Abstract
Aims.
To examine the lifetime prevalence and risk of psychiatric disorders associated with natural and man-made disaster exposure in Australia.
Methods.
We utilised data from a nationally representative population survey (N = 8841) which were analysed through univariate and multivariate logistic regression in order to examine the full spectrum of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) affective, anxiety and substance use disorders associated with exposure to natural and man-made disaster.
Results.
Man-made disaster exposure was primarily associated with an increased lifetime risk (odds ratio (95% CI)) of alcohol abuse disorder 2.29 (1.56–3.37), post-traumatic stress disorder (PTSD) 2.27 (1.36–3.79), obsessive–compulsive disorder (OCD) 1.95 (1.08–3.51) and major depressive disorder 1.69 (1.01–2.85). Multiple natural disaster exposure was associated with an increased lifetime risk of panic disorder 2.26 (1.11–4.61). Among the broader disorder spectrum examined, alcohol abuse disorder accounted for the single greatest increase in lifetime disorder prevalence associated with man-made disaster exposure, and the greatest number of natural or man-made disaster exposed individuals who had developed a lifetime psychiatric disorder. Despite the relatively greater disorder risk associated with man-made disaster, natural disaster exposure was associated with more cases of psychiatric disorder, likely due to the frequency with which these events occur in Australia.
Conclusions.
Notwithstanding the inability to draw causal inferences from cross-sectional survey data, population-based analyses provide a comprehensive and consistent method to ascertain the population imprint of psychiatric disorder and disaster exposure. Mental health policy and services should be targeting a range of psychiatric disorders in disaster contexts in addition to the usual focus on PTSD and depression, including alcohol abuse, panic disorder and OCD. Despite the relatively greater disorder risk associated with man-made disaster exposure, the national burden of psychiatric disorder in natural disaster contexts is particularly high.
Key words: Disasters, epidemiology, mental health, trauma, population survey
Introduction
Australia is exposed to a range of natural and man-made hazards, which impact on the health and wellbeing of its population. Natural hazards common to Australia primarily include floods, bushfires, cyclones, severe storms, droughts and heatwaves, and to a lesser extent earthquakes and tsunamis. Simultaneously, the country is exposed to a range of man-made hazards, which include technological accidents, such as fires, explosions and structural collapses; chemical, biological and radiological hazards; transport accidents; mass shootings; and acts of terrorism. Research has shown that approximately 8.4% of Australians are involved in major natural disasters and 4.8% in man-made disasters over their lifetime (Mills et al. 2011). In view of the increasing impacts of global climate change on the frequency and intensity of extreme climatic events and growing global and domestic concern with the threat of terrorism, there is a need for a comprehensive assessment of the national burden which exposure to natural and man-made disasters has on the mental health of the population.
Yet, surprisingly, despite advancing clinical and epidemiological insights into the mental health consequences of major disaster events (including into individual risk and protective factors for varied mental health outcomes and disorder trajectories), whole or population-based assessments of the psychiatric imprint of disaster exposure are not readily available today. Comprehensive national estimates of the psychiatric burden of disaster exposure are therefore currently reliant on either indirect or partial inferences from event-specific disaster studies (which tend to vary in focus and methodology), insights from international literature reviews (of specific event or disorder types), or comparative cross-national studies focussed on specific disorders (Bromet et al. 2017). This, in turn, provides an obstacle to the adequate recognition of the full spectrum and national burden of disaster mental health outcomes, the associated prioritisation and allocation of health resources, and the development of a proactive and targeted approach to disaster risk reduction and national health preparedness planning.
Reviews of international disaster mental health research indicate that while a majority of disaster affected individuals may typically experience transitory mild-to-moderate levels of distress, and recovery can generally be considered the norm rather than the exception for most, a significant minority will go on to develop more severe diagnosable mental disorders (Bonanno et al. 2010; Norris et al. 2002). Among the latter, post-traumatic stress disorder (PTSD), and to a lesser extent, major depressive disorder (MDD), have traditionally been the most frequently investigated and identified mental health outcomes in disaster contexts (Galea et al. 2005; Bonde et al. 2016), while other anxiety, affective and substance use disorders have received relatively little attention (North, 2007; McFarlane et al. 2009). Post-disaster PTSD prevalence rates have commonly been found to range between 5 and 10% in the general population and 30 and 40% among direct disaster victims (Galea et al. 2005), with greater odds (odds ratio (OR) 3.3, 95% CI 1.1–9.7) typically observed among those exposed to man-made rather than natural disasters (Bromet et al. 2017). Elevated odds of depressive disorder have equally been noted in natural (OR 2.28, 95% CI 1.30–3.98) and man-made (OR 1.47, 95% CI 1.30–1.65) disaster contexts (Bonde et al. 2016). Nevertheless, a growing body of evidence indicates that a whole range of psychiatric disorders can emerge with an increased risk following disastrous events (McFarlane & Williams, 2012). These arguments are therefore indicative of the need to investigate a wider range of psychiatric disorders in disaster contexts.
Previous research further indicates that constellations of traumatic event exposure and mental disorder prevalence can differ substantially between countries, and that besides traumatic event exposure, socioeconomic country context characteristics are important predictors for the variation in disorder prevalence between countries. Australia is, like New Zealand and the United States, a country with a relatively high level of trauma exposure, low socioeconomic vulnerability and high mental disorder prevalence (Kessler et al. 2009; Benjet et al. 2016; Dückers & Brewin, 2016; Dückers et al. 2016). This justifies a deeper analysis of presenting patterns of disaster exposure and mental disorder prevalence in nationally representative population samples, while at the same time controlling for the relative weight of risk and protective factors in the context of the sample and the event type.
