Abstract
The absence of the Duffy protein at the surface of erythrocytes was considered for decades to confer full protection against Plasmodium vivax as this blood group is the receptor for the key parasite ligand P. vivax Duffy binding protein (PvDBP). However, it is now clear that the parasite is able to break through this protection and induce clinical malaria in Duffy-negative people, although the underlying mechanisms are still not understood. Here, we briefly review the evidence of Duffy-negative infections by P. vivax and summarize the current hypothesis at the basis of this invasion process. We discuss those in the perspective of malaria-elimination challenges, notably in African countries.
Author summary
Plasmodium vivax is the most widespread of the parasite species causing human malaria. It was considered for decades to be almost absent from sub-Saharan African countries because the majority of people in these areas lack a red blood cell receptor, the Duffy protein, which is the critical gateway for the parasite’s entry into erythrocytes. In the last years, this dogma has been challenged by an increasing number of observations of P. vivax clinical infections into Duffy-negative people (individuals lacking the Duffy receptor) in many African countries as well as in South America where a significant number of people of African descent are also Duffy-negative. However, we still do not know how P. vivax is able to infect those individuals. Understanding how this invasion takes place will be critical for the implementation of adapted control solutions targeting this parasite species in order to achieve malaria elimination, especially in African countries where tremendous decline in the prevalence of the other major human malaria species, P. falciparum, has been achieved in the past decade.
Introduction
Plasmodium vivax is one of the five Plasmodium species causing human malaria and although considered as benign during prior decades, it is now recognized as a significant cause of morbidity and mortality in endemic populations [1–4]. Its geographic distribution is the widest, and more than three billion people live within the P. vivax transmission limits [5]. For decades, this parasite was considered to be almost absent from the African continent with the exception of the Horn of Africa [6, 7]. Indeed, during the era of malariotherapy, it was noted that individuals of African ancestry were often resistant to P. vivax infection [8–10]. Later on, it was shown that individuals lacking the Duffy antigen, a red blood cell membrane protein known to be absent in several populations of African origin, were protected from P. vivax infections, establishing the evidence that the receptor of P. vivax at the erythrocyte surface was the Duffy protein [11–13]. It’s not until the 2000s that the dogma was challenged by reports of Duffy-negative people infected by P. vivax [14, 15]. Here we review the Duffy nomenclature, the different polymorphisms affecting P. vivax invasion, the evidence describing infections of Duffy-negative individuals by P. vivax as well as the hypotheses currently held to explain the molecular basis of Duffy-negative P. vivax infections. We discuss those in the perspective of malaria-elimination challenges notably in African countries.
How Duffy affects P. vivax invasion
The Duffy protein is a receptor for chemokines (Duffy antigen receptor for chemokines [DARC]), officially called the atypical chemokine receptor 1 (ACKR1) [16, 17]. This protein is the receptor for P. vivax Duffy binding protein (PvDBP), allowing entry of the parasite into the red blood cells and more precisely, into the reticulocytes, the target cells of P. vivax invasion [18]. Duffy is polymorphic, and many variants have been described, with nomenclature often changing over time. In this Review, we briefly describe the main variants of relevance for interaction with P. vivax, using the nomenclature commonly used in the field (see [19] for thorough up to date description of the Duffy polymorphism). There are two major alleles known for Duffy: FY*A (coding for the Fya antigen) [20] and the ancestral allele FY*B (coding for the Fyb antigen) [21–26] (Table 1). Three major genotypes exist (FY*A/FY*A, FY*B/FY*B, and FY*A/FY*B), resulting in three possible phenotypes (corresponding to the associated blood groups): Fy(a+b-), Fy(a-b+), and Fy(a+b+), collectively called Duffy-positive. The Fy(a-b-) phenotype is referred to as the Duffy-negative phenotype [11]. One single point mutation in the GATA-1 transcription factor binding site of the promoter of the gene at position −67 changing a T nucleotide to a C underlies the Duffy-negative phenotype [19, 24]. This genotype is referred to as erythrocyte silent (ES) because individuals homozygous for this mutation lack the Duffy protein on erythrocytes, while heterozygous individuals display approximately 50% of the Duffy protein [27–30]. Duffy-negative people of African ancestry are homozygous for this mutation that is at near fixation in sub-Saharan Africa [31]. In those individuals, the mutation is located upstream of the FY*B allele, leading to the homozygous FY*BES/FY*BES genotype responsible for the refractoriness of Duffy-negative people to P. vivax infections.
Table 1. Major Duffy alleles, genotypes and phenotypes described in human populations and alternate nomenclature.
| Allelesa | Antigen | Genotypes | Phenotypes | |
|---|---|---|---|---|
| Pos | FY*A = FY*01 | Fya | FY*A/FY*A | Fy(a+b-) |
| FY*B = FY*02 | Fyb | FY*A/FY*B | Fy(a+b+) | |
| FY*A/FY*BES | Fy(a+b-) | |||
| Neg | FY*AES = FY*Anull = FY*01N.01 | FyES | FY*A/FY*AES | Fy(a+b-) |
| FY*BES = FY*O = FY*Bnull = FY*02N.01 | FyES | FY*B/FY*B | Fy(a-b+) | |
| FY*B/FY*BES | Fy(a-b+) | |||
| FY*BES/FY*BES | Fy(a-b-) |
aThe official allele nomenclature is indicated in bold.
Neg, negative, Pos, positive
Discrepant results have been reported concerning the impact on P. vivax infection of having only one ES allele. It was initially shown in Papua New Guinea that FY*A/FY*AES heterozygous individuals were at lower risk of P. vivax infection compared to FY*A/FY*A people (in Papua, the −67 T to C mutation has arisen upstream of the FY*A allele, independently of the FY*BES found in Africa) [30, 32]. Similarly, in the Brazilian Amazon, heterozygous FY*A/FY*BES individuals were at lower risk of P. vivax malaria compared to FY*A/FY*B people [33]. However, in the same Brazilian study, heterozygous FY*B/FY*BES individuals were at increased risk of malaria infection compared to homozygous FY*A/FY*B people [33]. These apparently conflicting observations might simply reflect differences between the numbers of individuals analyzed for each genotype, resulting in underpowered analysis. More epidemiological studies in different endemic settings are needed to get a clearer understanding of the associations between the Duffy genotypes and infection outcomes.
In addition, independently of the ES genotype, there seems to be a protective effect of the FY*A allele compared to the FY*B one against P. vivax infections. Indeed, in vitro studies have shown that the PvDBP binding to the FY*A allele was reduced compared to binding to the FY*B allele [34]. It was also observed that FY*A was associated with clinical protection, while FY*B was associated with increased infection risk by P. vivax [33, 34].
Altogether, those studies suggest that the link between Duffy genotypes and susceptibility to P. vivax is more complex than just the association between Duffy-negative and full protection.
