INTRODUCTION
Hospital volume has been shown to be inversely correlated with surgical mortality rates in complex surgery including pancreatectomy.1, 2 Based on this, there has been a push for regionalization of complex surgical procedures to high-volume centers, with several major medical health systems pledging to adopt the policy.3, 4 However, regionalization may increase travelling times, which imposes financial burdens and time demands on patients.5
On one hand, the intended mortality benefit may be realized if patients are able and willing to travel the added distance for better outcomes. For example, many would be willing to travel for vacation and major purchases, and should therefore be even more willing to do so for their own health care. On the other hand, not all patients have the needed resources to travel, especially marginalized populations. Moreover, it is important to note that while the added travel may only equate to a single trip for the patient’s operation, it will translate to multiple trips for their family members and loved ones, including additional overnight lodging that are not covered by insurance. Additionally, the added travel time would also factor into the needed preoperative clinic, postoperative follow-up, adjuvant treatment and long-term surveillance appointments.
Before this debate can be appropriately addressed, the first step is to quantitatively assess the real-world magnitude of the impact of a volume-based regionalization policy on travel times. Therefore, the aim of this study is to simulate the regionalization of pancreatectomies to quantitatively assess the impact of a proposed low-volume threshold policy on spatial access in terms of patient and family driving times. We selected pancreatectomy as the procedure of choice given that hospital volume had the most drastic impact on perioperative mortality compared to other gastrointestinal operations.2 We hypothesized that a simulated regionalization policy would significantly increase the required driving times for patients undergoing pancreatectomy and their families.
METHODS
Patient population
This study was exempted from review by the Partners Human Research Committee, the Institutional Review Board of Partners HealthCare (protocol no 2017P001211). All patients who underwent a pancreatectomy from 2005 to 2014 were identified using the California Office of Statewide Health Planning and Development (OSHPD) database. The California OSHPD database captures all episodes of patient care across all California-licensed facilities regardless of age or payer status. Each patient is assigned a unique identifier to capture his or her progression through the healthcare system (inpatient, ambulatory surgery, and emergency department care episodes) over time. Additionally, OSHPD is linked to the California Department of Public Health Death Statistical Master File for mortality records. Patients undergoing pancreatectomy were identified by International Classification of Diseases, Ninth Revision (ICD-9) procedure codes of 52.51, 52.52, 52.53, 52.59, 52.6 and 52.7 as a primary or secondary procedure in the inpatient database.
Variable definitions
Patient demographic variables such as age, gender, race, ethnicity and ZIP code of residence were self-reported by patients and captured by the OSHPD database. Patients’ payer status indicates the expected principal source of payment. Medicare or Medicaid patients covered under health maintenance organizations (HMO) were reported as source of payment Medicare or Medicaid. In-hospital mortality was captured by the designation of “died” under the “disposition of patient” variable. Annual case volume was determined for each hospital year. High-volume centers were defined as hospitals that perform >20 pancreatectomies per year.6
Simulated regionalization algorithm
Hospital street addresses were obtained from OSHPD’s hospital annual financial disclosure files.7 Round-trip driving times between patients’ residences and hospitals were obtained using the Google Maps™ Application Program Interface (API) Web Services Python client library (Google, Mountainview, CA).8 For patients included in the study, their home ZIP code and destination hospital address were imported into a custom database using DB Browser for SQLite (open-source software available at https://sqlitebrowser.org/). Origin for each patient was defined as the centroid of their listed ZIP code in the OSHPD database, while the destination was defined as the main address for the hospital at which they were treated. In the case of the simulated model, the alternative hospital’s main address was used as the destination. Driving duration was obtained for all included patients within the OSHPD database. Because driving times can vary based on traffic during the time of day, average driving times throughout the day were used for each patient as determined by Google Maps™’s API.
Simulated regionalization was performed by eliminating hospitals below a pre-determined volume threshold, and reassigning patients to the next closest hospital that satisfies the threshold. The median driving time was then recalculated for the population, and this was repeated for different volume thresholds. Similarly, the in-hospital mortality rate for the population was recalculated by having the reassigned patients assume the reassigned hospitals’ mortality rates for that year. The primary analysis was performed by simulating a volume-threshold of at least 20 cases per year.