In moving beyond a focus on specific disorders or single disaster events, the current study therefore seeks to develop a nationally representative picture of the full spectrum of psychiatric disorders to document the population imprint of disaster exposure. To this end, this study utilised nationally representative survey data and a consistent diagnostic algorithm to examine the lifetime prevalence and risk of psychiatric disorders that are associated with both natural and man-made disaster exposure in Australia.
Method
Data source
This study utilised data from the second National Survey of Mental Health and Wellbeing (NSMHWB), which was conducted by the Australian Bureau of Statistics (ABS) in 2007 (Australian Bureau of Statistics, 2009). This nationally representative, cross-sectional population survey employed random-stratified, multistage area probability sampling of persons aged 16–85 years who were the usual residents of private dwellings (such as houses, flats, home units or other private residence structures). A total of 14 805 private dwellings were included in the survey from an initial random sample of 17 352 households, after excluding those that were ineligible or out of scope. One eligible person in each household was randomly selected to complete the interview (with a higher chance of selection for those aged 16–24 and 65–85 years to improve the reliability of estimates for these groups). ABS-trained lay interviewers conducted computer-assisted, face-to-face interviews, which took on average 90 min to complete. Further detail on the sampling design and survey procedure can be found in the NSMHWB users’ guide (Australian Bureau of Statistics, 2009). The NSMHWB was completed by 8841 respondents, representing a response rate of 60% (Slade et al. 2009).
The base interview underpinning the NSMHWB was the Composite International Diagnostic Interview version 3.0 of the World Health Organization's World Mental Health Survey Initiative (WMH-CIDI 3.0) (Kessler & Ustün, 2004). The WMH-CIDI 3.0 is a fully structured interview for adults which assesses the prevalence of selected psychiatric disorders and their impact on day-to-day activities. The WMH-CIDI 3.0 provides an assessment of psychiatric disorders based on the definitions and diagnostic criteria specified in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). The WMH-CIDI 3.0 assesses key variables of relevance to this study, including: (a) the lifetime prevalence of DSM-IV psychiatric (i.e. affective, anxiety and substance use) disorders, (b) lifetime exposure to potentially traumatic events (including natural and man-made disasters), and (c) sociodemographic characteristics (i.e. age, gender, country of birth, marital status, qualification, labour force status, household location and relative socioeconomic disadvantage). Standard DSM-IV diagnostic algorithms, criteria and exclusion rules were applied to derive DSM-IV diagnoses. Wherever diagnostic hierarchy rules had been specified for psychiatric disorders (which precluded the diagnosis of a particular disorder on the basis that it had been accounted for by the presence of another disorder), we generally applied these diagnostic hierarchy rules in our analysis to derive accurate estimates.
Sociodemographic sample characteristics (unweighted) included: mean age 46.3 (range 16–85) years, gender (54.5% female, 45.5% male), country of birth (73.9% Australia, 11.7% main English speaking countries, 14.5% elsewhere), marital status (45.3% married, 32.7% never married, 22.0% previously married), qualification (55.7% holding a qualification or degree above school-level), labour force status (62.2% employed, 35.4% not in labour force, 2.4% unemployed) and household location (64.3% major urban, 23.2% other urban, 12.5% other). For further information on NSMHWB sample characteristics, readers are referred to (Slade et al. 2009; Reifels et al. Forthcoming).
Exposure variables
Type and frequency of natural or man-made disaster exposure were assessed by asking each survey respondent: ‘Were you ever involved in a major natural disaster, like a devastating flood, cyclone, or earthquake?’, ‘Were you ever in a man-made disaster, like a fire started by a cigarette, or a bomb explosion?’ and ‘How many times (did that happen in your life)?’, for each of those events. Two binary exposure variables were created representing the type of disaster exposure: man-made (coded yes = 1 or no = 0) and natural (coded yes = 1 or no = 0). Two categorical exposure variables represented the frequency (or level) of exposure to each respective disaster type: man-made (coded 0, 1, ‘2 or more’) and natural (coded 0, 1, ‘2 or more’). We refer to the former binary variables as ‘types’ of disaster exposure and to the latter categorical variables as ‘levels’ of disaster exposure.
An additional binary variable was created to control for exposure to other types of traumatic life events (coded yes = 1 or no = 0), reflecting the presence or absence of lifetime exposure to at least one of 27 ‘other’ potentially traumatic events that are assessed within the WMH-CIDI 3.0, irrespective of man-made or natural disaster exposure (Mills et al. 2011; Benjet et al. 2016). The WMH-CIDI 3.0 incorporates a DSM-IV PTSD module which enquires about lifetime exposure to 29 types of traumatic events, including natural and man-made disasters and accidents; combat, war and refugee experiences; sexual and interpersonal violence; witnessing or perpetrating violence; death or trauma to a loved one; as well as any other private or extremely traumatic event which the person may have experienced.
Outcome variables
The diagnostic spectrum of outcome variables covered three classes of DSM-IV lifetime psychiatric disorder: (a) affective disorders (MDD, dysthymia, bipolar affective disorder); (b) anxiety disorders (PTSD, generalised anxiety disorder, obsessive–compulsive disorder (OCD), panic disorder, agoraphobia, social phobia) and (c) substance use disorders (abuse and dependence derived separately for alcohol, cannabis, opioids, sedatives and stimulants). Each binary outcome variable was coded yes = 1 or no = 0 to reflect the presence or absence of respective lifetime psychiatric disorders.
