Abstract
Background.
Although financing represents a critical component of health system strengthening and also a defining concern of efforts to move towards universal health coverage, many countries lack the tools and capacity to plan effectively for service scale-up. As part of a multi-country collaborative study (the Emerald project), we set out to develop, test and apply a fully integrated health systems resource planning and health impact tool for mental, neurological and substance use (MNS) disorders.
Methods.
A new module of the existing UN strategic planning OneHealth Tool was developed, which identifies health system resources required to scale-up a range of specified interventions for MNS disorders and also projects expected health gains at the population level. We conducted local capacity-building in its use, as well as stakeholder consultations, then tested and calibrated all model parameters, and applied the tool to three priority mental and neurological disorders (psychosis, depression and epilepsy) in six low- and middle-income countries.
Results.
Resource needs for scaling-up mental health services to reach desired coverage goals are substantial compared with the current allocation of resources in the six represented countries but are not large in absolute terms. In four of the Emerald study countries (Ethiopia, India, Nepal and Uganda), the cost of delivering key interventions for psychosis, depression and epilepsy at existing treatment coverage is estimated at US$ 0.06–0.33 per capita of total population per year (in Nigeria and South Africa it is US$ 1.36–1.92). By comparison, the projected cost per capita at target levels of coverage approaches US$ 5 per capita in Nigeria and South Africa, and ranges from US$ 0.14–1.27 in the other four countries. Implementation of such a package of care at target levels of coverage is expected to yield between 291 and 947 healthy life years per one million populations, which represents a substantial health gain for the currently neglected and underserved sub-populations suffering from psychosis, depression and epilepsy.
Conclusions.
This newly developed and validated module of OneHealth tool can be used, especially within the context of integrated health planning at the national level, to generate contextualised estimates of the resource needs, costs and health impacts of scaled-up mental health service delivery.
Key words: Economic issues, epidemiology, health service research, mental health
Introduction
A critical component of health system strengthening, which underlies the universal health coverage agenda, is financing (WHO, 2010). Health financing is a far-reaching topic that addresses questions not only about what services to purchase, but also how resources can be best generated and pooled in a fair and sustainable way. An ongoing research programme called Emerald (Emerging mental health systems in low- and middle-income countries (LMICs)) is investigating a number of such questions as they pertain to mental health services, including the adequacy of resources for mental health, fairness in financial contributions to the costs of care, and the financial and economic impact of improved access to services (Semrau et al. 2015). In this study, we focus on the first of these, which concerns the adequacy of resources. Mental health remains a highly underfunded area of health system development, attracting <1% of the US$ 32 billion spent on official development assistance for health in 2013 (Gilbert et al. 2015) and manifesting itself in very low levels of reported government spending (of <US$ 2 per capita in LMICs; WHO, 2015). Many LMICs do not have – or are unable to report – data on mental health expenditure; for example, none of the six countries participating in the Emerald study – Ethiopia, India, Nepal, Nigeria, South Africa and Uganda – were able to provide a breakdown of inpatient and outpatient mental health expenditures in the recent WHO Mental Health Atlas 2014 survey (WHO, 2015).
Estimation of the human, physical and financial capital needed to develop or scale-up prioritised interventions is a task that can usefully be undertaken in order to demonstrate the existing funding gap and to indicate how it could be bridged over time. Previous work has shown that the cost of scaling-up an intervention package for psychosis, bipolar disorder, depression and harmful alcohol use ranged from US$ 1.85 to 2.60 per person per year in low-income countries and US$ 3.20 to 6.25 per year in lower-middle-income countries (Chisholm et al. 2007). Recent work focused more specifically on the resources needed to scale-up mental health plans in primary health care at the district level, and estimated a cost of <US$ 1 per head of population in the four low- and lower-middle-income countries represented in the study (Chisholm et al. 2015). Two important limitations of such analyses, however, are that no account is taken of the health system constraints that limit scale-up efforts in practice (such as the availability of skilled workers), and there is no estimate made of the expected health impact associated with each year of scale-up. Furthermore, health planners at the country level have, to date, lacked access to appropriate analytical tools for undertaking, in the context of overall national health plans, an integrated approach to their own mental health resource need assessments (as part of a policy of moving towards universal health coverage, for example).
In this study, therefore, we set out to develop, test and apply a fully integrated health systems resource planning and health impact tool for mental, neurological and substance use (MNS) disorders.
Methods
Development of OneHealth tool module on MNS disorders
In order to ensure that the development of national mental health plans is carried out within a framework of overall health system capacity assessment, and to take into account financial sustainability and outcomes-based planning, we developed and populated a mental health module for integration within the OneHealth systems planning tool (OHT). OneHealth is a software tool that has been developed by international costing experts from WHO and other UN agencies to strengthen health system analysis, costing and financing scenarios at the country level (http://www.who.int/choice/onehealthtool; Stenberg & Chisholm, 2012). It achieves this by bringing together disease-specific planning (for mental disorders and other diseases) and health systems planning (e.g., modules for human resources, logistics and other health system ‘building blocks’). OHT builds on previous costing tools that have been developed in the context of LMICs for a number of communicable and non-communicable health conditions, but takes the crucial next step of harmonising these efforts and drawing out the shared health system costs that appear in each of these vertically aligned costing tools.