Sensitivity analysis
In an effort to assess the generalizability of our findings to other states with different population and hospital densities and geography influences, the simulated regionalization procedure was similarly performed for the New York state population. This was done using the Statewide Planning and Research Cooperative System (SPARCS) database, a comprehensive all-payer data reporting system that collects information on discharges from all hospitals in the state of New York. Similarly, to account for the potential that certain hospitals only accept selected payers, we also performed the simulated regionalization procedure for California’s Medicare patients only.
Statistical analysis
Maps were created using ArcMap™ and ArcGIS® software (Esri, Redlands, CA). Statistical analyses were performed using Intercooled Stata software, version 15.0 (StataCorp, College Station, TX). Categorical variables were expressed in counts and percentages and analyzed comparatively using Pearson chi-square tests. Continuous variables were expressed in means ± standard deviations or median with interquartile ranges for normal and non-normal distribution of data respectively. Student T-tests and Kruskal-Wallis tests were used to analyze continuous variables with normal and non-normal distribution respectively. All tests were performed 2-sided, and statistical significance was accepted at the p-value≤0.05 level.
RESULTS
Patient demographics
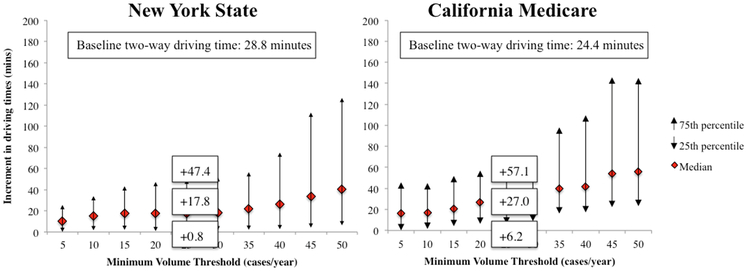
We identified 13,317 patients who underwent pancreatectomy in California during the study period, of whom 6,982 (52.4%) underwent the procedure at a high-volume center and 5,347 (40.2%) at teaching hospitals. In the most recent study year of 2014, there were a total of 128 hospitals; 109 (85.2%) were low-volume hospitals and 19 (14.8%) high-volume hospitals, with their geographic distribution displayed in Figure 1. The median age for the cohort was 63.0 years (IQR 52.0–72.0 years), with an equal distribution of male and female patients (Table 1). Almost 60% of patients were non-Hispanic White, with another 18.7%, 12.5% and 6.4% of patients identifying as Hispanics, Asian/Pacific Islanders and African American respectively. Most (44.9%) patients were on Medicare, with another 39.6% being covered by HMOs.
Figure 1.
A, Density map of patients who required pancreatectomy based on patient ZIP code and B, the distribution of low- (<20 cases/year) and high-volume (≥20 cases/year) hospitals for pancreatectomy in California in 2014.
Adapted from Fong ZV, Loehrer AP, Fernandez-Del Castillo C, et al. Potential impact of a volume pledge on spatial access: A population-level analysis of patients undergoing pancreatectomy. Surgery 2017; 162:203-210.
Table 1.
Demographics for patients who underwent a pancreatectomy in California during the study period.
| n=13,317 | |
|---|---|
| Age, median (IQR) | 63.0 (53.0, 72.0) |
| Female | 6,842 (51.4%) |
| Race | |
| Non-Hispanic White | 7,904 (59.6%) |
| Hispanic | 2,473 (18.7%) |
| Asian/Pacific Islander | 1,654 (12.5%) |
| African American | 853 (6.4%) |
| Other | 370 (2.8%) |
| Payer status | |
| Medicare | 5,976 (44.9%) |
| HMO private | 5,270 (39.6%) |
| Medicaid | 1,167 (8.8%) |
| Self-pay | 547 (4.1%) |
| Non-HMO private | 301 (2.3%) |
| Other | 56 (0.4%) |
| Teaching hospital | 5,347 (40.2%) |
| High-volume center* | 6,982 (52.4%) |
, High-volume center defined by centers performing >20 pancreatectomies/year.