Evidence of P. vivax infections in Duffy-negative people
Travelers infected by P. vivax coming back from sub-Saharan African regions
The first indirect evidence of P. vivax infection in Duffy-negative individuals comes from the reports of travelers presenting a P. vivax infection after returning from African areas where Duffy-negative is at near fixation [35, 36]. However, those observations did not question the prevailing dogma of Duffy-negative refractoriness for several reasons. First, P. vivax is morphologically similar to P. ovale endemic in most Africa, which could lead to microscopic misinterpretation. The advent of molecular techniques to diagnose parasites have ruled out this confounding factor and have allowed to unequivocally identify P. vivax [37–39]. Second, because of the occurrence of P. vivax hypnozoites hiding in the liver for months or even years before triggering a relapse infection, the origin of the parasite is difficult to determine. Third, it was suggested that a small proportion of Duffy-positive individuals is enough to sustain the transmission cycle of P. vivax independently of Duffy-negative infections [40]. Similarly, the detection of P. vivax in Anopheles mosquitoes collected in areas where the majority of people are Duffy-negative cannot conclusively demonstrate Duffy-negative infections [14]. Therefore, additional evidence is clearly needed to demonstrate the ability of P. vivax to infect Duffy-negative individuals.
P. vivax infections in Duffy-negative people from sub-Saharan Africa
In the last decade, reports of P. vivax infections in Duffy-negative individuals have increased steadily. There is no doubt that the advent of molecular techniques unambiguously detecting P. vivax at high sensitivity has greatly contributed to those observations. However, those observations come with caveats that can only be resolved by microscopic observations. Indeed, detection of P. vivax DNA by PCR in a Duffy-negative individual’s blood sample can arise from pre-erythrocytic stages of the parasites even in the absence of actual red blood cell invasion [41]. Similarly, seropositivity to P. vivax antigens can result from the presence of pre-erythrocytic parasite forms independently of blood-stage infection (not to mention the possible crossreactivity of the serological analysis with other Plasmodium species) [42]. Therefore, microscopic observation of P. vivax within a Duffy-negative erythrocyte, along with genotyping confirmation (especially to exclude a P. ovale infection), is necessary to prove Duffy-negative infection. The first mention of a microscopic observation of P. vivax in a Duffy-negative erythrocyte was made in 2006 [14] (Culleton and colleagues [40] mentioned a report by Van Ros in 1985 but we could not retrieve the original publication). However, when the slides were double read by two expert microscopists for confirmation, P. vivax could not be confirmed [14]. It is in 2010 that the definitive evidence of a P. vivax infection within Duffy-negative erythrocyte from patients living in Madagascar was reported [15]. It was hypothesized that it is the admixture of Duffy-positive and Duffy-negative people occurring in Madagascar that has allowed the parasites to become adapted to Duffy-negative individuals. Of note, when Bray assessed the susceptibility of 30 Nigerian people to P. vivax through experimental mosquito bite infections, he did observe P. vivax blood-stage infection in one of the subjects [43]. It can be speculated that this Nigerian individual was Duffy-negative, though this cannot be confirmed. Interestingly, the strain used by Bray was the “Madagascar strain” of P. vivax, and it is tempting to speculate that its Malagasy genetic background allowed the parasite to infect a Duffy-negative individual. However, the exact origin of this strain is controversial, and it cannot be ascertained that it indeed comes from Madagascar [2, 44–46]. Since then, further unequivocal P. vivax Duffy-negative infections were reported from Ethiopia where Duffy-negative and Duffy-positive people coexist [47, 48] and also from countries where Duffy negativity is at near fixation, such as Cameroon [49] and Mali [50] (though in some of those studies the morphological features of erythrocytic P. vivax were not well resolved). Additionally, the detection of P. vivax in Duffy-negative individuals either by molecular diagnostic or serological analysis only has been made in a large number of sub-Saharan countries (for extensive review, see [36]). The description of Duffy-negative patients harboring microscopically-confirmed P. vivax erythrocyte infections coupled to molecular diagnostic confirmation in genotyped Duffy-negative individuals have undoubtedly challenged the established paradigm that prevailed for decades, opening new research questions regarding this neglected malaria parasite.
P. vivax infections of Duffy-negative people from the American continent
Current American populations are characterized as an admixture of individuals of different ancestries, due to the historical human migrations over the last centuries (European, African, Native American, Asian, etc.). Depending on the areas, some variable numbers of people are Duffy-negative due to their African ancestry and are distributed throughout South America up to southern United States of America [6]. In South and Central America, where P. vivax is endemic, the paradigm of Duffy-negative protecting against P. vivax malaria was quite well established with a number of studies from diverse locations [51–56]. However, similarly to the situation in Africa, several studies have suggested through serological, molecular, and microscopic detection analysis that Duffy negativity is not completely protective against P. vivax infection [33, 57–59].
All those studies clearly show that the protection of the Duffy negativity does not constitute an absolute barrier against P. vivax infections.
Towards understanding the mechanisms of Duffy-negative invasion by P. vivax
How does P. vivax invade Duffy-negative red blood cells? Has P. vivax recently evolved strategies to infect Duffy-negative erythrocytes, or are alternative invasion pathways ubiquitous in P. vivax populations? Those are key questions, and answering them will be critical to develop strategies to prevent the emergence of Duffy-negative infections. No clear answer has been made yet, mainly because of the inherent difficulty in working on P. vivax as there is still no in vitro continuous culture available for this species [60, 61]; however, some hypothesis can be raised on the parasite and/or human sides.
Parasite side: PvDBP duplication and/or other parasite ligands?
The first mechanistic hypothesis that has been made following the observation of Duffy-negative, P. vivax-infected patients in Madagascar came through whole genome sequencing (WGS) of field isolates. This analysis showed a duplication in the PvDBP gene in Malagasy isolates, and further molecular epidemiology surveys revealed that this duplication was observed in parasites isolated from a wide range of geographic locations (South America, East Africa, Madagascar, Asia-Pacific) [62]. Noteworthy, the highest frequency of isolates with pvdbp duplication (nearly 53%) was detected in Madagascar, in comparison to other areas (12.5% in Sudan, 9% in Cambodia). It was thus speculated that this duplication might have been selected in Madagascar to respond to the Duffy negativity barrier perhaps by increasing the amount of PvDBP protein on the merozoite’s surface to bind to an unknown low-affinity receptor [62]. Interestingly, in two different studies, P. vivax-infecting, Duffy-negative individuals from Ethiopia (where the prevalence of pvdbp amplification is between 55% to 80% [63, 64]) carried multiple copies of pvdbp, although the number of individuals were too low to draw definitive conclusions (only two in each report) [48, 64]. However, PvDBP itself has been shown to not bind to Duffy-negative erythrocytes, questioning how it could be involved in Duffy-negative invasion [18, 48]. Furthermore, the analysis by WGS of more than 200 P. vivax isolates from around the world indicated that 33% of Cambodian parasites carried the pvdbp duplication, much higher than the previously reported 9% [65]. In fact the initial PCR-based surveys have missed isolates carrying the duplication, because of variation in the boundaries of the duplication among parasites [66]. Using a quantitative PCR assay that enables the gene copy number assessment independently of the duplication boundaries, no difference in the pvdbp copy number between Cambodian parasites (where there is virtually no Duffy-negative individuals) and Malagasy ones (where an admixture of Duffy-negative and Duffy-positive individuals coexist) was observed [67]. Those results suggest that pvdbp amplification is not selected in response to the Duffy negativity barrier [67]. In a recent molecular epidemiology study conducted on Ethiopian P. vivax isolates, it was observed that the proportion of parasites with pvdbp amplification was higher in individuals carrying the FY*A allele compared to individuals carrying the FY*B one [64]. As mentioned above, because the binding of PvDBP to FY*A is lower than to FY*B, it can be speculated that pvdbp amplification could have been selected to increase the affinity to erythrocytes expressing the FY*A allele by supposedly increasing the amount of PvDBP protein at the surface of the merozoites. In the same study, the proportion of parasites with multiple pvdbp copies was significantly higher in symptomatic patients compared to asymptomatic individuals, raising the possibility that pvdbp amplification is involved in immune evasion of the parasites. Further investigations are clearly needed to understand the role of pvdbp amplification.
