.
1. Methodological quality assessment scheme.
| Items | Scores |
| 1. Concealment of allocation | Trials with clear concealment of allocation (e.g. numbered sealed opaque envelopes drawn consecutively) were coded as A and scored 3. Those in which there was a possible chance of disclosure assignment were coded as B and scored 2. Those in which allocation concealment is not stated or unclear were coded as B and scored 1. Where allocation concealment was clearly not concealed such as trials using quasi‐randomisation (e.g. even or odd date of birth), they were coded as C and scored 0. |
| 2. Inclusion and exclusion criteria | Were the inclusion and exclusion criteria clearly defined? Score 1 if text states type of fracture and which patients were included and excluded. Otherwise score 0. |
| 3. Outcomes for participants who withdrew or were excluded | Were the outcomes of participants who withdrew or excluded after allocation described and included in an intention‐to‐treat analysis? Score 1 if yes or text states that no withdrawals occurred. Otherwise score 0. |
| 4. Description of treatment and control groups | Were the treatment and control groups adequately described at entry? Score 1 if at least four admission details given (e.g. age, sex, mobility, function score, mental test score, fracture type) with no clinically important differences between groups. Otherwise score 0. |
| 5. Description of the operative technique | Was the operative technique for both groups adequately described? Score 1 if yes. Otherwise score 0. |
| 6. Surgical experience | Did the surgeons have prior experience of the operations they performed in the trial, prior to commencement of the trial? Score 1 if text states there was an introductory period or that surgeons were experienced. Otherwise score 0. |
| 7. Identical care programmes | Were the care programmes other than trial options identical? Score 1 if text states they were. Otherwise score 0. |
| 8. Definition of outcome measures | Were the outcome measures clearly defined in the text with a definition of any ambiguous terms encountered? Score 1 if yes. Otherwise score 0. |
| 9. Blinding of outcome assessors | Were the outcome assessors blind to assignment status? Score 1 if assessors of anatomical restoration, pain and function at follow up were blinded to treatment outcome. Otherwise score 0. |
| 10. Timing of outcome measures | Was the timing of outcome measures appropriate? A minimum of six months follow up for all surviving trial participants. Score 1 if yes. Otherwise score 0. |
| 11. Loss to follow up | Was loss to follow up reported and if so were less than 5% of trial participants lost to follow up? Score 1 if yes. Otherwise score 0. |
Assessment of heterogeneity
Heterogeneity between comparable trials was assessed by visual inspection of the forest plot, and consideration of the standard chi² test and I² statistic (Higgins 2003).
Data synthesis
For each study, risk ratios (RR) and 95% confidence intervals (CI) were calculated for dichotomous outcomes; and mean differences and 95% confidence intervals for continuous outcomes. Where appropriate, data were pooled using the fixed‐effect model using 95% confidence intervals (CI). Where there was substantial clinical heterogeneity, we additionally planned to look at the results using the random‐effects model.
Results
Description of studies
In all, 16 trials were identified of which 11 are included (see the Characteristics of included studies for details) and five are excluded (see the Characteristics of excluded studies for reasons for exclusion). Three new trials were included in this update, and formed the basis of two new comparisons. Two of these (Mattsson 2004; Mattsson 2005) evaluated the use of calcium‐phosphate cement for fractures fixed with the sliding hip screw (SHS). The remaining trial (Moroni 2004, formerly excluded as Moroni 2002) tested the use of hydroxyapatite coating of the lag screw for SHS fixation.
Three other newly identified studies were excluded (Acharya 2003;Alobaid 2004;Moroni 2007). We revised the reasons for excluding Bong 1981, which compared two types of osteotomy with conservative treatment and appears in another review (Handoll 2008).
The study populations were predominantly female with the reported mean age being 80 years or over in nine trials. All participants in Calder 1995 were female and over 60 years old. Exceptionally, more participants were male with an average age of 58 years in Kumar 1996, a study conducted in India. The seven comparisons covered by the included trials are summarised below.
Osteotomy with anatomical reduction using a fixed nail plate
One study of 65 participants (Hubbard 1980) compared osteotomy with anatomical reduction in conjunction with a fixed nail plate.
Osteotomy with anatomical reduction using a SHS
Four studies with a total of 465 participants (Clark 1990; Desjardins 1993; Gargan 1994, Kumar 1996) compared osteotomy with anatomical reduction in conjunction with SHS fixation.
Bone cement augmentation at the fracture site
Two studies involving a total of 138 participants (Mattsson 2004 and Mattsson 2005) studied the augmentation of a SHS fixation with bone cement.
Compression of the fracture
Sernbo 1994 tested the use of compression in 200 participants treated with a SHS fixation. Compression was applied using a compression screw inserted during the surgery.
Hydroxyapatite coating of the lag screw
One study of 120 participants (Moroni 2004) tested the use of a lag screw coated with hydroxyapatite for SHS fixation against a control group in which a standard lag screw was used.
Modified reaming method
Calder 1995 tested the application of a modified reaming method versus the usual method in 19 participants. For this study the outer cortex of the femur is reamed first prior to reaming of the femoral head and neck for the lag screw.
Use of a venting hole when reaming
One study (Roder 1995), published in German, compared reaming of the femur for intramedullary nail insertion with versus without a venting hole in 50 participants.
Risk of bias in included studies
Based on our already established methods, we evaluated various aspects of methodological quality of the included trials rather than risk of bias. However, as well as presenting the results of our assessment, we highlight two key sources of bias associated with lack of blinding. These are selection bias from the failure to conceal allocation, and detection bias from the failure to blind outcome assessment.
Some details of the method of randomisation were given in 7 of the 11 studies. Moroni 2004 used numbered sealed envelopes containing the randomisation from a computer generated list. Gargan 1994 used sealed envelopes with the type of operation being determined from a table of random numbers. Mattsson 2004, Mattsson 2005 and Sernbo 1994 used sealed envelopes. Desjardins 1993 and Hubbard 1980 used a computer generated list. Clark 1990 was quasi‐randomised and used the patient's date of birth. No method was stated by Calder 1995, Kumar 1996 or Roder 1995. We considered the risk of selection bias associated with the failure to conceal allocation at randomisation was high in the only quasi‐randomised trial (Clark 1990), low in Moroni 2004 where an independent person opened the envelopes, and unclear in the remaining trials.
There was a risk of detection bias, particularly for clinician‐rated outcomes, in all the included trials given that there was no assessor blinding.
The results of the methodological assessment for individual trials are given below. SeeTable 6 for the descriptions of the criteria for items 1 to 11.
1 2 3 4 5 6 7 8 9 10 11 Trial 1 0 1 0 1 1 1 1 0 0 1 Calder 1995 0 0 0 0 1 0 1 1 0 0 1 Clark 1990 2 1 0 1 1 0 0 0 0 1 0 Desjardins 1993 2 1 0 1 0 0 0 0 0 0 1 Gargan 1994 2 0 0 0 1 0 1 0 0 0 1 Hubbard 1980 1 1 0 0 0 0 0 0 0 1 0 Kumar 1996 2 1 0 0 1 0 1 1 0 1 1 Mattsson 2004 2 1 0 1 1 1 1 1 0 1 0 Mattsson 2005 3 1 0 1 1 1 1 1 0 1 1 Moroni 2004 1 1 0 0 1 1 1 1 0 0 1 Roder 1995 2 0 0 1 1 1 0 0 0 0 1 Sernbo 1994
Effects of interventions
Where appropriate, data from each trial are presented in the analyses and by treatment comparison in the following section. Further unpublished details from the authors of each study would be welcomed by the reviewers.
Osteotomy (treatment group) versus anatomical reduction (control group) for fixed nail plate
One study (Hubbard 1980, 65 patients), all with unstable trochanteric fractures, was included. Three patients who were considered unfit for surgery were withdrawn from the trial.
a) Operative details
Hubbard 1980 reported only that the operating procedure for osteotomy took "no longer" and caused "no more bleeding" than for the control group".
