Abstract
A triad of seminal vesical cyst, ipsilateral renal agenesis and ipsilateral ejaculatory duct obstruction is known as Zinner Syndrome. First described in 1914, only about 200 cases have been reported in literature. Usually it stays undiagnosed until the second to third decade of life due to lack of symptoms or nonspecific symptoms such as lower urinary tract symptoms, dysuria or painful ejaculation. In this report we present the case of a 22-year-old patient with a Zinner syndrome as an incidental finding and underlie a review of literature to show the main clinical and imaging implications.
Keywords: Zinner syndrome, Seminal vesical cyst, Mesonephric duct abnormality, Epididymitis, MRI
Introduction
As cysts of the seminal vesicles are very rare and often remain asymptomatic, they are usually diagnosed as incidental findings in imaging studies due to non-related symptoms or diseases. Especially in young patients seminal vesicle cysts are considered to be congenital since the causes of acquired cysts are very rare in this population. The association of congenital vesicle cysts with ipsilateral upper urinary tract anomalies is very rare with a reported prevalence of 0.005% [1].
Zinner syndrome, first described by A. Zinner in 1914, describes a triad of seminal vesicle cyst, ipsilateral renal agenesis and ipsilateral ejaculatory duct obstruction [2]. Most patients are not diagnosed until the second or third decade of life due to lack of symptoms, some show only nonspecific symptoms such as lower urinary tract symptoms (LUTS), urinary urgency, dysuria, painful ejaculation, and perineal discomfort [3].
Case report
A 22-year-old male patient was transferred to our emergency department with suspected pulmonary embolism by his general physician. For a week he has been complaining about increasing dyspnea, left thoracic pain and hemoptysis. Other symptoms such as fever or other pre-existing conditions were unknown. An external blood test showed an elevated D-dimer level. For further evaluation and treatment the patient was hospitalized, an ECG, a chest CT, an ultrasound of the abdomen and deep veins of the lower extremities and a thrombophilia screening were disposed.
The thoracic CT revealed extensive bilateral pulmonary embolism with accompanying pleural effusion on the left side and infarct pneumonia in the left lower lobe (Fig. 1) The deep vein sonography showed normal findings without evidence of deep vein thrombosis. Sonography of the abdomen revealed left renal agenesis as well as a cystic structure on the left side adjacent to the prostate with 1.3 cm in size (Fig. 2).
Fig. 1.
Contrast enhanced CT of the thorax demonstrating (A) bilateral pulmonary embolism with left pleural effusion and (B) infarct pneumonia in the left lower lobe.
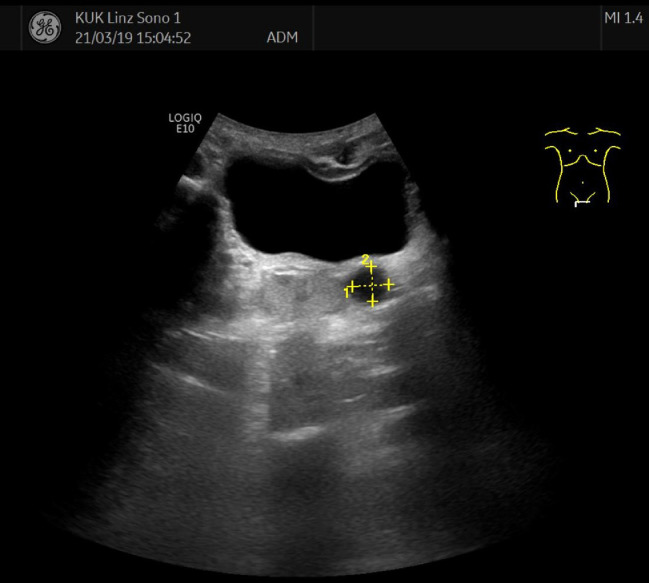
Fig. 2.
Sonography of the abdomen showing a cystic lesion, 1.3 cm in size, close to the bladder and the prostate additionally to left renal agenesis.
The thrombophilia screening revealed a mutation of the PAI 1 Gen, which is associated with a reduced fibrinolytic activity. A gastroscopy showed a mild gastritis and colonoscopy was performed to search for causes of the pulmonary embolism, which, however, remained inconspicuous. An ECG and echocardiography showed no pathological findings. Nevertheless he reported 1 episode of epididymitis but denied other lower-urinary-tract-symptoms such as dysuria, perineal or scrotal pain or painful ejaculation.
Contrast-enhanced MRI of the abdomen revealed renal agenesis on the left as well as a missing ipsilateral seminal vesicle (Fig. 3). Instead, however, several roundish-oval structures with a partly tubular configuration next to the bladder and the prostate appeared, correlating with the ultrasound examination, with a cranially pulling component without a visible connection to the surrounding structures. These showed no diffusion restriction, no contrast enhancement and were hyperintense in the T1 weighting and isointense in the T2 weighting compared to the muscle tissue. The ejaculatory duct was slightly dilated (Fig. 4).