Statistical analyses
Descriptive analyses were conducted to estimate the lifetime population prevalence of DSM-IV psychiatric disorders associated with natural or man-made disaster exposure. In addition, univariate and multivariate logistic regression analyses were conducted to examine the differential lifetime risk of DSM-IV psychiatric disorders associated with different types and levels of disaster exposure. Results of all univariate analyses are presented as crude ORs and results of all multivariate analyses as adjusted ORs (AORs).
The first set of multivariate regression analyses (model 1) examined the risk of DSM-IV lifetime psychiatric disorders associated with different ‘types’ of disaster exposure (i.e. natural or man-made), controlling for both types of disaster exposure, all sociodemographic variables listed above and for the likelihood of exposure to any other type of traumatic event.
The second set of multivariate regression analyses (model 2) examined the risk of DSM-IV lifetime psychiatric disorders associated with different ‘levels’ of natural or man-made disaster exposure, controlling for both natural and man-made disaster exposure levels, all sociodemographic variables and exposure to any other traumatic event. Thus, models 1 and 2 were largely identical and only differed in terms of the disaster exposure variables considered, with the former utilising binary and the latter categorical disaster exposure variables.
To explore the population imprint of disaster exposure in more depth, two more comparative analyses were conducted. The first examined relative changes in the prevalence rates of various psychiatric disorders that are associated with exposure to natural or man-made disaster. Resulting percentage differences in disorder prevalence rates (between those exposed, relative to those not exposed, to respective disaster types) were charted to enable comparison. In addition, we calculated and charted population estimates of the total number of Australians affected by each disaster type who had developed lifetime psychiatric disorders (with standard error bars provided).
All prevalence estimates and measures of association were weighted to account for differential response patterns in the population, the inverse probability of an individual being sampled and to conform to independent population estimates of national census data. The weighting procedure involved the application of 60 ABS provided person-level replicate weights, which were calibrated against independent population benchmarks in terms of age, gender, state/territory, part of state, educational attainment, labour force status and household composition (Australian Bureau of Statistics, 2009). Standard errors for population estimates were calculated through delete-a-group jack-knife variance technique. All analyses were conducted using STATA 13 (StataCorp, College Station, Texas, USA).
Results
Natural and man-made disaster exposure in Australia
Weighted population estimates indicated that Australians were overall more likely to be exposed to natural rather than man-made disasters, with 8.4 and 4.8%, respectively, involved in these events over their lifetime. Among those involved in respective disaster types, 67.5% had experienced one, and 32.5% multiple (‘two or more’), natural disasters, while 64.4% had experienced one, and 35.6% multiple, man-made disasters. Man-made disaster exposed individuals tended to be involved in a greater number of disaster events ( = 7.7, 95% CI 3.85–11.59, s.e. 1.93) than those exposed to natural disaster (
= 7.7, 95% CI 3.85–11.59, s.e. 1.93) than those exposed to natural disaster ( = 2.7, 95% CI 1.69–3.61, s.e. 0.48).
= 2.7, 95% CI 1.69–3.61, s.e. 0.48).
Prevalence and risk of lifetime psychiatric disorders
Tables 1–3 present data on the lifetime population prevalence and risk of DSM-IV psychiatric disorders that are associated with natural and man-made disaster exposure in Australia. Overall, almost 45% of participants exposed to natural disaster and 54% of those exposed to man-made disaster had developed a lifetime psychiatric disorder (compared with 41%, respectively, of those not exposed).
Table 1.
Lifetime prevalence and risk of any DSM-IV psychiatric, affective, anxiety and substance use disorder associated with disaster exposure (univariate logistic regression analyses)
| Any lifetime Psychiatric disordera,b |
Any lifetime Affective disordera,b |
Any lifetime Anxiety disordera,b |
Any lifetime Substance use disordera |
|||||
|---|---|---|---|---|---|---|---|---|
| Predictor | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) |
| ND exposure | ||||||||
| No | 41.19 | 1.00 | 14.22 | 1.00 | 19.63 | 1.00 | 23.86 | 1.00 |
| Yes | 44.58 | 1.15 (0.93–1.42) | 16.04 | 1.15 (0.83–1.61) | 23.55 | 1.26 (0.98–1.62) | 28.43 | 1.27 (0.94–1.70) |
| 0 | 41.19 | 1.00 | 14.22 | 1.00 | 19.63 | 1.00 | 23.86 | 1.00 |
| 1 | 42.90 | 1.07 (0.82–1.41) | 15.93 | 1.14 (0.74–1.77) | 23.03 | 1.22 (0.89–1.68) | 27.13 | 1.19 (0.83–1.71) |
| 2 or more | 48.42 | 1.34 (0.93–1.93) | 16.40 | 1.18 (0.75–1.87) | 24.82 | 1.35 (0.89–2.04) | 31.34 | 1.46 (0.92–2.30) |
| MD exposure | ||||||||
| No | 40.86 | 1.00 | 14.00 | 1.00 | 19.54 | 1.00 | 23.50 | 1.00 |
| Yes | 53.65 | 1.67** (1.21–2.32) | 21.82 | 1.71* (1.07–2.74) | 28.21 | 1.62* (1.10–2.38) | 38.92 | 2.07*** (1.49–2.89) |
| 0 | 40.86 | 1.00 | 14.00 | 1.00 | 19.54 | 1.00 | 23.50 | 1.00 |
| 1 | 55.39 | 1.80** (1.17–2.76) | 20.42 | 1.58 (0.91–2.73) | 31.64 | 1.91* (1.17–3.12) | 39.99 | 2.17** (1.34–3.52) |
| 2 or more | 46.94 | 1.28 (0.78–2.11) | 18.44 | 1.39 (0.80–2.41) | 25.75 | 1.43 (0.82–2.49) | 31.28 | 1.48 (0.89–2.46) |
ND, natural disaster; MD, man-made disaster; OR, odds ratio; CI, confidence interval.