In addition to copy number variation, there is a number of evidence pointing to the absence of a specific sequence polymorphism in PvDBP in relation to Duffy-negative invasion. Recently, PvDBP sequence analysis of parasites infecting Duffy-negative and Duffy-positive people from Sudan showed that most alleles were shared between parasites, and those alleles were found globally [68]. Also, recombinant PvDBP alleles isolated from two Duffy-negative individuals infected by P. vivax in Ethiopia were expressed in vitro, and none could bind to Duffy-negative erythrocytes while they were binding to Duffy-positive ones [48].
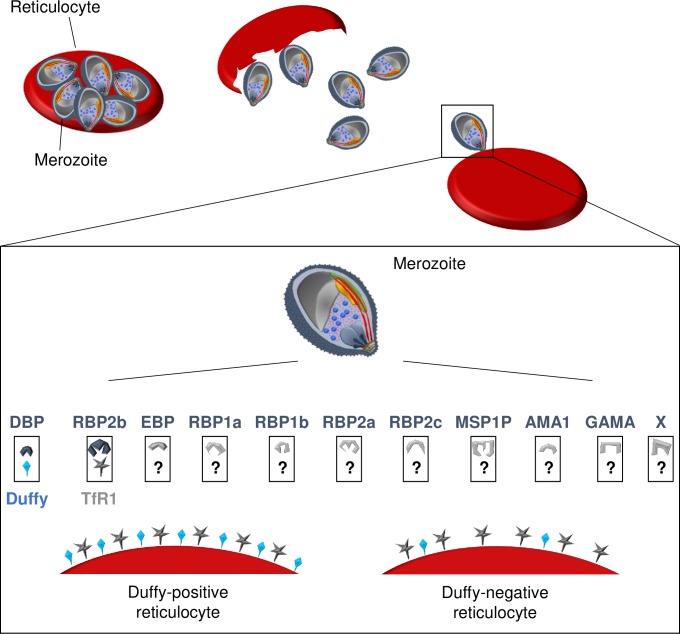
There are other parasite ligands described, such as P. vivax reticulocyte binding proteins (PvRBPs), although they have received much less attention than PvDBP and their role in erythrocyte invasion (whether Duffy-positive or Duffy-negative) for most of them is yet to be determined [69, 70]. PvRBPs are a family of ligands shown to bind to erythrocytes, but conflicting results were obtained for some of them regarding specific binding to reticulocytes [70, 71]. Among the different PvRBPs, the binding to Duffy-negative erythrocytes was evaluated only for PvRBP1a and PvRBP2c, and both were found to bind to Duffy-negative reticulocytes, indicating they could be involved in Duffy-independent invasion pathways [69]. Naturally-acquired antibodies against some RBPs inhibiting binding to erythrocytes or being associated with clinical protection have been described; however, the involvement of those ligands in actual parasite invasion was not assessed, except for PvRBP1a and PvRBP2b [72–77]. While PvRBP1a does not seem to be critical for P. vivax invasion in Duffy-positive cells [75], PvRBP2b was recently shown to be a key ligand involved in reticulocyte recognition and invasion through the transferrin receptor 1 (TfR1) [76]. However, the roles of PvRBP1a and of PvRBP2b–TfR1 have not been evaluated specifically in the invasion of Duffy-negative red blood cells. Recently, P. vivax merozoite surface protein-1 paralog (PvMSP1P) and P. vivax glycosylphosphatidylinositol-anchored micronemal antigen (PvGAMA) were shown to bind to both Duffy-positive and Duffy-negative red blood cells, and antibodies against PvMSP1P blocked the related P. knowlesi invasion in Duffy-positive reticulocytes [78–80]. Those results suggest that PvGAMA and PvMSP1P are ligands that could be involved in Duffy-independent reticulocyte invasion pathways, although functional demonstration is still lacking. Finally, P. vivax erythrocyte-binding protein (PvEBP, also known as PvDBP2) has also been shown to moderately bind to Duffy-negative reticulocytes [48, 81, 82]. Of interest, it was recently shown that this gene can be amplified and a higher proportion of parasites from Madagascar (where Duffy-negative and Duffy-positive people coexist) carry multiple copies of PvEBP compared to isolates from Cambodia (where only Duffy-positive people are present) [67]. Also, while only duplication was observed in Cambodia, up to five copies of PvEBP were detected in Malagasy parasites [67]. Altogether, those results suggest that PvEBP might be also involved in Duffy-negative invasion mechanisms, but again, functional demonstration is still lacking. Functional studies need to be developed in the future to figure out the role of each of the mentioned parasite ligands in the invasion of Duffy-positive and Duffy-negative reticulocytes as well as to identify possible unknown ligands involved in alternative invasion pathways (Fig 1).
Fig 1. Schematic representation of receptor-ligands involved in P. vivax invasion process of reticulocytes.
At the end of the erythrocytic cycle, the schizonts burst and release merozoites in the blood stream, enabling the invasion of uninfected reticulocytes. The recognition of reticulocytes and the invasion process require interactions between parasite ligands and reticulocyte receptors. For Duffy-positive reticulocyte invasion, PvRBP2b binds first to the TfR1 present on reticulocytes, and subsequently, PvDBP engages with the Duffy protein allowing the entry of the merozoite in the cell. Other ligands such as PvEBP, PvRBPs, PvMSP1P, PvAMA1, or PvGAMA are currently being investigated for their involvement in this invasion process, and their putative receptors are unknown. PvRBP2b probably also recognizes TfR1 of Duffy-negative reticulocytes; however, the subsequent invasion steps are still unknown. Are there a few Duffy molecules present on the surface of the erythrocyte enabling parasites with multiple PvDBP gene copies to invade the cell? Conversely, is the invasion process of Duffy-negative reticulocytes occurring through alternate, yet-to-identity receptors of, perhaps, ligands such as PvEBP, PvMSP1P, or PvGAMA? Finally, the invasion process might occur through complete unknown pathways with both unidentified ligands (noted with X) and receptors. AMA1, anchored micronemal antigen 1; DBP, Duffy binding protein; EBP, erythrocyte-binding protein; GAMA, glycosylphosphatidylinositol-anchored micronemal antigen; MSP1P, merozoite surface protein-1 paralog; Pv, Plasmodium vivax; RBP, reticulocyte binding proteins; TfR1, transferrin receptor 1.
Human side: Alternate receptor or Duffy involvement?
On the human erythrocyte side, the main question is: Through what receptor is P. vivax able to enter Duffy-negative red blood cells? While for P. falciparum many receptors have been described to ensure the parasite entry through multiple pathways, for P. vivax (until recently) only the Duffy protein was known. As mentioned above, TfR1 has recently been identified as the receptor to PvRBP2b for reticulocyte recognition and invasion [76]. TfR1 is one of the many membrane proteins lost during red blood cell maturation and is thus absent from normocytes [83, 84]. It is present on both Duffy-positive and Duffy-negative reticulocytes; however, it is believed that the critical interaction between PvRBP2b and TfR1 occurs upstream of the PvDBP–Duffy one, not independently of it [76]. Anyway, the role of this interaction in Duffy-negative has not been assessed, and an alternate human red blood cell receptor involved in Duffy-independent invasion pathways has yet to be discovered.