Simulated regionalization
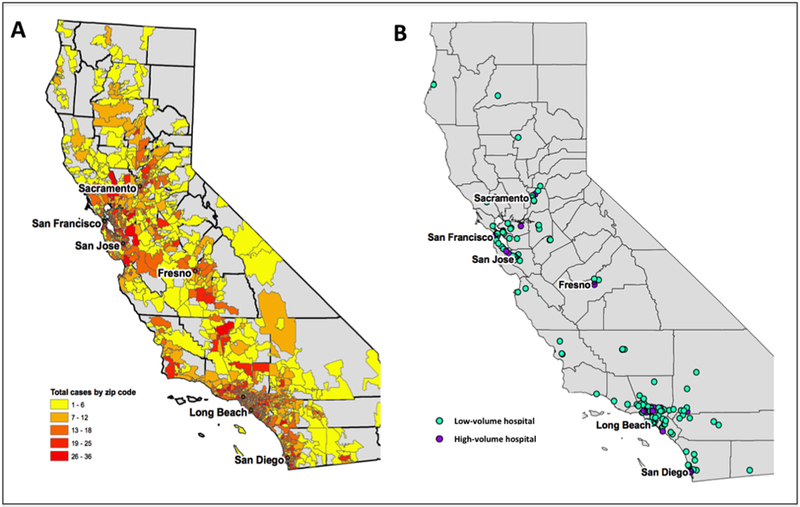
At baseline, patients who underwent pancreatectomy traveled a median of 49.8 minutes (IQR 30.8–96.2 minutes) for a round-trip. An access-restriction policy with a 20 cases per year threshold would increase median round-trip driving time by 24.1 minutes (IQR 4.5–53.5 minutes, Figure 2). This increment in round-trip driving time goes up by as much as 30.9 minutes (IQR 7.8–63.2 minutes) when the threshold was set at 30 cases per year. At a threshold of 20 cases per year, population mortality rates were predicted to decrease from 4.3% to 2.8% (p<0.001). When the threshold was set at 30 cases per year, the predicted population mortality rate was 2.9%, which was still significantly better than baseline (p<0.001) but no different than the 20 cases per year threshold (p=0.582).
Figure 2.
The impact of an increasing minimum pancreatectomy volume threshold on the increment in two-way driving times for patients and their caregivers in California.
Affected patients
Using a volume-threshold of 20 cases per year, we assessed the demographics of patients who would be affected by the simulated regionalization (Table 2). There were no differences in the age and gender distribution of patients who were affected by the simulated regionalization. There were higher proportions of African American (8.3% vs 4.8% of unaffected group) and Hispanic (22.3% vs 15.4% of unaffected group, p<0.001) patients who were affected by the simulated regionalization. Conversely, fewer non-Hispanic Whites were affected (55.4% vs 63.5% of unaffected group, p<0.001). When assessing patient payer status, more patients classified as Medicaid (10.8% vs 6.9% of unaffected group, p<0.001) and self-pay (5.5% vs 2.9% of unaffected group, p<0.001) were affected, while fewer HMO private patients (36.8% vs 42.1% of unaffected group, p<0.001) were affected by the simulated regionalization.
Table 2.
Demographics for patients affected by a 20-pancreatectomy/year minimum volume threshold.