Weighted population estimates.
DSM-IV diagnostic hierarchy rules applied.
Significance level: *p < 0.05; **p < 0.01; ***p < 0.001.
Table 2.
Lifetime prevalence and risk of DSM-IV affective and anxiety disorders associated with disaster exposure (univariate logistic regression analyses)
| Lifetime Major depressive disordera,b |
Lifetime PTSDa |
Lifetime OCDa |
Lifetime Panic disordera,c |
|||||
|---|---|---|---|---|---|---|---|---|
| Predictor | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) |
| ND exposure | ||||||||
| No | 12.68 | 1.00 | 7.06 | 1.00 | 3.60 | 1.00 | 2.53 | 1.00 |
| Yes | 14.67 | 1.18 (0.83–1.69) | 8.93 | 1.29 (0.90–1.85) | 5.64 | 1.60 (0.93–2.75) | 5.10 | 2.07 (0.99–4.32) |
| 0 | 12.68 | 1.00 | 7.06 | 1.00 | 3.60 | 1.00 | 2.53 | 1.00 |
| 1 | 14.48 | 1.17 (0.73–1.87) | 8.49 | 1.22 (0.73–2.03) | 5.40 | 1.53 (0.77–3.05) | 4.90 | 1.99 (0.65–6.09) |
| 2 or more | 15.19 | 1.23 (0.77–1.96) | 9.89 | 1.44 (0.84–2.47) | 6.17 | 1.76 (0.69–4.50) | 5.53 | 2.26* (1.11–4.61) |
| MD exposure | ||||||||
| No | 12.51 | 1.00 | 6.86 | 1.00 | 3.62 | 1.00 | 2.64 | 1.00 |
| Yes | 19.50 | 1.69* (1.01–2.85) | 14.34 | 2.27** (1.36–3.79) | 6.82 | 1.95* (1.08–3.51) | 4.84 | 1.88 (0.49–7.22) |
| 0 | 12.51 | 1.00 | 6.86 | 1.00 | 3.62 | 1.00 | 2.64 | 1.00 |
| 1 | 17.79 | 1.51 (0.82–2.81) | 14.47 | 2.30* (1.03–5.12) | 6.60 | 1.88 (0.85–4.15) | 6.00 | 2.36 (0.33–16.77) |
| 2 or more | 16.30 | 1.36 (0.72–2.56) | 15.51 | 2.49** (1.48–4.20) | 8.37 | 2.44* (1.03–5.76) | 3.55 | 1.36 (0.38–4.88) |
ND, natural disaster; MD, man-made disaster; PTSD, post-traumatic stress disorder; OCD, obsessive–compulsive disorder; OR, odds ratio; CI, confidence interval.
Weighted population estimates.
DSM-IV diagnostic hierarchy rules applied.
DSM-IV panic disorder without agoraphobia.
Note: Affective and anxiety disorders not significantly associated with disaster exposure reported in online Supplementary Information.
Significance level: *p < 0.05; **p < 0.01.
Table 3.
Lifetime prevalence and risk of DSM-IV substance use disorders associated with disaster exposure (univariate logistic regression analyses)
| Lifetime Alcohol abuse disordera,b |
Lifetime Cannabis abuse disordera,b |
Lifetime Stimulant abuse disordera,b |
||||
|---|---|---|---|---|---|---|
| Predictor | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) |
| ND exposure | ||||||
| No | 17.97 | 1.00 | 4.33 | 1.00 | 1.92 | 1.00 |
| Yes | 22.19 | 1.30 (0.93–1.81) | 4.26 | 0.98 (0.58–1.67) | 2.04 | 1.06 (0.56–2.02) |
| 0 | 17.97 | 1.00 | 4.33 | 1.00 | 1.92 | 1.00 |
| 1 | 21.09 | 1.22 (0.80–1.83) | 5.41 | 1.26 (0.72–2.22) | 2.07 | 1.08 (0.49–2.39) |
| 2 or more | 24.65 | 1.49 (0.92–2.43) | 1.91 | 0.43 (0.16–1.16) | 1.99 | 1.04 (0.40–2.67) |
| MD exposure | ||||||
| No | 17.59 | 1.00 | 4.30 | 1.00 | 1.88 | 1.00 |
| Yes | 32.82 | 2.29*** (1.56–3.37) | 4.73 | 1.10 (0.62–1.96) | 2.88 | 1.54 (0.75–3.18) |
| 0 | 17.59 | 1.00 | 4.30 | 1.00 | 1.88 | 1.00 |
| 1 | 34.14 | 2.43*** (1.44–4.08) | 6.15 | 1.46 (0.81–2.61) | 4.40 | 2.40* (1.14–5.04) |
| 2 or more | 24.39 | 1.51 (0.87–2.61) | 2.96 | 0.68 (0.20–2.31) | 0.62 | 0.32*** (0.18–0.58) |
ND, natural disaster; MD, man-made disaster; OR, odds ratio; CI, confidence interval.
Weighted population estimates.
DSM-IV diagnostic hierarchy rules applied.
Note: Substance use disorders not significantly associated with disaster exposure reported in online Supplementary Information.
Risk estimates for stimulant abuse disorder (by MD exposure level) are based on 59 completed (out of a possible total of 60) jack-knife replications.
