Abstract
Complicated type B aortic dissection (TBAD) is a life-threatening condition requiring surgical intervention. One such complication in the acute or chronic setting is aneurysmal degeneration. The dissected aortic wall is weakened, and the pressures in the false lumen are often high. In the past decade, thoracic endovascular aortic repair (TEVAR) has become the treatment of choice for TBAD. TEVAR can be complicated by lack of false lumen thrombosis, increasing the risk of death. We present three cases of TBAD with patent false lumens after TEVAR that were treated by false lumen coil embolization.
Keywords: TEVAR, False lumen, Aortic dissection, Coil embolization, Endovascular, Dissecting aortic aneurysm
Uncomplicated type B aortic dissection (TBAD) is managed by medical therapy focused on reducing heart rate and blood pressure.1,2 Uncontrolled hypertension, unrelenting pain, organ malperfusion, rupture, and shock or aneurysmal degeneration complicate TBAD in 25% to 40% of patients. Complicated TBAD (cTBAD) requires urgent surgical management to prevent malperfusion and potential rupture.1, 2, 3 Without progression to surgical treatment, cTBAD has a 33% 30-day mortality rate.3 During the past decade, there has been a trend toward endovascular intervention over open surgery in cTBAD patients.3 Recent studies indicate that thoracic endovascular aortic repair (TEVAR) has superior long-term survival to open thoracic aortic repair.4
Despite this trend toward endovascular repair, use of an endograft may not provide adequate thrombosis of the false lumen. The patent false lumen remains pressurized and can lead to further degeneration of aortic wall, leading to aneurysmal formation and rupture.5,6 As many as 15% to 30% of patients undergoing TEVAR require reintervention.6, 7, 8 Approximately 20% of these patients require reintervention because of false lumen perfusion and increasing aortic growth and degeneration.6,9,10 Lack of false lumen thrombosis and aortic remodeling after TEVAR can increase late mortality.11, 12, 13 Interventions leading to thrombosis of the false lumen can reduce mortality.11
Previous techniques for false lumen thrombosis include the candy-plug and knickerbocker techniques. The candy-plug technique deploys a modified covered stent graft into the false lumen, followed by an Amplatzer vascular plug (Abbott, St. Paul, Minn) at the waist to occlude flow.14, 15, 16 However, this graft can lead to true lumen narrowing or stent-induced wall injury.14,15,17 The knickerbocker technique involves inflation of a balloon inside of an oversized stent graft, causing a controlled rupture of the dissection flap and occluding false lumen flow.18 This technique is used more often to occlude distal false lumen flow and is less applicable in patients with proximal perfusion.18
We report three cases of TBAD complicated by aneurysmal degeneration of the aortic wall repaired by TEVAR followed by false lumen embolization. Consent from each patient was obtained for publication of these cases.
Case reports
Case 1
A 46-year-old man with uncontrolled hypertension presented with a complex acute type B dissection as well as a 6-cm thoracic aortic aneurysm and a 4.7-cm abdominal aortic aneurysm. Two false lumens were identified. The celiac artery was perfused through the false lumen, whereas the superior mesenteric artery was perfused through the true lumen. The abdominal aorta measured 4.2 × 4.4 cm at the distal seal zone, with a true lumen diameter of 2.1 × 2.6 cm (Fig 1, A). Despite initial treatment with medical therapy, back and chest pain persisted. The patient was a Jehovah's witness who declined blood products, so open surgical repair was not feasible. TEVAR was performed on hospital day 10 with a 40- × 270-mm Zenith Alpha thoracic endograft proximally, a 42- × 225-mm Zenith Alpha thoracic endograft bridge, and a 46- × 233-mm Zenith Alpha thoracic endograft distally (Cook Medical, Bloomington, Ind). A left carotid-subclavian bypass was performed at the time of TEVAR to land the graft in zone 2. After TEVAR, back and chest pain did not remit. Computed tomography (CT) angiography showed persistent retrograde filling of the false lumen (Fig 1, B). The candy-plug technique was possible, but to occlude the backflow, multiple plugs had to be placed, and some may have floated into the large false lumen. The graft placed during the index case was the largest graft, so the knickerbocker technique would not be possible in this case. On hospital day 24 (postoperative day 14), the false lumen was subsequently embolized with one 10-mm × 20-cm and three 15-mm × 40-cm Interlock Coils (Boston Scientific, Marlborough, Mass) at the base of the false lumen (Fig 2). In this case, the coils found their way into the area that was feeding retrograde into the false lumen and managed to thrombose it. The postoperative course was uncomplicated, and the patient was discharged on postoperative day 22/8. At 1-year after embolization, follow-up CT angiography showed that the false lumen remained thrombosed (Fig 3). Furthermore, there was remodeling of the aorta with a decrease in thoracic aortic diameter to 5.2 cm. The infrarenal segment distal to the endograft remodeled as well, measuring 4.3 cm, and the patient remains symptom free.