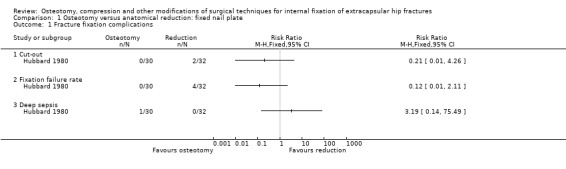
b) Fracture fixation complications (Analysis 1.1)
There was no statistically significant differences between the two groups in the fixation failure rate (0/30 versus 4/32; risk ratio (RR) 0.12; 95% confidence interval (CI) 0.01 to 2.11). Of the four cases of fixation failure in the anatomical reduction group, there were two cases of cut‐out and two cases of bending and breakage of the implant requiring reoperation. The only fracture fixation complication reported for the osteotomy group was a deep wound infection.
c) Post‐operative complications
These outcomes were not reported.
d) Anatomical restoration
These outcomes were not reported.
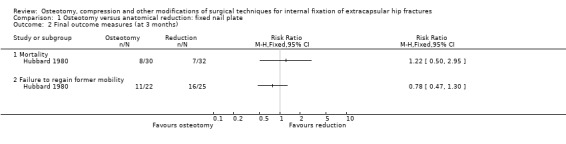
e) Final outcome measures (Analysis 1.2)
There was no significant difference in mortality (8/32 versus 7/32; RR 1.22, 95% CI 0.50 to 2.95) or the number of participants who were unable to regain their pre‐fracture mobility (11/22 versus 16/25; RR 0.78, 95% CI 0.47 to 1.30).
Sliding hip screw (SHS) using an osteotomy (treatment group) or anatomical reduction (control group)
Four studies (Clark 1990; Desjardins 1993; Gargan 1994; Kumar 1996) with a total of 465 patients were identified and included in the review.
a) Operative details
Data from Clark 1990 and Desjardins 1993 for length of surgery are presented in the analyses (Analysis 2.1). In including the data from Clark 1990, we have assumed that standard deviations were provided in their paper. Pooled data for length of surgery were heterogeneous with Clark 1990 finding no significant difference (56 versus 53 minutes) between the two groups, whereas Desjardins 1993 found a significantly increased operation time for osteotomy of 103 versus 83 minutes. Both Gargan 1994 and Kumar 1996 found similarly increased operative times for osteotomy group (respectively: 70 versus 47 minutes; 180 versus 120 minutes).
2.1. Analysis.
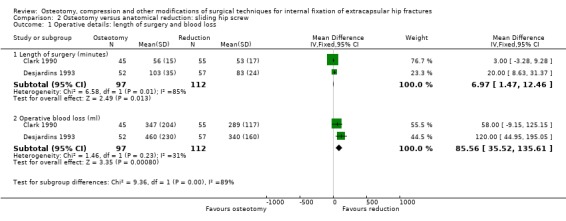
Comparison 2 Osteotomy versus anatomical reduction: sliding hip screw, Outcome 1 Operative details: length of surgery and blood loss.
Pooled data for operative blood loss showed a significantly increased mean operative blood loss in the osteotomy group (mean difference (MD) 85.56 ml, 95% CI 35.52 to 135.61 ml). Kumar 1996 reported, without statistical analysis, an increased mean blood loss for osteotomy (500 ml versus 300 ml). Gargan 1994 found that, on average, 2.0 units of blood were transfused after osteotomy compared with 1.6 units after anatomic reduction. These findings of greater blood loss with osteotomy are consistent with the more invasive nature of the operation.
No study reported radiographic screening time.
b) Fracture fixation complications
From the limited results available, there was no significant differences in the outcome measures of cut‐out, non‐union (this also includes "delayed union" in Desjardins 1993), fixation failure rate or reoperation rate (seeAnalysis 2.2). Gargan 1994 did not provide separate data by group for the 12 cases of fixation failure: in nine cases, the screw had penetrated the joint; in two cases, it had cut‐out of the neck; and in one case, the plate had pulled off the femoral shaft. Out of 110 patients followed up in Kumar 1996, there were 12 cases of fixation failure. Overall, there was a tendency to an increased overall fixation failure rate after osteotomy (20/190 versus 16/229; RR 1.51, 95% CI 0.81 to 2.83).
2.2. Analysis.
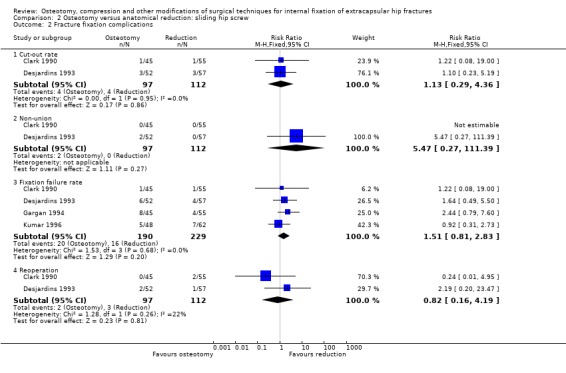
Comparison 2 Osteotomy versus anatomical reduction: sliding hip screw, Outcome 2 Fracture fixation complications.
Three deep wound infections were reported: all were after anatomic reduction (Analysis 2.3).
2.3. Analysis.
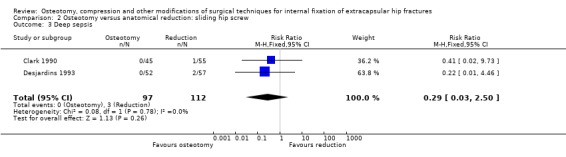
Comparison 2 Osteotomy versus anatomical reduction: sliding hip screw, Outcome 3 Deep sepsis.
c) Post‐operative complications
There was no mention of these in either Gargan 1994 or Kumar 1996 with only limited data presented in the other two reported studies (Clark 1990; Desjardins 1993). Overall there was no evidence of a difference in the incidence of complications between the two groups (30/97 versus 36/112; RR 0.98, 95 % CI 0.66 to 1.45). Only Desjardins 1993 gave some details of these complications from which it could be seen that the incidence of thromboembolic complications and pressure sores was the same in both groups.
Clark 1990 reported a significant increase in hospital stay in the osteotomy group (31 days versus 21 days in the anatomical reduction group). This was not the case when the data (we have assumed that standard deviations were provided in their paper) were included in the analysis. Analysis 2.5 also shows data from Desjardins 1993, who found no significant difference in the length of hospital stay between groups.
2.5. Analysis.

Comparison 2 Osteotomy versus anatomical reduction: sliding hip screw, Outcome 5 Length of hospital stay (days).
d) Anatomical restoration
Only Clark 1990 reported adequately on leg shortening (defined as more than 1 cm) and external rotational deformity (more than 10 degrees). Neither of these nor the pooled results for varus deformity showed a significant difference between the two groups (Analysis 2.6).
2.6. Analysis.
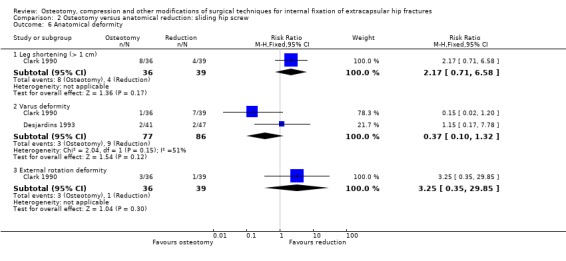
Comparison 2 Osteotomy versus anatomical reduction: sliding hip screw, Outcome 6 Anatomical deformity.
e) Final outcome measures (Analysis 2.7)
Pooled data for mortality from three studies (Clark 1990; Desjardins 1993; Gargan 1994) showed no significant difference between the treatment groups (25/142 versus 32/167; RR 0.92, 95% CI 0.57 to 1.47). Kumar 1996 reported that 10 patients died post‐operatively within six weeks but did not provide separate data by treatment group.
No study provided data for pain at follow up although Kumar 1996 reported that there was no difference in pain at follow up between the two treatment groups. Both Clark 1990 and Desjardins 1993 found no significant difference in the number of patients who were unable to return to their former residence (24/80 versus 19/87; RR 1.38, 95% CI 0.83 to 2.28) or regain their former mobility (42/77 versus 44/84; RR 1.04, 95% CI 0.78 to 1.39). Kumar 1996 stated there was no difference between the two groups in mobility, limping or walking distance at follow up.