Significance level: *p < 0.05; ***p < 0.001.
Univariate analyses indicated that only man-made (but not natural) disaster exposure was associated with an elevated risk (OR) of any lifetime psychiatric (1.67), affective (1.71), anxiety (1.62) and substance use (2.07) disorder. More specifically, man-made disaster exposure was linked to an increased lifetime risk of major depressive (1.69), post-traumatic stress (2.27) and OCDs (1.95), while single man-made disaster exposure was associated with an increased lifetime risk of alcohol abuse (2.43) and stimulant abuse (2.40) disorder. While exposure to a single natural disaster was not associated with an increased risk of disorder, exposure to multiple (i.e. ‘two or more’) natural disasters was associated with an increased lifetime risk of panic disorder (2.26). Cumulative effects of repeated man-made disaster exposure were also noted in terms of an increased lifetime risk of OCD (2.44) and decreased lifetime risk of stimulant abuse (0.32) disorder. Further information on the lifetime prevalence rates and risk of other DSM-IV affective, anxiety and substance use disorders (which were not significantly elevated in the context of disaster exposure) is available in online Supplementary Material, Tables S1–S4.
Multivariate analyses (model 1, online Supplementary Tables S5–7) that controlled for sociodemographic variables, respective ‘types’ of disaster exposure and exposure to any other traumatic event, confirmed that an elevated risk of any lifetime affective (AOR 1.67, 95% CI (1.01–2.78), p = 0.047), anxiety (AOR 1.62, 95% CI (1.09–2.40), p = 0.018) and substance use (AOR 1.61, 95% CI (1.06–2.43), p = 0.025) disorder is associated with exposure to man-made disaster. More specifically, man-made disaster exposure was linked to an increased risk of lifetime OCD (AOR 1.93, 95% CI (1.08–3.44), p = 0.026) and alcohol abuse (AOR 1.72, 95% CI (1.11–2.67), p = 0.016) disorder.
Similarly, when considering ‘levels’ of disaster exposure (model 2, online Supplementary Tables S5–7), an increased risk of any lifetime anxiety (AOR 1.88, 95% CI (1.10–3.20), p = 0.021), and substance use (AOR 1.84, 95% CI (1.07–3.17), p = 0.029) disorder, as well as, more specifically, of alcohol abuse disorder (AOR 2.04, 95% CI (1.17–3.54), p = 0.012), was found to be associated with single (but not multiple) man-made disaster exposure. Multiple man-made disaster exposure was associated with an increased lifetime risk of OCD (AOR 2.34, 95% CI (1.00–5.45), p = 0.050). No other associations identified in univariate analyses proved to be significant in multivariate analyses when controlling for the full set of predictor variables under model 1 or 2, partly due to insufficient observations to calculate jack-knife standard errors.
By way of sensitivity analysis of lifetime data, additional multivariate analyses were conducted to examine the 12-month risk of respective disorders in models 1 and 2. Multivariate regression results (shown in online Supplementary Table S8) confirmed that an elevated 12-month risk of any DSM-IV psychiatric disorder, any DSM-IV anxiety disorder and more specifically, of PTSD and OCD was associated with man-made disaster exposure. The 12-month risk of OCD was equally elevated in natural disaster contexts, and the 12-month risk of alcohol dependence decreased in man-made disaster contexts.
Exploring the population imprint of disaster exposure
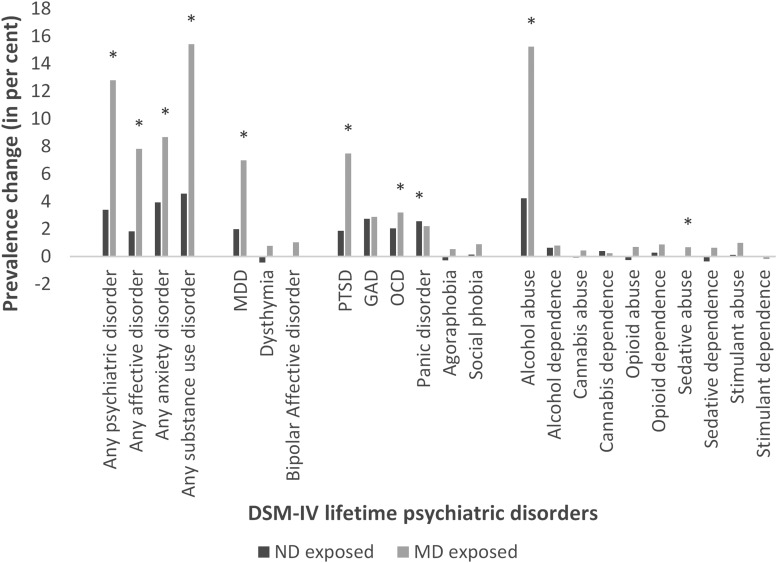
Figure 1 shows relative lifetime percentage increases or decreases in the prevalence rates of various psychiatric disorders that are associated with exposure to natural or man-made disaster (i.e. reflecting the difference in disorder prevalence rates between those exposed, relative to those not exposed, to respective disaster types).
Fig. 1.
Relative prevalence increase in DSM-IV lifetime psychiatric disorders associated with disaster exposure (representing the percentage difference in the prevalence rates of lifetime psychiatric disorders between those exposed, relative to those not exposed to disaster); ‘*’ denotes significant prevalence increase (p < 0.05).