In terms of the conceptual and technical development of this new module within OneHealth, significant time and effort was spent implementing a workable mechanism for capturing the cumulative impact of scaled-up mental health care interventions, since most of the health effects of such interventions relate to improvements in morbidity or disability (as opposed to saving lives); the selected metric for summarising these health effects at the population level was healthy life years gained (equivalent to disability-adjusted life years averted, where one DALY can be thought of as one lost year of healthy life; http://www.who.int/healthinfo/global_burden_disease/metrics_daly/en/). Healthy life years were computed with reference to country-specific life tables that are already built into the model, and reflect the combined time spent by the population in a particular state of health with a known degree (or free) of disability. Disability levels were drawn from the Global Burden of Disease 2010 study (Salomon et al. 2012). Implementation or scale-up of an effective intervention in the population was modelled to reduce the time spent in a disabling state, either by reducing prevalence (e.g., by decreasing the number of new cases or by increasing the rate of remission), or by improving the level of functioning of people with the condition in question. For example, a key effect of managing psychosis with anti-psychotic drugs and psychosocial treatment is to control symptoms and enhance functioning, while depression treatment mainly has the effect of reducing the duration of an episode (equivalent to increasing the remission rate).
Health impact estimates were developed for MNS disorders and interventions that are covered in the WHO's mental health gap action programme (mhGAP) Intervention Guide (WHO, 2010). Although this Intervention Guide covers evidence-based intervention strategies for at least eight disorders (from developmental and behavioural disorders in childhood, to dementia in older age), initial country-level testing and calibration was restricted to three conditions considered by the participating countries to represent high priority disorders: psychosis, depression and epilepsy. Default estimates for deriving the population-level health impact of specific interventions were based on UN population projections, the latest Global Burden of Disease prevalence estimates for 2010 (Whiteford et al. 2013), and previous reviews or analyses of clinical outcomes and cost-effectiveness (Hyman et al. 2006; Chisholm & Saxena, 2012; Patel et al. 2015). Web Appendix A provides a summary of default intervention effects for psychosis, depression and epilepsy (which countries were encouraged to overwrite with local data if available).
Treatment rates and patterns for specific interventions relied on previous cost-effectiveness studies and resource need profiles garnered from existing treatment guidelines and costing tools (WHO, 2010; Chisholm & Saxena, 2012; Chisholm et al. 2015). Key categories of health service use were: drug and supply costs (e.g., daily dose of a generically produced, first-line anti-psychotic or anti-epileptic medication); ambulatory contacts with mental health or general health workers (such as psychologists, counsellors and community health workers); and hospital-based outpatient/inpatient care. In addition, programme-level resource needs were identified, including overall programme management and administration, as well as training (in the use of mhGAP intervention guide, for example). Default drug prices were taken from the International Drug Price Indicator Guide, while country-specific unit costs of inpatient and outpatient care were taken from WHO-CHOICE (http://www.who.int/choice/country/country_specific). Total costs of scaling-up an intervention in a given year for a country were derived by multiplying resource use needs by their respective unit costs to give a cost per case, which was then multiplied by the total number of cases expected to receive a particular intervention (given by the prevalence of the disorder multiplied by the rate of treatment coverage of specific intervention strategies in the population). That is, total cost = Population × Prevalence rate × Coverage increase × Treatment cost per case.
OHT capacity-building and country-level adaptation in Emerald countries
Once a working tool had been developed, it was applied to the context of each of the six participating Emerald countries. As shown and described elsewhere, indicators of development, health resources and the mental health system vary substantially across the six Emerald countries (Semrau et al. 2015); for example, in Ethiopia one psychiatrist serves on average a population of over two million persons, compared with <400 000 in India and South Africa. A series of technical workshops were undertaken in participating countries in order to build local capacity in the adaptation and use of the MNS module of OHT. These workshops were facilitated by cross-country partners responsible for the development and validation of the tool, and were attended by local Emerald research team members as well as health service planners and experts from central and local governments. A series of presentations were developed for these workshops, together with practical exercises for actually using the software (available on request from the authors).
Working with local team members and other national staff, and with support from cross-country partners, appointed country focal points undertook a process of contextualising the input data that should be entered into OHT to best reflect local data, experiences and priorities. This process consisted of two main elements:
-
(1)
Strategic-level consideration involving consultation with an expert group of national planners, policy-makers and programme managers concerning the specification of appropriate mental health care packages and scenarios, current and target coverage levels for specific intervention strategies, and the period of scale-up (see Table 1 for the results of decisions taken, based on locally available data if available but more often relying upon expert opinion in the absence of such data).
