Abstract
Bronchial artery aneurysm (BAA) is a rare vascular abnormality that may result in life-threatening bleeding if it is left untreated. We present the case of a 35-year-old man with a mediastinal BAA characterized by a short inflow artery segment and tortuous single outflow vessel. The patient's BAA was treated with a novel approach involving placement of a patent ductus arteriosus closure device in the short inflow segment as well as coil embolization of the outflow vessel, successfully excluding the BAA. Two-week follow-up revealed no flow in the embolized artery on computed tomography angiography. This case demonstrates the first successful use of a patent ductus arteriosus occluder device in the treatment of a mediastinal BAA with short inflow segment.
Keywords: Bronchial artery aneurysm, Patent ductus arteriosus occluder, Endovascular, Embolization
Bronchial artery aneurysm (BAA) is a rare pathologic process observed in <1% of all selective bronchial angiography studies; depending on location, it can be classified as mediastinal or intrapulmonary.1 Although the majority of patients with BAA are asymptomatic, rupture can result in massive hemoptysis or mediastinal hemorrhage, which can be life-threatening.2 BAAs are usually diagnosed as incidental findings on computed tomography (CT) and require definitive treatment to prevent the potential risk of fatal hemorrhage. Traditionally, surgery was the only option in these patients; however, as endovascular techniques have developed, minimally invasive methods have become the mainstay for treatment of BAA.1
We present a challenging mediastinal BAA case characterized by a short inflow artery segment and tortuous single outflow artery, successfully embolized using a novel endovascular approach with a patent ductus arteriosus (PDA) closure device and microcoils.
Written informed consent was obtained from the patient with regard to publication of this case.
Case report
A 35-year-old man was referred to Toronto General Hospital for treatment of BAA detected incidentally on CT during follow-up of cystic fibrosis. The aneurysm measured 20 × 25 mm in axial dimensions.
The patient's cystic fibrosis had previously been complicated by Pseudomonas infection, Mycobacterium abscesses, and pneumothorax. He denied any cardiovascular symptoms, including chest pain and palpitations. His breathing was normal, with limited phlegm production and no hemoptysis.
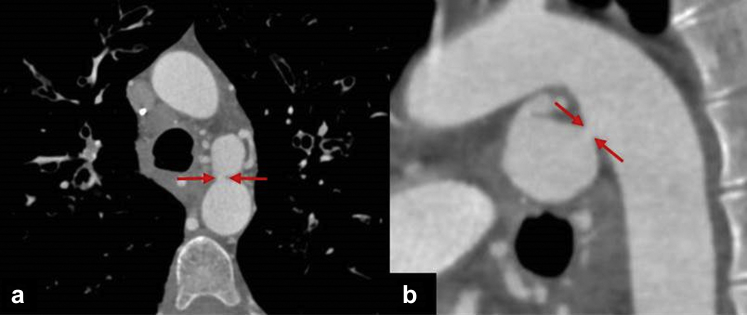
The BAA was technically challenging to treat because of a short inflow segment that spanned a length of approximately 1 mm beyond the origin of the left bronchial artery, arising from the proximal descending aorta (Fig 1). The single outflow vessel was also noted to be significantly tortuous.
Fig 1.
Axial (a) and sagittal (b) reconstructed images demonstrating large aneurysm located just beyond the origin of the left bronchial artery. The inflow segment is extremely short (arrows).
Access was gained through the right common femoral artery, and a 100-cm 7F sheath was introduced (Terumo, Shibuya, Japan). A 7F Vista Brite Tip guiding catheter (Cordis, Miami, Fla) was used to cannulate the origin of the left bronchial artery. Angiography showed brisk flow through the aneurysm sac located just beyond the origin of the left bronchial artery, with a short inflow segment and a dominant, tortuous single outflow vessel noted. There was no evidence of a bronchial artery to pulmonary artery fistula.
Initially, there was difficulty in cannulating the dominant outflow vessel as we were unable to determine the origin of the outflow ostium. The decision was made to use saline injection to propel 3-mm Tornado microcoils (Cook Medical, Bloomington, Ind), some of which lodged in the outflow tract and a few of which remained within the aneurysm sac. This served to provide an estimation of the outflow artery ostia and to approximate the distance the coils would travel if deployment was performed within the aneurysm sac. The outflow vessel was subsequently cannulated with moderate difficulty using a Transcend wire and a 2.4F Progreat microcatheter (Terumo) and embolized with a combination of 3- to 5-mm Tornado microcoils with good effect.