Fig. 3.
(A) Axial T2-weighted images and (B) Coronal MR-angiography confirmed left renal agenesis.
Fig. 4.
(A) Axial T1-, (B) Axial T2-,(C) Sagittal T2-, and (D) Coronal post-contrast T1-weighted MR showing left renal agenesis (white star) and a missing ipsilateral seminal vesicle. Instead, however, several roundish-oval structures with a partly tubular configuration next to the bladder and the prostate were detected, correlating with the ultrasound examination, with a cranially pulling component without a visible connection to the surrounding structures (white arrows). These showed no contrast enhancement and were hyperintense in the T1 weighting and isointense in the T2 weighting compared to muscle tissue. The ipsilateral ejaculatory duct was slightly dilated.
Due to the lack of symptoms and the priority treatment regarding pulmonary embolism, the urology agreed on watchful waiting for the time being.
Discussion
First described by Zinner in 1914, the syndrome is a rare congenital malformation consisting with a triad of seminal vesicle cyst, ipsilateral renal agenesis and ejaculatory duct obstruction [2]. In literature just over 200 cases were described [4], but as imaging techniques advance, more cases are suspected to be diagnosed. Zinner syndrome is considered to be the male equivalent to the Mayer-Rokitansky-Kustner-Hauser female syndrome [5], [6], [7]. Usually presenting as the triad mentioned above it can additionally be associated with other urogenital findings such as ureterocele, hypospadias or abnormality of the testes, epididymis and adrenal glands [4,8]. In a mass screening study the reported incidence of cystic lesions in the pelvis with ipsilateral renal agenesis or dysplasia is reported to be between 0.00035% and 0.0046%. In accordance to several studies up to 68% of all seminal vesicle cysts are associated with ipsilateral renal agenesis [1,[9], [10], [11].
The link between renal agenesis and seminal vesicle cysts derives from the fact that both differentiate from the mesonephric duct, which is formed during the fourth week of gestation [6]. A defect in the induction of the ureteric bud from the metanephric blastema can lead to a defect in kidney formation. Due to a developmental abnormality of the distal part of Wolffian ducts male patients may develop an atresia of the ejaculatory duct leading to a collection of fluid in the seminal vesicle resulting in formation of cysts. If the ureteric bud originates distal to the urogenital sinus it can give rise to an ectopic ureter which can empty into the seminal vesicle cysts, the vas deferens, the ejaculatory duct or the bladder neck and urethra [3,5,9].
Patients with Zinner syndrome usually develop symptoms in the second to fourth decade relating to the period of highest sexual and reproductive activity, however, they can also remain asymptomatic [4,8]. Due to lack of symptoms or nonspecific signs it often remain undiagnosed or misinterpreted [10,12,13]. Especially if cysts are less than 5 cm in diameter they stay silent and are usually detected incidentally, as shown in our case. Reported giant cysts up to 12 cm in size may present with symptoms related to bladder compression and outlet obstruction triggering lower urinary tract infections [10,14]. In unlikely cases a malignant transformation of these cysts can occur [4,5,15]. In literature the most frequent symptoms include dysuria, abnormal urinary frequency, prostatitis, perineal or scrotal pain, epididymitis and painful ejaculation [5,9,16,17]. A very special case was shown by Pavan et al., where a large paratesticular mass mimicked a varicocele [18]. Great attention should be paid to association of Zinner syndrome with fertility. Due to ejaculatory duct obstruction, a low volume of semen, oligozoospermia and later azoospermia can cause infertility in up to 45% of cases [3], [4], [5], [6].
The differential diagnosis contain a wide spectrum of pelvic cystic lesions including mullerian duct or ejaculatory duct cysts (usually more midline in location and rarely associated with renal agenesis), prostatic cyst, ureterocele, bladder diverticuli, abscess, prostatic utricle cyst, hydronephrotic pelvic kidneys or regional cystic neoplasms [4,8,11,13,15]. Gartner's duct cyst can occur with ipsilateral renal agenesis, but is a remnant in female development of the mesonephric ducts [19]. Acquired seminal cysts are unusual in young patients, they rather appear in patients with chronic prostatitis or post prostatic surgery [5]. Each of the imaging findings shown in our case can be associated with other differential diagnoses, but the triad of renal agenesis, ipsilateral seminal vesical cyst and ispilateral ejaculatory duct obstruction together is pathognomonic for the Zinner syndrome [1,2,8]. A tumorous transformation of seminal vesical cysts seems to be very rare, in literature only a few cases of squamous cell carcinoma, adenocarcinoma, cystadenoma and benign mesenchymal tumor are described [20], [21], [22], [23].