Bone cement augmentation at the fracture site
Two studies (Mattsson 2004; Mattsson 2005) compared SHS fixation augmented with an absorbable calcium phosphate bone cement, versus standard SHS fixation in 138 patients with an unstable trochanteric fracture. Very little data on clinical outcomes were available from Mattsson 2004.
a) Operative details
Mattsson 2005 reported the difference in the mean length of surgery (68.7 versus 56.7 minutes) between the two groups was not statistically significant. Conversely, the difference in the mean blood loss (405 ml versus 281 ml) was significantly in favour of the control group (reported P < 0.05).
b) Fracture fixation complications (Analysis 3.1)
There were no cases of cut‐out in Mattsson 2005. Mattsson 2005 reported two cases in the cement group where fracture union was delayed more than six months (both fractures united subsequently). In addition, the plate became detached from the femur in two cases in the cement group. No treatment was required. There were no reoperations in either Mattsson 2004 or Mattsson 2005. Mattsson 2004 reported no cases of wound infection.
c) Post‐operative complications
There was no reporting of medical complications in either trial. Mattsson 2005 found no significant difference between the two groups in the length of hospital stay (Analysis 3.3: MD 0.50 days, 95% CI ‐0.84 to 1.84 days).
3.3. Analysis.
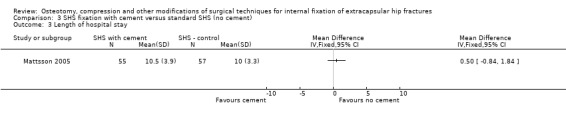
Comparison 3 SHS fixation with cement versus standard SHS (no cement), Outcome 3 Length of hospital stay.
d) Anatomical restoration
Mattsson 2004 reported a statistically significant difference (P < 0.02) in favour of augmentation in the mean varus angulation at the fracture site at six months (5.89 versus 10.57 degrees). Mattsson 2004 also measured movement or translation of the fracture site with tantalum markers inserted into the bone at the time of surgery: these data are not presented in the review analyses. At six months the total translation was significantly less in the cement group (7.77 mm versus 13.24 mm; P = 0.02). Mattsson 2005 reported the mean sliding distance of the lag screw was statistically significantly lower in the cement group (13.5 mm versus 15.9 mm). The clinical consequences of these outcomes were not reported in either trial.
e) Final outcome measures
These outcomes were only reported in Mattsson 2005 who found no significant difference between the groups in mortality (Analysis 3.4: 3/55 versus 2/57; RR 1.55, 95% CI 0.27 to 8.95). There was no statistically significant differences in global pain visual analogue scale scores at six months (Analysis 3.5). Although there was a statistically significant reduced level of pain during walking in the cement group at six months, the clinical significance of this result is not clear (Analysis 3.5: MD ‐5.00 mm, 95% CI ‐9.70 to ‐0.30 mm). No statistically significant differences were found for activities of daily living at six months. However, Mattsson 2005 reported improved abilities at six weeks in the cement group for rising from the chair (P < 0.003), getting off the toilet (P < 0.05) and climbing a step (P < 0.03). Mattsson 2005 reported, without providing full data, statistically significantly better quality of life at six months in the cement group as measured by the SF‐36 score: SF‐36 scores for general health (80.9 versus 66.3; reported P < 0.02); physical functioning domain (42.1 versus 28.0; P < 0.04); physical health domain (30.7 versus 22.8; not significant (NS)); role emotional domain (58.6 versus 52.3; NS); social functioning domain (83.7 versus 64.2; P < 0.002); vitality domain (62.9 versus 51.3; P < 0.02); mental health domain (77.9 versus 67.0; P < 0.03). There was no statistically significant difference in the abductor strength between the two groups at six months (Analysis 3.6).
3.4. Analysis.
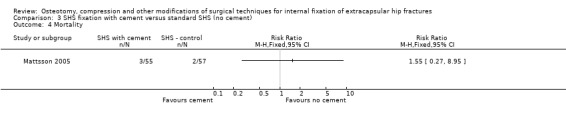
Comparison 3 SHS fixation with cement versus standard SHS (no cement), Outcome 4 Mortality.
3.5. Analysis.
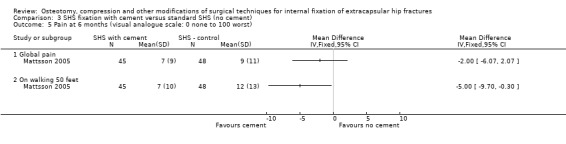
Comparison 3 SHS fixation with cement versus standard SHS (no cement), Outcome 5 Pain at 6 months (visual analogue scale: 0 none to 100 worst).
3.6. Analysis.
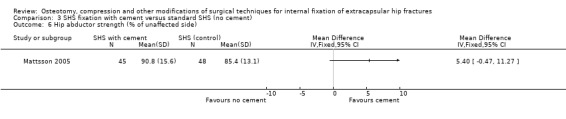
Comparison 3 SHS fixation with cement versus standard SHS (no cement), Outcome 6 Hip abductor strength (% of unaffected side).
Compression of a trochanteric fracture in conjunction with a SHS
One study of 200 participants was included (Sernbo 1994).
a) Operative details
The study demonstrated no difference in operative times or operative blood loss between the two techniques (Analysis 4.1).
4.1. Analysis.
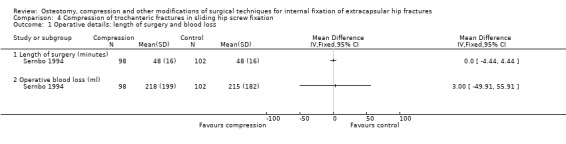
Comparison 4 Compression of trochanteric fractures in sliding hip screw fixation, Outcome 1 Operative details: length of surgery and blood loss.
b) Fracture fixation complications
There was no significant difference in non‐union, the only outcome measure in this category reported (Analysis 4.2).
4.2. Analysis.
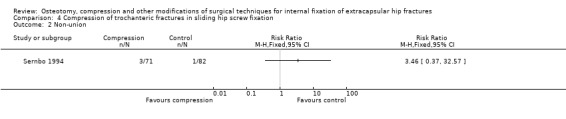
Comparison 4 Compression of trochanteric fractures in sliding hip screw fixation, Outcome 2 Non‐union.
c) Post‐operative complications
There was no report of these outcomes.
d) Anatomical restoration
Varus angulation of the fracture by more than 10 degrees was more frequent but not statistically significantly so after compression (Analysis 4.3: 6/71 versus 1/82; RR 6.93, 95% CI 0.85 to 56.19).
4.3. Analysis.
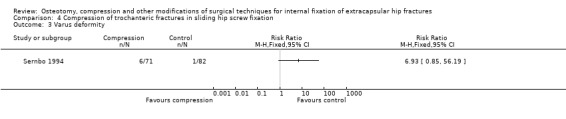
Comparison 4 Compression of trochanteric fractures in sliding hip screw fixation, Outcome 3 Varus deformity.
e) Final outcome measures
There was no report of these outcomes.
Hydroxyapatite coating of the lag screw
One study (Moroni 2004) of 120 participants was included.
a) Operative details
There was no report of these outcomes.
b) Fracture fixation complications
No cut‐out or reoperations occurred in the coated screw group compared with four and three respectively for the uncoated group. However, the differences between the two groups in these outcomes were not statistically significant (Analysis 5.1: cut‐out, RR 0.11, 95%CI 0.01 to 2.02; reoperation, RR 0.14, 95% CI 0.01 to 2.71).
5.1. Analysis.
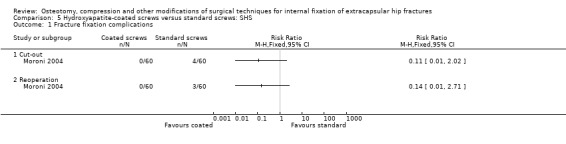
Comparison 5 Hydroxyapatite‐coated screws versus standard screws: SHS, Outcome 1 Fracture fixation complications.
c) Post‐operative complications
There was no report of these outcomes.
d) Anatomical restoration
Clinical deformity was not reported. However, there was a statistically significant difference between the two groups in mean femoral neck angle at six months (133 degrees versus 127 degrees; P = 0.003).
e) Final outcome measures
There was no significant difference between the two groups in six months mortality (Analysis 5.2: 4/65 versus 6/68; RR 0.70, 95% CI 0.21 to 2.36). At six months, both the Harris hip score and the SF‐36 scores were better in the coated screw group but the differences were not statistically significant for both outcome measures (Analysis 5.3).
5.2. Analysis.
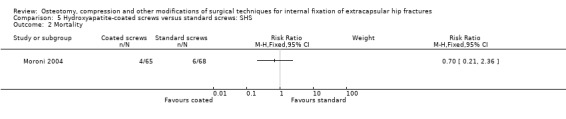
Comparison 5 Hydroxyapatite‐coated screws versus standard screws: SHS, Outcome 2 Mortality.