| California | |||
|---|---|---|---|
| Unaffected group, n (%) n = 6,982 |
Affected group, n (%) n = 6,335 |
p-value | |
| Age, years | 64 (IQR 54-72) | 63 (IQR 53-72) | 0.109 |
| Female | 3,540 (50.7) | 3,302 (52.1) | 0.099 |
| Race | <0.001 | ||
| Non-Hispanic White | 4,414 (63.5) | 3,490 (55.4) | |
| Hispanic | 1,068 (15.4) | 1,405 (22.3) | |
| Asian/Pacific Islander | 918 (13.2) | 736 (11.7) | |
| African American | 332 (4.8) | 521 (8.3) | |
| Other | 219 (3.2) | 151 (2.4) | |
| Payer status | 3,201 (45.9) | 2,775 (43.8) | <0.001 |
| Medicare | 2,936 (42.1) | 2,334 (36.8) | |
| HMO private | 2,936 (42.1) | 2,334 (36.8) | |
| Medicaid | 483 (6.9) | 347 (5.5) | |
| Self-pay | 200 (2.9) | 166 (2.6) | |
| Non-HMO private | 27 (0.4) | 29 (0.5) | |
| Other | |||
| Teaching hospital | 4,671 (66.9%) | 676 (10.7%) | <0.001 |
Sensitivity analysis
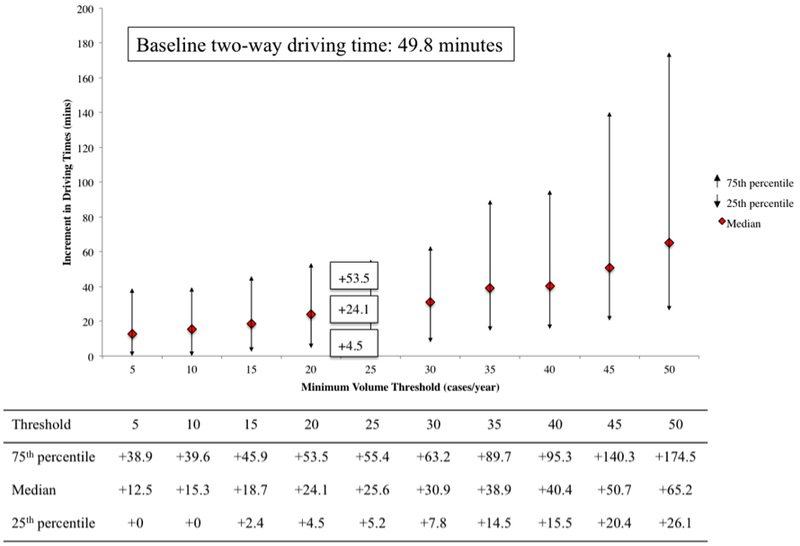
To account for the potential influence of geography, we performed the 20 cases per year threshold simulated regionalization procedure using the SPARCS dataset to represent a New York population. In New York, the baseline driving time for a round-trip was 28.8 minutes, and the simulation would increase round-trip driving times by 17.8 minutes (IQR 0.8–47.4 minutes, Figure 3). To account for insurance coverage, we also performed another sensitivity analysis with the California data that only included Medicare patients and demonstrated a baseline driving time of 24.4 minutes, with a 27.0-minute increment (IQR 6.2–57.1 minutes, Figure 3) with the simulation
Figure 3.
Sensitivity analysis comparing the impact of an increasing minimum pancreatectomy volume threshold on two-way driving times in New York State and Medicare patients in California.
DISCUSSION
In a statewide analysis of 13,317 patients undergoing pancreatectomy in California, patients traveled a median of 49.8 minutes for a round-trip to receive their operations. In our simulated regionalization with a volume-threshold of 20 cases per year, we found that round-trip driving time would be increased by 24 minutes, and up to 54 minutes for 25% of the population. Population mortality rates were predicted to decrease from 4.3% to 2.8%. Such a regionalization policy would impact over 50% of patients and up to 85% of hospitals secondary to facility closures. Racial minorities and uninsured patients were disproportionately affected by the policy when compared to non-Hispanic White and privately insured patients respectively.
Proponents of regionalization advocate minimum-volume standards that will bar hospitals not meeting the threshold from performing complex surgery, with several major medical health systems pledging to adopt the policy.3 Other health systems are hesitant to commit to the policy, as its implications and tradeoff between improved outcomes and decreased access to care are not fully understood.5 Such implications should be determined before widespread implementation of a proposed low-volume threshold mandate. Our analysis demonstrated a median 24-minute increment in round-trip driving time, with a 1.5% predicted decrease in mortality rate when regionalization was simulated with the proposed threshold. Just as importantly, the increase in driving time was as high as 54 minutes for 25% of the population. It is important to note that this 24-minute increase represents a minimum increment; our estimates obtained from Google Maps™ optimize travel routes and provide best-case estimates.9, 10 This increase is realistically much greater, depending on the route chosen by patients, road conditions, and traffic during rush hour. Additionally, patients with fewer resources may be dependent on public transportation, and its availability and efficiency may significantly increase traveling times beyond our conservative estimates.