-
(2)
Clinical-level consideration of average or expected resource use profiles for different disorders and interventions, efficacy/adherence estimates for specific intervention strategies, and unit costs and prices for health care services and commodities (such as for staff salaries, outpatient visits and psychotropic medications). For these latter data inputs, the research team identified and used local data sources and, where applicable, overwrote default values present in the tool. A data checklist was developed and disseminated in order to facilitate and document the process of data contextualisation.
Table 1.
Current and target coverage levels of interventions for priority MNS disorders modelled in OHT (%)
| Interpolation type* | Ethiopia | India | Nepal | Nigeria | South Africa | Uganda | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exponential | Exponential | Linear | Linear | Linear | Exponential | |||||||
| Baseline coverage | Target coverage | Baseline coverage | Target coverage | Baseline coverage | Target coverage | Baseline coverage | Target coverage | Baseline coverage | Target coverage | Baseline coverage | Target coverage | |
| Depression | ||||||||||||
| Basic psychosocial treatment for mild cases | – | – | 10 | 30 | – | – | – | – | – | – | 10 | 30 |
| Psychosocial treatment and anti-depressant medication of first episode moderate-severe cases | 1 | 20 | 5 | 20 | 5 | 35 | 10 | 30 | 15 | 30 | 5 | 20 |
| Intensive psychosocial treatment and anti-depressant medication of first episode moderate-severe cases | 0.1 | 10 | – | – | – | – | 5 | 15 | 5 | 20 | ||
| Psychosocial treatment and anti-depressant medication of recurrent moderate-severe cases on an episodic basis | 0.1 | 10 | 5 | 35 | 10 | 30 | – | – | 5 | 20 | ||
| Intensive psychosocial treatment and anti-depressant medication of recurrent moderate-severe cases on a maintenance basis | 0.1 | 10 | – | – | – | – | – | – | 5 | 20 | ||
| Psychosis | ||||||||||||
| Basic psychosocial treatment and anti-psychotic medication | 2 | 30 | 20 | 50 | 20 | 50 | 20 | 50 | 20 | 50 | 20 | 50 |
| Intensive psychosocial treatment and anti-psychotic medication | – | – | 5 | 20 | – | – | – | – | 0 | 10 | 5 | 20 |
| Epilepsy | ||||||||||||
| Basic psychosocial support, advice and follow-up, plus anti-epileptic medication | 15 | 50 | – | – | 40 | 80 | 20 | 60 | – | – | 50 | 90 |
Exponential scale-up provides for an initially slow degree of health system development but then speeds up exponentially as the target year approaches; Linear scale-up assumes a constant rate of coverage expansion between baseline and target year.
A representative example of the contextualisation process followed in one country is provided in Box 1. Once each country contextualised the tool to the extent possible, results could be presented to and discussed with local health policy makers, planners and other stakeholders.
Box 1.
Contextualisation process: Ethiopia
Background: The Ethiopian National Mental Health Strategy was published in 2012 and embraced a plan to scale-up mental health care based on the WHO mhGAP programme and utilising the mhGAP evidence-based packages of care for priority MNS use disorders. In 2014, the Ministry of Health of Ethiopia launched an ambitious 12-year plan to scale-up mental health care across the whole country. The Federal Ministry of Health of Ethiopia has adopted the OneHealth planning tool to support planning for its Health Sector Transformation Plan (2015/16 to 2019/20).
Selecting priority MNS disorders: As part of the mhGAP pilot in Ethiopia, a prioritisation workshop of all relevant stakeholders was convened. At that workshop, the decision was made to focus on psychosis, epilepsy and depression. Alcohol use disorders were later added by the Ethiopia mhGAP working group. For the purpose of this current exercise the focus was on the three conditions initially prioritised by the FMOH of Ethiopia.
Epidemiology: Ethiopia has a distinguished history in mental health research and it was therefore possible to make use of high quality epidemiological data from within country. Age- and sex-stratified data on the prevalence of schizophrenia, for example, was available from the Butajira Severe Mental Disorder study, in which more than 68 000 people were screened for psychosis and possible cases were investigated using gold standard clinician interviews (Kebede et al. 2000; Alem et al. 2009).
Packages of care: The selection of packages of care for each of the three priority MNS disorders (psychosis, epilepsy and depression) was informed by the availability of appropriate human resources and learning from the Emerald-affiliated Programme for Improving Mental health carE (PRIME) in Ethiopia (Hanlon et al. 2014). Although Ethiopia has very few specialist professionals who have the capacity to train, deliver or supervise intensive psychological therapies., the formative work for the PRIME study indicated that task sharing for intensive psychological therapies, for example with primary health nurses and community-based health workers, is not feasible. Therefore, for psychosis, we did not include intensive psychological therapy. For depression, intensive psychological therapy was felt to be appropriate and potentially feasible for a small proportion of people with moderate-severe depression, given the work underway to scale-up interpersonal therapy for depression in primary care settings (the Biaber project; http://mhinnovation.net/innovations/biaber-project) and the work in PRIME to develop feasible psychosocial interventions for depression. The medications used for each package were adapted to the Ethiopian setting, with a particular focus on medications which are likely to become available in the primary care setting. The costs of relevant psychotropic medications were obtained from the central Pharmaceutical Fund and Supply Agency.