Fig 1.
A, Computed tomography (CT) angiography showing a complex type B aortic dissection, with two false lumens and one true lumen. The superior mesenteric artery (SMA) is shown with perfusion through the true lumen. The celiac artery (CA) was perfused through the false lumen. The patient also had an abdominal aortic aneurysm (AAA) measuring up to 4.7 cm. B, Status post thoracic endovascular aortic repair (TEVAR) with persistent filling of the false lumen. The SMA maintained true lumen perfusion; the CA is still perfused through the false lumen.
Fig 2.
A, Persistent retrograde flow into the false lumen. B, Status post embolization, no flow seen.
Fig 3.
A, One-year status post thoracic endovascular aortic repair (TEVAR) and coil embolization and false lumen thrombosis. B, No flow is seen in the false lumen (arrow). Coil artifact can be seen.
Case 2
A 70-year-old man with human immunodeficiency virus infection receiving highly active antiretroviral therapy (rilpivirine, emtricitabine, and tenofovir [Complera]; CD4 cell count, 672; viral load <20), Coccidioides meningitis complicated by hydrocephalus requiring shunt placement, pulmonary cryptococcosis, and type A aortic dissection status post repair with aortic valve replacement 17 years earlier presented with altered mental status and was admitted to the intensive care unit. The initial dissection was repaired with a Dacron graft and the aortic valve was replaced with a mechanical valve. During workup of altered mental status, CT demonstrated an 8.7-cm aortic pseudoaneurysm in the descending aortic arch and a type B aortic dissection distal to the left subclavian artery (Fig 4). Given the size of the thoracic aorta, we elected to perform TEVAR once he was medically stable. During this period, he developed lower extremity deep venous thromboses requiring inferior vena cava filter placement to allow warfarin to be held. On hospital day 12, a 28- × 201-mm Zenith Alpha thoracic endograft was placed into zone 2 with successful sealing of the pseudoaneurysm proximally (Fig 5, A and B). This failed to thrombose the false lumen, so we embolized the false lumen with seven 20-mm × 40-cm Interlock coils during the same procedure (Fig 5, C and D). Although either of the two previously described techniques could have been used here, we decided to use coil embolization. Anticoagulation was resumed 48 hours after TEVAR and embolization to prevent prosthetic aortic valve thrombosis. He also required a percutaneous endoscopic gastrostomy tube on postoperative day 10 for dysphagia. He was discharged to rehabilitation on postoperative day 29. At 1-month follow up, the patient denied further symptoms, and the pseudoaneurysm had thrombosed (Fig 6). Six months later, the patient died of complications from human immunodeficiency virus-related infection.
Fig 4.
Computed tomography (CT) angiography showing 8.7-cm dissecting aortic pseudoaneurysm and dissection. The partially thrombosed false lumen can be seen.
Fig 5.
A, Arch aortogram showing pseudoaneurysm distal to the left subclavian artery (LSA). B, Status post thoracic endovascular aortic repair (TEVAR), LSA flow was maintained. C, Status post TEVAR, large pseudoaneurysm remained. D, Status post false lumen embolization, decreased flow in false lumen and pseudoaneurysm.
Fig 6.
One-month status post thoracic endovascular aortic repair (TEVAR) and false lumen coil embolization. Thrombosis within the false lumen has increased.
