Highlights
-
•
Our study suggests that intra-fractional bladder filling does not affect the delivery of adaptive bladder radiotherapy.
-
•
Current use of the adaptive bladder treatment planning margins and decision making for all plan selections sufficed.
-
•
This study addressed its aims and its findings are supported by other national and international studies.
Keywords: Adaptive bladder radiotherapy, Intra-fractional bladder filling, Plan of the day selection
Abstract
A retrospective audit on the “Plan of the day” (POD) selection and intra-fractional bladder fillings were carried out on twenty adaptive bladder radiotherapy patients at a single institution. Treatment time, differences in bladder volume and displacement of outer bladder wall expansion over the treatment fraction were analysed. Average treatment time was 8.9 min. The mean percentage difference in bladder volume pre and post treatment was 13.7%, resulting in expansion of the bladder predominately in the superior and anterior directions. This audit confirmed that the institution’s POD process sufficed without being significantly affected by the intra-fractional bladder filings.
Introduction
Radiotherapy provides a radical treatment approach for many bladder cancer patients either unsuitable for surgery, chemotherapy or undergoing a multimodality management [1], [2]. The unpredictable variations in bladder volume due to intra- and inter-fractional filling during treatment have been evidently documented in bladder radiotherapy [2]. Large treatment planning margins are often used to ensure coverage and minimise geographical miss, however this also led to unnecessary irradiation vast areas of normal tissue [2], [3].
Bladder cancer is the second most common urological cancer [4]. In order to strike a balance between local control and long-term toxicity for the bladder cancer patients, it is essential that the bladder target volume is covered adequately by high radiation dose whilst sparing the surrounding healthy tissue as much as possible [3]. This facilitated the development of adaptive techniques in bladder radiotherapy. Several adaptive strategies were available with the aim to irradiate bladder cancer accurately while minimising radiation to the surrounding organs at risk [5], [6], [7]. One of the commonest adaptive methods in bladder radiotherapy is ‘Plan of the Day’ (POD) plan selection from a plan library [5], [8], [9]. The POD approach utilises volumetric image guidance with cone-beam computed tomography (CBCT) to select the most appropriate prepared plan for that patient on a daily basis [3].
The effect of intra-fractional bladder filling has been investigated and it suggested that intra-fractional bladder filling motion could result in three-dimensional directional variations [10], [11], [12]. The bladder motion can be deemed to be unpredictable and can increase significantly between pre and post-treatment, thus intra-fractional filling must be carefully assessed [11].
Against this background, this study aimed to assess whether the current departmental treatment planning expansion margins and POD treatment options were appropriately applied; and the impact of intra-fractional bladder filling on adaptive bladder radiotherapy.
Methods & materials
Twenty patients with transitional cell carcinoma of the bladder (T2/3N0M0) were treated with adaptive bladder radiotherapy from January 2015 to December 2015 at a single institution.
The patients received verbal advice on bladder preparation at their CT planning appointments. The advice was to stop drinking one hour prior to planning CT. Patients were asked to void their bladders, wait ten minutes, and then to void for a second time before proceeding with the planning scan. This process would then be repeated daily prior to each treatment.
All patients were planned and treated supine utilising an in-house made knee and footrest immobilisation device. Once the bladder clinical target volumes were outlined the following planning margins defined in Table 1 were used to create three different sized plans. A 3-field conformal technique was used with all patients receiving 55 Gy in twenty fractions over four weeks. Daily online CBCTs were used to analyse the size of the bladder and select the most appropriate POD treatment for that daily treatment from a library of three different sized plans generated from the planning CT scan. Two post-treatment CBCTs were randomly undertaken over the course of four weeks treatment for each patient. Two patients only had one post CBCT acquired.
Table 1.
Planning margins (CTV to PTV margins) used to generate three different bladder radiotherapy plans.
| Planning margin (cm) |
||||||
|---|---|---|---|---|---|---|
| Plan size | Superior | Inferior | Anterior | Posterior | Right | Left |
| Small | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 |
| Intermediate | 1.5 | 0.5 | 1.5 | 1.0 | 0.5 | 0.5 |
| Large | 2.5 | 0.8 | 2.0 | 1.2 | 0.8 | 0.8 |
A retrospective audit on the POD selection and intra-fractional bladder fillings were carried out on all twenty patients in this study. Descriptive statistics were collated on CBCTs of all patients (N = 20) to evaluate the difference in bladder volumes between pre and post-treatment CBCTs, intra-fractional bladder wall displacements, and the treatment duration for each faction (time taken between pre and post treatment CBCTs). The bladder volumes were delineated by a single observer on treatment fractions where both pre and post treatment CBCTs were conducted. Treatment duration was determined from acquisition of pre-treatment CBCT until acquisition of the post-treatment CBCT. A Wilcoxon Signed Rank test was used to assess any significant differences between the pre and post-treatment CBCT bladder volume and non-parametric Spearman’s Rank Correlation Coefficient was used to investigate the association between intra-fractional bladder filling and treatment time.