5.3. Analysis.
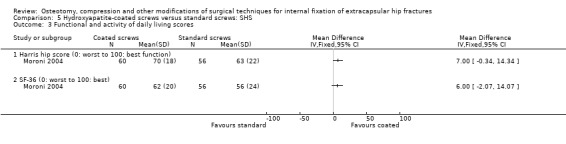
Comparison 5 Hydroxyapatite‐coated screws versus standard screws: SHS, Outcome 3 Functional and activity of daily living scores.
Reaming of the femur for SHS fixation using a modified reaming method or a standard method
The only study identified (Calder 1995) did not record data for any of the clinical outcome measures sought. The only outcome reported was the temperature within the femoral head. There was no statistically significant different in the mean peak temperature recorded in the two groups (modified reamer: n = 10; mean 46.3 degrees, standard deviation (SD) 8.4 versus standard reamer: n = 9; mean 51.9 degrees, standard deviation 3.3). However, the difference in the time (5.7 versus 17.4 seconds) the temperature remained above 44 degrees centigrade was reported to be statistically significant (P < 0.05) between methods.
Provision of a distal femoral venting hole to reduce the risk of bone marrow embolisation during reaming
Roder 1995 recorded the degree of bone marrow embolisation, as measured by transoesophageal oesophageal ultrasound, during reaming and insertion of a Gamma nail with or without a femoral venting hole in 50 patients. A 4.5 millimetre vent hole was drilled in the lateral femoral cortex approximately 25 centimetres distal to the tip of the greater trochanter before opening the bone marrow cavity in 25 Gamma nail patients. The amount of embolisation was graded, in a semi‐quantitative way, into four groups from none (grade 0) through to heavy (grade three). Results of observations made during operations were presented by intervention group rather than by individual patients. No patient of the 25 Gamma nail patients with a vent hole had grade three embolisation but grade two embolisation was observed during reaming for 25 out of 575 observations (4.3%). For the 25 patients treated with the Gamma nail without a vent hole, grade three embolisation was observed for 365 out of 575 observations (63.5%) and grade two embolisation in 74 out of 575 observations (12.9%). No other outcomes were reported.
Discussion
This review involves a mixed collection of studies testing various aspects of surgical fixation. It reports on the comparisons that have been evaluated in randomised or quasi‐randomised controlled clinical trials that we have identified so far. It can be viewed as a 'work in progress', and we will continue to assess and report on new trials that arise in this area. The relevance of some included trials to current practice can and should be questioned. An example is those trials using the fixed nail plate, which is an inferior implant to sliding hip screw (Parker 2006b). Overall, the available evidence from these small trials, with only modest methodological quality or worse, is limited and thus only tentative conclusions can be drawn for each of the seven comparisons.
Fixed nail plate using an osteotomy (treatment group) or anatomical reduction (control group)
Osteotomy of the proximal femur for an unstable trochanteric fracture was originally described with the use of a fixed nail plate. The theory was that collapse at the fracture site would be reduced as bone to bone contact was restored medially. This would reduce the risk of the implant penetrating through the femoral head into the joint. The one included trial comparing osteotomy with anatomical reduction for a fixed nail plate presented only limited results for a small number of patients. While none of the differences between the two groups for fracture fixation complications, mortality and mobility were statistically significant, all four cases of fixation failure occurred in the anatomical reduction group. An osteotomy may therefore be appropriate if a fixed nail plate is used to fix an unstable trochanteric fracture. As noted above, physicians should however be aware that a fixed nail plate may not be the choice of implant for this type of fracture (Parker 2006b).
Sliding hip screw (SHS) using an osteotomy (treatment group) or anatomical reduction (control group)
The dynamic nature of the SHS, when used for trochanteric fractures, allows for collapse at the fracture site. Thus theoretically, this reduces the possible benefits of osteotomy. Osteotomy appears to have no beneficial effect on reducing the risk of implant cut‐out or the overall fixation failure rate. Gargan 1994 observed that the incidence of fixation failure within the osteotomy group was reduced when a short barrel SHS was used; they reported that they had only one failure out of 11 osteotomy cases after the short barrel plate was introduced as opposed to seven out of 34 prior to this.
As would be expected, the addition of osteotomy as part of the surgical procedure increased the length of surgery and operative blood loss. Few data were presented on the incidence of post‐operative complications but overall there was no significant difference in complications between groups. Neither was there any significant difference for mortality or morbidity. Nor was there for measures of anatomical deformity. However, the increased tendency for leg shortening with osteotomy found in Clark 1990 is consistent with the results from theoretical studies.
Bone cement augmentation at the fracture site
The limited number of patients and incomplete recording and reporting of outcome in the two trials mean that no definite conclusions can be made. Movement at the fracture site appeared less in the cement augmented group as demonstrated by the reduced translation at the fracture site and slide of the lag screw within the barrel. The clinical significance of this difference was not demonstrated. Of concern were the two cases of delayed union and the two cases of detachment of the plate from the femur in the cement augmented group of Mattsson 2005. In addition, removal of the implant when cement is used may be more difficult should a reoperation be required. The favourable results for cement augmentation in terms of pain, earlier recovery of basic activities of living at six weeks, and quality of life at six months also need confirmation. In all, further good quality randomised trials with larger number of patients are required. Blinding of some outcome assessors and participants should also be possible.
Compression of a trochanteric fracture in conjunction with a SHS
The one study identified indicated that compression of a trochanteric fracture internally fixed with a SHS may offer no benefit and may increase the risk of varus angulation of the fracture.
Hydroxyapatite coating of the lag screw
The one study identified on this topic suggested that coating the lag screw with hydroxyapatite reduced the occurrence of cut‐out of the femur and improved the function at six months. However, these findings were not statistically significant and thus no definite conclusions should be drawn. Removal of the screws that are hydroxyapatite coated, should it be required subsequently, may be more difficult and this was not discussed in this study. Given that the lead investigator of this study has conducted several studies evaluating hydroxyapatite‐coated screws in other fractures that show promising results also, it is important (particularly for reasons of applicability) that further trials are carried out by other investigators.
Reaming of the femur for SHS fixation using a modified reaming method
The data presented on this small study indicated that the modified reaming method reduced the temperature generated within the femoral head. However there was no measurement of clinical outcomes, even those which may be directly affected by the high temperatures within the femoral head such as non‐union or avascular necrosis. Thus, the clinical relevance of this is open to question.
The provision of a distal femoral venting hole during reaming for Gamma nail fixation
The data presented for 50 patients undergoing Gamma nail fixation indicated that vascular embolisation of bone marrow can be reduced by drilling a vent hole in the distal femoral cortex. However, as there were no measures of clinical outcome the clinical relevance of this is open to question. Furthermore, given that one of the problems of Gamma nail fixation is fracture of the femur below the implant, the vent hole would weaken the bone in this area and the extra risk of fracture would need to be assessed.
Authors' conclusions
Implications for practice.
There is no evidence available to support the routine use of either osteotomy or intra‐operative fracture compression when a SHS is used for the internal fixation of a trochanteric proximal femoral fracture.
Insufficient evidence exists to support use of bone cement augmentation, hydroxyapatite coating of the lag screw, the reaming of the femur using a modified technique for SHS fixation or the use of a vent hole in the femur for Gamma nail fixation.
Implications for research.
The evidence base from these small trials often with flawed methodology is insufficient to draw conclusions of the effects of the different techniques tested so far. Any new or modified technique should be tested in good quality randomised trials against the best standard procedure, collecting clinically relevant outcomes. Many other aspects of the surgical fixation of extracapsular fracture have not been studied within randomised trials, but it is important to establish beforehand that any proposed change in technique would have sufficient impact on clinical outcome to merit further research.
