Highlights
-
•
Overall treatment time for HNC treatment was reduced according to DAHANCA guidelines.
-
•
Sufficient accelerator capacity alone did not sufficiently minimize treatment time.
-
•
Surveillance of treatment calendars reduced breaches to 3% (6fx/wk) and 13% (5 fx/wk).
-
•
Radiobiological efficacy was increased by 1.3 Gy (6 fx/wk) and 2.0 Gy (5 fx/wk).
-
•
Surveillance of treatment calendars presented minimal financial costs.
Keywords: Head and neck cancer, Radiotherapy, Overall treatment time, Radiobiology, Workflow management, Health economics
Abstract
Background and purpose
Overall treatment time (OTT) is essential for local tumour control and survival in radiotherapy of head and neck cancer (HNC). National radiotherapy guidelines of the Danish Head and Neck Cancer Group (DAHANCA) recommend a maximum OTT of 41 days for moderately accelerated radiation treatment (6 fractions/week) and 48 days for conventional treatment (5 fractions/week). The purpose of this study was to evaluate the effect of surveillance of the radiotherapy course length and treatment gaps in HNC patients to reduce OTT.
Methods
The study included 2011 patients with HNC undergoing radical radiation treatment with 66–68 Gy in 33–34 fractions in 2003–2017 at Odense University Hospital. In February 2016, a systematic weekly review by two radiation therapists of all planned treatment courses was introduced to check OTT of individual patients to portend likely breaks or treatment prolongations. Schedules that violated the OTT guidelines were conferred with the responsible radiation oncologist, and treatment rescheduled by treating twice daily to catch up with a delay.
Results
The mean length of accelerated treatment courses was reduced from a maximum of 40.9 days in 2007 to 38.3 days in 2017 and from 50.3 days to 45.9 days for conventional courses. The percentage of individual treatment courses that violated the recommended OTT was reduced to 3% of the accelerated treatments and 13% for the conventional treatments.
Conclusion
Continuous surveillance of treatment schedules of HNC patients by a brief weekly survey reduced treatment course duration to an extent that was radiobiologically and clinically meaningful.
Introduction
Randomized clinical trials in head and neck cancer (HNC) have demonstrated a detrimental effect on tumour control and overall survival from prolongation of overall treatment time (OTT) during radiotherapy [1], [2], [3]. Such findings have been supported by further clinical studies [4], [5], [6], [7], and it has been estimated that one missed treatment day may decrease the absolute local control probability by 1.4% for carcinoma of the larynx [8] and 3.3% for nasopharyngeal tumours [9]. Correspondingly, Withers et al [10] and others [11] showed that a dose increment of about 0.6 Gy is required to compensate for tumour cell proliferation in head and neck cancer patients per day the OTT is prolonged. Recently, prolongation of OTT as a cause of treatment failure has also been demonstrated in breast [12], [13] and prostate cancer [14]. Thus, precautions must be taken in daily clinical practice to avoid prolongation of radiation treatment time.
Various practical measures have been used and recommended to compensate for missed treatment days in head and neck radiotherapy [15], [16]. In 2002, national radiotherapy guidelines for HNC from the Danish Head and Neck Cancer Group (DAHANCA) has thus recommended that compensation for missing fractions should be given as quickly as possible, and ideally within a week, if clinically applicable, by delivering an additional fraction during weekends or two fractions in one day, six hours apart. A quality assurance standard from DAHANCA of the OTT has also been set at 41 days for moderately accelerated radiation treatment (6 fractions/week) and 48 days for conventional treatment (5 fractions/week) [17], [18]. The IMRT update of the DAHANCA guidelines in 2004 further specified that no more than 13 fractions should be delivered over two weeks and that large treatment breaks required a change of the fractionation schedule [19]. An overview of treatment regimens specified by DAHANCA and followed in our department is given in Table 1.
Table 1.