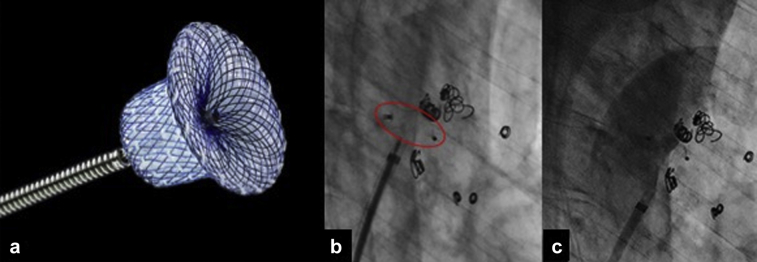
The wire was exchanged for a 1-cm floppy tip Amplatz wire (Boston Scientific, Marlborough, Mass) and the sheath upsized to 8F. An 8F Mach 1 guiding catheter (Boston Scientific) was inserted with the tip parked in the BAA. An 8-mm Amplatzer PDA occluder (product reference 9-PDA-005; St. Jude Medical, St. Paul, Minn) was placed across the neck and deployed in a satisfactory position (Fig 2, a and b).
Fig 2.
a, Illustrative image of Amplatzer patent ductus arteriosus (PDA) occluder device. (Courtesy St. Jude Medical, St. Paul, Minn. Product reference 9-PDA-005). Angiographic image (b) demonstrating Amplatzer PDA occluder spanning the inflow segment as well as coils within the outflow tract and within the aneurysm sac. Completion angiography through the long sheath (c) demonstrates no filling of the bronchial artery aneurysm (BAA).
Completion angiography demonstrated no filling of the BAA (Fig 2, c). Hemostasis was achieved with an 8F Angio-Seal vascular closure device (Terumo). Because of the patient's thin body habitus, a salinoma was created anterior to the right groin puncture site to accommodate the collagen plug of the Angio-Seal device.
No postprocedural complications were encountered, and the patient was discharged on the same day. Two weeks after BAA embolization, the patient denied any symptoms, and CT angiography evaluation revealed no opacification of the aneurysm, indicating successful treatment (Fig 3). A repeated CT study has been arranged for 6 months after intervention to assess for aneurysmal sac regression.
Fig 3.

Follow-up computed tomography (CT) performed 2 weeks after embolization shows the in situ plug (arrow), embolization coils, and successful exclusion of the bronchial artery aneurysm (BAA).
Discussion
BAA is an uncommon vascular phenomenon that often is manifested asymptomatically but can result in massive hemoptysis or mediastinal hemorrhage in the case of rupture. Given the multitude of underlying causes, including bronchiectasis, chronic bronchopulmonary inflammation, trauma, and infection, BAA may be detected incidentally on routine cross-sectional investigation of the lungs.3 Because of the potential risk of life-threatening hemorrhage, definitive surgical or endovascular treatment is indicated regardless of size.
Traditionally, treatment involved surgical resection or ligation from the midline or lateral thoracotomy.2 The endovascular approach has become favored, given the reduced postoperative morbidity and faster recovery time. New technologies are also pushing the boundaries of what can be achieved by minimally invasive methods. Studies have demonstrated that both surgical and endovascular options result in similar outcomes.4
Narrow-necked proximal BAAs, such as that exemplified in this case, are particularly challenging to treat. The use of conventional coils to embolize the inflow segment was deemed too risky, given the high risk of coil migration and subsequent nontarget embolization. Even the controlled use of detachable coils would have been impossible, given the approximately 1-mm length of the inflow segment. Several previous reports have described the use of thoracic stent grafts to exclude proximal mediastinal BAAs that originate close to the thoracic aorta.5,6 In a case described by Hu et al,7 the sac of the proximal BAA was initially embolized with gelatin sponge before the deployment of a thoracic stent graft, resulting in occlusion of both the inflow and outflow of the aneurysm. Although thoracic stent grafts are useful in emergent situations, for example, in cases of acute rupture with active bleeding, their use can lead to complications such as endoleak.