Coverage: Estimates of baseline coverage were obtained from Ethiopia research studies. The National Mental Health Strategy aspired to 50% coverage for all of the priority MNS disorders by the end of 2015. However, the more detailed mental health scale-up plan for Ethiopia aims for 44% coverage (at the health facility level) by the end of 2019. Given the challenges experienced by the mhGAP pilot in Ethiopia and by the PRIME Ethiopia project with respect to demand for mental health care for depression, a modest coverage target of 30% by 2020 was set. For psychosis the target coverage was 30%, and for epilepsy the target coverage was 50%. The higher target for coverage for epilepsy reflected the lower baseline treatment gap and the success in the mhGAP pilot in delivering care to people with epilepsy in the primary care setting.
Programme costs: Information on the programme specific staff inputs required for scale-up were obtained from the National Mental Health Strategy, for example, to include a new mental health co-ordinator at each level of the health system (district, regional and national). Furthermore, information on the training plans, in terms of the number of health workers per health centre per year were obtained from MoH plans developed within the NCD unity. Information on human resource costs, training costs for mhGAP and infrastructure costs were obtained from the planning department of the Ministry of Health.
Application and use of the MNS module in OHT
Application of the MNS module of the OneHealth tool in the six participating Emerald countries produced new estimates of the resource needs, costs and health impacts of scaled-up delivery of their specified intervention packages (see Results section below); each country's finalised estimates, including all assigned input parameters as well as detailed model outputs, were saved as a discrete projection file that could be opened, reviewed and shared with other project team members (or other OHT users). Following further testing and validation, the module has now been made publicly available for download and use (in any country) at the following URL: http://spectrumbeta.futuresinstitute.org/. Users are able to generate a new projection for their own country setting, specifying the diseases and interventions to be included as well as the scale-up period and (current and target) coverage levels to be utilised. Following direct entry of hospital unit costs, salary information and programme management and training costs into the tool, as well as revision as needed for any other key data inputs, users can view computed output relating to the costs and health impacts of mental health service scale-up in their local setting. It is anticipated that the tool can and will be used by health planners in national health agencies and by health system researchers. A detailed user manual dedicated to the MNS module and its operationalisation has been developed (available at http://www.avenirhealth.org/software-onehealth.php) to facilitate its deployment.
Availability of data and materials
Data extracted from OHT and used for the purpose of this article can be found at the following Dropbox folder: https://www.dropbox.com/sh/pngvjw1mxziejpg/AADn2cHSL6Vw_xwbMkpqT61Ja?dl=0
Results
For the purposes of concise, consistent and comparable reporting across the six participating Emerald sites, results presented below are restricted to selected output parameters of the modelling process. All cost values have been converted into US dollars for ease of interpretation and comparison, but in the context of ongoing policy dialogue local currency values are also being used.
OHT configuration
Table 1 provides an overview of the interventions modelled for psychosis, depression and epilepsy in each country, and also shows the baseline and target coverage levels set, based on a situational analysis of service availability and expert opinion regarding the target level that can be reasonably expected to be attained over the scale-up period. The scale-up period was chosen by each country team and ranged between 5 and 7 years in length; four of the six sites selected 2020 as the final, target year for scale-up. As can be seen, current coverage levels are generally very low, indicating the enormous treatment gap for these key disorders in the populations of these (and most other) LMICs. Target coverage levels, by contrast, are set relatively high, and represent ambitious goals for rapid scale-up of service coverage, especially within such a limited period of time. These target coverage levels have a crucial impact on the expected costs and health impacts of increased treatment coverage, and are likely to be a key topic of discussion in future discussions and interactions with government health planners.
OHT output: estimated costs of scale-up
Web Appendix Tables B–D provide a breakdown of costs by priority disorder for drugs and supplies, ambulatory and outpatient care, and inpatient care, respectively. These represent the total resource requirements in each year of scale up, based on the contextualised estimates of what each element of this package of care should comprise in the local situation. They illustrate well the substantial monetary resources that need to be made available if the stated coverage goals are to be reached. At target treatment coverage levels in Nigeria, for example, over US$ 200 million would be required in terms of drugs and supplies, a further US$ 200 million for ambulatory care and outpatient services, and nearly $500 million for inpatient services. By 2018, however, the population of Nigeria is projected to reach 200 million, so when considered on a per capita or proportionate basis these amounts appear more realistic (<US$ 5 per capita or <5% of projected health spending), particularly if a steady incremental approach is taken to budgetary resource allocation. Programmatic costs (in particular training, supervision and programme administration or management) can be found in Web Table E; these resources are shared across specific disease entities; for example, an mhGAP training course can cover psychosis, depression and epilepsy.