What's new
| Date | Event | Description |
|---|---|---|
| 18 February 2009 | New search has been performed | For the fourth review update (Issue 2, 2009), the following changes were made: 1. Review title changed from "Osteotomy, compression and reaming techniques for internal fixation of extracapsular hip fractures"; 2. Search updated (January 2008); 3. Three new studies (Mattsson 2004; Mattsson 2005; Moroni 2004), generating two new comparisons, were included; 4. Three newly identified studies (Acharya 2003; Alobaid 2004; Moroni 2007) were excluded; 5. Additional reference (Pedlow 1991) found for included trial (Desjardins 1993); 6. Updated methods, including the removal of overall quality assessment scores, and formatting. Though the conclusions were adjusted to accommodate the two new comparisons, the finding of insufficient evidence was unchanged. |
| 18 February 2009 | New citation required but conclusions have not changed | The fourth review update also saw a change in authorship (see 'Contributions of authors'). |
History
Protocol first published: Issue 4, 1997 Review first published: Issue 3, 1998
| Date | Event | Description |
|---|---|---|
| 20 October 2008 | Amended | Converted to new review format |
| 28 February 2001 | New search has been performed | In the third update (Issue 3, 2001), the search for trials was updated to February 2001, and no new trials for inclusion were identified. One identified study, Papanikolaou 1999, was excluded. The conclusions of the review were unchanged. For details of previous updates, please see 'Notes'. |
Notes
Previous titles no longer in use: 1. Extracapsular hip fractures: Surgical techniques 2. Osteotomy, compression and reaming techniques for internal fixation of extracapsular hip fractures
First update (Issue 2, 1999). 1. Roder 1995 included.
Second update (Issue 2, 2000). 1. Kumar 1996 included and Papanikolaou 1999 excluded. 2. Risk ratios were presented instead of odds ratios. Conclusions of the review unchanged.
Acknowledgements
We thank our two co‐authors (G Tripuraneni and J McGreggor‐Riley) who were involved with the first two versions of this review. We thank Dr Joanne Elliott for her help with the search for trials and Mrs Lindsey Elstub and Ms Amy Kavanagh for editorial support.
We would also like to thank the following for useful comments from editorial and external review: Dr Vicki Livingstone, Dr Janet Wale, Assoc Prof Leif Ceder and Prof Rajan Madhok.
Appendices
Appendix 1. Search strategies
The Cochrane Library (Wiley InterScience)
#1MeSH descriptor Hip Fractures explode all trees #2((hip* or pertrochant* or intertrochant* or trochanteric or subtrochanteric or extracapsular* or ((femur* or femoral*) NEAR/3 (neck or proximal))) NEAR/4 fracture*):ti,ab,kw #3(#1 OR #2) #4MeSH descriptor Orthopedics, this term only #5MeSH descriptor Fracture Fixation, Internal explode all trees #6MeSH descriptor Internal Fixators, this term only #7MeSH descriptor Osteotomy, this term only #8MeSH descriptor Bone Nails, this term only #9MeSH descriptor Bone Screws, this term only #10MeSH descriptor Bone Plates, this term only #11(#4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10) #12(#3 AND #11)
MEDLINE (OVID‐WEB)
1 exp Femoral Fractures/ 2 ((hip$ or pertrochant$ or intertrochant$ or trochanteric or subtrochanteric or extracapsular$ or ((femur$ or femoral$) adj3 (neck or proximal))) adj4 fracture$).tw. 3 or/1‐2 4 Surgery/ or Osteotomy/ or Internal Fixators/ or Bone Screws/ or exp Fracture Fixation, Internal/ or Bone Plates/ or Bone Nails/ 5 (osteotom$ or ream$ or compression or pin$1 or nail$ or screw$1 or plate$1).tw. 6 or/4‐5 7 and/3,6
EMBASE (OVID‐WEB)
1 exp Hip Fracture/ 2 ((hip$ or pertrochant$ or intertrochant$ or trochanteric or subtrochanteric or extracapsular$ or ((femur$ or femoral$) adj3 (neck or proximal))) adj4 fracture$).tw. 3 or/1‐2 4 Fracture Treatment/ or Hip Surgery/ or Femur Intertrochanteric Osteotomy/ or Femur Osteotomy/ or Hip Osteotomy/ or exp Fracture Fixation/ or Bone Screw/ or Bone Plate/ or Bone Nail/ or ender Nail/ or Interlocking Nail/ or Osteosynthesis Material/ 5 (osteotom$ or ream$ or compression or pin$1 or nail$ or screw$1 or plate$1).tw. 6 or/4‐5 7 and/3,6 8 Clinical trial/ 9 Randomized controlled trial/ 10 Randomization/ 11 Single blind procedure/ 12 Double blind procedure/ 13 Crossover procedure/ 14 Placebo/ 15 Randomi?ed controlled trial$.tw. 16 Rct.tw. 17 Random allocation.tw. 18 Randomly allocated.tw. 19 Allocated randomly.tw. 20 (allocated adj2 random).tw. 21 Single blind$.tw. 22 Double blind$.tw. 23 ((treble or triple) adj blind$).tw. 24 Placebo$.tw. 25 Prospective study/ 26 or/8‐25 27 Case study/ 28 Case report.tw. 29 Abstract report/ or letter/ 30 or/27‐29 31 26 not 30 32 limit 31 to human 33 and/7,32
CINAHL (OVID‐WEB)
1 Hip Fractures/ 2 ((hip$ or pertrochant$ or intertrochant$ or trochanteric or subtrochanteric or extracapsular$ or ((femur$ or femoral$) adj3 (neck or proximal))) adj4 fracture$).tw. 3 or/1‐2 4 Hip Surgery/ or Fracture Fixation/ or Osteotomy/ or Orthopedic Fixation Devices/ 5 (osteotom$ or ream$ or compression or pin$1 or nail$ or screw$1 or plate$1).tw. 6 or/4‐5 7 and/3,6 8 exp Clinical Trials/ 9 exp Evaluation Research/ 10 exp Comparative Studies/ 11 exp Crossover Design/ 12 clinical trial.pt. 13 or/8‐12 14 ((clinical or controlled or comparative or placebo or prospective or randomi#ed) adj3 (trial or study)).tw. 15 (random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw. 16 ((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw. 17 (cross?over$ or (cross adj1 over$)).tw. 18 ((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw. 19 or/14‐18 20 or/13,19 21 and/7,20
Data and analyses
Comparison 1. Osteotomy versus anatomical reduction: fixed nail plate.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture fixation complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Cut‐out | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Fixation failure rate | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Deep sepsis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Final outcome measures (at 3 months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Mortality | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Failure to regain former mobility | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.1. Analysis.
Comparison 1 Osteotomy versus anatomical reduction: fixed nail plate, Outcome 1 Fracture fixation complications.
1.2. Analysis.
Comparison 1 Osteotomy versus anatomical reduction: fixed nail plate, Outcome 2 Final outcome measures (at 3 months).
Comparison 2. Osteotomy versus anatomical reduction: sliding hip screw.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Operative details: length of surgery and blood loss | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Length of surgery (minutes) | 2 | 209 | Mean Difference (IV, Fixed, 95% CI) | 6.97 [1.47, 12.46] |
| 1.2 Operative blood loss (ml) | 2 | 209 | Mean Difference (IV, Fixed, 95% CI) | 85.56 [35.52, 135.61] |
| 2 Fracture fixation complications | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Cut‐out rate | 2 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.29, 4.36] |
| 2.2 Non‐union | 2 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.47 [0.27, 111.39] |
| 2.3 Fixation failure rate | 4 | 419 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.51 [0.81, 2.83] |
| 2.4 Reoperation | 2 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.16, 4.19] |
| 3 Deep sepsis | 2 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.03, 2.50] |
| 4 Medical complications | 2 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.66, 1.45] |
| 5 Length of hospital stay (days) | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Anatomical deformity | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Leg shortening (> 1 cm) | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.17 [0.71, 6.58] |
| 6.2 Varus deformity | 2 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.10, 1.32] |
| 6.3 External rotation deformity | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.25 [0.35, 29.85] |
| 7 Final outcome measures | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Mortality | 3 | 309 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.57, 1.47] |
| 7.2 Failure to return to same residential status | 2 | 167 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.83, 2.28] |
| 7.3 Failure to regain mobility | 2 | 161 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.78, 1.39] |
2.4. Analysis.
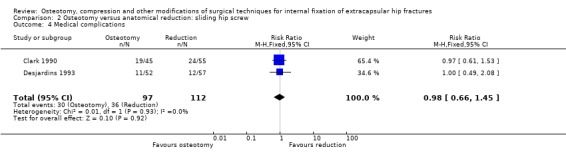
Comparison 2 Osteotomy versus anatomical reduction: sliding hip screw, Outcome 4 Medical complications.