Today's imaging techniques provide a wide spectrum of modalities to evaluate and differentiate pelvic masses. Usually transrectal or abdominal ultrasound are the first techniques to diagnose and evaluate pelvic masses, as shown in our case. Excretory urography can be used to show ipsilateral renal agenesis and an abnormal appearance of the collecting system. CT and MRI are definitely the most accurate imaging modalities to evaluate the genitourinary system and can provide the necessary information to confirm Zinner syndrome without further invasive investigations. In our case we used MRI to evaluate the initial findings on ultrasound. Seminal vesical cysts can be of variable signal, usually low on T1-weighted images and high on T2-images. Higher signal on T1-weighted images reflect hemorrhage or proteinaceous fluid [3,9,10,18].
A recently published study has also proposed a new strategy for the analysis of seminal vesicle lesions in the diagnosis and treatment of Zinner syndrome, which is based on the morphology of the cysts. The study looked at the size, contents, possible calcifications, the structure of the cyst wall and possible solid lesions in association with the cysts [8].
In asymptomatic or minimally symptomatic patient treatment is usually conservative, using for example antibiotics or transurethral aspiration of the seminal vesicle cyst. Invasive procedures are used in cases of cysts bigger than 5 cm, symptomatic cysts and patients who failed conservative treatment. This includes laparoscopic surgery and robotic techniques [3,9,14,24,25].
Conclusion
A combined seminal vesical cyst with ipsilateral upper urinary tract anomaly is a very rare condition. The Zinner Syndrome is consisting as a triad of unilateral renal agenesis, ipsilateral seminal vesicle cyst and ipsilateral ejaculatory duct obstruction and occurs exclusively in males. Our case meets these criteria and further demonstrates that the Zinner syndrome is usually diagnosed incidentally due to the lack of symptoms. Differential diagnosis such as ureterocele, prostatic utricle cysts, ejaculatory duct cysts or acquired seminal vesical cysts could be ruled out based on imaging findings and patient history. Our patient was hospitalized with a pulmonary embolism, which we assume has no association to the Zinner syndrome. Except for 1 episode of epididymitis, the patient reported no other lower urinary tract symptoms. If symptomatic, the patients may present unspecific urinary symptoms, ejaculatory difficulty and/or pain. Abdominal and transrectal ultrasound are useful, but only CT or MRI can accurately underlie the anatomy and help differentiate between Zinner syndrome and other malformations as mentioned above. Surgical treatment should only be considered for symptomatic patients, as follow-up studies should provide enough information in asymptomatic patients to contribute to its management.
Footnotes
Funding: No financial supports.
Competing Interests: All co-authors do not report conflicts of interest.
References
- 1.Sheih C.P., Hung C.S., Wei C.F., Lin C.Y. Cystic dilatations within the pelvis in patients with ipsilateral renal agenesis or dysplasia. J. Urol. 1990;144(2):324–327. doi: 10.1016/s0022-5347(17)39444-2. [DOI] [PubMed] [Google Scholar]
- 2.Zinner A. Ein Fall von Intravesikaler Samen blasen cyste. Wien Med Wochenschr. 1914;64:605–609. [Google Scholar]
- 3.Florim S., Oliveira V., Rocha D. Zinner syndrome presenting with intermittent scrotal pain in a young man. Radiol Case Rep. 2018;13(6):1224–1227. doi: 10.1016/j.radcr.2018.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pereira B.J. Zinner's syndrome: an up-to-date review of the literature based on a clinical case. Andrologia. Oct. 2009;41(5):322–330. doi: 10.1111/j.1439-0272.2009.00939.x. [DOI] [PubMed] [Google Scholar]
- 5.Kanavaki A., Vidal I., Merlini L., Hanquinet S. Congenital seminal vesicle cyst and ipsilateral renal agenesis (Zinner Syndrome): a rare association and its evolution from early childhood to adolescence. Eur J Pediatr Surg Reports. 2015;03(02):098–102. doi: 10.1055/s-0035-1555605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mehra S., Ranjan R., Garga U.C. Zinner syndrome—a rare developmental anomaly of the mesonephric duct diagnosed on magnetic resonance imaging. Radiol Case Rep. 2016;11(4):313–317. doi: 10.1016/j.radcr.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Symeonidis E.N. Incidental finding of Zinner syndrome in a Greek military recruit: a case report of a rare clinical entity. Mil. Med. Res. 2019;6(1):4. doi: 10.1186/s40779-019-0194-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tan Z., Li B., Zhang L., Han P., Huang H., Taylor A. Classifying seminal vesicle cysts in the diagnosis and treatment of Zinner syndrome : A report of six cases and review of available literature. Andrologia. 2019;June:1–10. doi: 10.1111/and.13397. [DOI] [PubMed] [Google Scholar]