Could the invasion of Duffy-negative people require a particular Duffy protein not recognized by serological tools and therefore falsely assigned as negative? Probably not, as sequencing of this gene has consistently shown that the basis for Duffy-negative is a single mutation in the promoter of the gene upstream of the FY*B allele in African populations [24]. More conclusively, the full coding sequence of the Duffy gene, including its promoter, of 14 Duffy-negative individuals actually infected by P. vivax, have been sequenced, and all were homozygous with the expected −67 T to C mutation upstream of the FY*B alleles, indicating that no cryptic allele was at the origin of the infection [15].
However, what has not been definitely ruled out and is perhaps the most parsimonious explanation for the mechanisms of Duffy-negative invasion is that the Duffy-negative phenotype is not Duffy null [85]. Indeed, it can be speculated that although the −67 T to C mutation reduces the binding of the GATA-1 transcription factor and therefore transcription of the gene, this reduction might not be complete and RNA transcription could still be occurring at very low levels, leading to an amount of Duffy protein below the limit of detection of current analytical tools. Some recent data suggest that Duffy protein is notably detectable in erythroid precursor cells typically found in the bone marrow where P. vivax invasion is believed to occur to some extent [85–87]. It is worth mentioning here that Duffy-negative people do express the Duffy protein in other cell types such as in endothelial cells, indicating that the expression of Duffy is not intrinsically abolished by the −67 T to C mutation [23, 88]. This hypothesis would explain the very low parasitemia usually observed in Duffy-negative infected patients and also imply that P. vivax does not necessarily require an alternate pathway but could instead go through the classical PvDBP−Duffy invasion process. Such a hypothesis is so far only a speculation, and the involvement of an unknown receptor cannot be excluded (Fig 1). More investigations are needed to determine how the parasite is able to infect Duffy-negative red blood cells.
Future directions and conclusive remarks
With such evidence of P. vivax infections in Duffy-negative people, a better understanding of the epidemiology of this parasite is necessary and will involve the implementation of specific diagnostics in the African continent, where apart from the Horn of Africa and Madagascar, P. vivax is usually not looked for. A characteristic of P. vivax infections in Duffy-negative individuals is the usually low parasitemia easily missed by microscopy or conventional rapid diagnostics tests (RDTs) and leading to asymptomatic infections often detected through community-based, cross-sectional surveys [50, 89]. As such, sensitive molecular detection tools such as PCR should be implemented for P. vivax diagnostics.
To provide better insights in the mechanisms underlying Duffy-negative infections, next-generation sequencing technologies will be extremely useful both at the genomic and transcriptomic level. By identifying genomic loci under selection in P. vivax isolates infecting Duffy-negative individuals compared to Duffy-positive ones or originating from areas where Duffy negativity is at near fixation compared to areas where Duffy-positive are predominant, candidate genes involved in the adaptation to Duffy-negative reticulocytes might be detected. Similarly, by comparing the gene expression profiles of parasites infecting Duffy-negative or Duffy-positive people, the signature of genes specifically regulated to respond to the Duffy negativity barrier might be identified. Such an approach could also make use of the Saimiri and Aotus nonhuman primate model—as both species can be infected by P. vivax, while PvDBP can bind only to Aotus erythrocytes and not to Saimiri ones, indicating an alternative invasion pathway reminiscent of what is observed for Duffy-negative human erythrocytes [90]. Alternative models to decipher erythrocyte invasion mechanisms could also rely on the genetically tractable P. knowlesi that shares many biological similarities with P. vivax, including the requirement of the Duffy receptor for erythrocyte invasion [91] or even on P. cynomolgi, closely related to P. vivax and recently adapted to in vitro culture [92].
Providing definitive evidence of the involvement of any candidate ligand involved in Duffy-negative reticulocytes’ invasion will anyway require functional demonstration in a P. vivax human reticulocyte model. However, as mentioned before, there is still no continuous in vitro culture for this parasite species, and consequently no genetic transformation is possible. Only tedious, short-term cultures conducted in a handful of laboratories around the world can be performed [76, 93–95]. Nevertheless, using those assays in order to evaluate the capacity of parasites with different genotypes (i.e., single or multicopy pvdbp parasites) to invade Duffy-negative reticulocytes in presence or absence of monoclonal antibodies specific for a candidate ligand or receptor will allow one to determine the pathways used by P. vivax to infect Duffy-negative erythrocytes. In addition, on the erythrocyte side, elegant technologies have been developed to manipulate the repertoire of proteins expressed on erythropoietic cells using an immortalized erythroid progenitor cell line that can provide additional evidence on the involvement of specific receptors in P. vivax invasion [96]. All those approaches, combined with structural biology techniques, have the potential to identify receptor–ligand interactions involved in P. vivax invasion as performed for the recent discovery of PvRBP2b–TfR1 involvement [76].
In Africa, malaria burden is largely due to the more virulent and severe P. falciparum that is, of course, currently the primary target of elimination strategies. However, it can be expected that in the future while the elimination of falciparum malaria hopefully continues as seen for the last decade [97], more cases of P. vivax will be reported, as often the proportion of P. vivax cases increases while elimination progresses [5]. In those countries and elsewhere, in order to achieve elimination of all malaria species it will be necessary to implement strategies targeting P. vivax [98]. Among those, a PvDBP-based vaccine is currently under clinical development [99, 100], and deciphering the molecular pathways by which P. vivax is able to infect Duffy-negative people will be critical for ensuring the success of such a strategy.