Results
POD adaptive bladder radiotherapy plan selection
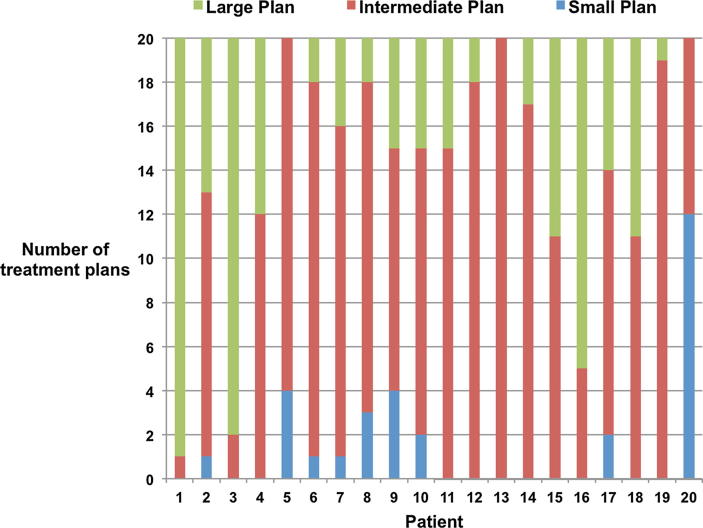
20/20 patients had daily online CBCTs resulting in a total of 400 pre-treatment CBCTs for the adaptive bladder radiotherapy POD selection. As shown in Fig. 1 30/400 (8%), 250/400 (63%) and 120/400 (30%) were treated with small, intermediate and large treatment plans, respectively. 2/20 patients only obtained one post-treatment CBCT, thus a total of 38 pairs of pre and post CBCTs were analysed.. Reviewing all 38 pairs of pre and post treatment CBCTs (a total number of 76 CBCTs), it’s confirmed that all POD selections were appropriately chosen to ensure that adequate coverage of the bladder target treatment volume was maintained post treatment.
Fig. 1.
Scatter plot of intra-fractional bladder filling against time between pre and post cone-beam CT scans.
Intra-fractional bladder filling
As shown in Table 2, the mean percentage difference in bladder volume pre and post CBCT was 13.7% and the mean absolute intra-fractional filling volume was 10.2 cc. There was significant difference in bladder volumes between pre- and post-treatment CBCTs (p < 0.05). A range of intra-fractional displacements of the outer bladder wall were noted. The expansion of the bladder predominately occurred in the superior (mean = 2.5 mm) and anterior (mean = 1.5 mm) directions.
Table 2.
Summary of intra-fractional bladder fillings and volumes, time and displacements of the outer bladder wall.
| Variables | Mean | Median | SD | 95% Confidence Interval | |
|---|---|---|---|---|---|
| Pre CBCT bladder volume (cc) | 97.0 | 79.7 | 48.4 | 81.1–113.0 | |
| Post CBCT bladder volume (cc) | 107.3 | 89.6 | 49.2 | 91.1–123.5 | |
| Absolute Intra-fractional bladder filling volume (cc) | 10.2 | 9.2 | 7.1 | 7.9–12.6 | |
| Percentage difference in bladder volumes between pre and post-treatment CBCT (%) | 13.7 | 9.2 | 13.9 | 9.1–18.3 | |
| Treatment duration (minutes) | 8.9 | 8.4 | 1.8 | 8.3–9.5 | |
| Intra-fractional bladder wall displacements | Superior (mm) | 2.5 | 2.5 | 1.9 | 1.9–3.1 |
| Inferior (mm) | 0.0 | 0.0 | 0.0 | N/A | |
| Left (mm) | 0.4 | 0.0 | 0.8 | 0.1–0.6 | |
| Right (mm) | 0.2 | 0.0 | 0.6 | 0.0–0.4 | |
| Anterior (mm) | 1.5 | 1 | 1.4 | 1.0–2.0 | |
| Posterior (mm) | 0.3 | 0 | 0.6 | 0.0–0.5 | |
The mean treatment duration was 8.9 min and all treatments were finished within the departmental 15-minute time slot. As illustrated in Fig. 2, intra-fractional bladder filling was associated with a weak correlation over time taken between the pre and post-treatment CBCT (rs = 0.26, p < 0.05).