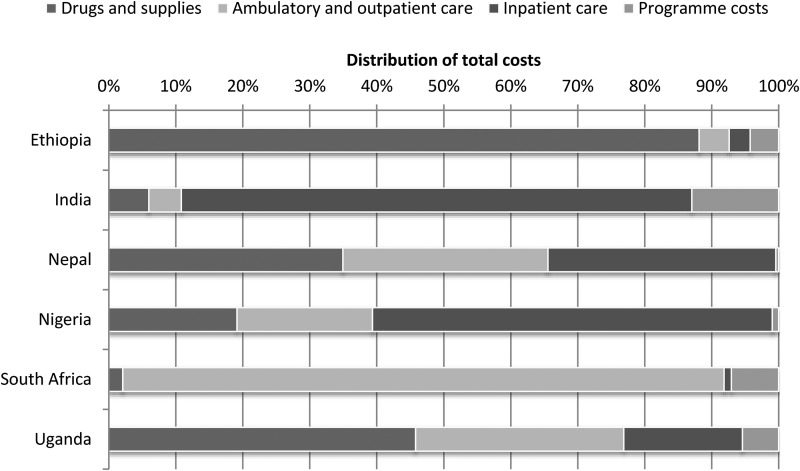
Figure 1 shows the breakdown of costs between these different categories of resource need for the scale-up period as a whole. There are stark differences in the expected contribution of different service elements to overall costs of provision; for example, essential psychotropic drugs absorb a large share of overall costs in the three low-income countries (Ethiopia, Nepal and Uganda), while the proportion of total costs taken up by inpatient services ranges from <5% (in Ethiopia and South Africa) to over 80% (in India). This pattern of costs reflects the fact that traded goods such as psychotropic medicines are relatively more expensive to purchase in low-income settings, while non-traded goods that go into clinical care (including human resources) are relatively low cost compared with middle-income countries.
Fig. 1.
Distribution of total costs of service scale-up for psychosis, depression and epilepsy
Table 2 brings together all these cost elements and expresses them both in total terms (per year) and also per head of population. The latter metric is particularly useful for looking across countries because it standardises for population size. In four of the Emerald study countries (Ethiopia, India, Nepal and Uganda), the cost of delivering key interventions for psychosis, depression and epilepsy at existing treatment coverage (in the baseline year) is estimated at US$ 0.06–0.33 per capita of total population (in Nigeria and South Africa it is US$ 1.36–1.92). By comparison, the projected cost per year at target levels of coverage approaches US$ 5 per capita in Nigeria and South Africa, and ranges from US$ 0.14 to 1.27 in the other four countries.
Table 2.
Total costs (US$)
| Country | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | Total | |
|---|---|---|---|---|---|---|---|---|---|
| Ethiopia | Total (US$) | 10 793 057 | 15 994 423 | 21 161 420 | 26 896 829 | 32 536 724 | 38 359 656 | 44 104 042 | 189 846 151 |
| Per capita (US$) | 0.11 | 0.16 | 0.21 | 0.25 | 0.30 | 0.34 | 0.39 | 1.76 | |
| India | Total (US$) | 84 350 415 | 102 692 518 | 122 084 066 | 142 116 507 | 162 750 775 | 181 410 772 | 202 873 902 | 998 278 955 |
| Per capita (US$) | 0.07 | 0.08 | 0.10 | 0.11 | 0.12 | 0.14 | 0.15 | 0.77 | |
| Nepal | Total (US$) | 9 123 511 | 13 580 538 | 18 105 276 | 22 774 097 | 27 590 348 | 32 551 737 | 37 527 394 | 161 252 900 |
| Per capita (US$) | 0.33 | 0.49 | 0.64 | 0.80 | 0.95 | 1.11 | 1.27 | 5.58 | |
| Nigeria | Total (US$) | 240 290 580 | 373 889 010 | 529 966 888 | 709 339 852 | 911 992 658 | – | – | 2 765 478 988 |
| Per capita (US$) | 1.36 | 2.06 | 2.84 | 3.69 | 4.61 | 14.56 | |||
| South Africa | Total (US$) | 102 656 451 | 124 426 615 | 144 002 944 | 170 362 472 | 198 851 125 | 228 849 571 | 262 147 132 | 1 320 179 429 |
| Per capita (US$) | 1.92 | 2.29 | 2.63 | 3.07 | 3.55 | 4.05 | 4.59 | 23.81 | |
| Uganda | Total (US$) | 6 742 625 | 9 583 382 | 11 725 832 | 13 539 385 | 14 987 252 | – | – | 56 578 476 |
| Per capita (US$) | 0.18 | 0.24 | 0.29 | 0.32 | 0.34 | – | – | 7.35 |
OHT output: estimated health impacts of scale-up
Table 3 shows the health impact or implications of substantially scaled-up coverage of included interventions, expressed in terms of healthy life years. As can be seen, there is a short lag between greater uptake of services and consequent reductions in the prevalence or disability associated with these disorders, which is partly due to the exponential pattern of scale-up chosen by countries (this pattern assumes a slow start as resources are mobilised and staff are trained, and a rapid increase in the final years of the scale-up period). The total size of the health impact will evidently vary with the interventions chosen, as well as starting and target levels of coverage, but across the six countries the total, cumulative health gains amounted to more than two million extra healthy life years. In the final year of each country's projection, at which point target coverage levels are assumed to have been reached, the number of healthy life years gained per one million population ranged between 291 in India to 947 in Uganda. Depression accounted for the largest proportion of generated public health gain, with the exception of Nigeria, where epilepsy generated the greatest number of healthy life years.