Funding Statement
Agence Nationale de la Recherche Tremplin-ERC (TERC3) 2017 http://www.agence- nationale-recherche.fr/Project-ANR-17-ERC3-0002 (grant number EVAD: Evolutionary history and genetic adaptation of Plasmodium vivax). Received by VR. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Barber BE, William T, Grigg MJ, Parameswaran U, Piera KA, Price RN, et al. Parasite Biomass-Related Inflammation, Endothelial Activation, Microvascular Dysfunction and Disease Severity in Vivax Malaria. PLoS Pathog. 2015;11(1):e1004558 10.1371/journal.ppat.1004558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baird JK. Evidence and Implications of Mortality Associated with Acute Plasmodium vivax Malaria. Clinical Microbiology Reviews. 2013;26(1):36–57. 10.1128/CMR.00074-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Douglas N, Pontororing G, Lampah D, Yeo T, Kenangalem E, Poespoprodjo J, et al. Mortality attributable to Plasmodium vivax malaria: a clinical audit from Papua, Indonesia. BMC Medicine. 2014;12(1):217 10.1186/s12916-014-0217-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siqueira A, Lacerda M, Magalhaes B, Mourao M, Melo G, Alexandre M, et al. Characterization of Plasmodium vivax-associated admissions to reference hospitals in Brazil and India. BMC Medicine. 2015;13(1):57 10.1186/s12916-015-0302-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Battle KE, Lucas TCD, Nguyen M, Howes RE, Nandi AK, Twohig KA, et al. Mapping the global endemicity and clinical burden of Plasmodium vivax, 2000–17: a spatial and temporal modelling study. The Lancet. 2019. 10.1016/S0140-6736(19)31096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howes RE, Patil AP, Piel FB, Nyangiri OA, Kabaria CW, Gething PW, et al. The global distribution of the Duffy blood group. Nat Commun. 2011;2:266 10.1038/ncomms1265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenberg R. Plasmodium vivax in Africa: hidden in plain sight? Trends Parasitol. 2007;23(5):193–6. 10.1016/j.pt.2007.02.009 [DOI] [PubMed] [Google Scholar]
- 8.Mayne B. NOTE ON EXPERIMENTAL INFECTION OF ANOPHELES PUNCTIPENNIS WITH QUARTAN MALARIA. Public Health Reports 1932;47(35):1771–811. 10.2307/458087019315362 [DOI] [Google Scholar]
- 9.Boyd MF, Stratman-Thomas WK. STUDIES ON BENIGN TERTIAN MALARIA: 4. ON THE REFRACTORINESS OF NEGROES TO INOCULATION WITH PLASMODIUM VIVAX. American Journal of Epidemiology. 1933;18(2):485–9. [Google Scholar]
- 10.Young MD, Don EE, Burgess RW, Jeffery GM. Experimental Testing of the Immunity of Negroes to Plasmodium vivax. The Journal of Parasitology. 1955;41(3):315–8. 10.2307/3274214 [DOI] [PubMed] [Google Scholar]
- 11.Sanger R, Race RR, Jack J. The Duffy Blood Groups of New York Negroes: The Phenotype Fy (a−b−). British Journal of Haematology. 1955;1(4):370–4. 10.1111/j.1365-2141.1955.tb05523.x [DOI] [PubMed] [Google Scholar]
- 12.Miller L, Mason S, Dvorak J, McGinniss M, Rothman I. Erythrocyte receptors for (Plasmodium knowlesi) malaria: Duffy blood group determinants. Science. 1975;189(4202):561–3. 10.1126/science.1145213 [DOI] [PubMed] [Google Scholar]
- 13.Miller LH, Mason SJ, Clyde DF, McGinniss MH. The Resistance Factor to Plasmodium vivax in Blacks. N Engl J Med. 1976;295(6):302–4. 10.1056/NEJM197608052950602 . [DOI] [PubMed] [Google Scholar]
- 14.Ryan JR, Stoute JA, Amon J, Dunton RF, Mtalib R, Koros J, et al. Evidence for transmission of Plasmodium vivax among a duffy antigen negative population in Western Kenya. The American journal of tropical medicine and hygiene. 2006;75(4):575–81. [PubMed] [Google Scholar]
- 15.Ménard D, Barnadas C, Bouchier C, Henry-Halldin C, Gray LR, Ratsimbasoa A, et al. Plasmodium vivax clinical malaria is commonly observed in Duffy-negative Malagasy people. Proceedings of the National Academy of Sciences. 2010;107(13):5967–71. 10.1073/pnas.0912496107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bachelerie F, Ben-Baruch A, Burkhardt AM, Combadiere C, Farber JM, Graham GJ, et al. International Union of Basic and Clinical Pharmacology. [corrected]. LXXXIX. Update on the extended family of chemokine receptors and introducing a new nomenclature for atypical chemokine receptors. Pharmacol Rev. 2014;66(1):1–79. 10.1124/pr.113.007724 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horuk R, Chitnis CE, Darbonne WC, Colby TJ, Rybicki A, Hadley TJ, et al. A receptor for the malarial parasite Plasmodium vivax: the erythrocyte chemokine receptor. Science. 1993;261(5125):1182 10.1126/science.7689250 [DOI] [PubMed] [Google Scholar]
- 18.Chitnis C, Miller LH. Identification of the erythrocyte binding domains ofPlasmodium vivax and Plasmodium knowlesi proteins involved in erythrocyte invasion. Journal of Experimental Medicine. 1994;180:497–506. 10.1084/jem.180.2.497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Höher G, Fiegenbaum M, Almeida S. Molecular basis of the Duffy blood group system. Blood Transfus. 2018;16(1):93–100. Epub 01/30. 10.2450/2017.0119-16 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cutbush M, Mollison PL. The Duffy blood group system. Heredity (Edinb). 1950;4(3):383–9. Epub 1950/12/01. 10.1038/hdy.1950.31 . [DOI] [PubMed] [Google Scholar]
- 21.Ikin EW, Mourant AE, Pettenkofer HJ, Blumenthal G. Discovery of the expected haemagglutinin, anti-Fyb. Nature. 1951;168(4288):1077–8. Epub 1951/12/22. 10.1038/1681077b0 . [DOI] [PubMed] [Google Scholar]
- 22.Seixas S, Ferrand N, Rocha J. Microsatellite Variation and Evolution of the Human Duffy Blood Group Polymorphism. Mol Biol Evol. 2002;19(10):1802–6. 10.1093/oxfordjournals.molbev.a004003 [DOI] [PubMed] [Google Scholar]
- 23.Chaudhuri A, Polyakova J, Zbrzezna V, Pogo AO. The coding sequence of Duffy blood group gene in humans and simians: restriction fragment length polymorphism, antibody and malarial parasite specificities, and expression in nonerythroid tissues in Duffy- negative individuals. Blood. 1995;85(3):615 [PubMed] [Google Scholar]
- 24.Tournamille C, Colin Y, Cartron JP, Le Van Kim C. Disruption of a GATA motif in the Duffy gene promoter abolishes erythroid gene expression in Duffy-negative individuals. Nat Genet. 1995;10(2):224–8. 10.1038/ng0695-224 [DOI] [PubMed] [Google Scholar]
- 25.Tournamille C, Blancher A, Le Van Kim C, Gane P, Apoil PA, Nakamoto W, et al. Sequence, evolution and ligand binding properties of mammalian Duffy antigen/receptor for chemokines. Immunogenetics. 2004;55(10):682–94. 10.1007/s00251-003-0633-2 [DOI] [PubMed] [Google Scholar]
- 26.Li J, Iwamoto S, Sugimoto N, Okuda H, Kajii E. Dinucleotide repeat in the 3′ flanking region provides a clue to the molecular evolution of the Duffy gene. Hum Genet. 1997;99(5):573–7. 10.1007/s004390050408 [DOI] [PubMed] [Google Scholar]
- 27.Michon P, Woolley I, Wood EM, Kastens W, Zimmerman PA, Adams JH. Duffy-null promoter heterozygosity reduces DARC expression and abrogates adhesion of the P. vivax ligand required for blood-stage infection. FEBS Letters. 2001;495(1–2):111–4. 10.1016/s0014-5793(01)02370-5 [DOI] [PubMed] [Google Scholar]