Overview of DAHANCA treatment regimens used from 2002 to 2017.
| Conventional 2.0 Gy per fraction |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CTV1 |
CTV2 |
CTV3 |
OTT threshold | ||||||||||
| Total dose | # frac | dose/frac | frac/week | Total dose | # frac | dose/frac | frac/week | Total dose | # frac | dose/frac | days | ||
| Conventional fractionation | 66 | 33 | 2 | 5 | 46 | 23 | 2 | 5 | 48 | ||||
| 68 | 34 | 2 | 5 | 46 | 23 | 2 | 5 | 48 | |||||
| 66 | 33 | 2 | 5 | 48 | 24 | 2 | 5 | 48 | |||||
| 68 | 34 | 2 | 5 | 48 | 24 | 2 | 5 | 48 | |||||
| Moderately accelerated | 66 | 33 | 2 | 6 | 46 | 23 | 2 | 6 | 41 | ||||
| 68 | 34 | 2 | 6 | 46 | 23 | 2 | 6 | 41 | |||||
| 66 | 33 | 2 | 6 | 48 | 24 | 2 | 6 | 41 | |||||
| 68 | 34 | 2 | 6 | 48 | 24 | 2 | 6 | 41 | |||||
| Accelerated hyperfractionated | 76 | 56 | 1.36 | 10 | 44.5 | 33 | 1.35 | 10 | 41 | ||||
| Simultaneous-integrated boost | |||||||||||||
| Conventional fractionation | 66 | 33 | 2 | 5 | 60 | 33 | 1.82 | 5 | 50 | 33 | 1.52 | 5 | 48 |
| 68 | 34 | 2 | 5 | 60 | 34 | 1.76 | 5 | 50 | 34 | 1.47 | 5 | 48 | |
| Moderately accelerated | 66 | 33 | 2 | 6 | 60 | 33 | 1.82 | 6 | 50 | 33 | 1.52 | 6 | 41 |
| 68 | 34 | 2 | 6 | 60 | 34 | 1.76 | 6 | 50 | 34 | 1.47 | 6 | 41 | |
| Accelerated hyperfractionated | 76 | 56 | 1.36 | 10 | 66 | 56 | 1.18 | 10 | 56 | 56 | 1 | 10 | 41 |
In 2013, guidelines recommend to minimize treatment time by never starting a treatment course on a Friday or finish on a Monday. Furthermore, moderately accelerated patients should receive at least 3 fractions before the first weekend break. OTT exceeding 41 calendar days for moderately accelerated patients or 48 days for normal fractionation patients is defined as a minor protocol deviation. A major protocol deviation is reported if OTT exceeds 46 calendar days for moderately accelerated patients or 53 days for normal fractionation patients [17], [18].
Hence, the importance of minimizing OTT is well documented. However, due to a variety of reasons such as acute toxicity, co-morbidity, family events, social issues, machine breakdown etc. [19], [20], it is inevitable that treatments are missed on specific occasions. The purpose of this study was to assess whether OTT of radiation treatment during a 15-year period in our institution was in adherence with the national DAHANCA guidelines and to propose weekly surveillance of individual radiotherapy treatment calendars as a means to reduce breaches of OTT.
Material and methods
Patients and treatment technique
This study included all 2011 curatively treated head and neck cancer patients in our clinic in the period 2003–2017. Data were extracted retrospectively from the departments’ record and verification system database, Mosaiq (Elekta AB, Stockholm, Sweden). All patients were treated according to the DAHANCA guidelines version 2002, 2004 or 2013 [17], [19] shown in Table 1. Prior to 2007, conformal 3D technique was used to deliver conventional 2 Gy fractions. From 2007 onwards, simultaneous-integrated boost (SIB) was used for intensity modulated radiotherapy (IMRT) and volumetric-modulated arc therapy (VMAT). The DAHANCA guidelines interpret the prescription dose as the mean dose to the CTV with coverage by 95% of the prescription dose to 99% of the CTV volume, in accordance with ICRU recommendations.