Table 3.
Healthy life years gained – impact of scale-up
| Country | Disorder | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| Ethiopia | Depression | – | 7329 | 15 941 | 25 283 | 35 278 | 45 919 | 57 202 | 186 952 | |
| Psychosis | – | 983 | 2047 | 3199 | 4443 | 5769 | 7186 | 23 627 | ||
| Epilepsy | – | 5702 | 10 474 | 14 432 | 17 671 | 20 212 | 22 107 | 90 598 | ||
| Total | – | 14 014 | 28 462 | 42 914 | 57 392 | 71 900 | 86 495 | 301 177 | ||
| Per 1m population | 140 | 277 | 406 | 529 | 645 | 755 | ||||
| India* | Depression | – | 36 217 | 77 440 | 120 994 | 166 359 | 213 376 | 261 961 | 876 347 | |
| Psychosis | – | 19 357 | 39 510 | 60 471 | 82 250 | 104 676 | 127 811 | 434 075 | ||
| Epilepsy | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | ||
| Total | – | 55 574 | 116 950 | 181 465 | 248 609 | 318 052 | 389 772 | 1 310 422 | ||
| Per 1m population | 44 | 91 | 140 | 190 | 240 | 291 | ||||
| Nepal | Depression | – | 1985 | 4239 | 6632 | 9137 | 11 746 | 14 453 | 48 192 | |
| Psychosis | – | 380 | 782 | 1207 | 1656 | 2125 | 2617 | 8767 | ||
| Epilepsy | – | 1080 | 2271 | 3564 | 4949 | 6418 | 7961 | 26 243 | ||
| Total | – | 3445 | 7292 | 11 403 | 15 742 | 20 289 | 25 031 | 83 202 | ||
| Per 1m population | 123 | 258 | 398 | 544 | 693 | 844 | ||||
| Nigeria | Depression | – | 10 200 | 21 928 | 34 486 | 47 789 | – | – | 114 403 | |
| Psychosis | – | 3512 | 7253 | 11 241 | 15 493 | – | – | 37 499 | ||
| Epilepsy | – | 17 741 | 32 960 | 45 987 | 57 070 | – | – | 153 758 | ||
| Total | – | 31 453 | 62 141 | 91 714 | 120 352 | – | – | 305 660 | ||
| Per 1m population | 173 | 333 | 477 | 609 | ||||||
| South Africa | Depression | – | 2685 | 5880 | 9305 | 12 906 | 16 673 | 20 603 | 68 052 | |
| Psychosis | – | 216 | 445 | 684 | 935 | 1197 | 1470 | 4947 | ||
| Epilepsy | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | ||
| Total | − | 2901 | 6325 | 9989 | 13 841 | 17 870 | 22 073 | 72 999 | ||
| Per 1m population | 54 | 117 | 182 | 250 | 319 | 390 | 463 | |||
| Uganda | Depression | – | 5290 | 11 505 | 18 246 | 25 467 | – | – | 60 508 | |
| Psychosis | – | 989 | 2057 | 3210 | 4454 | – | – | 10 710 | ||
| Epilepsy | – | 3699 | 6795 | 9370 | 11 485 | – | – | 31 349 | ||
| Total | – | 9978 | 20 357 | 30 826 | 41 406 | – | – | 102 567 | ||
| Per 1m population | 253 | 499 | 730 | 947 | ||||||
Population refers to the State of Madhya Pradesh.
Discussion
In the face of a large disease burden and treatment gap, the Emerald project aims to generate new understanding and insights into the current extent of financial protection and service provision in a range of LMIC, as well as future resource needs and mechanisms for moving closer towards the goal of universal health coverage for MNS disorders. The component of this broader research agenda presented here has been concerned with preparing and implementing a tool capable of informing local policy makers about the resource needs and costs of scaling up mental health services in their local populations. Following the initial development of a bespoke module, its incorporation into the OneHealth strategic planning tool, and its subsequent use in six LMICs, it can be concluded that such a tool is now ready and available for use in other LMICs.
Technical capacity in the use of the tool remains a concern, however. Although a manual and other materials have been developed to enable new users to familiarise themselves with the OneHealth tool generally and the MNS module more specifically, the acquired experience of testing it out in Emerald countries suggests that expertise in its deployment only comes about after dedicated training, prolonged practice and follow-up support from its developers (or their consultants). This is especially true for considering health system components, such as infrastructure, logistics, governance and fiscal space, which are an integral part of the tool but require such a breadth of information and knowledge about health systems and plans that it can be a challenge to populate and use. Moreover, identification and measurement of shared health system costs is most applicable to a genuine sector-wide resource need assessment that covers many or all diseases (as well as any underlying preventable risk factors), and less so for a programme-oriented analysis such as that aimed for in the current developmental phase. A further issue concerns the development and distribution of version updates of the OHT software, which particularly in the latter stages of testing and calibration caused a number of compatibility problems that led to delays and confusion among country-based users.