2.7. Analysis.
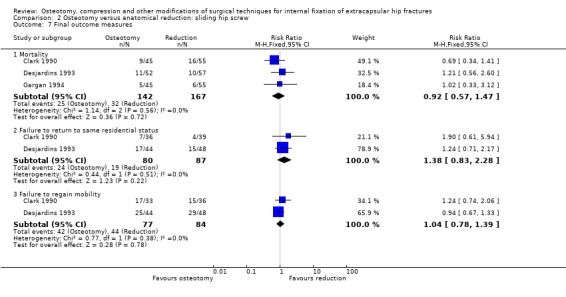
Comparison 2 Osteotomy versus anatomical reduction: sliding hip screw, Outcome 7 Final outcome measures.
Comparison 3. SHS fixation with cement versus standard SHS (no cement).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture fixation complications | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Cut‐out | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Loosening of the plate | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Delayed union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Reoperation | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Length of hospital stay | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Mortality | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Pain at 6 months (visual analogue scale: 0 none to 100 worst) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Global pain | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 On walking 50 feet | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Hip abductor strength (% of unaffected side) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
3.1. Analysis.
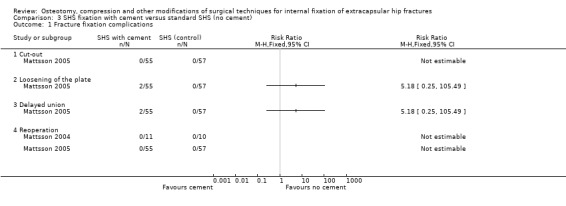
Comparison 3 SHS fixation with cement versus standard SHS (no cement), Outcome 1 Fracture fixation complications.
3.2. Analysis.
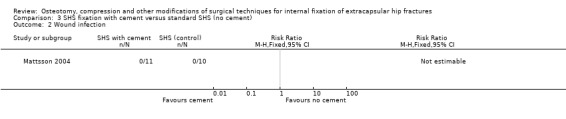
Comparison 3 SHS fixation with cement versus standard SHS (no cement), Outcome 2 Wound infection.
Comparison 4. Compression of trochanteric fractures in sliding hip screw fixation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Operative details: length of surgery and blood loss | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Length of surgery (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Operative blood loss (ml) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Varus deformity | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 5. Hydroxyapatite‐coated screws versus standard screws: SHS.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fracture fixation complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Cut‐out | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Reoperation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Mortality | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Functional and activity of daily living scores | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Harris hip score (0: worst to 100: best function) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 SF‐36 (0: worst to 100: best) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Calder 1995.
| Methods | Randomised trial: method of randomisation not stated | |
| Participants | 19 patients with a hip fracture treated with a sliding hip screw (SHS) Orthopaedic hospital in Leicester, UK Age: 60+ years % male: 0% (all female) Number lost to follow up: 0 | |
| Interventions | Reaming of the femur for the lag screw of the SHS with a modified reaming technique in which the outer cortex is first reamed with the reamer set to the minimum, then reaming is continued as normal (study group) versus reaming as normal (control group). | |
| Outcomes | Length of follow up: not stated Temperatures generated within the femoral head on reaming | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Clark 1990.
| Methods | Randomised by year of birth | |
| Participants | 100 patients with unstable intertrochanteric proximal femoral fractures treated with a SHS Orthopaedic hospitals in London, UK Mean age: 83 years (range 51‐100) % male: 14% Number lost to follow up: 3 (3%) | |
| Interventions | Sarmiento valgus osteotomy versus anatomical reduction | |
| Outcomes | Length of follow up: 3 months Length of surgery Operative blood loss Cut‐out of implant Fixation failure rate Reoperation Deep sepsis Mortality Length of hospital stay Any medical complications Failure to return to residential status Failure to regain mobility Shortening Varus deformity External rotation deformity | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Desjardins 1993.
| Methods | Randomised using computer generated list | |
| Participants | 127 patients with unstable intertrochanteric proximal femoral fractures treated with a SHS Orthopaedic hospitals in Montreal, Canada Mean age: 80.5 years (range 60‐99) % male: 23% Number lost to follow up: 18 (14%) | |
| Interventions | Dimon and Hughston medial displacement osteotomy versus anatomical reduction | |
| Outcomes | Length of follow up: mean 11 months Length of surgery Operative blood loss Cut‐out of implant Fixation failure rate Reoperation Deep sepsis Mortality Length of hospital stay Any medical complications Failure to return to residential status Failure to regain mobility Varus deformity | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Gargan 1994.
| Methods | Randomised using sealed envelopes | |
| Participants | 100 patients with an unstable intertrochanteric proximal femoral fractures treated with a SHS Orthopaedic hospitals in Oxford, UK Mean age: 82 years (range 60‐100) % male: 15% Number lost to follow up: 0 | |
| Interventions | Sarmiento valgus osteotomy or Dimon and Hughston medial displacement osteotomy versus anatomical reduction | |
| Outcomes | Length of follow up: till fracture union or fixation failure Length of surgery Blood transfusion requirements Fixation failure rate Mortality | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Hubbard 1980.
| Methods | Randomised using computer random numbers | |
| Participants | 65 patients with an pertrochanteric fracture of which 62 were treated with a Jewett nail plate Orthopaedic hospital in Shropshire, UK Mean age 82.5 years % male: not stated Number lost to follow up: 0 (except 3 not operated on) | |
| Interventions | Sarmiento osteotomy versus anatomical reduction | |
| Outcomes | Length of follow up: mean 3 months Length of surgery Operative blood loss Cut‐out Breakage of implant Reoperation Deep wound infection Mortality Failure to regain mobility | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kumar 1996.
| Methods | Randomised trial ‐ method of randomisation not stated | |
| Participants | 138 patients with an unstable trochanteric hip fracture treated with a SHS Hospital in Mumbai, India Mean age: 58 years (range 28‐101) % male: 59% Number lost to follow up: 18 (13%) | |
| Interventions | Medialisation osteotomy versus anatomical reduction | |
| Outcomes | Length of follow up: 6 months Length of surgery Operative blood loss Failure of fixation Pain Mortality Limping Mobility Walking distance | |
| Notes | The results for 28 patients were not included: 10 of these died and 18 were lost to follow up by 6 weeks. More of the patients allocated to the osteotomy group had their operation performed by a senior surgeon | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Mattsson 2004.
| Methods | Randomised using closed envelopes | |
| Participants | 26 patients with an unstable trochanteric hip fracture treated with a SHS Hospital in Uppsala, Sweden Mean age: 83 years (range 66‐95) % male: 15% Number lost to follow up: 1 (4%) (unable to attend) | |
| Interventions | Augmentation of a SHS fixation of a trochanteric fracture with calcium phosphate cement (Norian SRS) versus SHS fixation without cement. | |
| Outcomes | Length of follow up: 6 months Movement of the fracture site (via tantalum markers) Varus angulation Reoperation Wound infection | |
| Notes | Five participants were not followed up "per protocol": 2 had died; 2 were excluded for technical reasons; and 1 couldn't attend because of concurrent illness. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Mattsson 2005.
| Methods | Randomised using closed envelopes | |
| Participants | 112 patients with an unstable trochanteric hip fracture treated with a SHS Three hospitals in Sweden Mean age: 82 years (range not stated) male: 19% Number lost to follow up: 14 (13%) | |
| Interventions | Augmentation of a SHS fixation of a trochanteric fracture with calcium phosphate cement (Norian SRS) versus SHS fixation without cement. | |
| Outcomes | Length of follow up: 6 months Length of surgery Operative blood loss Sliding of the SHS Cut‐out of the implant Delayed union of the fracture Loosening of the plate Reoperation Abductor strength Mortality Length of hospital stay Pain (at 1 week, 6 weeks, 6 months) Ability to rise from a chair, get of a toilet, climb a step Mobility SF36 outcome score | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Moroni 2004.
| Methods | Randomised using computer generated list and sealed numbered opaque envelopes | |
| Participants | 133 patients (see Notes) with a trochanteric hip fracture treated with a sliding hip screw (SHS) Orthopaedic hospital in Bologna, Italy Mean age: 81 years %male: 0% (females only) Number lost to follow up: 3 (2%) | |
| Interventions | Fixation of the fracture with hydroxyapatite‐coated AO/ASIF lag and cortical stainless steel screws in conjunction with a standard SHS plate versus standard stainless steel AO/ASIF screws and plate fixation. | |
| Outcomes | Length of follow up: 6 months Cut‐out of lag screw Harris hip score SF‐36 score | |
| Notes | Additional information supplied by Dr Moroni and Dr Hoque. Participants who died in the six months follow up period (5 cases) or were lost to follow up (8 cases) were excluded from the study. In order to keep the number for follow up at 120, further patients were recruited. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Roder 1995.