Deviations in OTT, as specified in the 2013 DAHANCA guidelines, were evaluated for each patient. Thereby, it was possible to disentangle the effect of awareness and surveillance of OTT introduced in 2016 from the effects of increased linear accelerator (linac) capacity in 2007 and changed scheduling of QA procedures from 2013.
The accelerated (total 1220) and non-accelerated (total 791) patients were divided into four groups according to temporal milestones: Group A was treated prior to 2007 when the department experienced a shortage of linacs, Group B belongs to the era of increased linac capacity (2007–2012), Group C was treated in the era of the 2013 DAHANCA guidelines (2013–2015) with increased focus on OTT, and Group D (2016–2017) was treated in the era of awareness and weekly surveillance of OTT.
Surveillance of treatment calendars
In February 2016, an active surveillance of all HNC treatment schedule deviations was introduced in our department. Two radiation therapists (RTT) alternated in performing a weekly survey of patients in the Mosaiq system by running a customized report for each patient undergoing treatment. In case of deviations from guidelines, the RTTs would adjust the patient’s treatment schedule with one day of double-fractionation per week, following written instructions from DAHANCA [17], [18] that no more than 13 fractions should be delivered over two weeks. Larger treatment breaks owing to acute toxicity, hospitalization, machine breakdown or patient requests, requiring a further change of the fractionation schedule were discussed with the radiation oncologist.
Statistics
The differences in OTT between the four groups were tested with one-way ANOVA and the test of equality of variance was tested with the Leven’s test. Differences in mean between pairs of groups were tested with Students t-test. Differences in the frequency of deviations were tested with a Kruskal-Wallis test, and the 68% confidence interval (CI) was calculated as the exact binomial test. The significance level was set at 0.05.
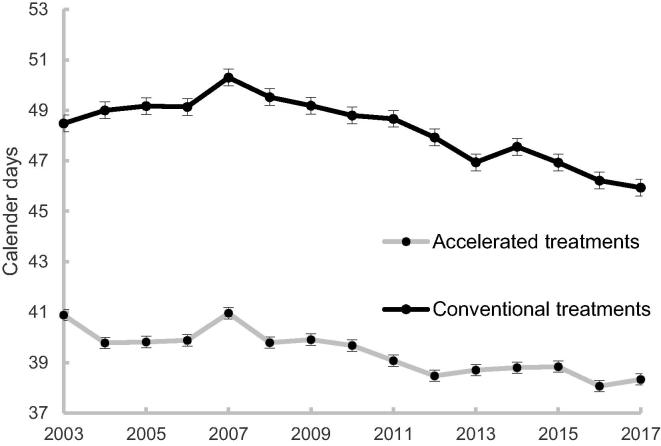
Results
The largest OTT was observed in 2007 for both accelerated and conventional head and neck treatments. The mean OTT for accelerated treatment was 40.3 days ± 0.1 (std. error), 39.4 ± 0.1, 38.8 ± 0.1 and 38.2 ± 0.1 in group A, B, C and D, respectively. The differences in OTT were highly significant (p < 0.001) between all groups (one-way ANOVA) and between any pairs of groups. The mean length of accelerated treatment courses was reduced from 40.9 days in 2007 to 38.8 days in 2015, and to 38.3 days in 2017 (Fig. 1).
Fig. 1.
Average overall treatment time. Mean OTT of accelerated and conventional fractionated treatments per year. Whiskers indicate standard errors.
For conventional treatment courses, the mean OTT was 49.3 days ± 0.2 (std. error), 48.8 ± 0.1, 47.1 ± 0.2 and 46.1 ± 0.2 for group A, B, C and D, respectively. The difference is highly significant (p < 0.001) for all groups (one-way ANOVA) as well as when comparing groups in pairs (A vs B p = 0.05, B vs C p < 0.001 and C vs D p < 0.001). The mean OTT was reduced from 50.3 days in 2007 to 46.9 days in 2015, and to 45.9 days in 2017 (Fig. 1).