- 28.Yazdanbakhsh K, Rios M, Storry JR, Kosower N, Parasol N, Chaudhuri A, et al. Molecular mechanisms that lead to reduced expression of Duffy antigens. Transfusion. 2000;40(3):310–20. 10.1046/j.1537-2995.2000.40030310.x [DOI] [PubMed] [Google Scholar]
- 29.Woolley IJ, Hotmire KA, Sramkoski RM, Zimmerman PA, Kazura JW. Differential expression of the Duffy antigen receptor for chemokines according to RBC age and FY genotype. Transfusion. 2000;40(8):949–53. 10.1046/j.1537-2995.2000.40080949.x [DOI] [PubMed] [Google Scholar]
- 30.Zimmerman PA, Woolley I, Masinde GL, Miller SM, McNamara DT, Hazlett F, et al. Emergence of FY*Anull in a Plasmodium vivax-endemic region of Papua New Guinea. Proceedings of the National Academy of Sciences. 1999;96(24):13973–7. 10.1073/pnas.96.24.13973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hamblin MT, Di Rienzo A. Detection of the signature of natural selection in humans: evidence from the Duffy blood group locus. Am J Hum Genet. 2000;66(5):1669–79. Epub 04/12. 10.1086/302879 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kasehagen LJ, Mueller I, Kiniboro B, Bockarie MJ, Reeder JC, Kazura JW, et al. Reduced Plasmodium vivax erythrocyte infection in PNG Duffy-negative heterozygotes. PLoS ONE. 2007;2(3):e336–e. 10.1371/journal.pone.0000336 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kano FS, de Souza AM, de Menezes Torres L, Costa MA, Souza-Silva FA, Sanchez BAM, et al. Susceptibility to Plasmodium vivax malaria associated with DARC (Duffy antigen) polymorphisms is influenced by the time of exposure to malaria. Scientific reports. 2018;8(1):13851–. 10.1038/s41598-018-32254-z . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.King CL, Adams JH, Xianli J, Grimberg BT, McHenry AM, Greenberg LJ, et al. Fy(a)/Fy(b) antigen polymorphism in human erythrocyte Duffy antigen affects susceptibility to Plasmodium vivax malaria. Proc Natl Acad Sci U S A. 2011;108(50):20113–8. 10.1073/pnas.1109621108 PMC3250126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Howes RE, Reiner RC Jr., Battle KE, Longbottom J, Mappin B, Ordanovich D, et al. Plasmodium vivax Transmission in Africa. PLoS Negl Trop Dis. 2015;9(11):e0004222–e. 10.1371/journal.pntd.0004222 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Twohig KA, Pfeffer DA, Baird JK, Price RN, Zimmerman PA, Hay SI, et al. Growing evidence of Plasmodium vivax across malaria-endemic Africa. PLoS Negl Trop Dis. 2019;13(1):e0007140–e. 10.1371/journal.pntd.0007140 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rubio JM, Benito A, Roche J, Berzosa PJ, García ML, Micó M, et al. Semi-nested, multiplex polymerase chain reaction for detection of human malaria parasites and evidence of Plasmodium vivax infection in Equatorial Guinea. The American Journal of Tropical Medicine and Hygiene. 1999;60(2):183–7. 10.4269/ajtmh.1999.60.183 [DOI] [PubMed] [Google Scholar]
- 38.Gautret P, Legros F, Koulmann P, Rodier MH, Jacquemin JL. Imported Plasmodium vivax malaria in France: geographical origin and report of an atypical case acquired in Central or Western Africa. Acta Trop. 2001;78(2):177–81. 10.1016/s0001-706x(00)00181-9 [DOI] [PubMed] [Google Scholar]
- 39.BLOSSOM DB, KING CH, ARMITAGE KB. OCCULT PLASMODIUM VIVAX INFECTION DIAGNOSED BY A POLYMERASE CHAIN REACTION–BASED DETECTION SYSTEM: A CASE REPORT. The American Journal of Tropical Medicine and Hygiene. 2005;73(1):188–90. 10.4269/ajtmh.2005.73.188. [DOI] [PubMed] [Google Scholar]
- 40.Culleton RL, Mita T, Ndounga M, Unger H, Cravo PVL, Paganotti GM, et al. Failure to detect Plasmodium vivax in West and Central Africa by PCR species typing. Malaria Journal. 2008;7(1):174 10.1186/1475-2875-7-174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abkallo HM, Liu W, Hokama S, Ferreira PE, Nakazawa S, Maeno Y, et al. DNA from pre-erythrocytic stage malaria parasites is detectable by PCR in the faeces and blood of hosts. Int J Parasit. 2014;44(7):467–73. 10.1016/j.ijpara.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 42.Culleton R, Ndounga M, Zeyrek FY, Coban C, Casimiro PN, Takeo S, et al. Evidence for the Transmission of Plasmodium vivax in the Republic of the Congo, West Central Africa. J Infect Dis. 2009;200(9):1465–9. 10.1086/644510 [DOI] [PubMed] [Google Scholar]
- 43.Bray RS. The Susceptibility of Liberians to the Madagascar Strain of Plasmodium vivax. The Journal of Parasitology. 1958;44(4):371–3. 10.2307/3274317 [DOI] [PubMed] [Google Scholar]
- 44.Battle K, Karhunen M, Bhatt S, Gething P, Howes R, Golding N, et al. Geographical variation in Plasmodium vivax relapse. Malaria Journal. 2014;13(1):144 10.1186/1475-2875-13-144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Garnham PC, Bray RS, Bruce-Chwatt LJ, Draper CC, Killick-Kendrick R, Sergiev PG, et al. A strain of Plasmodium vivax characterized by prolonged incubation: morphological and biological characteristics. Bulletin of the World Health Organization. 1975;52(1):21–32. . [PMC free article] [PubMed] [Google Scholar]
- 46.Lover AA. Note on the origin of the Madagascar strain of Plasmodium vivax. The American journal of tropical medicine and hygiene. 2014;91(6):1283–. 10.4269/ajtmh.14-0507 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Woldearegai TG, Kremsner PG, Kun JF, Mordmüller B. Plasmodium vivax malaria in Duffy-negative individuals from Ethiopia. Transactions of The Royal Society of Tropical Medicine and Hygiene. 2013;107(5):328–31. 10.1093/trstmh/trt016 [DOI] [PubMed] [Google Scholar]
- 48.Gunalan K, Lo E, Hostetler JB, Yewhalaw D, Mu J, Neafsey DE, et al. Role of Plasmodium vivax Duffy-binding protein 1 in invasion of Duffy-null Africans. Proc Natl Acad Sci U S A. 2016;113(22):6271–6. Epub 2016/05/18. 10.1073/pnas.1606113113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fru-Cho J, Bumah V, Safeukui I, Nkuo-Akenji T, Titanji V, Haldar K. Molecular typing reveals substantial Plasmodium vivax infection in asymptomatic adults in a rural area of Cameroon. Malaria Journal. 2014;13(1):170 10.1186/1475-2875-13-170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Niangaly A, Karthigayan G, Amed O, Coulibaly D, Sá JM, Adams M, et al. Plasmodium vivax Infections over 3 Years in Duffy Blood Group Negative Malians in Bandiagara, Mali. The American journal of tropical medicine and hygiene. 2017;97(3):744–52. Epub 07/24. 10.4269/ajtmh.17-0254 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Spencer HC, Miller LH, Collins WE, Knud-Hansen C, McGinnis MH, Shiroishi T, et al. The Duffy Blood Group and Resistance to Plasmodium Vivax in Honduras. The American Journal of Tropical Medicine and Hygiene. 1978;27(4):664–70. 10.4269/ajtmh.1978.27.664 [DOI] [PubMed] [Google Scholar]
