Abstract
As more older adults undergo surgical procedures, it is incumbent upon us to learn how to provide them with the safest possible perioperative care. We conducted a retrospective cohort study at a large tertiary care center to determine whether outcomes following anesthesia-related adverse events differed between patients 65 and older versus patients under 65 years old. 1,424 cases were referred to the Performance Improvement committee of the Department of Anesthesiology from the years 2007-2015. After exclusions of cases that were not anesthesia related, could not be identified, or were duplicates, 747 cases with anesthesia-related adverse events were included in the study. 286 were ≥ age 65 and 461 were < age 65. Anesthesia-related adverse events occurred more commonly in the postoperative period in older patients relative to younger patients. (37.7% vs 21.9%, p = 0.001), and older patients had a greater incidence of mortality compared to a propensity-matched group of younger patients (adjusted odds ratio 1.87 (1.14-3.12), p <0.05). We concluded that older patients have a greater likelihood of mortality as a result of suffering an anesthesia-related adverse event and may benefit from increased vigilance in the postoperative period.
Keywords: Geriatrics, Patient Safety, Anesthesia
Introduction:
As the population ages, perioperative medical providers must understand the complexities of providing care to older patients. Older patients are living longer, undergoing more surgeries,1,2,3 and often present with multiple comorbidities. Older patients also have anatomic and physiologic changes that differ from the younger population that make the provision of safe anesthetic care more challenging.4,5 Indeed, older patients have been shown to suffer postoperative adverse events, including cerebrovascular accident, myocardial infarction, kidney injury, pneumonia, unplanned intubation, and mortality at greater rates than younger adults.6 Furthermore, when complications occur, failure to rescue is more common in older adults, leading to an increased risk of mortality following the complication.7-9 To date, no prior study has reported on adverse events in the perioperative period that are specifically anesthesia-related in older patients.
In a prior study we characterized anesthesia-related adverse events in patients of all ages including which organ systems were affected, the timing of the event in the perioperative period, the underlying cause of the event and whether it was preventable, and the ultimate outcome of the patient related to the adverse event.10 We undertook this secondary analysis of the dataset to compare anesthesia-related adverse events between patients age 65 and above versus those under the age of 65.
Methods:
This secondary analysis of our prior retrospective study7 was approved by the Institutional Review Board at Icahn School of Medicine at Mount Sinai, New York, NY. The requirement for written informed consent was waived.
At our institution, perioperative adverse events are reviewed by the Performance Improvement (PI) committee of the Department of Anesthesiology. The PI committee meets monthly in a closed session, and consists of approximately 20 board-certified anesthesiologists representing all subspecialties as well as chief residents and the chief nurse anesthetist. In addition to adverse events reviewed because they met departmental criteria for review, e.g., respiratory and cardiac arrest or neurologic injury, and those self-reported by anesthesiology personnel; the committee also reviews patient complaints, events referred through the hospital-wide electronic medical error reporting system, all mortalities within 48 hours of anesthetic care, and cases referred by other departmental PI committees.
Cases for review are first assigned to a member of the committee who performs a chart review, interviews the involved providers, and writes a detailed narrative and formal assessment of the adverse outcome. The case is then verbally presented to the PI committee. A detailed description of the case along with the committee’s assessment and corrective action plan, if applicable, are recorded in the monthly minutes. We performed a retrospective review of each anesthetic case presented to the anesthesiology department PI committee from 2007 to 2015. The review panel consisted of four anesthesiologists with subspecialties including pain (CC), obstetrics (YB), and neuroanesthesia (PM). One of the panelists is a former naval nuclear engineering officer with prior experience in critical incident study and root cause analysis (CC), and another panelist is board certified in clinical informatics (PM).
Two authors were assigned to review each year of cases. The pairings were switched for subsequent years so that all possible reviewer combinations were achieved. Materials available for review included the PI committee report, the anesthetic record (CompuRecord, Philips, Andover, MA), and the institutional electronic health record (Epic Systems Corporation, Verona, WI.) Using the Research Electronic Data Capture tool (REDCap; Vanderbilt University, Nashville, TN), data for each case was electronically entered by each reviewer.
Cases were excluded if the patient was unable to be identified, the case was a duplicate, no adverse event occurred, or the event was not anesthesia related. An example of “no adverse event occurred” is a case referred to the committee because of a patient complaint, however, no complication occurred. The “not anesthesia related” exclusion applied to cases where both reviewers independently agreed that the complication was clearly not due to a decision or action by the anesthesia team, e.g., a technical error by the surgeon.
Each study investigator reviewed the case and filled out the reporting template individually using a written taxonomy as guidance, which was jointly developed by all four investigators prior to starting the study. Investigators determined the underlying cause of the adverse event as adapted from Lagasse et al.11 This process is more fully described in our prior publication.10 We regarded two underlying causes: “limitation of therapeutic standard” and “limitation of diagnostic standard” as non-modifiable underlying causes, and therefore the adverse event was deemed non-preventable because either the patient and/or the surgical procedure was complex, and despite appropriate care there was an adverse event. Investigators also classified the type of adverse event for each case using a classification scheme derived from the Anesthesia Quality Institute (AQI) Anesthesia Incident Reporting System (AIRS).12 Adverse events categories included: Neurologic, Cardiac, Respiratory, Trauma, Hematologic, and Medication. Patient outcomes related to the event, including unplanned intensive care unit (ICU) admission, residual injury (defined as not returning to the patient’s baseline level of health), all cause death within 48 hours of the procedure, and death related to the adverse event at time of review were recorded. Demographic and comorbidity data (in the form of administrative diagnosis codes) were retrieved from the electronic medical record.