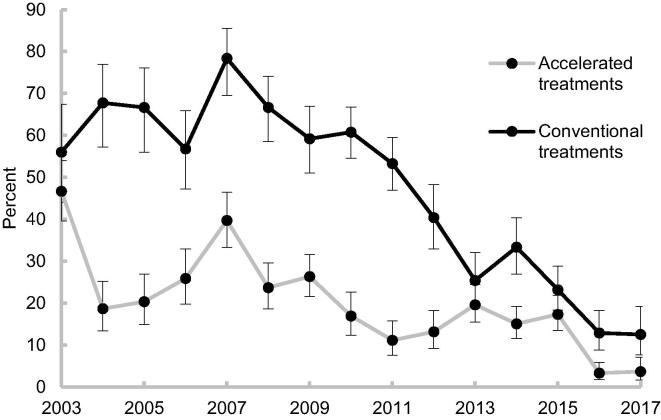
The frequency of minor protocol deviations was significantly reduced over time except between group B and C for accelerated patients. Minor protocol deviations were reduced from 31% in group A to 3% in group D for accelerated patients and from 66% in group A to 13% in group D for conventional patients (Table 2). Major protocol deviations were observed in 3 and 27 cases for accelerated and non-accelerated patients, respectively. For the non-accelerated patients the majority of these major deviations were observed in 2007–2009.
Table 2.
Frequency of protocol deviations per group are given for conventional and accelerated treatment regimes. Resulting p-values of Kruskal-Wallis test between the groups are given as well as 95% CI for each group.
| Conventional |
Accelerated |
|||||
|---|---|---|---|---|---|---|
| Group | Threshold deviations | 95% CI | p-value | Threshold deviations | 95% CI | p-value |
| A [<2007] | 66% | 58–73% | 0.046 | 31% | 25–36% | <0.001 |
| B [2007–2012] | 56% | 50–62% | <0.001 | 19% | 15–23% | 0.64 |
| C [2013–2015] | 27% | 21–33% | 0.003 | 17% | 13–22% | <0.001 |
| D [2015–2017] | 13% | 7–20% | 3% | 1.4–7% | ||
After the introduction of the systematic RTT review of treatment schedule, the fraction of treatment course time violations was further reduced to 3% for accelerated treatments, and to 13% for the conventional treatments (Fig. 2). No major deviations were observed after initiation of the systematic review.
Fig. 2.
Fraction of protocol deviations. Fraction of patients for whom OTT violated national guidelines per year. Whiskers indicate 68% confidence interval, corresponding to 1 standard deviation.
The surveillance procedure took in total 5–15 min for an RTT to perform per week for all patients on treatment. It was possible to compensate most violations defined by the national guidelines, but for the last 3% (conventional regime) and 13% (accelerated regime), OTT was prolonged, mainly due to clinical decisions by the treating oncologist.
Discussion
OTT is an important factor for loco-regional tumour control and survival after radiotherapy. In this study, we demonstrated that OTT can be effectively reduced with a minimal effort of awareness and surveillance of the treating staff of the radiation treatment unit. An increase in OTT was observed in this study from 2003 to 2007, likely due to an increased demand for RT in general and a general lack of linacs and staff, a problem that was described in the Danish National Cancer Plan I. In 2007, the national cancer plan funding had resulted in an increased number of treatment machines and associated staffing. At the same time awareness of the importance of minimizing OTT rose and consequently, the frequency of fraction protocol deviations, and thus OTT, decreased from 2008. It is obvious that in order to compensate for missed fractions or treatment interruptions, appropriate treatment time slots must be available. Thus, linac capacity plays an important role in ensuring OTT guideline compliance.