- 52.Weppelmann TA, Carter TE, Chen Z, von Fricken ME, Victor YS, Existe A, et al. High frequency of the erythroid silent Duffy antigen genotype and lack of Plasmodium vivax infections in Haiti. Malaria Journal. 2013;12(1):30 10.1186/1475-2875-12-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cavasini CE, Pereira FJT, Ribeiro WL, Wunderlich G, Ferreira MU. Duffy blood group genotypes among malaria patients in Rondônia, Western Brazilian Amazon. Revista da Sociedade Brasileira de Medicina Tropical. 2001;34:591–5. 10.1590/s0037-86822001000600016 [DOI] [PubMed] [Google Scholar]
- 54.Sousa TN, Sanchez BAM, Cerávolo IP, Carvalho LH, Brito CFA. Real-time multiplex allele-specific polymerase chain reaction for genotyping of the Duffy antigen, the Plasmodium vivax invasion receptor. Vox Sanguinis. 2007;92(4):373–80. 10.1111/j.1423-0410.2007.00902.x [DOI] [PubMed] [Google Scholar]
- 55.Ginouves M, Veron V, Musset L, Legrand E, Stefani A, Prevot G, et al. Frequency and distribution of mixed Plasmodium falciparum-vivax infections in French Guiana between 2000 and 2008. Malaria Journal. 2015;14(1):446 10.1186/s12936-015-0971-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vallejo AF, Chaparro PE, Benavides Y, Álvarez Á, Quintero JP, Padilla J, et al. High prevalence of sub-microscopic infections in Colombia. Malaria Journal. 2015;14(1):201 10.1186/s12936-015-0711-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.HERRERA S, GÓMEZ A, VERA O, VERGARA J, VALDERRAMA-AGUIRRE A, MAESTRE A, et al. ANTIBODY RESPONSE TO PLASMODIUM VIVAX ANTIGENS IN FY-NEGATIVE INDIVIDUALS FROM THE COLOMBIAN PACIFIC COAST. The American Journal of Tropical Medicine and Hygiene. 2005;73(5_suppl):44–9. 10.4269/ajtmh.2005.73.44. [DOI] [PubMed] [Google Scholar]
- 58.Cavasini CE, Mattos LCd, Couto ÁADA, Bonini-Domingos CR, Valencia SH, Neiras WCdS, et al. Plasmodium vivax infection among Duffy antigen-negative individuals from the Brazilian Amazon region: an exception? Transactions of The Royal Society of Tropical Medicine and Hygiene. 2007;101(10):1042–4. 10.1016/j.trstmh.2007.04.011 [DOI] [PubMed] [Google Scholar]
- 59.Carvalho TA, Queiroz MG, Cardoso GL, Diniz IG, Silva AN, Pinto AY, et al. Plasmodium vivax infection in Anajas, State of Para: no differential resistance profile among Duffy-negative and Duffy-positive individuals. Malaria journal. 2012;11(1):430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bermúdez M, Moreno-Pérez DA, Arévalo-Pinzón G, Curtidor H, Patarroyo MA. Plasmodium vivax in vitro continuous culture: the spoke in the wheel. Malaria journal. 2018;17(1):301–. 10.1186/s12936-018-2456-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Noulin F, Borlon C, Van Den Abbeele J, D’Alessandro U, Erhart A. 1912–2012: a century of research on Plasmodium vivax in vitro culture. Trends Parasitol. 2013;29(6):286–94. 10.1016/j.pt.2013.03.012 [DOI] [PubMed] [Google Scholar]
- 62.Menard D, Chan ER, Benedet C, Ratsimbasoa A, Kim S, Chim P, et al. Whole Genome Sequencing of Field Isolates Reveals a Common Duplication of the Duffy Binding Protein Gene in Malagasy Plasmodium vivax Strains. PLoS Negl Trop Dis. 2013;7(11):e2489 10.1371/journal.pntd.0002489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Auburn S, Getachew S, Pearson R, Amato R, Miotto O, Trimarsanto H, et al. Genomic analysis of plasmodium vivax in southern Ethiopia reveals selective pressures in multiple parasite mechanisms. The Journal of Infectious Diseases. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lo E, Hostetler JB, Yewhalaw D, Pearson RD, Hamid MMA, Gunalan K, et al. Frequent expansion of Plasmodium vivax Duffy Binding Protein in Ethiopia and its epidemiological significance. PLoS Negl Trop Dis. 2019;13(9):e0007222 10.1371/journal.pntd.0007222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pearson RD, Amato R, Auburn S, Miotto O, Almagro-Garcia J, Amaratunga C, et al. Genomic analysis of local variation and recent evolution in Plasmodium vivax. Nature Genetics. 2016;48:959 10.1038/ng.3599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hostetler JB, Lo E, Kanjee U, Amaratunga C, Suon S, Sreng S, et al. Independent Origin and Global Distribution of Distinct Plasmodium vivax Duffy Binding Protein Gene Duplications. PLoS Negl Trop Dis. 2016;10(10):e0005091 10.1371/journal.pntd.0005091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roesch C, Popovici J, Bin S, Run V, Kim S, Ramboarina S, et al. Genetic diversity in two Plasmodium vivax protein ligands for reticulocyte invasion. PLoS Negl Trop Dis. 2018;12(10):e0006555–e. 10.1371/journal.pntd.0006555 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hoque MR, Elfaki MMA, Ahmed MA, Lee S-K, Muh F, Ali Albsheer MM, et al. Diversity pattern of Duffy binding protein sequence among Duffy-negatives and Duffy-positives in Sudan. Malaria Journal. 2018;17(1):297 10.1186/s12936-018-2425-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Galinski MR, Medina CC, Ingravallo P, Barnwell JW. A reticulocyte-binding protein complex of plasmodium vivax merozoites. Cell. 1992;69(7):1213–26. 10.1016/0092-8674(92)90642-p [DOI] [PubMed] [Google Scholar]
- 70.Chan L-J, Dietrich MH, Nguitragool W, Tham W-H. Plasmodium vivax Reticulocyte Binding Proteins for invasion into reticulocytes. Cell Microbiol. 0(0):e13110 10.1111/cmi.13110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gunalan K, Niangaly A, Thera MA, Doumbo OK, Miller LH. Plasmodium vivax Infections of Duffy-Negative Erythrocytes: Historically Undetected or a Recent Adaptation? Trends Parasitol. 2018;34(5):420–9. 10.1016/j.pt.2018.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.França CT, White MT, He W-Q, Hostetler JB, Brewster J, Frato G, et al. Identification of highly-protective combinations of Plasmodium vivax recombinant proteins for vaccine development. eLife. 2017;6:e28673 10.7554/eLife.28673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gupta ED, Anand G, Singh H, Chaddha K, Bharti PK, Singh N, et al. Naturally Acquired Human Antibodies Against Reticulocyte-Binding Domains of Plasmodium vivax Proteins, PvRBP2c and PvRBP1a, Exhibit Binding-Inhibitory Activity. The Journal of Infectious Diseases. 2017;215(10):1558–68. 10.1093/infdis/jix170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.França CT, He W-Q, Gruszczyk J, Lim NTY, Lin E, Kiniboro B, et al. Plasmodium vivax Reticulocyte Binding Proteins Are Key Targets of Naturally Acquired Immunity in Young Papua New Guinean Children. PLoS Negl Trop Dis. 2016;10(9):e0005014 10.1371/journal.pntd.0005014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gupta S, Singh S, Popovici J, Roesch C, Shakri AR, Guillotte-Blisnick M, et al. Targeting a Reticulocyte Binding Protein and Duffy Binding Protein to Inhibit Reticulocyte Invasion by Plasmodium vivax. Scientific reports. 2018;8(1):10511–. 10.1038/s41598-018-28757-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gruszczyk J, Kanjee U, Chan L-J, Menant S, Malleret B, Lim NTY, et al. Transferrin receptor 1 is a reticulocyte-specific receptor for Plasmodium vivax. Science (New York, NY). 2018;359(6371):48–55. 