Finally, the pair of reviewers assigned to each case met in person to merge their case assessments using the REDCap double data entry tool. The tool provided a work list of cases with disparate reviewer responses, which were reviewed by the two investigators. A verbal agreement was reached on those items to produce a final, merged record. If agreement was unable to be reached, a group consensus was sought by discussion with the other two investigators.
After exclusions, the final dataset was divided into two groups for comparison, age < 65 and age ≥ 65.
Statistical Analysis
Data are presented as mean (standard deviation), median [quartile 1 – quartile 3], and count (percent). For comparisons between age groups, chi squared test was used for categorical variables and Wilcoxon rank-sum for continuous variables, with p < 0.05 considered significant. To account for differences in patient populations propensity matched scoring was performed on the data set. Patients were matched on the following variables: gender, Body Mass Index (BMI), ASA classification, presence of hypertension, diabetes, congestive heart failure, arrhythmia, valvular disease, peripheral vascular disease, neurologic disease, renal failure, hepatic failure, cancer, coagulopathy, Charleston Co-morbidity Index, specialty category, and total anesthesia time. These variables were chosen because they have been associated with poor outcomes after perioperative complications, or in the case of specialty category because they may represent a similar group of patients or procedures.13-26 After matching, a total of 210 matched pairs were included for further analysis. Differences between groups in outcomes (unplanned ICU admission, failure to return to baseline health, all-cause mortality within 48 hours of the anesthetic, and mortality related to the adverse event) found in univariate analysis were entered into a multivariable logistic regression analysis to assess for independence. We then performed sensitivity analyses by examining models of interaction terms and assessing different age cutoffs. All calculations were performed using R version 3.3.2 (R Foundation for Statistical Computing, Vienna, Austria.) The R package medicalrisk version 1.2 was used to determine Charlson Comorbidity Index values.27
Results:
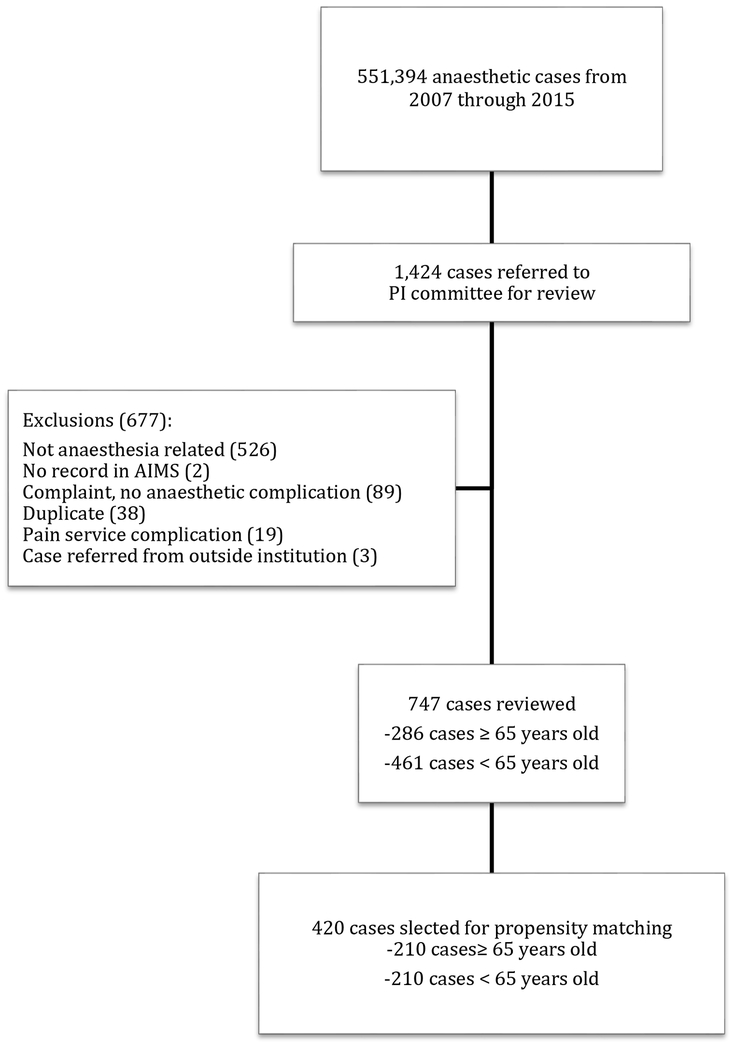
Of 551,394 anesthetics during the years 2007-2015, 144,353 (26.2%) were performed in patients ≥ 65 and 407,041 (73.8%) occurred in those < age 65. Overall during the study period, 1,424 records were referred to the PI committee for review (0.26%) and after exclusions, 747 were included in the final study; 286 (38.3%) were ≥ age 65 and 461 (61.7%) were < age 65 (Fig 1). Older patients were over-represented in the dataset, as 26.2% of all anesthetics were performed in older patients but 38.3% of the anesthesia-related events occurred in this group, p < 0.00001.
Figure 1:
Flow chart of case selection. The majority of cases excluded were because two reviewers independently agreed that the adverse event was unrelated to anesthetic management. PI = Performance Improvement; AIMS = Anesthesia Information Management System.
There were significant differences in the demographics and general state of health between the two patient groups. A higher percentage of patients ≥ 65 had an American Society of Anesthesiologists-Physical Status (ASA-PS) score >2 (91.3% vs 63.3%, p < 0.001). Older patients were also more often inpatient (92.0% vs 82.6%, p < 0.001), and had hypertension (79.7% vs 42.7% p < 0.001), diabetes (27.3% vs 16.7% p < 0.001), congestive heart failure (CHF) (28.0% vs 14.3%, p < 0.001), and pulmonary disease (28.3% vs 18.0% p < 0.001). The proportion of cases classified as emergent was similar between groups (17.8% vs 18.4%, p = 0.83), (Supplementary Table 1).