While not all prevalence rate changes associated with disaster exposure were statistically significant, the vast majority were in the direction of a general increase in lifetime disorder prevalence, and typically more pronounced for man-made disasters. Largest prevalence increases in relation to man-made disaster exposure (p < 0.05) were noted for substance use disorders (most notably, alcohol abuse disorder), followed by anxiety (PTSD and OCD), and affective (MDD) disorders. By contrast, the only significant prevalence increase in the context of natural disaster exposure was noted for panic disorder (p < 0.05).
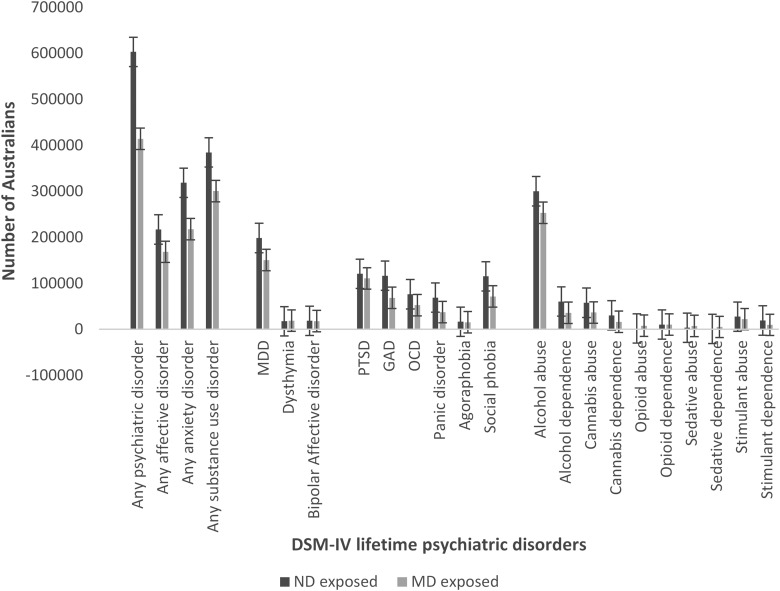
Figure 2 presents weighted population estimates of the total number of disaster-affected Australians who had developed lifetime psychiatric disorders. Contrasting with findings on the relatively greater increase in disorder prevalence associated with man-made disaster exposure (Fig. 1), the overall greatest number of disaster-affected Australians who had developed lifetime psychiatric disorders had been exposed to natural disasters n = 602 975 (s.e. = 49 992), compared with n = 414 061 (s.e. = 43 289) of those exposed to man-made disasters. This latter finding would be expected in view of the overall greater likelihood of natural disaster exposure. Both types of disaster exposure were most frequently associated with lifetime substance use disorders, followed by anxiety, and affective disorders.
Fig. 2.
Total number of disaster-affected Australians who develop lifetime psychiatric disorders (Note: weighted population estimates; error bars represent standard errors).
Discussion
Our study findings confirm central disaster mental health correlates identified in event-specific studies and international literature reviews, and highlight the importance of increasing attention to the broader range of psychiatric disorders. Consistent with international literature reviews, post-traumatic stress and MDDs featured as prominent psychiatric correlates of man-made disaster exposure among Australians (Galea et al. 2005; Bonde et al. 2016). However, due to their increased risk and prevalence in disaster exposure contexts, alcohol abuse, OCD and panic disorders may warrant increasing research and attention in future.
Within the broader range of psychiatric disorders associated with disaster, alcohol abuse disorder accounted for the single greatest increase in lifetime disorder prevalence associated with man-made disaster exposure, as well as the greatest number of natural or man-made disaster exposed Australians who had developed a lifetime psychiatric disorder. Disasters have rarely been found to be accompanied by large increases in the prevalence of substance use disorders, and increased post-disaster alcohol abuse can often reflect an exacerbation of existing use rather than new onset disorders (Van der Velden & Kleber, 2009). Yet, while the current study did not distinguish pre-existing from post-disaster alcohol abuse, the overall strength of the association of disaster exposure and lifetime alcohol abuse is noteworthy and indicative of a significant degree of attention that should be devoted to alcohol use disorders in future Australian disaster contexts.
The elevation in the prevalence of OCD within the context of disaster exposure is an interesting finding. Phenomenologically, recurrent and persistent thoughts that make up the obsessions criteria for OCD may look similar to the intrusive cluster of symptoms in PTSD (Dykshoorn, 2014). Functionally, trauma-related OCD and PTSD symptoms have also been hypothesised to have a dynamic relationship, in that the former can serve a protective coping function to alleviate unpleasant trauma-related thoughts and emotions (Gershuny et al. 2003), and thereby partially mask the latter in turn. The significant elevation of OCD prevalence after trauma exposure has been noted in studies (O'Donnell et al. 2016) and warrants further investigation.
Overall, only man-made disaster exposure was associated with an increased lifetime risk of a range of psychiatric disorders, while repeated natural disaster exposure was associated with an increased risk of panic disorder. By contrast to previous research which identified cumulative effects of repeated disaster exposure in relation to population suicidality (Reifels et al. Forthcoming), cumulative exposure effects were only rarely observed across the wider psychiatric disorder spectrum (and largely limited to OCD and panic disorders). Pursuant to further confirmation of these distinctive lifetime disaster exposure correlates, our findings suggest that we cannot necessarily assume that repeat disaster exposure is inevitably linked to worse mental health outcomes (when compared with single disaster exposure), or for that matter, that cumulative disaster exposure will have the same uniform (adverse) impact across the psychiatric disorder spectrum.