In 2011, the revision of the DAHANCA radiotherapy guidelines sparked an external audit of treatment protocols, including DAHANCA10, which showed that protocol deviations in OTT varied between centres [19]. This led to increased awareness of OTT, resulting in a further decrease in fraction protocol deviations and OTT. This was achieved by scheduling department service and QA to outside clinical hours to allocate more treatment slots during day-time. It was furthermore requested that head and neck patients were moved to another treatment machine in case of emergency break down to avoid treatment gaps and theoretically minimizing the risk of repopulation during treatment.
Increased treatment capacity by obtaining more linacs and employing more staff is expensive, but necessary to reduce OTT. Although the treatment capacity became sufficient over the years, a survey initiated after a DAHANCA QA audit in 2015 revealed a surprisingly high fraction of patients not adhering to the OTT guideline without any apparent reason. Investigation of individual patient treatment schedules in our department showed that the guideline threshold of 41 and 48 days was always secured initially in our booking system. Yet, upon completion of their radiation treatment course, up to 20% of patients still had OTT protocol deviations due to rescheduling or unexpected missed fractions. These deviations were almost eliminated through our weekly surveillance by RTTs. The strategy to perform a weekly surveillance described in this study demonstrated efficiency at a very limited cost to reduce OTT in a large cohort of patients; surveillance of the individual patient schedules required only a total of 5–15 min of RTT time per week.
The clinical benefit of the RTT surveillance strategy may be determined from a radiobiological point of view. Approximately 0.6 Gy is lost per day that OTT is increased due to tumour cell proliferation, negatively affecting the probability of tumour control as concluded from reviews by Gonzales Ferreira et al. [20] and Bese et al. [21]. Local control rate would decrease by approximately 10% per month in a typical series of patients with carcinoma of the tonsillar region, dependent on tumour doubling time [4], as described by Bentzen et al. [11] in carcinoma of the oropharynx. Reducing OTT for accelerated treatments by 2.2 days from 2007 to 2015 meant that a mean loss of 1.3 Gy in radiobiological treatment efficacy was eliminated for the cohort. Correspondingly, a mean loss of 2.0 Gy in radiobiological efficacy was eliminated for conventional treatments in the same period without increasing late toxicity probability as mean OTT was shortened by 3.4 days.
Time from diagnosis to initiation of radiation treatment also plays an important role for survival in head and neck cancer [22]. Modern treatment planning for HNC includes imaging of multiple modalities such as PET/CT and MRI, often performed in different departments of the hospital. In treatment planning, imaging is followed by delineation of organs at risk and target structures, dose planning and plan verification; a process where the patients plan changes hands several times. To minimize time wasted in the pre-treatment phase, all steps and their time components in this process should be optimized for the full treatment to be as effective as possible. Thus, fast track programs have been initiated, where time from suspicion of head and neck cancer to initiation of primary radical treatment has been reduced considerably [23], [24]. Over the time period investigated in this study, the treatment planning time between CT and the first fraction has decreased from up to 10 calendar days to a maximum 7 calendar days presently, i.e. a patient CT scanned on a Monday will receive the first treatment fraction the following Monday.
This study has demonstrated that by investing in linacs and staff to secure sufficient availability of treatment slots in a radiotherapy department, it was possible to decrease OTT. However, this did not in itself ensure that HNC patients were treated as rapidly as possible; awareness and surveillance of patients treatment schedules added further significant reductions in OTT. Based on the literature, other indications, such as breast and prostate cancer, are likely to benefit from surveillance of radiation treatment schedules as well.
Conclusion
Awareness and weekly surveillance of individual head and neck radiotherapy schedules significantly reduced the OTT, which was considered radiobiologically and clinically meaningful, by recognizing possible causes that may have led to treatment gaps. The effort comprised a minimal financial burden to the department. Therefore, guidelines for maximum overall treatment time should be complemented by local procedures to eliminate treatment delays.
Conflict of interest
The authors have no conflicts of interest to declare.
Acknowledgements
This work has been supported financially by: Danish Cancer Society grant, University of Southern Denmark scholarship, Odense University Hospital scholarship and Danish Cancer Research Fund.