It is also important to recognize that while this increment in travel times would only apply once to patients for their operation’s hospital stay, it would apply 7 times to their family caregivers for a typical median length of hospital stay of 7 days if they were to visit daily.11, 12 Additionally, it would further impact both patients and their caregivers when accounting for required visits for adjuvant therapy, follow-up and surveillance appointments. Fragmentation of care may also contribute to lapses in care quality should patients choose to receive adjuvant therapy and follow-up closer to home,13, 14 although recent advances in telemedicine have provided a reason for optimism.15
When assessing the real-life impact of the simulated regionalization, we found that 6,335 patients and 246 hospitals would have been affected throughout the study period. If implemented, a volume-restriction policy would undoubtly impose resource constraints and capacity issues for high-volume hospitals, and may not be practical.16 It could potentially cause longer wait times and delays in receipt of pancreatectomy, of which its clinical significance remains unknown but great concern exists that it could adversely affect patient survival in a biologically aggressive disease like pancreatic cancer.17
Additionally, we also found that a volume-restriction policy would disproportionately impact racial and ethnic minorities, Medicaid and uninsured patients in our simulation model. In an analysis of 719,608 patients across 10 complex operations, Liu and colleagues demonstrated that black, Asian and Hispanic patients were significantly less likely to receive care at high-volume centers when compared to white patients.18 Medicaid and uninsured patients were also less likely to receive care at high-volume centers when compared to privately insured patients.18-20 Taken together, a volume-restriction policy may exacerbate existing disparities in spatial access to care.
In an effort to account for potential biases that may be introduced by geographical differences on the impact of the simulated regionalization algorithm, we performed a sensitivity analysis simulating regionalization in an all-payer New York State database. The discrepancy in the increase in driving times highlights the importance of tailoring geospatial analysis to specific states instead of general analyses that don’t differentiate state-lines typically seen with Medicare claims analyses.21 Similarly, regionalization policies, if implemented, should not be sweepingly enforced throughout the country and should be tailored towards each state’s specific population density and facility distribution (Figure 1).22 Like politics, healthcare is local, and policies should be personalized to individual states.
To eliminate potential confounding from insurance restrictions, we also performed a second sensitivity analysis of only Medicare patients and found a similar increment in travel times under the simulated regionalization algorithm. This suggests that the current underutilization of high-volume centers by vulnerable populations extends beyond the lack of insurance coverage, with travel distances potentially playing a more prominent role in the issue.23 In fact, McDermott et al recently reported that the Affordable Care Act’s Medicaid expansion had no impact on both the utilization rates of high-volume hospitals by vulnerable populations or the narrowing of disparities,24 further supporting the importance of non-insurance related barriers, such as spatial access.
One of the strengths of our analysis is that California represents the nation’s most racially/ethnically diverse state,25 allowing us to meaningfully assess the impact of volume-based regionalization on a diverse racial/ethnic and payer group of patients. Our sensitivity analysis population, New York State, is the fourth most populous state in the country with an estimated 19.6 million residents in 2014, allowing us to perform the analysis in a large cohort in the Northeast. Importantly, we demonstrated the feasibility of merging Google Maps™ data with an administrative state database for spatial access analysis. Historically, studies analyzing travel distances operationalize the measure as “the crow flies”, i.e. a straight-line distance between two points.22, 26-31 Utilizing map and traffic data allowed more than a straight-line analysis, and allowed us to account for both road networks and local traffic patterns.
However, our study should also be interpreted in the context of its design. While we accounted for insurance status with our sensitivity analysis, we could not account for the influence of local referral networks. Additionally, our findings may not be generalizable to the rest of the country. Our findings with the New York State analysis suggest that we should not be generalizing these findings and each state should be individually assessed if a volume threshold policy were to be implemented. The driving times were also calculated using Google Maps™ that selects the fastest route and provide best-case numbers. There may also be a proportion of patients without the means to drive, who depend on public transportation for their travels. Taken together, our simulation may underestimate the true burden of any added traveling time. Finally, while we assume that an increment in 24 minutes of driving time is significant to patients, their true perception, preferences and ability to travel for better outcomes are unknown.32 Current investigations by our group are underway to further delineate this in actual patients who require complex operations.