| Methods | Randomised trial: method of randomisation not stated | |
| Participants | 50 patients with a stable trochanteric hip fracture treated with a Gamma nail Hospital in Wiesbaden, Germany Mean age: 81 years % male: 25% Number lost to follow up: 0 | |
| Interventions | Fixation of a trochanteric fracture with a Gamma nail with the addition of a 4.5mm venting drill hole in the lateral femoral cortex versus fixation with an intramedullary Gamma nail without a venting hole | |
| Outcomes | Length of follow up: not stated Bone marrow intravascular embolism as demonstrated by oesophageal ultrasound | |
| Notes | German article ‐ translation obtained. We thank Dr J Rasmus Kuester for this. The third intervention group of this trial involved 25 patients who were treated with a sliding hip screw. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Sernbo 1994.
| Methods | Randomised using sealed envelope opened in the operating theatre | |
| Participants | 200 patients with a trochanteric fracture treated with a SHS Orthopaedic hospital in Malmo, Sweden Mean age: 80 years % male: 32% Lost to follow up: 2 (1%) | |
| Interventions | SHS screw fixation of a trochanteric fracture with the locking screw to compress the fracture or without | |
| Outcomes | Length of follow up: 4 months Length of surgery Operative blood loss Non‐union rate Occurrence of varus deformity (> 10 degrees) Mortality (38 by 4 months) | |
| Notes | Separate data split by intervention group for mortality and people (7) who were too ill for a radiogram were not provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
SHS = sliding hip screw
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Acharya 2003 | Many of the fixation systems for trochanteric fracture have a flat surface on the lag screw that engages with a similar surface on the barrel. This prevents the screw rotating within the barrel. The potential benefit of this 'keyed' system is a reduce risk of the proximal part of the fixation rotating and a reduce risk of the lag screw migrating medially and becoming disengaged from the barrel. In this randomised study of 40 patients with a trochanteric fracture, 20 were treated using a 'keyed' (locked) sliding hip screw and 20 with an 'unkeyed' (unlocked) sliding hip screw. There was one case of fixation failure within the keyed group and two in the unkeyed group. No significant differences in pain scores were seen between the two groups. The study, which is currently reported only in conference abstracts, is excluded due to insufficient information. |
| Alobaid 2004 | Traditionally a sliding hip screw is inserted after a surgical incision has been made to expose the femur. The length of this incision may vary from about four centimetres to over 20 centimetres. Minimally invasive techniques use a small incision as possible by modifying the surgical technique of using a smaller length of side plate. This was reported as a 'surgeon randomised' study of 48 patients with a trochanteric fracture in which 21 patients were treated using a minimally invasive approach to insert a sliding hip screw and the remainder were treated by a conventional surgical approach. The study was excluded because the contact author (E J Harvey) did not provide any details of the actual method of randomisation aside from clarifying that he supervised the test intervention whilst the other staff continued to do a conventional technique. The choice of using 2‐hole or 4‐hole plate was not controlled for and there were insufficient data on the distribution of 2 hole plates and fracture types. It is possible that this trial could be included in a future update if adequate clarification on study methods and results in obtained. |
| Bong 1981 | In this randomised trial of 150 people with unstable intertrochanteric fractures, 50 were treated conservatively, 50 by a medial displacement osteotomy and fixation with a McLaughlin pin and plate, and 50 with a valgus osteotomy and fixation with a Mclaughlin pin and plate. This trial is included in the Cochrane review comparing conservative versus operative treatment (Handoll 2008). However, although it meets the stated inclusion criteria of this review, this trial is excluded because it presents only limited evidence for a comparison of variants of a technique (osteotomy) performed in conjunction with an inferior implant (the fixed nail plate). It is increasingly unlikely that the results of this trial would inform current practice. |
| Moroni 2007 | Randomised trial involving 16 patients whose trochanteric fractures were fixed with a trochanteric external fixator using hydroxyapatite coated pins. Patients were randomised to receive oral alendronate 70 mg weekly for three months versus no therapy in the control group. This study was excluded because it evaluated a pharmacological intervention. |
| Papanikolaou 1999 | This study was a comparative study of 63 patients with an unstable intertrochanteric fracture treated with a sliding compression screw in conjunction with a Dimon and Hughston osteotomy. These patients were compared with 45 patients treated with anatomical reduction and a sliding compression screw. Complications in the osteotomy group were one deep infection, one cut‐out and one non‐union. Complications in the other group were one deep infection, varus deformity in seven cases, cut‐out in three, breakage of the plate in one and plate detachment from the femur in one. The study was excluded as it was not a randomised study. |
Contributions of authors
Martyn Parker initiated and designed the review, performed study selection, contacted trialists, assessed study quality, extracted data and compiled the first drafts of the review and all subsequent updates. Gopi Tripuraneni and John McGreggor‐Riley checked data extraction and assessed the trials for methodological quality for the versions of the review available up to 2008. Helen Handoll checked over and corrected the pre‐existing review (2008), updated review methodology, performed study selection, contacted trialists, assessed study quality, extracted data and revised successive drafts. Martyn Parker is the guarantor of the review.
Sources of support
Internal sources
University of Teesside, Middlesbrough, UK.
Peterborough and Stamford Hospitals NHS Foundation Trust, Peterborough, UK.
External sources
No sources of support supplied
Declarations of interest
None known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Calder 1995 {published data only}
- Calder SJ, Barnes MR, Harper WM. Reduction of temperatures generated by the triple reamer within the femoral head. Injury 1995;26:183‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Clark 1990 {published data only}
- Clark DW, Ribbans WJ. Treatment of unstable intertrochanteric fractures of the femur: a prospective trial comparing anatomical reduction and valgus osteotomy. Injury 1990;21:84‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Desjardins 1993 {published data only}
- Desjardins AL, Roy A, Paiement C, Newman N, Pedlow F, Desloges D, Turcotte R. Unstable intertrochanteric fractures: A prospective randomized study comparing anatomic reduction and medial osteotomy. Journal of Bone and Joint Surgery ‐ British Volume 1992;74 Suppl 3:281‐2. [DOI] [PubMed] [Google Scholar]
- Desjardins AL, Roy A, Paiement G, Newman N, Pedlow F, Desloges D, et al. Unstable intertrochanteric fracture of the femur: A prospective randomized study comparing anatomical reduction and medial displacement osteotomy. Orthopedic Transactions 1994;18(3):735. [DOI] [PubMed] [Google Scholar]
- Desjardins AL, Roy A, Paiement G, Newman N, Pedlow F, Desloges D, Turcotte RE. Unstable intertrochanteric fracture of the femur: a prospective randomised study comparing anatomical reduction and medial displacement osteotomy. Journal of Bone and Joint Surgery ‐ British Volume 1993;75:445‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Pedlow F, Desjardins AL, Roy A, Paiement G. [Instable intertrochanteric fractures: a prospective study comparing anatomic reduction and osteotomy of medialisation]. Annales de Chirurgie 1991;45(9):849. [Google Scholar]
Gargan 1994 {published data only}
- Gargan MF, Gundle R, Simpson AHRW. How effective are osteotomies for unstable intertrochanteric fractures?. Journal of Bone and Joint Surgery ‐ British Volume 1994;76:789‐92. [MEDLINE: ] [PubMed] [Google Scholar]
- Gundle R, Gargan MF, Simpson AHRW. How to minimize failures of fixation of unstable intertrochanteric fractures. Injury 1995;26:611‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hubbard 1980 {published data only}
- Hubbard MJS, Burke FD, Bracey DJ, Houghton GR. A prospective controlled trial of valgus osteotomy in the fixation of unstable pertrochanteric fractures of the femur [Abstract]. Journal of Bone and Joint Surgery ‐ British Volume 1978;60:144. [DOI] [PubMed] [Google Scholar]
- Hubbard MJS, Burke FD, Houghton GR, Bracey DJ. A prospective controlled trial of valgus osteotomy in the fixation of unstable pertrochanteric fractures of the femur. Injury 1980;11:228‐32. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kumar 1996 {published data only}
- Kumar MM, Sudhakar GM, Shar DD, Pathak RH. A study of the role of osteotomy in unstable intertrochanteric fractures. Journal of Postgraduate Medicine 1996;42(1):4‐6. [PubMed] [Google Scholar]
Mattsson 2004 {published data only}
- Mattsson P, Larsson S. Unstable trochanteric fractures augmented with calcium phosphate cement. A prospective randomized study using radiostereometry to measure fracture stability. Scandinavian Journal of Surgery 2004;93(3):223‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mattsson 2005 {published data only}
- Mattsson P, Alberts A, Dahlberg G, Sohlman M, Hyldahl HC, Larsson S. Resorbable cement for the augmentation of internally‐fixed unstable trochanteric fractures. A prospective, randomised multicentre study. Journal of Bone and Joint Surgery ‐ British Volume 2005;87(9):1203‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Moroni 2004 {published and unpublished data}
- Hoque M. personal communication June 25 2008.