Jagia et al8 and Chadha et al9 have both described cases of short-necked pulmonary artery aneurysms successfully treated with PDA occlusion devices. With regard to the use of closure devices for PDAs, complications have been described in large studies with long-term follow-up; these studies have demonstrated that complications are exceedingly rare.10, 11, 12 Hemolytic anemia is the most commonly reported complication, occurring in approximately 1% of cases. There have been no reports of distal emboli in these studies.
Conclusions
This case report exemplifies the successful use of a PDA closure device for the treatment of ostial BAA, demonstrating it to be a viable treatment option in patients who would otherwise not be candidates for endovascular embolization because of adverse technical factors.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Tanaka K., Ihaya A., Horiuci T., Morioka K., Kimura T., Uesaka T. Giant mediastinal bronchial artery aneurysm mimicking benign esophageal tumor: a case report and review of 26 cases from literature. J Vasc Surg. 2003;38:1125–1129. doi: 10.1016/s0741-5214(03)00707-9. [DOI] [PubMed] [Google Scholar]
- 2.Misselt A.J., Krowka M.J., Misra S. Successful coil embolization of mediastinal bronchial artery aneurysm. J Vasc Interv Radiol. 2010;21:295–296. doi: 10.1016/j.jvir.2009.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iida Y., Saguchi T., Ikeda N., Ogino H. Bronchial artery aneurysm. J Vasc Surg. 2013;58:217. doi: 10.1016/j.jvs.2012.01.075. [DOI] [PubMed] [Google Scholar]
- 4.San Norberto E.M., Urbano García J., Montes J.M., Vaquero C. Endovascular treatment of bronchial aneurysms. J Thorac Cardiovasc Surg. 2018;156:e109–e117. doi: 10.1016/j.jtcvs.2017.12.121. [DOI] [PubMed] [Google Scholar]
- 5.Sanchez E., Alados P., Zurera L., Canis M., Muñoz I., Casares J. Bronchial artery aneurysm treated with aortic stent graft and fibrin sealant. Ann Thorac Surg. 2007;83:693–695. doi: 10.1016/j.athoracsur.2006.06.082. [DOI] [PubMed] [Google Scholar]
- 6.Matsumoto T., Uchida T., Ono T., Hirayama K., Fukumura F., Ando H. Bronchial artery aneurysm treated using aortic stent graft alone: a case report. Ann Vasc Dis. 2017;10:152–154. doi: 10.3400/avd.cr.16-00091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hu C., Huang S., Xu Z., Chen W., Huang J., Fu Z. Combination of aortic stent-graft and arterial embolization for ruptured bronchial artery aneurysm. Ann Thorac Surg. 2011;92:e19–e21. doi: 10.1016/j.athoracsur.2011.02.082. [DOI] [PubMed] [Google Scholar]
- 8.Jagia P., Sharma S., Juneja R., Guleria R. Transcatheter treatment of pulmonary artery pseudoaneurysm using PDA closure device. Diagn Interv Radiol. 2011;17:92–94. doi: 10.4261/1305-3825.DIR.2657-09.1. [DOI] [PubMed] [Google Scholar]
- 9.Chadha D., Handa A., Chandra S. Innovative endovascular technique for treatment of rare cause of haemoptysis in young. BMJ Case Rep. 2013:2013. doi: 10.1136/bcr-2012-008205. bcr2012008205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jang G.Y., Son C.S., Lee J.W., Lee J.Y., Kim S.J. Complications after transcatheter closure of patent ductus arteriosus. J Korean Med Sci. 2007;22:484. doi: 10.3346/jkms.2007.22.3.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi D.Y., Kim N.Y., Jung M.J., Kim S.H. The results of transcatheter occlusion of patent ductus arteriosus: success rate and complications over 12 years in a single center. Korean Circ J. 2010;40:230–234. doi: 10.4070/kcj.2010.40.5.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Behjati-Ardakani M., Rafiei M., Behjati-Ardakani M.A., Vafaeenasab M., Sarebanhassanabadi M. Long-term results of transcatheter closure of patent ductus arteriosus in adolescents and adults with Amplatzer duct occluder. N Am J Med Sci. 2015;7:208–211. doi: 10.4103/1947-2714.157478. [DOI] [PMC free article] [PubMed] [Google Scholar]