Propensity matching was used in an effort to control for the significant differences in baseline characteristics. The twenty-four specialty categories were constructed into five groups based on the general type of patient characteristics and anesthesia care provided.
There were no obstetric cases in patients over 65 in our original dataset, thus these case were excluded from the propensity matching. There were no significant differences in the underlying characteristics or comorbidities between the two groups in the propensity matched population, (Table 1).
Table 1.
Characteristics of the Propensity Matched Population Stratified by Age (n=420).
| <65 | ≥65 | p | |
|---|---|---|---|
| N (%) | 210 (100) | 210 (100) | |
| Specialty Category Group | |||
| Cardiac, Thoracic, Cardiology (%) | 49 ( 23.3) | 57 ( 27.1) | 0.432 |
| Dental, ENT, OMFS (%) | 15 ( 7.1) | 16 ( 7.6) | 1 |
| GI, Pulmonology, Psychiatry, IR, Radiology, Ophthalmology, Pain (%) | 22 ( 10.5) | 22 ( 10.5) | 1 |
| General/Colorectal, Gynecology, Plastics, Urology, Transplant, Vascular (%) | 93 ( 44.3) | 82 ( 39.0) | 0.322 |
| Neurosurgery, Orthopedics, Spine (%) | 33 ( 15.7) | 36 ( 17.1) | 0.792 |
| OB (%) | 0 ( 0) | 0 ( 0) | 1 |
| Female Gender (%) | 102 ( 48.6) | 92 ( 43.8) | 0.378 |
| BMI(median [IQR]) | 28.95 [23.28, 34.10] | 26.56 [23.82, 31.30] | 0.161 |
| ASA PS Score (%) | 0.902 | ||
| 1 | 5 ( 2.4) | 3 ( 1.4) | |
| 2 | 21 ( 10.0) | 22 ( 10.5) | |
| 3 | 92 ( 43.8) | 95 ( 45.2) | |
| 4 | 81 ( 38.6) | 82 ( 39.0) | |
| 5 | 11 ( 5.2) | 8 ( 3.8) | |
| Length of Anesthesia (mins) (median [IQR]) | 257.00 [143.25, 393.25] | 265.00 [175.00, 396.25] | 0.322 |
| Emergency Status (%) | 44 ( 21.0) | 40 ( 19.0) | 0.714 |
| Inpatient | 182 (86.7) | 189 (90) | 0.362 |
| Hypertension (%) | 148 ( 70.5) | 154 ( 73.3) | 0.587 |
| Diabetes (%) | 53 ( 25.2) | 59 ( 28.1) | 0.581 |
| CHF (%) | 51 ( 24.3) | 49 ( 23.3) | 0.909 |
| Pulmonary Disease (%) | 50 ( 23.8) | 53 ( 25.2) | 0.821 |
| Arrhythmia (%) | 69 ( 32.9) | 73 ( 34.8) | 0.757 |
| Valvular Disease 1 (%) | 30 ( 14.3) | 29 ( 13.8) | 1 |
| Pulmonary Circulation Disease(%) | 18 ( 8.6) | 21 ( 10.0) | 0.737 |
| Peripheral Vascular Disease (%) | 22 ( 10.5) | 28 ( 13.3) | 0.451 |
| Paralysis (%) | 7 ( 3.3) | 7 ( 3.3) | 1 |
| Neurological Disorders (%) | 24 ( 11.4) | 25 ( 11.9) | 1 |
| Hypothyroid (%) | 13 ( 6.2) | 15 ( 7.1) | 0.845 |
| Renal Failure (%) | 53 ( 25.2) | 48 ( 22.9) | 0.648 |
| Liver Disease (%) | 25 ( 11.9) | 23 ( 11.0) | 0.878 |
| Peptic Ulcer Disease (%) | 3 ( 1.4) | 2 ( 1.0) | 1 |
| Cancer (%) | 44 ( 21.0) | 46 ( 21.9) | 0.905 |
| Rheumatoid Arthritis (%) | 3 ( 1.4) | 4 ( 1.9) | 1 |
| Psychiatric Disease (%) | 22 ( 10.5) | 27 ( 12.9) | 0.543 |
ENT= Ear, Nose and Throat Surgery, OMF= Oral and Maxillofacial Surgery, GYN= Gynecological Surgery, IR= Interventional Radiology, OB= Obstetrics, BMI= Body Mass Index, ASA-PS= American Society of Anesthesiologists Physical Status Score, CHF= Congestive Heart Failure
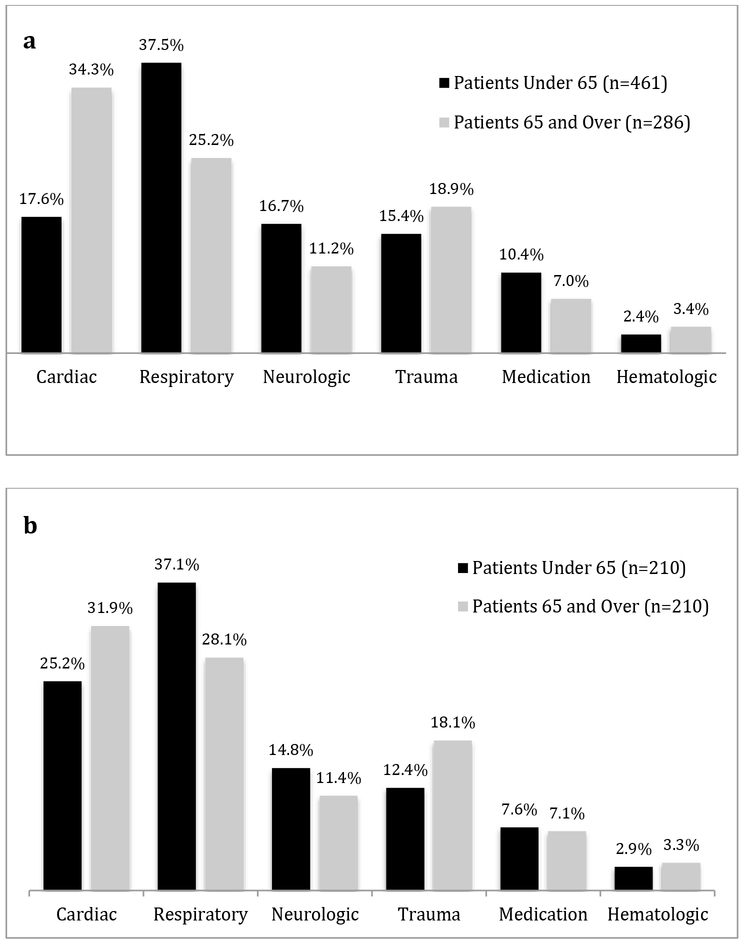
In the original dataset of 747 anesthesia-related adverse events, respiratory events (n= 245, 32.8%) were the most commonly reported adverse event category,followed by cardiac (n= 179, 24.0%), traumatic injuries (n= 125 16.7%), neurologic events (n= 110, 14.7%), medication errors (n= 68, 9.1%), and hematologic complications (n= 21, 2.8%).