Case 3
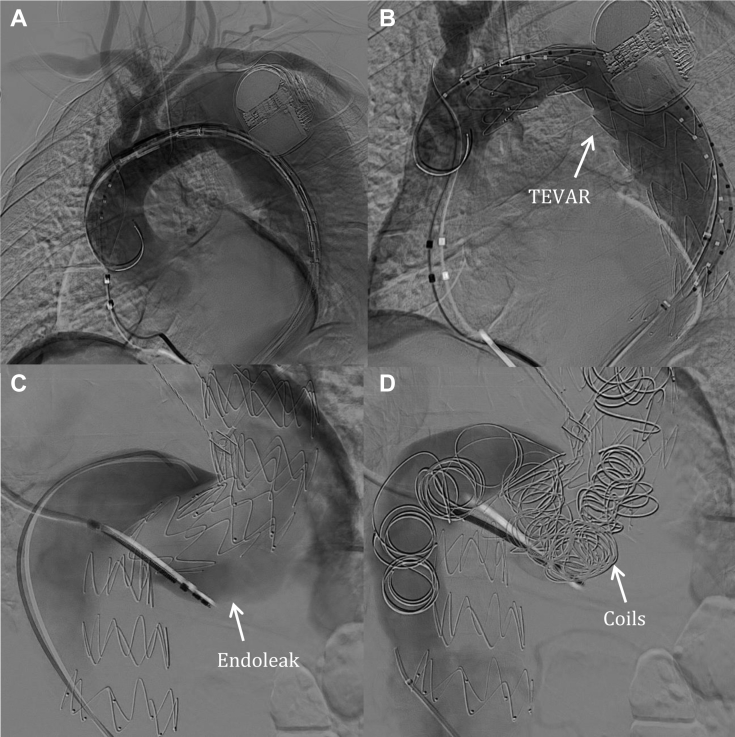
A 61-year-old man with congestive heart failure with an ejection fraction of 10% status post automated implantable cardioverter-defibrillator, diverticulitis, and chronic type B dissection secondary to hypertension from cocaine abuse 6 years before this admission presented with unrelenting chest pain. A CT scan demonstrated growth of his known dissecting type B aneurysm to 7.5 cm, with a 3.4- × 0.6-cm true lumen diameter (Fig 7). He was admitted, and TEVAR was performed with 38- × 217-mm and 46- × 233-mm Zenith Alpha thoracic endografts (Fig 8, A and B). There was successful sealing of the proximal zone, but the distal landing site did not provide adequate seal, and there was retrograde flow into the false lumen (Fig 8, C). On postoperative day 7, the false lumen was embolized with 2 15-mm × 40-cm, 3 20-mm × 40-cm, and 5 18-mm × 40-cm Interlock coils as well as twelve 20-mm Nestor coils (Cook Medical; Fig 8, D). In this case, the knickerbocker technique again could not be used because the total lumen diameter was too large. The candy-plug technique was also not used because the area of retrograde flow was large and coils would easily find the space where retrograde flow was present and would help seal and thrombose the flow. Pneumonia developed postoperatively, but the patient was discharged home on postoperative day 10/3. Symptoms of chest pain resolved after this, and repeated CT scan demonstrated thrombosis of the false lumen in the chest (Fig 9). The patient was seen 1-month postoperatively with no evidence of chest pain.
Fig 7.
Computed tomography (CT) angiography showing a 7.5-cm dissecting aortic aneurysm with large false lumen.
Fig 8.
A, Arch aortogram showing dissecting aortic aneurysm. B, Status post thoracic endovascular aortic repair (TEVAR). C, Status post TEVAR, type IB endoleak remained. D, Status post coil embolization, no flow seen into the false lumen.
Fig 9.
One-month status post thoracic endovascular aortic repair (TEVAR) and coil embolization, no flow seen into false lumen.
Discussion
The introduction of TEVAR revolutionized the treatment of TBAD with aneurysmal degeneration, but false lumen patency remains a problem and often requires reintervention to prevent late aortic rupture and death.6, 7, 8 Dongze and Cao13 reported a hazard ratio of 2.79 in TEVAR treatment of TBAD with residual false lumen patency. Patent false lumens confer a fivefold increased risk of any aortic event compared with thrombosed false lumens.13 Akutsu et al12 showed false lumen patency to be an independent risk factor for mortality after TEVAR. Coil embolization of the false lumen encourages thrombosis, thereby reducing mortality and rates of aortic events.