10.1126/science.aan1078 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.He W-Q, Karl S, White MT, Nguitragool W, Monteiro W, Kuehn A, et al. Antibodies to Plasmodium vivax reticulocyte binding protein 2b are associated with protection against P. vivax malaria in populations living in low malaria transmission regions of Brazil and Thailand. PLoS Negl Trop Dis. 2019;13(8):e0007596–e. 10.1371/journal.pntd.0007596 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Han J-H, Cheng Y, Muh F, Ahmed MA, Cho J-S, Nyunt MH, et al. Inhibition of parasite invasion by monoclonal antibody against epidermal growth factor-like domain of Plasmodium vivax merozoite surface protein 1 paralog. Scientific Reports. 2019;9(1):3906 10.1038/s41598-019-40321-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Han J-H, Cho J-S, Cheng Y, Muh F, Yoo WG, Russell B, et al. Plasmodium vivax Merozoite Surface Protein 1 Paralog as a Mediator of Parasite Adherence to Reticulocytes. Infect Immun. 2018;86(9):e00239–18. 10.1128/IAI.00239-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cheng Y, Lu F, Wang B, Li J, Han J-H, Ito D, et al. Plasmodium vivax GPI-anchored micronemal antigen (PvGAMA) binds human erythrocytes independent of Duffy antigen status. Scientific reports. 2016;6:35581–. 10.1038/srep35581 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hester J, Chan ER, Menard D, Mercereau-Puijalon O, Barnwell J, Zimmerman PA, et al. De Novo Assembly of a Field Isolate Genome Reveals Novel Plasmodium vivax Erythrocyte Invasion Genes. PLoS Negl Trop Dis. 2013;7(12):e2569 10.1371/journal.pntd.0002569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ntumngia FB, Thomson-Luque R, Torres LdM, Gunalan K, Carvalho LH, Adams JH. A Novel Erythrocyte Binding Protein of Plasmodium vivax Suggests an Alternate Invasion Pathway into Duffy-Positive Reticulocytes. mBio. 2016;7(4):e01261–16. 10.1128/mBio.01261-16 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pan B-T, Johnstone RM. Fate of the transferrin receptor during maturation of sheep reticulocytes in vitro: Selective externalization of the receptor. Cell. 1983;33(3):967–78. 10.1016/0092-8674(83)90040-5 [DOI] [PubMed] [Google Scholar]
- 84.Malleret B, Xu F, Mohandas N, Suwanarusk R, Chu C, Leite JA, et al. Significant Biochemical, Biophysical and Metabolic Diversity in Circulating Human Cord Blood Reticulocytes. PLoS ONE. 2013;8(10):e76062 10.1371/journal.pone.0076062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dechavanne C, Dechavanne S, Metral S, Roeper B, Krishnan S, Fong R, et al. Duffy Antigen Expression in Erythroid Bone Marrow Precursor Cells of Genotypically Duffy Negative Individuals. bioRxiv. 2018:508481 10.1101/508481 [DOI] [Google Scholar]
- 86.Malleret B, Li A, Zhang R, Tan KSW, Suwanarusk R, Claser C, et al. Plasmodium vivax: restricted tropism and rapid remodeling of CD71-positive reticulocytes. Blood. 2015;125(8):1314–24. Epub 11/20. 10.1182/blood-2014-08-596015 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Obaldia N 3rd, Meibalan E, Sa JM, Ma S, Clark MA, Mejia P, et al. Bone Marrow Is a Major Parasite Reservoir in Plasmodium vivax Infection. mBio. 2018;9(3):e00625–18. 10.1128/mBio.00625-18 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Peiper SC, Wang ZX, Neote K, Martin AW, Showell HJ, Conklyn MJ, et al. The Duffy antigen/receptor for chemokines (DARC) is expressed in endothelial cells of Duffy negative individuals who lack the erythrocyte receptor. The Journal of experimental medicine. 1995;181(4):1311–7. 10.1084/jem.181.4.1311 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lo E, Yewhalaw D, Zhong D, Zemene E, Degefa T, Tushune K, et al. Molecular epidemiology of Plasmodium vivax and Plasmodium falciparum malaria among Duffy-positive and Duffy-negative populations in Ethiopia. Malaria journal. 2015;14:84–. 10.1186/s12936-015-0596-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gunalan K, Sá JM, Moraes Barros RR, Anzick SL, Caleon RL, Mershon JP, et al. Transcriptome profiling of Plasmodium vivax in Saimiri monkeys identifies potential ligands for invasion. Proceedings of the National Academy of Sciences. 2019;116(14):7053 10.1073/pnas.1818485116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mohring F, Hart MN, Rawlinson TA, Henrici R, Charleston JA, Diez Benavente E, et al. Rapid and iterative genome editing in the malaria parasite Plasmodium knowlesi provides new tools for P. vivax research. eLife. 2019;8:e45829 10.7554/eLife.45829 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chua ACY, Ong JJY, Malleret B, Suwanarusk R, Kosaisavee V, Zeeman A-M, et al. Robust continuous in vitro culture of the Plasmodium cynomolgi erythrocytic stages. Nature communications. 2019;10(1):3635–. 10.1038/s41467-019-11332-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Russell B, Suwanarusk R, Borlon C, Costa FTM, Chu CS, Rijken MJ, et al. A reliable ex vivo invasion assay of human reticulocytes by Plasmodium vivax. Blood. 2011;118(13):e74–e81. 10.1182/blood-2011-04-348748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Urusova D, Carias L, Huang Y, Nicolete VC, Popovici J, Roesch C, et al. Structural basis for neutralization of Plasmodium vivax by naturally acquired human antibodies that target DBP. Nature Microbiology. 2019;4(9):1486–96. 10.1038/s41564-019-0461-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Prajapati SK, Borlon C, Rovira-Vallbona E, Gruszczyk J, Menant S, Tham W-H, et al. Complement Receptor 1 availability on red blood cell surface modulates Plasmodium vivax invasion of human reticulocytes. Scientific reports. 2019;9(1):8943–. 10.1038/s41598-019-45228-6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Scully EJ, Shabani E, Rangel GW, Gruring C, Kanjee U, Clark MA, et al. Generation of an immortalized erythroid progenitor cell line from peripheral blood: A model system for the functional analysis of Plasmodium spp. invasion. Am J Hematol. 2019. Epub 2019/05/31. 10.1002/ajh.25543 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Weiss DJ, Lucas TCD, Nguyen M, Nandi AK, Bisanzio D, Battle KE, et al. Mapping the global prevalence, incidence, and mortality of Plasmodium falciparum, 2000–17: a spatial and temporal modelling study. The Lancet. 2019. 10.1016/S0140-6736(19)31097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lover AA, Baird JK, Gosling R, Price RN. Malaria Elimination: Time to Target All Species. The American Journal of Tropical Medicine and Hygiene. 2018;99(1):17–23. 10.4269/ajtmh.17-0869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Singh K, Mukherjee P, Shakri AR, Singh A, Pandey G, Bakshi M, et al. Malaria vaccine candidate based on Duffy-binding protein elicits strain transcending functional antibodies in a Phase I trial. NPJ vaccines. 2018;3:48-. 10.1038/s41541-017-0043-3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Payne RO, Silk SE, Elias SC, Milne KH, Rawlinson TA, Llewellyn D, et al. Human vaccination against Plasmodium vivax Duffy-binding protein induces strain-transcending antibodies. JCI Insight. 2017;2(12):e93683 10.1172/jci.insight.93683 . [DOI] [PMC free article] [PubMed] [Google Scholar]