- Moroni A. Surgical techniques for osteoporotic bone. Journal of Bone and Joint Surgery ‐ British Volume 2006;88(Suppl 1):11. [Google Scholar]
- Moroni A, Faldini C, Pegreffi F, Giannini S. Better clinical outcomes for osteoporotic trochanteric fracture patients: DHS fixed with hydroxyapatite‐coated AO/ASIF screws [abstract]. Journal of Bone and Joint Surgery ‐ British Volume 2004;86(Suppl 3):243. [Google Scholar]
- Moroni A, Faldini C, Pegreffi F, Giannini S. HA‐coated screws decrease the incidence of fixation failure in osteoporotic trochanteric fractures. Clinical Orthopaedics and Related Research 2004;(425):87‐92. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Moroni A, Faldini C, Pegreffi F, Giannini S. How to improve results in osteoporotic hip fractures treated with dynamic hip screw fixation: a prospective randomized study [abstract]. Hip International 2002;12(2):244‐5. [Google Scholar]
Roder 1995 {published data only}
- Roder W, Isemer F‐E, Weigel TF, Zimmermann F, Peifer A. Bone marrow introvasion during operative pertrochanteric femur fracture care ‐ Gamma nail versus DHS [Markeinschwemmung bei operativer Versorgung pertrochantarer Femurfrakturen. Vergleich Gammanagel gegen DHS]. Aktuelle Traumatologie 1995;25:67‐71. [MEDLINE: ] [Google Scholar]
Sernbo 1994 {published data only}
- Sernbo I, Johnell O, Gardsell A. A prospective randomized trial in trochanteric hip fractures treated with compression hip screw with and without locking and compression of the lag screw [Abstract]. Acta Orthopaedica Scandinavica ‐ Supplementum 1990;237:55. [DOI] [PubMed] [Google Scholar]
- Sernbo I, Johnell O, Gardsell A. Locking and compression of the lag screw in trochanteric fractures is not beneficial: a prospective, randomized study of 153 cases. Acta Orthopaedica Scandinavica 1994;65:24‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Acharya 2003 {published data only}
- Acharya MR, Eastwood G, Bing A, Harper WH. Fixation of hip fractures with a sliding hip screw: a randomised controlled trial comparing fixation of the plate in the keyed and unkeyed position [abstract]. Injury‐International Journal of the Care of the Injured 2003;34:629. [Google Scholar]
- Acharya MR, Eastwood G, Bing A, Harper WH. Fixation of hip fractures with a sliding hip screw: a randomised controlled trial comparing fixation of the plate in the keyed and unkeyed position [abstract]. Journal of Bone and Joint Surgery ‐ British Volume 2004;86(Suppl 1):78. [Google Scholar]
- Acharya MR, Eastwood G, Bing A, Harper WH. Fixation of hip fractures with a sliding hip screw: a randomised controlled trial comparing fixation of the plate in the keyed and unkeyed position [abstract]. Journal of Bone and Joint Surgery ‐ British Volume 2004;86(Suppl 3):377. [Google Scholar]
Alobaid 2004 {published data only}
- Alobaid A, Harvey EJ, Elder GM, Lander P, Guy P, Reindl R. Minimally invasive dynamic hip screw: prospective randomized trial of two techniques of insertion of a standard dynamic fixation device. Journal of Orthopaedic Trauma 2004;18(4):207‐12. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bong 1981 {published and unpublished data}
- Bong SC, Lau HK, Leong JCY, Fang D, Lau MT. The treatment of unstable intertrochanteric fractures of the hip: a prospective trial of 150 cases. Injury 1981;13:139‐46. [DOI] [PubMed] [Google Scholar]
Moroni 2007 {published data only}
- Moroni A, Faldini C, Hoang‐Kim A, Pegreffi F, Giannini S. Alendronate improves screw fixation in osteoporotic bone. Journal of Bone and Joint Surgery ‐ American Volume 2007;89(1):96‐101. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Papanikolaou 1999 {published data only}
- Papanikolaou A, Deimedes G, Lochovitis K, Darmanis S, Antoniou N. The treatment of unstable intertrochanteric fractures: medial displacement osteotomy versus anatomical nailing [Abstract]. Journal of Bone and Joint Surgery. British Volume 1999;81 Suppl 2:64. [Google Scholar]
Additional references
Calder 1995a
- Calder SJ, Barnes MR, Harper WM. Reduction of temperatures generated by the triple reamer within the femoral head. Injury 1995;26:183‐5. [DOI] [PubMed] [Google Scholar]
Christie 1995
- Christie J, Robinson CM, Pell AC, McBirnie J, Burnett R. Transcardiac echocardiography during invasive intramedullary procedures. Journal of Bone and Joint Surgery ‐ British Volume 1995;77:450‐5. [PubMed] [Google Scholar]
Dimon 1967
- Dimon JH, Hughston JC. Unstable intertrochanteric fractures of the hip. Journal of Bone and Joint Surgery ‐ American Volume 1967;49(3):440‐50. [MEDLINE: ] [PubMed] [Google Scholar]
Eriksson 1984
- Eriksson AR, Albrektsson T, Albrektsson B. Heat caused by drilling: cortical bone‐temperature measured in vivo in patients and animals. Acta Orthopaedica Scandinavica 1984;55:629. [DOI] [PubMed] [Google Scholar]
Evans 1949
- Evans EM. The treatment of trochanteric fractures of the femur. Journal of Bone and Joint Surgery ‐ British Volume 1949;31:190‐203. [PubMed] [Google Scholar]
Handoll 2008
- Handoll HHG, Parker MJ. Conservative versus operative treatment for hip fractures in adults. Cochrane Database of Systematic Reviews 2008, Issue 3. [DOI: 10.1002/14651858.CD000337.pub2] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2006
- Higgins JPT, Green S, editors. Highly sensitive search strategies for identifying reports of randomized controlled trials in MEDLINE. Cochrane Handbook for Systematic Reviews of Interventions 4.2.6 [updated September 2006]; Appendix 5b. www.cochrane.org/resources/handbook/hbook.htm (accessed 01 May 2007).
Jenson 1980
- Jensen JS. Classification of trochanteric fractures. Acta Orthopaedica Scandinavica 1980;51:803‐10. [DOI] [PubMed] [Google Scholar]
Parker 1998
- Parker MJ, Handoll HHG. Condylocephalic nails versus extramedullary implants for extracapsular hip fractures. Cochrane Database of Systematic Reviews 1998, Issue 4. [DOI: 10.1002/14651858.CD000338] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parker 2006a
- Parker M, Gurusamy KS. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD001706.pub3] [DOI] [PubMed] [Google Scholar]
Parker 2006b
- Parker MJ, Handoll HHG. Extramedullary fixation implants and external fixators for extracapsular hip fractures in adults. Cochrane Database of Systematic Reviews 2006, Issue 1. [DOI: 10.1002/14651858.CD000339.pub2] [DOI] [PubMed] [Google Scholar]
Parker 2008
- Parker MJ, Handoll HHG. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database of Systematic Reviews 2008, Issue 3. [DOI: 10.1002/14651858.CD000093.pub4] [DOI] [Google Scholar]
Sarmiento 1970
- Sarmiento A, Williams EM. The unstable intertrochanteric fracture: treatment with a valgus osteotomy and I‐beam nail plate. Journal of Bone and Joint Surgery ‐ American Volume 1970;52:1309‐18. [PubMed] [Google Scholar]