The technique used here involves placing the endograft in the true lumen. This requires adequate seal at the proximal landing zone. We ensured true lumen cannulation with the use of transesophageal ultrasound, intravascular ultrasound, and aortography. In the three cases described here, the distal aorta was aneurysmal. There was a lack of seal zone, and retrograde flow continued to fill the false lumen into the chest. The false lumen was then cannulated through a known fenestration previously reviewed on CT scan. The false lumen was subsequently embolized with coils. Large coils were used, and these were packed with smaller coils. When possible, coils were placed at the narrowest area (usually at the tortuosity right above the diaphragm) to seal retrograde flow and to thrombose the flow to the thoracic portion false lumen in the dissection.
Norberto et al19 and Pellenc et al20 showed that thrombosis of the false lumen after TEVAR for TBAD promotes aortic remodeling. Watanabe et al21 showed that aortic remodeling after TEVAR decreases the risk of aortic adverse events. By promoting aortic remodeling and decreasing aneurysm size, false lumen embolization could decrease the risk of aortic rupture and mortality after TEVAR.11, 12, 13
Both the candy-plug and knickerbocker techniques have been used to encourage false lumen thrombosis after TEVAR.14,15,17,18 Coil embolization of the false lumen has been used as another method of encouraging thrombosis, but fewer than 100 cases have been reported in the literature.16,19,20 In patients with a larger false lumen relative to total aortic diameter, coil embolization may be preferred to the knickerbocker technique. Coils placed into the false lumen could provide less potential for stent graft injury than overexpanding a graft into a large false lumen.17,18 Coil embolization also provides an advantage over the candy-plug technique in patients with narrower true lumens. The candy-plug has the potential to narrow the true lumen, whereas coil embolization is more able to conform to the false lumen.14,15 False lumen coil embolization provides an option for false lumen thrombosis in patients with more challenging anatomy.
False lumen coil embolization appears to be a safe procedure, with none of our patients experiencing coil-related complications. Spanos et al16 also suggested that false lumen embolization is a safe procedure in cTBAD, with a 0% 30-day mortality and a 7.1% late mortality. However, no study to date has commented on spinal cord ischemia in false lumen embolization. Increasing the percentage of thoracic aorta covered by stent grafts has been shown to increase spinal cord ischemia, but it is unclear whether this is due to false lumen thrombosis or coverage of lumbar vessels.22 Kim et al23 described 25 patients who underwent false lumen procedures without spinal cord ischemia. However, 2.4% of patients developed paraplegia in their 2018 analysis.24 It is unclear what impact on spinal cord ischemia could result from using a shorter stent graft combined with false lumen embolization.
There has been ongoing debate about resumption of anticoagulation after TEVAR. De Rango et al25 demonstrated increased rates of endoleak and reintervention with anticoagulation. However, Song et al26 and Öztürk et al27 found that early resumption of anticoagulation has no impact on long-term mortality after type A dissection repair, raising questions as to the necessity of holding anticoagulation for false lumen thrombosis in TEVAR for TBAD. Coil embolization of the false lumen would encourage thrombosis while allowing anticoagulation to be resumed more expediently after TEVAR.
A limitation of these case reports is the length of follow-up for patients in Case 2 and Case 3. The patient in Case 2 died of his extensive medical comorbidities unrelated to TBAD, and long-term follow-up was not possible. The patient in Case 3 is doing well, but follow-up is limited because of how recently embolization occurred. In addition, our case reports are a small sample and not a randomized controlled trial. More investigation should be done to determine the long-term outcomes of patients undergoing false lumen embolization in conjunction with TEVAR.