In conclusion, a policy that limits access to low-volume pancreatectomy hospitals could increase round-trip driving time by 24 minutes for patients and their family caregivers, but up to 54 minutes for 25% of them. Population mortality rates may improve by 1.5%. Racial minorities and the uninsured would be most affected. Further work is needed to better delineate patients’ ability, preferences, and willingness to travel for improved outcomes when requiring complex operations.
Acknowledgments
DISCLOSURES
This study was supported by the National Cancer Institute of the National Institute of Health under award number: F32CA217455 and the Andrew L Warshaw, MD Institute for Pancreatic Cancer Research Grant under award number: 0004852948.
Daniel Hashimoto was partially funded by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institute of Health grant T32DK007754–17 for this work. He is an independent consultant for Verily Life Sciences, the Johnson & Johnson Institute, and Gerson Lehrman Group. He receives research support from Olympus Corporation for unrelated research.
REFERENCES
- 1.Begg CB, Cramer LD, Hoskins WJ, et al. Impact of hospital volume on operative mortality for major cancer surgery. JAMA 1998; 280:1747–51. [DOI] [PubMed] [Google Scholar]
- 2.Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon volume and operative mortality in the United States. N Engl J Med 2003; 349:2117–27. [DOI] [PubMed] [Google Scholar]
- 3.Sternberg S Hospitals Move to limit Low-Volume Surgeries 2015. Available at: http://www.usnews.com/news/articles/2015/05/19/hospitals-move-to-limit-low-volume-surgeries. Accessed 5/27/2016. [Google Scholar]
- 4.Pronovost P, Higgins RS. Mastery of Care-toward Communitarian Regulation. Ann Surg 2017; 265:271–272. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz DM, Fong ZV, Warshaw AL, et al. The Hidden Consequences of the Volume Pledge: “No Patient Left Behind”? Ann Surg 2016. [DOI] [PubMed] [Google Scholar]
- 6.Urbach DR. Pledging to Eliminate Low-Volume Surgery. N Engl J Med 2015; 373:1388–90. [DOI] [PubMed] [Google Scholar]
- 7.OSHPD Hospital Financials. Available at: https://oshpd.ca.gov/data-and-reports/cost-transparency/hospital-financials/. Accessed February 24, 2019.
- 8.GitHub. Python client library for Google Maps API Web Services. Available at: https://github.com/googlemaps/google-maps-services-python. Accessed February 28, 2019.
- 9.Seefeld B Meet the new Google Maps: A map for every person and place 2013. Available at: https://maps.googleblog.com/2013/05/meet-new-google-maps-map-for-every.html. Accessed April 24, 2019. [Google Scholar]
- 10.Waibel JMM. Optimized route planning and personalized real-time location-based travel management In Patent US, ed., Vol. US 9.261.374 B2. United States: Routerank ltd., 2016. [Google Scholar]
- 11.Fong ZV, Ferrone CR, Thayer SP, et al. Understanding hospital readmissions after pancreaticoduodenectomy: can we prevent them?: a 10-year contemporary experience with 1,173 patients at the Massachusetts General Hospital. J Gastrointest Surg 2014; 18:137–44; discussion 144–5. [DOI] [PubMed] [Google Scholar]
- 12.Lee GC, Fong ZV, Ferrone CR, et al. High performing whipple patients: factors associated with short length of stay after open pancreaticoduodenectomy. J Gastrointest Surg 2014; 18:1760–9. [DOI] [PubMed] [Google Scholar]
- 13.Tsai TC, Orav EJ, Jha AK. Care fragmentation in the postdischarge period: surgical readmissions, distance of travel, and postoperative mortality. JAMA Surg 2015; 150:59–64. [DOI] [PubMed] [Google Scholar]
- 14.Frandsen BR, Joynt KE, Rebitzer JB, et al. Care fragmentation, quality, and costs among chronically ill patients. Am J Manag Care 2015; 21:355–62. [PubMed] [Google Scholar]