The toxic nature and adverse mental health impacts of acts of interpersonal (Forbes et al. 2012) or mass violence involving intentional harm (Norris & Elrod, 2006) are well documented, which may explain the higher risk of psychiatric disorder associated with man-made disaster. It is worth also noting that individuals involved in man-made disasters had been exposed to a greater number of disaster events than those involved in natural disasters, hence underscoring the need to control for respective disaster exposure levels. These findings, however, do not take away from the importance of natural disaster and its psychiatric impact in Australia. In this study, natural disaster was associated with more cases of psychiatric disorder than man-made disaster, probably due to the frequency with which these events occur in Australia.
Study strengths and limitations
Methodological study strengths and limitations need to be considered in interpreting the findings. Study strengths included the use of nationally representative population data and a consistent diagnostic algorithm (based on established DSM-IV criteria) to assess a broad spectrum of psychiatric disorders, across distinct disaster types. Due to the focus on examining diagnosable psychiatric disorders in the Australian population, findings may not be generalisable to populations in other countries, or indicative of sub-threshold levels of distress. Multivariate analyses of cross-sectional survey data adjusted for numerous factors to determine key variable associations, but did not permit definitive causal inferences. Lifetime self-report data are more likely to be subject to recall bias which can adversely impact the accuracy of prevalence estimates. While the NSMHWB differentiated natural and man-made disaster exposure type, it did not distinguish more specific disaster event or exposure characteristics, which can be predictive of mental health outcomes. Since our analysis of lifetime correlates did not differentiate pre-existing from post-disaster disorders, resulting estimates are likely to reflect inflated estimates of the true prevalence of new onset (or exacerbated) disorders, which can be causally linked to, and observed following, disaster exposure. In view of our limited knowledge about the timing of psychiatric symptom onset in disaster contexts, future population-based studies may therefore benefit from adopting prospective study designs to examine the full spectrum of disorder risks and associated prevalence estimates, over time.
Study implications
In view of Australia's existing disaster risk profile, our findings have important implications for an all-hazards approach to disaster preparedness planning and a better understanding of the associated mental health burden of disasters. In ascertaining the population imprint of disaster exposure in Australia, it is critical to recognise a basic and yet fundamental principle of the inverse relationship of disaster type prevalence and associated mental health impacts. Relatively infrequent man-made disasters are likely to carry greater mental health risks (in terms of the likelihood and severity of adverse mental health consequences). Nevertheless, more frequently occurring natural disasters likely account for the greater share of the total burden of disaster mental health consequences (in terms of the total number of disaster-affected Australians developing lifetime psychiatric disorders).
Population-based disaster mental health research can thus complement existing research in the field by providing an overarching national picture of (the relative weight of) relevant disaster mental health correlates, while longitudinal event-specific studies are required to obtain accurate post-disaster prevalence estimates and inform the timing of assistance in specific disaster circumstances. As such, population-based trends are also not necessarily reflective of individual-level outcome trajectories, or of the spectrum and magnitude of mental health outcomes observed in unique disaster contexts. Nevertheless, by establishing the previously unknown national risk and prevalence of the wide range of lifetime psychiatric disaster correlates, our findings can inform future research and preparedness activities in regard to natural and man-made disasters in Australia.
Globally increasing disaster risks further call for effective disaster risk reduction strategies which minimise the likelihood of disaster exposure and of associated adverse health impacts in the population (Aitsi-Selmi & Murray, 2016). Such strategies, in turn, require up-to-date population data and suitable methodologies in order to monitor future population mental health impacts of increasing disaster exposure and the effectiveness of these strategies across varied scales and contexts over time. This study will contribute to fostering initiatives which seek to develop clearer population-based estimates of the mental health risks and outcomes associated with disaster exposure as a means to informing effective disaster risk reduction strategies.
Conclusion
Population-based analyses of nationally representative survey data provide a comprehensive and consistent method to ascertain the full spectrum of psychiatric disorders associated with the population imprint of varied types of disaster exposure. Mental health policy and services should be targeting a range of psychiatric disorders in disaster contexts in addition to the usual focus on PTSD and depression, including alcohol abuse, panic disorder and OCD. Despite the relatively greater disorder risk associated with man-made disaster, natural disaster exposure was associated with more cases of psychiatric disorder, likely due to the frequency with which these events occur in Australia.
Acknowledgements
The authors wish to thank Matthew J. Spittal for initial statistical advice regarding the study.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Availability of Data and Materials
The data are available from the Australian Bureau of Statistics at http://www.abs.gov.au/ and the computing code is available from the authors upon request.
Footnotes
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796017000531.
click here to view supplementary material
Conflicts of Interest
None.