References
- 1.Overgaard J., Alsner J., Eriksen J., Horsman M.R., Grau C. Importance of overall treatment time for the response to radiotherapy in patients with squamous cell carcinoma of the head and neck. Rays. 2000;25:313–319. [PubMed] [Google Scholar]
- 2.Lee A.W., Sze W.M., Yau T.K., Yeung R.M., Chappell R., Fowler J.F. Retrospective analysis on treating nasopharyngeal carcinoma with accelerated fractionation (6 fractions per week) in comparison with conventional fractionation (5 fractions per week): report on 3-year tumor control and normal tissue toxicity. Radiother Oncol. 2001;58:121–130. doi: 10.1016/s0167-8140(00)00312-1. [DOI] [PubMed] [Google Scholar]
- 3.Marcu L.G. Altered fractionation in radiotherapy: from radiobiological rationale to therapeutic gain. Cancer Treat Rev. 2010;36:606–614. doi: 10.1016/j.ctrv.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Mackillop W.J. Killing time: the consequences of delays in radiotherapy. Radiother Oncol. 2007;84:1–4. doi: 10.1016/j.radonc.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 5.Overgaard J., Hjelm-Hansen M., Johansen L.V., Andersen A.P. Comparison of conventional and split-course radiotherapy as primary treatment in carcinoma of the larynx. Acta Oncol. 1988;27:147–152. doi: 10.3109/02841868809090334. [DOI] [PubMed] [Google Scholar]
- 6.Shaikh T., Handorf E.A., Murphy C.T., Mehra R., Ridge J.A., Galloway T.J. The impact of radiation treatment time on survival in patients with head and neck cancer. Int J Radiat Oncol Biol Phys. 2016;96:967–975. doi: 10.1016/j.ijrobp.2016.08.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wyatt R.M., Jones B.J., Dale R.G. Radiotherapy treatment delays and their influence on tumour control achieved by various fractionation schedules. Br J Radiol. 2008;81:549–563. doi: 10.1259/bjr/94471640. [DOI] [PubMed] [Google Scholar]
- 8.Barton M.B., Keane T.J., Gadalla T., Maki E. The effect of treatment time and treatment interruption on tumour control following radical radiotherapy of laryngeal cancer. Radiother Oncol. 1992;23:137–143. doi: 10.1016/0167-8140(92)90323-m. [DOI] [PubMed] [Google Scholar]
- 9.Kwong D.L., Sham J.S., Chua D.T., Choy D.T., Au G.K., Wu P.M. The effect of interruptions and prolonged treatment time in radiotherapy for nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 1997;39:703–710. doi: 10.1016/s0360-3016(97)00339-8. [DOI] [PubMed] [Google Scholar]
- 10.Withers H.R., Taylor J.M., Maciejewski B. The hazard of accelerated tumor clonogen repopulation during radiotherapy. Acta Oncol. 1988;27:131–146. doi: 10.3109/02841868809090333. [DOI] [PubMed] [Google Scholar]
- 11.Bentzen S.M., Johansen L.V., Overgaard J., Thames H.D. Clinical radiobiology of squamous cell carcinoma of the oropharynx. Int J Radiat Oncol Biol Phys. 1991;20:1197–1206. doi: 10.1016/0360-3016(91)90228-v. [DOI] [PubMed] [Google Scholar]
- 12.Haviland J.S., Bentzen S.M., Bliss J.M., Yarnold J.R., Group S.T.M. Prolongation of overall treatment time as a cause of treatment failure in early breast cancer: an analysis of the UK START (Standardisation of Breast Radiotherapy) trials of radiotherapy fractionation. Radiother Oncol. 2016;121:420–423. doi: 10.1016/j.radonc.2016.08.027. [DOI] [PubMed] [Google Scholar]