There were significant differences in the distribution of adverse events between younger and older patients (Fig 2a) (P<0.0001). Cardiac events represented a larger portion of adverse events in older patients (34.3% vs 17.6% p < 0.0001) in the unmatched dataset. More specifically, cardiac arrest accounted for 23.1% of adverse events in older patients, versus 12.6% of adverse events in younger patients, p < 0.001. Within the propensity matched data set, the distribution of types of adverse events was not significantly different based on age p = 0.18 (Fig 2b). A complete list of adverse events for both age groups is included in Appendix A.
Figure 2.
a. Adverse event type by age (n=747). Cardiac events were more common in patients ≥ 65 years-old and respiratory events were more common in patients <65 years-old. p< 0.001
b. Adverse event types in the propensity-matched population (n=420) were not significantly different based on age. p = 0.18
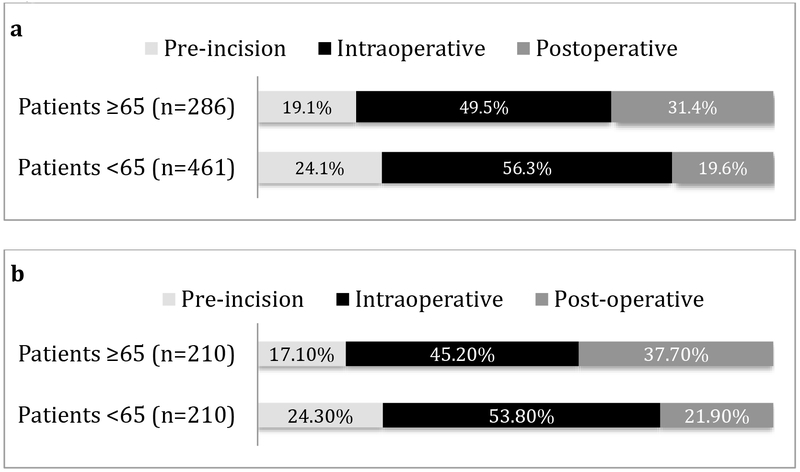
The percentage of events considered preventable was not different between older or younger patients (40.9% vs 44.0% P= 0.40). The timing of the adverse events was different between older and younger patients in both the unmatched dataset as well as in the propensity-matched data set (p=0.001). Events in younger patients occurred more frequently during the pre-incision period, whereas older patients experienced more adverse events in the postoperative period (Fig 3).
Figure 3.
a. Timing of adverse events in unmatched patient population (n=747).
b. Timing of adverse events in propensity matched population (n=420).
Pre-incision= induction, intubation, positioning. Intraoperative= from procedure start to procedure finish. Postoperative = emergence, extubation, transport, post-anesthesia care unit, intensive care unit/inpatient floor/home. Patients < 65 years-old had more pre-incision adverse events and patients ≥ 65 years-old had more postoperative adverse events. p = 0.001
The reviewers classified each event as being attributable to either a system or human cause. Overall, system causes accounted for 73.8% of all adverse events. There was not a significant difference noted in the proportion of events attributed to system causes between older and younger patients (76.9% vs 71.8%, p=0.14) (Table 2) An age-stratified table of adverse events by underlying cause is available in Appendix B.
Table 2.
Events by Primary Cause Stratified by Age.
| Total (n=747) | Age <65 (n=461) | Age ≥65 (n=286) | P value | |
|---|---|---|---|---|
| Primary Cause | 0.14 | |||
| System | 551 (73.8%) | 331 (71.8%) | 220 (76.9%) | |
| Human | 196 (26.2%) | 130 (28.2%) | 66(23.1%) |
Univariate logistic regression results from the unmatched dataset can be found in (Supplementary Table 2). Multivariable logistic regression analysis revealed that age ≥ 65 was independently associated with failure to return to baseline after the event, all cause 48-hour mortality, and overall mortality as a result of the adverse event. Emergency surgery was associated with all-cause death within 48 hours and mortality related to the event. ASA-PS score >2 was also an independent predictor of all three of these outcomes. (Supplementary Table 3)
In the propensity-matched data sets, age ≥65 remained a significant predictor of mortality related to the adverse event, but not failure to return to baseline or all-cause death within 48 hours. Increasing ASA-PS scores above 2 remained predictive of failure to return to baseline, all-cause death within 48-hours, and mortality related to the adverse event. Emergency surgery predicted both all-cause death within 48 hours and mortality related to the adverse event. (Table 3)
Table 3.