A second broad concern relates to the available evidence in these countries on a number of domains. These include epidemiological data on the burden and course of MNS disorders, the extent of current coverage and expenditure, and the evidence base for locally adapted cost-effective interventions. While the current tool makes use of the best available local evidence, further iterations of this tool will need to draw on new and better quality evidence as it becomes available.
Nevertheless, and due to the capacity-building activities made possible through Emerald project resources, new estimates of the resource needs, costs and health impacts of scaled-up mental health service delivery have been generated. Results of this estimation exercise indicate that the resource needs for scaling-up mental health services need not be substantial, particularly if priority disorders and cost-effective intervention strategies are judiciously selected. Using a spreadsheet-based tool for estimation, a separate costing study undertaken at the district level in five of the Emerald countries came to similar estimates of cost, for example showing that the cost per capita for delivering a specified package of interventions at target coverage levels ranged from US$ 0.39 to 0.69 per capita in low-income countries such as Ethiopia and Uganda (Chisholm et al. 2015).
The health returns on such an investment are substantial, as demonstrated by the additional number of healthy life years that are generated over the scaling-up period. Such information on the costs and health impacts of scale-up provides important evidence that can be brought to bear in dialogue with health planners and policymakers at the national level, particularly in the context of increased policy attention to the rising burden of non-communicable diseases. In Ethiopia, for example, an earlier cost estimation exercise helped to articulate the resource requirements underlying the objectives of a new Mental Health strategy (Federal Democratic Republic of Ethiopia Ministry of Health, 2012), while the ongoing work using OHT provided a timely analysis as the national government sought to implement an ambitious plan of mental health scale up across the country. Similarly in India, where a national mental health plan has just been launched, the findings from this work can make a useful contribution to state-level deliberations on the implementation of this plan, especially in Madhya Pradesh where the local Emerald research team is based.
Estimates reported herein represent an initial set of projections, based on locally available evidence and the informed inputs of local experts; however, such estimates are subject to further discussion, review and revision as planning cycles and political processes evolve. Looking ahead, therefore, plans are in place to further engage with local planners and policy makers in each of the countries via policy workshops, where key findings from this work can be presented and discussed. New projections will be prepared in the light of changes to policies and plans, such as revised target coverage levels or lengthened implementation periods. Modelling of other MNS disorders in certain countries where these have been identified as a key priority or as an integral component of national mental health strategies can also be undertaken. For example, bipolar disorder would be included in future projections for Ethiopia, and alcohol dependence in South Africa. More work will also be conducted on the integration of the MNS module of OHT into a broader, sector-wide analysis of health system constraints and needs; this requires more involved effort as the scope of analysis stretches to inclusion of other priority programmes. For example in the South African context, where an integrated approach to chronic disease management and prevention is being rolled out, findings and estimates from the MNS module can be linked to other disease-specific programme needs, with a view to determining overall health system requirements for human resources, infrastructural development and financing.
Acknowledgements
The research leading to these results is funded by the European Union's Seventh Framework Programme (FP7/2007-2013) under grant agreement no 305968. The funder had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. We would like to thank all expert panel members who participated in this study. We also acknowledge the contribution of Dr Anita Patel to initial discussions about the tool's development.
Disclaimer
D.C. is a staff member of the World Health Organization. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions, policy or views of the World Health Organization
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of Interests
The authors declare no competing interests.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796016000408.