Fig. 2.
A bar chart illustrating the adaptive treatment plan selection per CBCT for each patient.
Discussion
This study examined the POD plan selections and the impact of intra-fractional bladder filling on our departmental adaptive bladder radiotherapy delivery.
As indicated in Fig. 2, the majority of patients utilised all three plan options which signifies the daily variation in bladder motion. Compared to a POD protocol basing a library of plans on the first week of CBCTs, our approach could maximise the benefits of adaptive radiotherapy and avoid using a conventional plan with big PTV margins for the first week which contributed to 25% of the treatment course [9] Similarly to our selected plan options findings, Foroudi et al did find that a variety of plan options, with the small, medium and large plans being used 9.8%, 49.2% and 39.5% respectively, were all utilised in their online adaptive study [11]. This reinforces the need for a variety of plans to be available to account for the unpredictable bladder motion that can occur. The low percentage of small plans being used questions whether more can be done with the patient preparation information. Although all patients were asked to follow the set guidelines, the actual patient compliance was beyond the scope of this study.
With the analysis of the pre and post treatment CBCTs, it’s suggested that all POD options were appropriately chosen to ensure that adequate coverage of the bladder target treatment volume was maintained post treatment. This implied our departmental adaptive bladder radiotherapy process, including the use of the planning treatment margins, plan options and time taken to select the most appropriate plan has taken account of the impact of intra-factional bladder filling. As expected, there was significant difference in bladder volumes between pre- and post-treatment CBCTs (p < 0.05). Several studies reported that the average intra-fractional bladder filling approximately ranged from 9 to 11 cm3. These were comparable with our finding of 10.2 cc. A variety of intra-fractional displacements of the outer bladder wall were noted in our study but predominately occurred in the anterior and superior directions. This was supported by other studies and suggested that the bladder wall tended to expand the most in the anterior and superior anatomical directions but with minimal expansions in the inferior, posterior and lateral anatomical directions due to the design of the pelvis anatomy [10], [11], [12], [13], [14].
The intra-fractional bladder filling did increase with longer treatment duration although the correlation was suggested to be weak (rs = 0.26, p < 0.05). The average intra-fractional bladder filling and average time taken findings are supported by other studies investigating intra-fractional filling over time [11], [12], [13], [14], [15]. However our average time (8.9 min) was shorter in comparison with other similar studies which measured the time taken between pre and post cone beam CT scans (13 min). It is suggested that shorter treatment time cannot only have a perceived positive impact on time efficiency in terms of treatment time slot availability and department resources, but also reduce the risk of intra-fractional bladder motion as an increase in time is associated with an increase in intra-fractional bladder filling [15], [11], [12]. Furthermore, using a 3-field conformal plan over a longer 6–10 field intensity modulated radiotherapy plan highlights the advantage of our department’s planning and delivery technique. Our treatment time can potentially be decreased further using volumetric modulated arc therapy.
It is recognised that the main limitations of this audit were its retrospective nature, one single observer contouring the bladder volumes, the relatively small sample size, and the limited number of post-treatment CBCTs available to analyse.
In conclusion, this study has addressed its research aim and generates findings, supported by other national and international studies that help confirm that the effect of intra-fractional bladder filling does not affect the delivery of adaptive bladder radiotherapy and that the current treatment margins and process suffices.
Conflict of interest
The authors declare that there is no conflict of interest.
Acknowledgments
Acknowledgement
Permission for this study to be carried out was granted from our institution’s Information Governance department to ensure compliance with the necessary data protection requirements was met before undertaking any data collection.
We thank all the patients who participated in this study, and the doctors, nurses, radiographers and physicists at our centre. We acknowledge the support of Prof Peter Hoskin, Dr Peter Ostler, Dr Robert Hughes, Dr Roberto Alonzi, Dr Nicola Anyamene, Dr Karen Venables, Mr James Burnely, Ms Rita Simoes and Mrs Jagdeep Kudhail.