Adjusted Odds Ratio for Outcomes via Multivariable Logistic Regression on Propensity-matched Subgroup
| (n=420) | Return to Baseline (n=245) | Death within 48 hours (n=115) | Overall Mortality as a result of adverse event (n=76) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient Characteristic | AOR | 95% CI | p | AOR | 95% CI | p | AOR | 95% CI | p | |||
| Age ≥65 | 0.73 | 0.48 | 1.11 | 0.143 | 1.76 | 1.00 | 3.16 | 0.054 | 1.87 | 1.14 | 3.12 | 0.014 |
| ASA-PS Score 3 | 0.40 | 0.15 | 0.91 | 0.040 | 4.29 | 0.80 | 79.62 | 0.169 | 7.54 | 1.49 | 137.79 | 0.053 |
| ASA-PS Score 4 | 0.20 | 0.07 | 0.48 | 0.001 | 18.13 | 3.50 | 334.14 | 0.006 | 29.82 | 5.88 | 545.78 | 0.001 |
| ASA-PS Score 5 | 0.05 | 0.01 | 0.23 | <0.001 | 44.17 | 5.99 | 939.01 | 0.001 | 131.40 | 16.28 | 3019.85 | <0.001 |
| Emergency | 0.62 | 0.35 | 1.11 | 0.108 | 2.96 | 1.53 | 5.71 | 0.001 | 2.48 | 1.34 | 4.61 | 0.004 |
| Hypertension | 0.98 | 0.59 | 1.63 | 0.934 | 0.61 | 0.31 | 1.20 | 0.148 | 0.66 | 0.36 | 1.22 | 0.179 |
| Diabetes | 0.82 | 0.50 | 1.34 | 0.431 | 1.27 | 0.64 | 2.49 | 0.498 | 1.38 | 0.77 | 2.46 | 0.276 |
| Congestive Heart Failure | 0.95 | 0.56 | 1.62 | 0.847 | 0.88 | 0.43 | 1.74 | 0.715 | 1.10 | 0.60 | 2.00 | 0.758 |
| Pulm Disease | 1.09 | 0.67 | 1.78 | 0.741 | 0.38 | 0.17 | 0.78 | 0.012 | 0.63 | 0.34 | 1.14 | 0.132 |
AOR= Adjusted Odds Ratio, ASA-PS= American Society of Anesthesiologists Physical Status Score, for ASA-PS score, a score of 2 was used as the reference.
Pulm = pulmonary
As part of the sensitivity analysis, the logistic regressions were run utilizing different age cutoffs. Age ≥55 was independently predictive of overall mortality as a result of an adverse event, Age ≥ 75 was independently predictive of failure to return to baseline, death within 48 hours, and overall mortality as a result of the event. (Supplementary Table 4) When the population is constrained to patients between 55 and 75 years old, or 60-70 years old, age over 65 ceases to be predictive of adverse outcomes, which may indicate that the effect is more concentrated at the extremes of the older population. (Supplementary table 5)
Limitations:
This study has several limitations. It is a single institution study, and the distribution of adverse events may be different in other practice settings. Minor adverse events that occurred during the study period but were not significant enough to be reported to the PI committee would not have been included in the study. It is also possible that significant adverse events occurred over the study period that were not reported to the PI committee. The decisions to exclude cases are to some extent subjective. Excluding cases for being “not anesthesia related” has been done in prior studies of adverse events. Previous studies have utilized screening by a single anesthesiologist to determine whether a case required further review.28-30 Our study design required two anesthesiologists to independently review each case to help strengthen the quality of the data reviewed. Furthermore, our sample was too small to make significant conclusions about specific subtypes of adverse events beyond the 6 broad adverse event categories discussed here. Additionally, any comparison of populations is vulnerable to omitted variable bias. Though our propensity models attempt to control for non-age differences within the groups, we are only able to control for a limited number of factors thus it is possible that omitted variables (e.g. measures of frailty, baseline cognitive function, lab results, other unmeasured characteristics), impacted our observed results.
Discussion
The main findings of this study were that as compared to patients < 65, those ≥ age 65 suffered anesthesia-related adverse events more commonly in the postoperative period and were more likely to die as a result of an adverse event. Additionally, approximately 40% of adverse events were preventable regardless of age.
Previous large database studies have shown that age independently predicts a composite of major adverse outcomes, length of stay, and mortality in the perioperative period.3,7,25,31-34One of the largest studies, a retrospective cohort study utilizing the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database from 2005-2008 included 165,600 patients and found that within the first 30 days following non-emergency general surgery, older adults had higher rates of surgical site infections, venous thromboembolism, cerebrovascular accident, myocardial infarction, kidney injury, urinary tract infection, pneumonia, prolonged mechanical ventilation, unplanned intubation, and return to the operating room.6 Furthermore, once a complication occurred, older patients were significantly less likely to survive the event (i.e. failure to rescue) relative to younger patients, especially in the cohort great than 80 years old. Though advances in surgical techniques and systems improvements have led to decreases in mortality for patients of all ages, older adults who suffer a postoperative complication have a much higher risk of mortality than younger patients across studies and failure to rescue has been identified as a key driver of the wide variability in mortality for older adults who suffer a complication across different institutions.8,9,33,35,36. This makes anticipating, preventing, and, importantly responding to complications particularly important in older adults.