Conclusions
False lumen patency is a complication after TEVAR in some patients with dissecting aortic aneurysm. False lumen coil embolization should be considered when applicable in TBAD repair to reduce the risk of false lumen patency, aneurysm rupture, and mortality in the short to moderate term. Longer follow-up is needed to determine efficacy and safety over time.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Nauta F.J., Trimarchi S., Kamman A.V., Moll F.L., van Herwaarden J.A., Patel H.J. Update in the management of type B aortic dissection. Vasc Med. 2016;21:251–263. doi: 10.1177/1358863X16642318. [DOI] [PubMed] [Google Scholar]
- 2.Qin Y.L., Deng G., Li T.X., Wang W., Teng G.J. Treatment of acute type-B aortic dissection: thoracic endovascular aortic repair or medical management alone? JACC Cardiovasc Interv. 2013;6:185–191. doi: 10.1016/j.jcin.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 3.Sumpio B.J., Cordova A.D., Mahler D., Sumpio B.E. Use of negative pressure wound therapy in healing below knee amputation in patients with chronic venous insufficiency and/or Charcot disease. Angiology Open Access. 2013;1:1000112. [Google Scholar]
- 4.Chiu P., Goldstone A.B., Schaffer J.M., Lingala B., Miller D.C., Mitchell R.S. Endovascular versus open repair of intact descending thoracic aortic aneurysms. J Am Coll Cardiol. 2019;73:643–651. doi: 10.1016/j.jacc.2018.10.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruddy J.M., Reisenman P., Priestley J., Brewster L.P., Duwayri Y., Veeraswamy R.K. Stent graft therapy for false lumen aneurysmal degeneration in established type B aortic dissection (FADED) results in differential volumetric remodeling of the thoracic versus abdominal aortic segments. Ann Vasc Surg. 2014;28:1602–1609. doi: 10.1016/j.avsg.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 6.Zhang L., Zhao Z., Chen Y., Sun Y., Bao J., Jing Z. Reintervention after endovascular repair for aortic dissection: a systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2016;152:1279–1288.e3. doi: 10.1016/j.jtcvs.2016.06.027. [DOI] [PubMed] [Google Scholar]
- 7.Lou X., Chen E.P., Duwayri Y.M., Veeraswamy R.K., Jordan W.D., Jr., Zehner C.A. The impact of thoracic endovascular aortic repair on long-term survival in type B aortic dissection. Ann Thorac Surg. 2018;105:31–38. doi: 10.1016/j.athoracsur.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 8.Garbade J., Jenniches M., Borger M.A., Barten M.J., Scheinert D., Gutberlet M. Outcome of patients suffering from acute type B aortic dissection: a retrospective single-centre analysis of 135 consecutive patients. Eur J Cardiothorac Surg. 2010;38:285–292. doi: 10.1016/j.ejcts.2010.02.038. [DOI] [PubMed] [Google Scholar]
- 9.Hanna J.M., Andersen N.D., Ganapathi A.M., McCann R.L., Hughes G.C. Five-year results for endovascular repair of acute complicated type B aortic dissection. J Vasc Surg. 2014;59:96–106. doi: 10.1016/j.jvs.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Leshnower B.G., Duwayri Y.M., Chen E.P., Li C., Zehner C.A., Binongo J.N. Aortic remodeling after endovascular repair of complicated acute type B aortic dissection. Ann Thorac Surg. 2017;103:1878–1885. doi: 10.1016/j.athoracsur.2016.09.057. [DOI] [PubMed] [Google Scholar]
- 11.Evangelista A., Salas A., Ribera A., Ferreira-Gonzalez I., Cuellar H., Pineda V. Long-term outcome of aortic dissection with patent false lumen: predictive role of entry tear size and location. Circulation. 2012;125:3133–3141. doi: 10.1161/CIRCULATIONAHA.111.090266. [DOI] [PubMed] [Google Scholar]
- 12.Akutsu K., Nejima J., Kiuchi K., Sasaki K., Ochi M., Tanaka K. Effects of the patent false lumen on the long-term outcome of type B acute aortic dissection. Eur J Cardiothorac Surg. 2004;26:359–366. doi: 10.1016/j.ejcts.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 13.Dongze L., Cao Y. GW27-e0166 False lumen status in patients with acute aortic dissection: a systematic review and meta-analysis. J Am Coll Cardiol. 2016;68(Suppl):C123. doi: 10.1161/JAHA.115.003172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kolbel T., Lohrenz C., Kieback A., Diener H., Debus E.S., Larena-Avellaneda A. Distal false lumen occlusion in aortic dissection with a homemade extra-large vascular plug: the candy-plug technique. J Endovasc Ther. 2013;20:484–489. doi: 10.1583/13-4318.1. [DOI] [PubMed] [Google Scholar]