References
- 1.Kotwal S., Choudhury A., Johnston C., Paul A.B., Whelan P., Kiltie A.E. Similar treatment outcomes for radical cystectomy and radical radiotherapy in invasive bladder cancer treated at a United Kingdom specialist treatment centre. Int J Radiat Oncol Biol Phys. 2008;70(2):456–463. doi: 10.1016/j.ijrobp.2007.06.030. [DOI] [PubMed] [Google Scholar]
- 2.Taylor V., Kong A., Rosewall T. Adaptive radiotherapy for bladder cancer- a systematic review. J Med Imag Radiat Sci. 2017;48(2):199–206. doi: 10.1016/j.jmir.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 3.Kibrom A.Z., Knight K.A. Adaptive radiation therapy for bladder cancer: a review of adaptive techniques used in clinical practice. J Med Radiat Sci. 2015;62(4):277–285. doi: 10.1002/jmrs.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tobias J., Hockhauser D. Chapter 18: Genitourinary cancer. 7th ed. John Wiley & sons, Ltd.; Chichester: 2015. Cancer and its management; pp. 355–370. [Google Scholar]
- 5.Tuomikoski L., Valli A., Tenhunen M., Muren L., Vestergaard A. A comparison between two clinically applied plan library strategies in adaptive radiotherapy of bladder cancer. Radiother Oncol. 2015;117(3):448–452. doi: 10.1016/j.radonc.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 6.Kong V., Taylor A., Chung P., Rosewall T. Evaluation of resource burden for bladder adaptive strategies: a timing study. J Med Imag Radiat Oncol. 2018;62(6):861–865. doi: 10.1111/1754-9485.12787. [DOI] [PubMed] [Google Scholar]
- 7.Kong V., Taylor A., Chung P., Craig T., Rosewall T. Comparison of 3 image-guided adaptive strategies for bladder locoregional radiotherapy. Med Dosim. 2018 doi: 10.1016/j.meddos.2018.03.004. pii: S0958-3947(18)30037-2. [DOI] [PubMed] [Google Scholar]
- 8.Foroudi F., Pham D., Rolfo, Tang C.L., Tan A., Turner S. The outcome of a multi-centre feasibility study of online adaptive radiotherapy for muscle-invasive bladder cacner TROG 10.01 BOLART. Radiother Oncol. 2014;111(2):316–320. doi: 10.1016/j.radonc.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 9.Collins S., Leech M. A review of plan library approaches in adaptive radiotherapy of bladder cancer. Acta Oncol. 2018;57(5):566–573. doi: 10.1080/0284186X.2017.1420908. [DOI] [PubMed] [Google Scholar]
- 10.Foroudi F., Wong J., Kron T., Rolfo A., Haworth A., Roxby P. Online adaptive radiotherapy for muscle-invasive bladder cancer: Results of a pilot study. Int J Radiat Oncol Biol Phys. 2011;81(3):765–771. doi: 10.1016/j.ijrobp.2010.06.061. [DOI] [PubMed] [Google Scholar]
- 11.Foroudi F., Pham D., Bressel M., Gill S., Kron T. Intrafraction bladder motion in radiation therapy estimated from pretreatment and posttreatment volumetric imaging. Int J Radiat Oncol Biol Phys. 2013;86(1):77–82. doi: 10.1016/j.ijrobp.2012.11.035. [DOI] [PubMed] [Google Scholar]
- 12.Lalondrelle S., Huddart R.A., Warren-Oseni K., Hansen V.N., Mcnair H.A., Thomas K. Adaptive-predictive organ localisation using cone-beam computed tomography for improved accuracy in external beam radiotherapy for bladder cancer. Int J Radiat Oncol Biol Phys. 2011;79(3):705–712. doi: 10.1016/j.ijrobp.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 13.Lotz H.T., Pos F.J., Hulshof M.C.C.M., van Herk M., Lebesque J.V., Duppen J.C. Tumour motion and deformation during external radiotherapy of bladder cancer. Int J Radiat Oncol Biol Phys. 2006;64(5):1551–1558. doi: 10.1016/j.ijrobp.2005.12.025. [DOI] [PubMed] [Google Scholar]
- 14.Dees-Ribbers H.M., Betgen A., Pos F.J., Witteveen T., Remeijer P., van Herk M. Inter- and intra-fractional bladder motion during radiotherapy for bladder cancer: a comparison of full and empty bladders. Radiother Oncol. 2014;113(2):254–259. doi: 10.1016/j.radonc.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 15.MacDonald F., Lalondrelle S., Taylor H., Warren-Oseni K., Khoo V., McNair H.A. Clinical implementation of adaptive hypo fractionated bladder radiotherapy for improvement in normal tissue irradiation. Clin Oncol. 2013;25(9):549–556. doi: 10.1016/j.clon.2013.06.001. [DOI] [PubMed] [Google Scholar]