Compared to previous studies, this study is unique in that we focused specifically on anesthesia-related adverse events. We found that among patients who suffered anesthesia-related adverse events, older patients had a decreased likelihood of returning to their baseline level of health, and after propensity matching for pre-existing co-morbidities and type of surgery, age remained an independent predictor of mortality as a result of the adverse event. Older adults have a lower functional reserve in all organ systems to varying degrees. This limited physiologic reserve may not be apparent at baseline, but may become evident during acute processes such as illness or surgery, and may in part explain the greater incidence of mortality as a result of an anesthesia-related adverse event in our study, as well as failure to rescue after perioperative complications in general.
The older patients in our unmatched dataset suffered more cardiac adverse events, likely explained by the burden of pre-existing co-morbidities in the older population as the propensity matched sample did not show a difference between groups in adverse event type. Cardiovascular adverse events were found to be the most common perioperative adverse event in older patients by a prior group of investigators.37 In another study, increasing age was independently associated with an increased risk of major adverse cardiovascular events (MACE) after non-cardiac surgery.38 Older patients have also been shown to have a higher risk of cardiac arrest compared to younger patients.33 and older age is associated with lower survival after perioperative cardiac arrest.39 In general, greater than 60% of in-hospital cardiac arrests may be avoidable, especially those that happen in non-critical care areas as it has been demonstrated that survival after cardiac arrest is improved if the arrest occurs in critical care areas.40 Given the greater number of cardiac arrests in older patients relative to other adverse events and that they occurred in the postoperative period, careful consideration should be given to the postoperative disposition of older patients with multiple co-morbidities and may warrant consideration for ICU admission relative to younger patients.
We expected that anesthesia-related adverse events would not be preventable in older patients, given their higher burden of co-morbidities and decreased functional reserve. Approximately 40% of anesthesia-related adverse events in this dataset were determined to be preventable, and this did not differ between older versus younger patients, suggesting that there is room for improvement in patient safety for all age groups.
Conclusions:
Our data suggests that there are significant differences in the timing and outcomes of anesthesia-related adverse events between older and younger patients, most notably that older patients have a higher likelihood of mortality as a result of suffering an anesthesia-related adverse event. Approximately 40% of anesthesia related adverse events were preventable in both older and younger patients, and future efforts should be made to reduce the incidence of these preventable events.
Supplementary Material
1). Study population Characteristics Stratified by Age
2).Adjusted Odds Ratios for Outcomes on Univariate Logistic Regression
3). Adjusted Odds Ratio for Outcomes via Multivariable Logistic Regression
4). Adjusted Odds Ratio for Outcomes via Multivariable Logistic Regression on Propensity Matched Subgroup, Alternate Age Stratifications
5). Adjusted Odds Ratio for Outcomes via Multivariable Logistic Regression on Propensity Matched Subgroup, Constrained by Age
A). A complete list of adverse events by type for each age group
B). Events by underlying cause, stratified by age
Implications:
Older patients may benefit from a longer period of heightened vigilance in the PACU and postoperative period, as this is the time period when they were most susceptible to anesthesia-related adverse events in our study. Further studies utilizing larger samples from multiple centers are needed to more precisely determine the significance of the differences seen here.
Acknowledgments
Conflicts of Interest and Source of Funding:
Mr. Root received funding for this project, which was provided by the National Institute on Aging and the American Federation for Aging Research through the Medical Student Training in Aging Research (MSTAR) Program.
Dr. McCormick’s research is supported by the National Cancer Institute of the National Institutes of Health under Award Number P30CA008748.
These entities had no role in the design of this study, the collection, interpretation or analysis of the data or the preparation of this manuscript. The remaining authors had no sources of funding or conflicts of interest to declare.
Biography
Christopher W. Root is a medical student at the Icahn School of Medicine at Mount Sinai, New York, NY. He is also a Paramedic in the department of Emergency Medical Services at New York Presbyterian Hospital, New York, NY.
Yaakov Beilin, MD is a Professor of Anesthesiology in the Departments of the Department of Anesthesiology, Pain, and Perioperative Medicine, and Obstetrics Gynecology and Reproductive Sciences at the Icahn School of Medicine at Mount Sinai, New York, NY; and Systems Vice Chair for Quality and Director of Obstetric Anesthesiology at the Mount Sinai Hospital, New York, NY