- 15.Ogawa Y., Nishimaki H., Chiba K., Murakami K., Sakurai Y., Fujiwara K. Candy-plug technique using an excluder aortic extender for distal occlusion of a large false lumen aneurysm in chronic aortic dissection. J Endovasc Ther. 2016;23:483–486. doi: 10.1177/1526602816640523. [DOI] [PubMed] [Google Scholar]
- 16.Spanos K., Kolbel T., Rohlffs F., Heidemann F., Giannoukas A.D., Debus S.E. Intentional targeted false lumen occlusion after aortic dissection: a systematic review of the literature. Ann Vasc Surg. 2019;56:317–329. doi: 10.1016/j.avsg.2018.08.086. [DOI] [PubMed] [Google Scholar]
- 17.Furukawa T., Uchida N., Yamane Y., Yamada K. A pitfall of false lumen embolization in chronic aortic dissection: intimal injury caused by the embolization device edge. Interact Cardiovasc Thorac Surg. 2017;24:153–155. doi: 10.1093/icvts/ivw279. [DOI] [PubMed] [Google Scholar]
- 18.Kolbel T., Carpenter S.W., Lohrenz C., Tsilimparis N., Larena-Avellaneda A., Debus E.S. Addressing persistent false lumen flow in chronic aortic dissection: the knickerbocker technique. J Endovasc Ther. 2014;21:117–122. doi: 10.1583/13-4463MR-R.1. [DOI] [PubMed] [Google Scholar]
- 19.Norberto E.M., Gutierrez V.M., Taylor J., Vaquero C. Coil embolization of persistent false lumen after stent graft repair of type B aortic dissection. J Vasc Surg. 2011;54:201–204. doi: 10.1016/j.jvs.2010.11.110. [DOI] [PubMed] [Google Scholar]
- 20.Pellenc Q., Roussel A., De Blic R., Girault A., Cerceau P., Ben Abdallah I. False lumen embolization in chronic aortic dissection promotes thoracic aortic remodeling at midterm follow-up. J Vasc Surg. 2019;70:710–717. doi: 10.1016/j.jvs.2018.11.038. [DOI] [PubMed] [Google Scholar]
- 21.Watanabe Y., Shimamura K., Yoshida T., Daimon T., Shirakawa Y., Torikai K. Aortic remodeling as a prognostic factor for late aortic events after thoracic endovascular aortic repair in type B aortic dissection with patent false lumen. J Endovasc Ther. 2014;21:517–525. doi: 10.1583/13-4646R.1. [DOI] [PubMed] [Google Scholar]
- 22.Bisdas T., Panuccio G., Sugimoto M., Torsello G., Austermann M. Risk factors for spinal cord ischemia after endovascular repair of thoracoabdominal aortic aneurysms. J Vasc Surg. 2015;61:1408–1416. doi: 10.1016/j.jvs.2015.01.044. [DOI] [PubMed] [Google Scholar]
- 23.Kim T.H., Song S.W., Lee K.H., Baek M.Y., Yoo K.J. Effects of false lumen procedures on aorta remodeling of chronic DeBakey IIIb aneurysm. Ann Thorac Surg. 2016;102:1941–1947. doi: 10.1016/j.athoracsur.2016.05.036. [DOI] [PubMed] [Google Scholar]
- 24.Kim T.H., Song S.W., Lee K.H., Baek M.Y., Yoo K.J., Cho B.K. The effect of false lumen procedures during thoracic endovascular aortic repair in patients with chronic DeBakey type IIIB dissections. J Vasc Surg. 2018;68:976–984. doi: 10.1016/j.jvs.2018.01.045. [DOI] [PubMed] [Google Scholar]
- 25.De Rango P., Verzini F., Parlani G., Cieri E., Simonte G., Farchioni L. Safety of chronic anticoagulation therapy after endovascular abdominal aneurysm repair (EVAR) Eur J Vasc Endovasc Surg. 2014;47:296–303. doi: 10.1016/j.ejvs.2013.12.009. [DOI] [PubMed] [Google Scholar]
- 26.Song S.W., Yoo K.J., Kim D.K., Cho B.K., Yi G., Chang B.C. Effects of early anticoagulation on the degree of thrombosis after repair of acute DeBakey type I aortic dissection. Ann Thorac Surg. 2011;92:1367–1374. doi: 10.1016/j.athoracsur.2011.04.111. discussion: 1374-5. [DOI] [PubMed] [Google Scholar]
- 27.Öztürk P., Apaydın A.Z., Karakuş E., Kılıç A.Ö., Özbaran M. The impact of oral anticoagulation on false lumen patency in acute type A aortic dissections. J Turk Thorac Cardiovasc Surg. 2018;26:345–350. doi: 10.5606/tgkdc.dergisi.2018.15013. [DOI] [PMC free article] [PubMed] [Google Scholar]