click here to view supplementary material
References
- Alem A, Kebede D, Fekadu A, Shibre T, Fekadu D, Beyero T, Medhin G, Negash A, Kullgren G (2009). Clinical course and outcome of schizophrenia in a predominantly treatment-naive cohort in rural Ethiopia. Schizophrenia Bulletin 35, 646–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chisholm D, Saxena S (2012). Cost effectiveness of strategies to combat neuropsychiatric conditions in sub-Saharan Africa and South East Asia: mathematical modelling study. British Medical Journal 344, e609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chisholm D, Lund C, Saxena S (2007). Cost of scaling up mental healthcare in low- and middle-income countries. British Journal of Psychiatry 191, 528–535. [DOI] [PubMed] [Google Scholar]
- Chisholm D, Burman-Roy S, Fekadu A, Kathree T, Kizza D, Luitel NP, Petersen I, Shidhaye R, De Silva M, Lund C (2015). Estimating the cost of implementing district mental healthcare plans in five low- and middle-income countries: the PRIME study. British Journal of Psychiatry 208 (Suppl. 56), s71–s78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Democratic Republic of Ethiopia Ministry of Health (2012). National Mental Health Strategy 2012/13–2015/16. Federal Democratic Republic of Ethiopia Ministry of Health: Ethiopia. [Google Scholar]
- Gilbert B, Patel V, Farmer P, Lu C (2015). Assessing development assistance for mental health in developing countries: 2007–2013. PLoS Medicine 12, e1001834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanlon C, Luitel NP, Kathree T, Murhar V, Shrivasta S, Medhin G, Ssebunnya J, Fekadu A, Shidhaye R, Petersen I, Jordans M, Kigozi F, Thornicroft G, Patel V, Tomlinson M, Lund C, Breuer E, De Silva M, Prince M (2014). Challenges and opportunities for implementing integrated mental health care: a district level situation analysis from five low- and middle-income countries. PLoS ONE 9, e88437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyman S, Chisholm D, Kessler R, Patel V, Whiteford H (2006). Mental disorders In Disease Control Priorities in Developing Countries, 2nd edn, Chapter 31 (ed. Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Jha P, Mills A and Musgrove P), pp. 605–626. Oxford University Press and The World Bank: New York. [Google Scholar]
- Kebede D, Alem A, Shibre T, Fekadu A, Fekadu D, Kullgren G, Jacobbson L (2000). The Butajira-Ethiopia study on the incidence, course and outcome of schizophrenia and bipolar disorders. I. Descriptions of study settings, methods and preliminary results. Schizophrenia Research 41, 78. [Google Scholar]
- Patel V, Chisholm D, Parikh R, Charlson F, Degenhardt L, Dua T, Ferrari AL, Hyman S, Laxminarayan R, Levin C, Lund C, Medina-Mora M, Petersen I, Scott J, Shidhaye R, Vijayakumar L, Thornicroft T, Whiteford H (2015). Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edn. Lancet 387, 1672–1685. [DOI] [PubMed] [Google Scholar]
- Salomon J, Vos T, Hogan DR, Gagnon M, Naghavi M, Mokdad A, Begum N, Shah R, Karyana M, Kosen S, Farje MR, Moncada G, Dutta A, Sazawal S, Dyer A, Seiler J, Aboyans V, Baker L, Baxter A, Benjamin EJ, Bhalla K, Bin Abdulhak A, Blyth F, Bourne R, Braithwaite T, Brooks P, Brugha TS, Bryan-Hancock C, Buchbinder R, Burney P, Calabria B, Chen H, Chugh SS, Cooley R, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, Davis A, Degenhardt L, Díaz-Torné C, Dorsey ER, Driscoll T, Edmond K, Elbaz A, Ezzati M, Feigin V, Ferri CP, Flaxman AD, Flood L, Fransen M, Fuse K, Gabbe BJ, Gillum RF, Haagsma J, Harrison JE, Havmoeller R, Hay RJ, Hel-Baqui A, Hoek HW, Hoffman H, Hogeland E, Hoy D, Jarvis D, Karthikeyan G, Knowlton LM, Lathlean T, Leasher JL, Lim SS, Lipshultz SE, Lopez AD, Lozano R, Lyons R, Malekzadeh R, Marcenes W, March L, Margolis DJ, McGill N, McGrath J, Mensah GA, Meyer AC, Michaud C, Moran A, Mori R, Murdoch ME, Naldi L, Newton CR, Norman R, Omer SB, Osborne R, Pearce N, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Pourmalek F, Prince M, Rehm JT, Remuzzi G, Richardson K, Room R, Saha S, Sampson U, Sanchez-Riera L, Segui-Gomez M, Shahraz S, Shibuya K, Singh D, Sliwa K, Smith E, Soerjomataram I, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Taylor HR, Tleyjeh IM, van der Werf MJ, Watson WL, Weatherall DJ, Weintraub R, Weisskopf MG, Whiteford H, Wilkinson JD, Woolf AD, Zheng ZJ, Murray CJ, Jonas JB (2012). Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet 380, 2129–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semrau M, Evans-Lacko S, Alem A, Ayuso-Mateos JL, Chisholm D, Gureje O, Hanlon C, Jordans M, Kigozi F, Lempp H, Lund C, Petersen I, Shidhaye R, Thornicroft G (2015). Strengthening mental health systems in low- and middle-income countries: the Emerald programme. BMC Medicine 13, 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stenberg K, Chisholm D (2012). Resource needs for addressing noncommunicable disease in low- and middle-income countries: current and future developments. Global Heart 7, 53–60. [DOI] [PubMed] [Google Scholar]
- Whiteford H, Degenhardt L, Rehm J, Baxter A, Ferrari A, Erskine HE, Charlson FJ, Norman R, Flaxman A, Johns N, Burstein R, Murray CJL, Vos T (2013). Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 382, 1575–1586. [DOI] [PubMed] [Google Scholar]
- WHO (2010). mhGAP (Mental Health Gap Action Programme) Intervention Guide. World Health Organization: Geneva. [Google Scholar]
- WHO (2015). Mental Health Atlas 2014. World Health Organization: Geneva. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796016000408.
click here to view supplementary material
Data Availability Statement
Data extracted from OHT and used for the purpose of this article can be found at the following Dropbox folder: https://www.dropbox.com/sh/pngvjw1mxziejpg/AADn2cHSL6Vw_xwbMkpqT61Ja?dl=0