- 13.Gupta S., King W.D., Korzeniowski M., Wallace D.L., Mackillop W.J. The effect of waiting times for postoperative radiotherapy on outcomes for women receiving partial mastectomy for breast cancer: a systematic review and meta-analysis. Clin Oncol (R Coll Radiol) 2016;28:739–749. doi: 10.1016/j.clon.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 14.Thames H.D., Kuban D., Levy L.B., Horwitz E.M., Kupelian P., Martinez A. The role of overall treatment time in the outcome of radiotherapy of prostate cancer: an analysis of biochemical failure in 4839 men treated between 1987 and 1995. Radiother Oncol. 2010;96:6–12. doi: 10.1016/j.radonc.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 15.Hendry J.H., Bentzen S.M., Dale R.G., Fowler J.F., Wheldon T.E., Jones B. A modelled comparison of the effects of using different ways to compensate for missed treatment days in radiotherapy. Clin Oncol (R Coll Radiol) 1996;8:297–307. doi: 10.1016/s0936-6555(05)80715-0. [DOI] [PubMed] [Google Scholar]
- 16.Dale R.G., Hendry J.H., Jones B., Robertson A.G., Deehan C., Sinclair J.A. Practical methods for compensating for missed treatment days in radiotherapy, with particular reference to head and neck schedules. Clin Oncol (R Coll Radiol) 2002;14:382–393. doi: 10.1053/clon.2002.0111. [DOI] [PubMed] [Google Scholar]
- 17.Hansen C.R., Johansen J., Samsoe E., Andersen E., Petersen J.B.B., Jensen K. Consequences of introducing geometric GTV to CTV margin expansion in DAHANCA contouring guidelines for head and neck radiotherapy. Radiother Oncol. 2018;126:43–47. doi: 10.1016/j.radonc.2017.09.019. [DOI] [PubMed] [Google Scholar]
- 18.Danish head and neck cancer group. DAHANCA Radiotherapy Guidelines 2013. 2nd ed. 30-01-2015. <https://www.dahanca.oncology.dk/assets/files/GUID_DAHANCA%20Radiotherapy%20Guidelines.pdf>. [Accessed Dec 21, 2018].
- 19.Hansen C.R., Johansen J., Kristensen C.A., Smulders B., Andersen L.J., Samsoe E. Quality assurance of radiation therapy for head and neck cancer patients treated in DAHANCA 10 randomized trial. Acta Oncol. 2015;54:1669–1673. doi: 10.3109/0284186X.2015.1063780. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez Ferreira J.A., Jaen Olasolo J., Azinovic I., Jeremic B. Effect of radiotherapy delay in overall treatment time on local control and survival in head and neck cancer: review of the literature. Rep Pract Oncol Radiother. 2015;20:328–339. doi: 10.1016/j.rpor.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bese N.S., Hendry J., Jeremic B. Effects of prolongation of overall treatment time due to unplanned interruptions during radiotherapy of different tumor sites and practical methods for compensation. Int J Radiat Oncol Biol Phys. 2007;68:654–661. doi: 10.1016/j.ijrobp.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 22.Murphy C.T., Galloway T.J., Handorf E.A., Egleston B.L., Wang L.S., Mehra R. Survival impact of increasing time to treatment initiation for patients with head and neck cancer in the United States. J Clin Oncol. 2016;34:169–178. doi: 10.1200/JCO.2015.61.5906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lyhne N.M., Christensen A., Alanin M.C., Bruun M.T., Jung T.H., Bruhn M.A. Waiting times for diagnosis and treatment of head and neck cancer in Denmark in 2010 compared to 1992 and 2002. Eur J Cancer. 2013;49:1627–1633. doi: 10.1016/j.ejca.2012.11.034. [DOI] [PubMed] [Google Scholar]
- 24.Roennegaard A.B., Rosenberg T., Bjorndal K., Sorensen J.A., Johansen J., Godballe C. The Danish Head and Neck Cancer fast-track program: a tertiary cancer centre experience. Eur J Cancer. 2018;90:133–139. doi: 10.1016/j.ejca.2017.10.038. [DOI] [PubMed] [Google Scholar]