Patrick J. McCormick, MD, MEng, is an Assistant Attending in the Department of Anesthesiology & Critical Care Medicine at Memorial Sloan Kettering Cancer Center in New York, New York. He is also an Assistant Professor of Clinical Anesthesiology at Weill Cornell Medical College in New York, New York
Christopher J. Curatolo, MD, MEM, is an Interventional Pain Physician, Attending Anesthesiologist, and Clinical Informatics Physician of the Department of anesthesiology, Seacoast Pain Institute of New England, and The Center for Pain Management, Wentworth-Douglass Hospital, Dover, NH
Daniel Katz, MD is an Assistant Professor in the Department of Anesthesiology, Pain, and Perioperative Medicine at the Icahn School of Medicine at Mount Sinai, New York, NY
Jaime Hyman, MD is an Assistant Professor and Clinical Coordinator in the Department of Anesthesiology, Pain, and Perioperative Medicine at the Icahn School of Medicine at Mount Sinai, New York, NY
References
- 1.Levine WC, Mehta V, Landesberg G. Anesthesia for the elderly: selected topics. Curr Opin Anaesthesiol. 2006;19(3):320–324. doi: 10.1097/01.aco.0000192807.63785.59 [DOI] [PubMed] [Google Scholar]
- 2.Sieber F, Pauldine R. Geriatric Anesthesia In: Miller’s Anesthesia. 8th ed. Saunder’s; 2014:2407–2422. [Google Scholar]
- 3.Deiner S, Westlake B, Dutton RP. Patterns of Surgical Care and Complications in Elderly Adults. J Am Geriatr Soc. 62(5):829–835. doi: 10.1111/jgs.12794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.John A, Sieber FE. Age associated issues: geriatrics. Preoperative Eval. 2004;22(1):45–58. doi: 10.1016/S0889-8537(03)00119-6 [DOI] [PubMed] [Google Scholar]
- 5.Sieber FE, Barnett SR. Preventing Postoperative Complications in the Elderly. Qual Anesth Care. 2011;29(1):83–97. doi: 10.1016/j.anclin.2010.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gajdos C, Kile D, Hawn MT, Finlayson E, Henderson WG, Robinson TN. Advancing Age and 30-Day Adverse Outcomes After Nonemergent General Surgeries. J Am Geriatr Soc. 61(9):1608–1614. doi: 10.1111/jgs.12401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Massarweh NN, Kougias P, Wilson MA. Complications and Failure to Rescue After Inpatient Noncardiac Surgery in the Veterans Affairs Health System. JAMA Surg. 2016;151(12):1157–1165. doi: 10.1001/jamasurg.2016.2920 [DOI] [PubMed] [Google Scholar]
- 8.Sheetz KH, Krell RW, Englesbe MJ, Birkmeyer JD, Campbell DA, Ghaferi AA. The Importance of the First Complication: Understanding Failure to Rescue after Emergent Surgery in the Elderly. J Am Coll Surg. 2014;219(3):365–370. doi: 10.1016/j.jamcollsurg.2014.02.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sheetz KH, Guy K, Allison JH, et al. Improving the Care of Elderly Adults Undergoing Surgery in Michigan. J Am Geriatr Soc. 2014;62(2):352–357. doi: 10.1111/jgs.12643 [DOI] [PubMed] [Google Scholar]
- 10.Curatolo CJ, McCormick PJ, Hyman JB, Beilin Y. Preventable Anesthesia-Related Adverse Events at a Large Tertiary Care Center. Jt Comm J Qual Patient Saf. 2018;0(0). doi: 10.1016/j.jcjq.2018.03.013 [DOI] [PubMed] [Google Scholar]
- 11.Lagasse M Robert S, Steinberg M Ellen S, Katz M Robert I, Saubermann M Albert J. Defining Quality of Perioperative Care by Statistical Process Control of Adverse Outcomes. Anesthesiology. 1995;82(5):1181–1188. [DOI] [PubMed] [Google Scholar]
- 12.Anesthesia Incident Reporting System (AIRS). https://www.aqihq.org/AIRS/.
- 13.Al-Taki M, Sukkarieh HG, Hoballah JJ, et al. Effect of Gender on Postoperative Morbidity and Mortality Outcomes: A Retrospective Cohort Study. https://www.ingentaconnect.com/content/sesc/tas/2018/00000084/00000003/art00021%3bjsessionid=spdptz0svgk8.x-ic-live-03. Published March 2018. Accessed April 3, 2019. [PubMed]
- 14.Howell SJ, Sear JW, Foëx P. Hypertension, hypertensive heart disease and perioperative cardiac risk. Br J Anaesth. 2004;92(4):570–583. doi: 10.1093/bja/aeh091 [DOI] [PubMed] [Google Scholar]
- 15.Ri M, Aikou S, Seto Y. Obesity as a surgical risk factor. Ann Gastroenterol Surg. 2017;2(1):13–21. doi: 10.1002/ags3.12049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hopkins TJ, Raghunathan K, Barbeito A, et al. Associations between ASA Physical Status and postoperative mortality at 48 h: a contemporary dataset analysis compared to a historical cohort. Perioper Med. 2016;5(1):29. doi: 10.1186/s13741-016-0054-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leung V, Ragbir-Toolsie K. Perioperative Management of Patients with Diabetes. Health Serv Insights. 2017;10. doi: 10.1177/1178632917735075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hammill BG, Curtis LH, Bennett-Guerrero E, et al. Impact of Heart Failure on Patients Undergoing Major Noncardiac Surgery. Anesthesiol J Am Soc Anesthesiol. 2008;108(4):559–567. doi: 10.1097/ALN.0b013e31816725ef [DOI] [PubMed] [Google Scholar]
- 19.Melduni RM, Koshino Y, Shen W-K. Management of Arrhythmias in the Perioperative Setting. Clin Geriatr Med. 2012;28(4):729–743. doi: 10.1016/j.cger.2012.08.006 [DOI] [PubMed] [Google Scholar]
- 20.Samarendra P, Mangione MP. Aortic Stenosis and Perioperative Risk With Noncardiac Surgery. J Am Coll Cardiol. 2015;65(3):295–302. doi: 10.1016/j.jacc.2014.10.051 [DOI] [PubMed] [Google Scholar]