- 15.Nikolian VC, Williams AM, Jacobs BN, et al. Pilot Study to Evaluate the Safety, Feasibility, and Financial Implications of a Postoperative Telemedicine Program. Ann Surg 2018; 268:700–707. [DOI] [PubMed] [Google Scholar]
- 16.Kahn JM, Asch RJ, Iwashyna TJ, et al. Perceived barriers to the regionalization of adult critical care in the United States: a qualitative preliminary study. BMC Health Serv Res 2008; 8:239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Winter JM, Brennan MF, Tang LH, et al. Survival after resection of pancreatic adenocarcinoma: results from a single institution over three decades. Ann Surg Oncol 2012; 19:169–75. [DOI] [PubMed] [Google Scholar]
- 18.Liu JH, Zingmond DS, McGory ML, et al. Disparities in the utilization of high-volume hospitals for complex surgery. JAMA 2006; 296:1973–80. [DOI] [PubMed] [Google Scholar]
- 19.Huang LC, Tran TB, Ma Y, et al. Factors that influence minority use of high-volume hospitals for colorectal cancer care. Dis Colon Rectum 2015; 58:526–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scarborough JE, Pietrobon R, Clary BM, et al. Regionalization of hepatic resections is associated with increasing disparities among some patient populations in use of high-volume providers. J Am Coll Surg 2008; 207:831–8. [DOI] [PubMed] [Google Scholar]
- 21.Birkmeyer JD, Siewers AE, Marth NJ, et al. Regionalization of high-risk surgery and implications for patient travel times. JAMA 2003; 290:2703–8. [DOI] [PubMed] [Google Scholar]
- 22.Diaz A, Schoenbrunner A, Cloyd J, et al. Geographic Distribution of Adult Inpatient Surgery Capability in the USA. J Gastrointest Surg 2019. [DOI] [PubMed] [Google Scholar]
- 23.Loehrer AP, Chang DC, Song Z, et al. Health Reform and Utilization of High-Volume Hospitals for Complex Cancer Operations. J Oncol Pract 2018; 14:e42–e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McDermott J, Zeymo A, Chan K, et al. Affordable Care Act’s Medicaid Expansion and Use of Regionalized Surgery at High-Volume Hospitals. J Am Coll Surg 2018; 227:507–520 e9. [DOI] [PubMed] [Google Scholar]
- 25.McCann A Most & Least Diverse States in America 2018. Available at: https://wallethub.com/edu/most-least-diverse-states-in-america/38262/. Accessed April 9, 2019.
- 26.Stitzenberg KB, Sigurdson ER, Egleston BL, et al. Centralization of cancer surgery: implications for patient access to optimal care. J Clin Oncol 2009; 27:4671–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fong ZV, Loehrer AP, Fernandez-Del Castillo C, et al. Potential impact of a volume pledge on spatial access: A population-level analysis of patients undergoing pancreatectomy. Surgery 2017; 162:203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jindal M, Zheng C, Quadri HS, et al. Why Do Long-Distance Travelers Have Improved Pancreatectomy Outcomes? J Am Coll Surg 2017; 225:216–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lidsky ME, Sun Z, Nussbaum DP, et al. Going the Extra Mile: Improved Survival for Pancreatic Cancer Patients Traveling to High-volume Centers. Ann Surg 2016. [DOI] [PubMed] [Google Scholar]
- 30.Speicher PJ, Englum BR, Ganapathi AM, et al. Traveling to a High-volume Center is Associated With Improved Survival for Patients With Esophageal Cancer. Ann Surg 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kansagra SM, Curtis LH, Schulman KA. Regionalization of percutaneous transluminal coronary angioplasty and implications for patient travel distance. JAMA 2004; 292:1717–23. [DOI] [PubMed] [Google Scholar]
- 32.Resio BJ, Chiu AS, Hoag JR, et al. Motivators, Barriers, and Facilitators to Traveling to the Safest Hospitals in the United States for Complex Cancer Surgery. JAMA Netw Open 2018; 1:e184595. [DOI] [PMC free article] [PubMed] [Google Scholar]