References
- Aitsi-Selmi A & Murray V (2016). Protecting the health and well-being of populations from disasters: health and health care in the Sendai Framework for Disaster Risk Reduction 2015–2030. Prehospital and Disaster Medicine 31, 74–78. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics (2009). 2007 National Survey of Mental Health and Wellbeing: Users’ Guide, Cat. No. 4327.0. Australian Bureau of Statistics: Canberra. [Google Scholar]
- Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, Shahly V, Stein DJ, Petukhova M, Hill E, Alonso J, Atwoli L, Bunting B, Bruffaerts R, Caldas-de-Almeida JM, de Girolamo G, Florescu S, Gureje O, Huang Y, Lepine JP, Kawakami N, Kovess-Masfety V, Medina-Mora ME, Navarro-Mateu F, Piazza M, Posada-Villa J, Scott KM, Shalev A, Slade T, ten Have M, Torres Y, Viana MC, Zarkov Z & Koenen KC (2016). The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychological Medicine 46, 327–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno GA, Brewin CR, Kaniasty K & La Greca AM (2010). Weighing the costs of disaster: consequences, risks, and resilience in individuals, families, and communities. Psychological Science in the Public Interest 11, 1–49. [DOI] [PubMed] [Google Scholar]
- Bonde JP, Utzon-Frank N, Bertelsen M, Borritz M, Eller NH, Nordentoft M, Olesen K, Rod NH & Rugulies R (2016). Risk of depressive disorder following disasters and military deployment: systematic review with meta-analysis. British Journal of Psychiatry 208, 330–336. [DOI] [PubMed] [Google Scholar]
- Bromet EJ, Atwoli L, Kawakami N, Navarro-Mateu F, Piotrowski P, King AJ, Aguilar-Gaxiola S, Alonso J, Bunting B, Demyttenaere K, Florescu S, de Girolamo G, Gluzman S, Haro JM, de Jonge P, Karam E, Lee S, Kovess-Masfety V, Medina-Mora ME, Mneimneh Z, Pennell BE, Posada-Villa J, Salmerón D, Takeshima T & Kessler RC (2017). Post-traumatic stress disorder associated with natural and human-made disasters in the World Mental Health Surveys. Psychological Medicine 47, 227–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dückers MLA & Brewin CR (2016). A paradox in individual versus national mental health vulnerability: Are higher resource levels associated with higher disorder prevalence? Journal of Traumatic Stress 29, 572–576. [DOI] [PubMed] [Google Scholar]
- Dückers MLA, Alisic E & Brewin CR (2016). A vulnerability paradox in the cross-national prevalence of post-traumatic stress disorder. British Journal of Psychiatry 209, 300–305. [DOI] [PubMed] [Google Scholar]
- Dykshoorn KL (2014). Trauma-related obsessive-compulsive disorder: a review. Health Psychology & Behavioural Medicine 2, 517–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes D, Fletcher S, Parslow R, Phelps A, O'Donnell M, Bryant RA, McFarlane A, Silove D & Creamer M (2012). Trauma at the hands of another: longitudinal study of differences in the posttraumatic stress disorder symptom profile following interpersonal compared with noninterpersonal trauma. The Journal of Clinical Psychiatry 73, 372–376. [DOI] [PubMed] [Google Scholar]
- Galea S, Nandi A & Vlahov D (2005). The epidemiology of post-traumatic stress disorder after disasters. Epidemiologic Reviews 27, 78–91. [DOI] [PubMed] [Google Scholar]
- Gershuny BS, Baer L, Radomsky AS, Wilson KA, & Jenike MA (2003). Connections among symptoms of obsessive-compulsive disorder and posttraumatic stress disorder: a case series. Behaviour Research and Therapy 41, 1029–1041. [DOI] [PubMed] [Google Scholar]
- Kessler RC & Ustün TB (2004). The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research 13, 93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Chatterji S, Lee S, Ormel J, Ustün TB & Wang PS (2009). The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiologia E Psichiatria Sociale 18, 23–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane AC & Williams R (2012). Mental health services required after disasters: learning from the lasting effects of disasters. Depression Research and Treatment 2012, 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane AC, Van Hooff M & Goodhew F (2009). Anxiety disorders and PTSD In Mental Health and Disasters (ed. Neria Y, Galea S and Norris FH), pp. 47–66. Cambridge University Press: Cambridge. [Google Scholar]
- Mills KL, McFarlane AC, Slade T, Creamer M, Silove D, Teesson M & Bryant R (2011). Assessing the prevalence of trauma exposure in epidemiological surveys. Australian and New Zealand Journal of Psychiatry 45, 407–415. [DOI] [PubMed] [Google Scholar]
- Norris FH & Elrod C (2006). Psychosocial consequences of disaster: a review of past research In Methods for Disaster Mental Health Research (ed. Norris FH, Galea S, Friedman M and Watson P), pp. 20–44. Guilford: New York. [Google Scholar]
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E & Kaniasty K (2002). 60,000 disaster victims speak: part I. An empirical review of the empirical literature, 1981–2001. Psychiatry 65, 207–239. [DOI] [PubMed] [Google Scholar]
- North CS (2007). Epidemiology of disaster mental health In Textbook of Disaster Psychiatry (ed. Ursano RJ, Fullerton CS, Weisaeth L and Raphael B), pp. 29–47. Cambridge University Press: Cambridge. [Google Scholar]
- O'Donnell ML, Alkemade N, Creamer MC, McFarlane AC, Silove D, Bryant RA & Forbes D (2016). The long term psychiatric sequelae of severe injury: a six year follow-up study. Journal of Clinical Psychiatry 77, e473–e479. [DOI] [PubMed] [Google Scholar]
- Reifels L, Spittal MJ, Dückers MLA, Mills K & Pirkis J (Forthcoming). Suicidality risk and (repeat) disaster exposure: findings from a nationally representative population survey. Psychiatry. [DOI] [PubMed] [Google Scholar]
- Slade T, Johnston A, Oakley Browne MA, Andrews G & Whiteford H (2009). 2007 national Survey of Mental Health and Wellbeing: methods and key findings. Australian & New Zealand Journal of Psychiatry 43, 594–605. [DOI] [PubMed] [Google Scholar]
- Van der Velden PG & Kleber RJ (2009). Substance use and misuse after disasters: prevalences and correlates In Mental Health and Disasters (ed. Neria Y, Galea S and Norris FH), pp. 94–115. Cambridge University Press: New York. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796017000531.
click here to view supplementary material
Data Availability Statement
The data are available from the Australian Bureau of Statistics at http://www.abs.gov.au/ and the computing code is available from the authors upon request.