- 21.Chu D, Bakaeen FG, Wang XL, et al. The impact of peripheral vascular disease on long-term survival after coronary artery bypass graft surgery. Ann Thorac Surg. 2008;86(4):1175–1180. doi: 10.1016/j.athoracsur.2008.06.024 [DOI] [PubMed] [Google Scholar]
- 22.Jørgensen ME, Torp-Pedersen C, Gislason GH, et al. Time Elapsed After Ischemic Stroke and Risk of Adverse Cardiovascular Events and Mortality Following Elective Noncardiac Surgery. JAMA. 2014;312(3):269–277. doi: 10.1001/jama.2014.8165 [DOI] [PubMed] [Google Scholar]
- 23.Craig RG, Hunter JM. Recent developments in the perioperative management of adult patients with chronic kidney disease. BJA Br J Anaesth. 2008;101(3):296–310. doi: 10.1093/bja/aen203 [DOI] [PubMed] [Google Scholar]
- 24.Patel T Surgery in the Patient With Liver Disease. Mayo Clin Proc. 1999;74(6):593–599. doi: 10.4065/74.6.593 [DOI] [PubMed] [Google Scholar]
- 25.Manku K, Bacchetti P, M Leung J. Prognostic Significance of Postoperative In-Hospital Complications in Elderly Patients. I. Long-Term Survival. Anesth Analg. 2003;96:583–9, table of contents. doi: 10.1097/00000539-200302000-00051 [DOI] [PubMed] [Google Scholar]
- 26.Puvanesarajah V, Jain A, Shimer A, Shen F, Hassanzadeh H. The Effect of Coagulopathies on Perioperative Complications and Clinical Outcomes in Patients Treated With Posterior Lumbar Fusions. Spine. 2016;41(17). doi: 10.1097/BRS.0000000000001550 [DOI] [PubMed] [Google Scholar]
- 27.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 28.Posner KL, Kendall-Gallagher D, Wright IH, Glosten B, Gild WM, Cheney FW. Linking Process and Outcome of Care in a Continuous Quality Improvement Program for Anesthesia Services. Am J Med Qual. 1994;9(3):129–137. doi: 10.1177/0885713X9400900305 [DOI] [PubMed] [Google Scholar]
- 29.Posner KL, Freund PR. Resident Training Level and Quality of Anesthesia Care in a University Hospital. Anesth Analg. 2004;98(2). http://journals.lww.com/anesthesia-analgesia/Fulltext/2004/02000/Resident_Training_Level_and_Quality_of_Anesthesia.31.aspx. [DOI] [PubMed] [Google Scholar]
- 30.Wanderer JP, Gratch DM, Jacques PS, Rodriquez LI, Epstein RH. Trends in the Prevalence of Intraoperative Adverse Events at Two Academic Hospitals After Implementation of a Mandatory Reporting System. Anesth Analg. 2018;126(1):134. doi: 10.1213/ANE.0000000000002447 [DOI] [PubMed] [Google Scholar]
- 31.Li G, Warner M, Lang BH, Huang L, Sun LS. Epidemiology of Anesthesia-related Mortality in the United States, 1999–2005. Anesthesiology. 2009;110(4):759–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Turrentine FE, Wang H, Simpson VB, Jones RS. Surgical Risk Factors, Morbidity, and Mortality in Elderly Patients. J Am Coll Surg. 2006;203(6):865–877. doi: 10.1016/j.jamcollsurg.2006.08.026 [DOI] [PubMed] [Google Scholar]
- 33.Hamel MB, Henderson WG, Khuri SF, Daley J. Surgical Outcomes for Patients Aged 80 and Older: Morbidity and Mortality from Major Noncardiac Surgery. J Am Geriatr Soc. 53(3):424–429. doi: 10.1111/j.1532-5415.2005.53159.x [DOI] [PubMed] [Google Scholar]
- 34.Al-Refaie W, Parsons H, Habermann E, et al. Operative Outcomes Beyond 30-day Mortality. Ann Surg. 2011;253(5):947–952. doi: 10.1097/SLA.0b013e318216f56e [DOI] [PubMed] [Google Scholar]
- 35.Sheetz KH, Waits SA, Krell RW, Campbell DAJ, Englesbe MJ, Ghaferi AA. Improving Mortality Following Emergent Surgery in Older Patients Requires Focus on Complication Rescue. Ann Surg. 2013;258(4):614. doi: 10.1097/SLA.0b013e3182a5021d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in Hospital Mortality Associated with Inpatient Surgery. N Engl J Med. 2009;361(14):1368–1375. doi: 10.1056/NEJMsa0903048 [DOI] [PubMed] [Google Scholar]
- 37.Leung JM, Dzankic S. Relative Importance of Preoperative Health Status Versus Intraoperative Factors in Predicting Postoperative Adverse Outcomes in Geriatric Surgical Patients. J Am Geriatr Soc. 49(8):1080–1085. doi: 10.1046/j.1532-5415.2001.49212.x [DOI] [PubMed] [Google Scholar]
- 38.Hansen PW, Gislason GH, Jørgensen ME, et al. Influence of age on perioperative major adverse cardiovascular events and mortality risks in elective non-cardiac surgery. Eur J Intern Med. 2016;35:55–59. doi: 10.1016/j.ejim.2016.05.028 [DOI] [PubMed] [Google Scholar]
- 39.Kazaure HS, Roman SA, Rosenthal RA, Sosa JA. Cardiac Arrest Among Surgical Patients: An Analysis of Incidence, Patient Characteristics, and Outcomes in ACS-NSQIP. JAMA Surg. 2013;148(1):14–21. doi: 10.1001/jamasurg.2013.671 [DOI] [PubMed] [Google Scholar]
- 40.Hodgetts TJ, Kenward G, Vlackonikolis I, et al. Incidence, location and reasons for avoidable in-hospital cardiac arrest in a district general hospital. Resuscitation. 2002;54(2):115–123. doi: 10.1016/S0300-9572(02)00098-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1). Study population Characteristics Stratified by Age
2).Adjusted Odds Ratios for Outcomes on Univariate Logistic Regression
3). Adjusted Odds Ratio for Outcomes via Multivariable Logistic Regression
4). Adjusted Odds Ratio for Outcomes via Multivariable Logistic Regression on Propensity Matched Subgroup, Alternate Age Stratifications
5). Adjusted Odds Ratio for Outcomes via Multivariable Logistic Regression on Propensity Matched Subgroup, Constrained by Age
A). A complete list of adverse events by type for each age group
B). Events by underlying cause, stratified by age