- 9.Fiaschetti V., Greco L., Giuricin V., De Vivo D., Di Caprera E., Di Trapano R. Zinner syndrome diagnosed by magnetic resonance imaging and computed tomography: role of imaging to identify and evaluate the uncommon variation in development of the male genital tract. Radiol. Case Reports. 2017;12(1):54–58. doi: 10.1016/j.radcr.2016.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Slaoui A., Regragui S., Lasri A., Karmouni T., El Khader K., Koutani A. Zinner’s syndrome: report of two cases and review of the literature. Basic Clin Androl. 2016;26:10. doi: 10.1186/s12610-016-0037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farrelly J.S., Cleary M.A., Weiss R.M., Morotti R., Stitelman D.H. Acquired seminal vesicle cyst in a teenager with a urethral stricture of unknown etiology. J. Pediatr Surg Case Rep. 2016;7:8–12. [Google Scholar]
- 12.Campora M., Olivero A., Toncini C., Spina B., Fulcheri E., Terrone C. Zinner Syndrome: a diagnostic challenge. The aid of morphology, embryology, and immunohistochemistry. Urology. Oct. 2017;108:e3–e5. doi: 10.1016/j.urology.2017.06.013. [DOI] [PubMed] [Google Scholar]
- 13.Fiaschetti V., Greco L., Giuricin V., De Vivo D., Di Caprera E., Di Trapano R. Congenital Seminal Vesicle Cyst and Ipsilateral Renal Agenesis (Zinner Syndrome): A Rare Association and Its Evolution from Early Childhood to Adolescence. J. Pediatr Surg Case Rep. 2015;16(12):530–532. doi: 10.1055/s-0035-1555605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sundar R., Sundar G. Zinner syndrome: An uncommon cause of painful ejaculation. BMJ Case Rep. 2015:1–5. doi: 10.1136/bcr-2014-207618. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Livingston L., Larsen C.R. Original Report. AJR Am J Roentgenol. 2008;July:177–180. [Google Scholar]
- 16.Shah S., Patel R., Sinha R., Harris M. Zinner syndrome: an unusual cause of bladder outflow obstruction. BJR|case reports. 2016;3(2) doi: 10.1259/bjrcr.20160094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kao C.C., Wu C.J., Sun G.H., Yu D.S., Chen H.I., Chang S.Y. Congenital seminal vesicle cyst associated with ipsilateral renal agenesis mimicking bladder outlet obstruction: a case report and review of the literature. Kaohsiung J Med Sci. 2010;26(1):30–34. doi: 10.1016/S1607-551X(10)70005-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pavan N., Bucci S., Mazzon G., Bertolotto M., Trombetta C., Liguori G. It's not always varicocele: a strange case of Zinner syndrome. Can Urol Assoc J. 2015;9(7–8):535. doi: 10.5489/cuaj.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuo J., Foster C., Shelton D.K. Zinner's Syndrome. World J Nucl Med. Jan. 2011;10(1):20–22. doi: 10.4103/1450-1147.82115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim Y., Baek H.W., Choi E., Moon K.C. Squamous cell carcinoma of the seminal vesicle from Zinner syndrome: a case report and review of literature. J. Pathol Transl Med. 2015;49(1):85–88. doi: 10.4132/jptm.2014.10.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lorber G., Pizov G., Gofrit O.N., Pode D. Seminal vesicle cystadenoma: a rare clinical perspective. Eur Urol. Aug. 2011;60(2):388–391. doi: 10.1016/j.eururo.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 22.Okada Y., Tanaka H., Takeuchi H., Yoshida O. Papillary adenocarcinoma in a seminal vesicle cyst associated with ipsilateral renal agenesis: a case report. J. Urol. 1992;148(5):1543–1545. doi: 10.1016/s0022-5347(17)36964-1. [DOI] [PubMed] [Google Scholar]
- 23.Wang J., Yue X., Zhao R., Cheng B., Wazir R., Wang K. Primary squamous cell carcinoma of seminal vesicle: an extremely rare case report with literature review. Int Urol Nephrol. 2013;45(1):135–138. doi: 10.1007/s11255-012-0373-z. [DOI] [PubMed] [Google Scholar]
- 24.Chemaly A.K. Minimal invasive approach should become the standard for the management of Zinner Syndrome. Arch Cancer Res. 2015;3(4):2–4. [Google Scholar]
- 25.Jarzemski P., Listopadzki S., Kowalski M. Laparoscopic removal of a congenital seminal vesicle cyst in Zinner's syndrome. J Soc Laparoendosc Surg. 2014;18(2):367–371. doi: 10.4293/108680813X13753907291477. [DOI] [PMC free article] [PubMed] [Google Scholar]