Abstract
Introduction
IGRT in cervical cancer treatment delivery is complex due to significant target and organs at risk (OAR) motion. Implementing image assessment of soft-tissue target and OAR position to improve accuracy is recommended. We report the development and refinement of a training and competency programme (TCP), leading to on-line Radiation Therapist (RTT) led soft-tissue assessment, evaluated by a prospective audit.
Methods and materials
The TCP comprised didactic lectures and practical sessions, supported by a comprehensive workbook. The content was decided by a team comprised of Clinical Oncologists, RTTs, and Physicists. On completion of training, RTT soft-tissue review proficiency (after bony anatomy registration) was assessed against a clinician gold-standard from a database of 20 cervical cancer CBCT images. Reviews were graded pass or fail based on PTV coverage assessment and decision taken in concordance with the gold-standard. Parity was set at ≥80% agreement.
The initial TCP (stage one) focussed on offline verification and decision making. Sixteen RTTs completed this stage, four achieved ≥80%. This was not sufficient to support clinical implementation.
The TCP was redesigned, more stringent review guidelines and greater anatomy teaching was added. TCP stage two focussed on online verification and decision making supported by a decision flowchart. Twenty-one RTTs completed this TCP, all achieved ≥80%. This supported clinical implementation of RTT-led soft-tissue review under prospective audit conditions.
The prospective audit was conducted between March 2017 and August 2017. Daily online review was performed by two trained RTTs. Online review and decision making proficiency was evaluated by a clinician.
Results
Thirteen patients were included in the audit. Daily online RTT-led IGRT was achieved for all 343 fractions. Two-hundred CBCT images were reviewed offline by the clinician; the mean number of reviews per patient was 15. 192/200 (96%) RTT image reviews were in agreement with clinician review, presenting excellent concordance.
Discussion and conclusion
Multidisciplinary involvement in training development, redesign of the TCP and inclusion of summative competency assessment were important factors to support RTT skill development. Consequently, RTT-led cervical cancer soft-tissue IGRT was clinically implemented in the hospital.
Keywords: Image guided radiotherapy, Cervical cancer, Cone-beam computed tomography, Radiation Therapists (RTT), RTT training, Competency assessment, RTT-led
Introduction
Effective radiotherapy for cervix cancer relies on delivery of a tumouricidal radiation dose to a clinical target volume (CTV) while limiting dose received by healthy tissue [1]. Significant position and shape variations occur in cervical cancer CTV anatomy, which includes the uterus, cervix, parametrium and upper-vagina, during radiotherapy largely due to changes in bladder [2], [3]; rectal [2], [4]; and tumour volume [4], [5]. Insufficient CTV coverage occurs even with large CTV to planning target volume (PTV) margins, resulting in target under-dosing [6] or over-dosing of normal tissue [7].
Image guided radiotherapy (IGRT) improves the ability to attain the desired CTV coverage whilst avoiding normal tissue [8], potentially reducing patients’ side-effects and improving outcomes. Image assessment of soft-tissue target and organ at risk (OAR) position to improve accuracy is recommended [9]. Implementation is complex as the cervix and uterus vary in spatial position relative to bony anatomy and each-other, causing CTV deformation [2], [5], while included pelvic-nodes are fixed relative to bony anatomy [2], [5]. Solely employing soft-tissue registration and translational isocentre corrections is not optimal to ensure correct target coverage [2], [10]. Images should be registered to stable pelvic bony anatomy with online assessment of CTV coverage by the PTV contour performed daily and set-up interventions made if CTV coverage is not achieved. The effect of bladder volume, rectal volume and pelvic pitch on set-up also requires daily consideration. To facilitate online review centres are encouraged to educate Therapeutic Radiographers/Radiation Therapists, hereafter referred to as RTTs, to evaluate the relevant structures on cervical cancer volumetric verification images [11].
When first considering implementation of RTT-led cervical cancer IGRT, a baseline study of RTTs’ cervical cancer IGRT knowledge and skills established a lack of confidence across many areas. Twelve RTTs with varying levels of clinical experience (1–18 years) completed a self-assessment questionnaire on their knowledge, understanding and technical skill related to cervical cancer soft-tissue IGRT (Appendix A). They rated their ability as some, competent or expert in relation to each of the nine statements. Unpublished results found that the majority of individuals rated their ability for each statement as less than expert (56 some, 46 competent and 6 expert). These results highlighted a need for additional training and guidance in this area before implementation.
At this time only two-dimensional departmental IGRT guidance was available and although nationally recommended no standard soft-tissue IGRT solution was proposed [9]. Radiotherapy centres were expected to develop their own protocols [9], accordingly we decided to develop and run a dedicated training and competency programme (TCP), with the aim of implementing RTT-led soft-tissue assessment on cone-beam computer tomography (CBCT). The methodology presented follows the TCP path through development; redesign and clinical implementation which was evaluated by a prospective audit. As the project includes several stages, to improve readability we have presented the work in chronological order.
Methods and materials
The TCP was reviewed and approved by The Royal Marsden Hospital (NHS Foundation Trust) Clinical Audit Committee (RT70).
TCP stage one
Development
Content of the TCP was developed by a multi-disciplinary implementation team (MDIT) comprising Clinical Oncologists; Physicists; and RTTs. The programme was organised to be relevant to all staff irrespective of delivery system.
The developed TCP comprised five hours of inter-professional didactic lectures and practical sessions covering; cervical cancer and pelvic anatomy, disease staging, radiotherapy techniques, organ motion recognition and IGRT principles. It was delivered over the course of one week and recorded for repeat viewing via the hospital’s online secure database. The programme was supported by a comprehensive workbook to reiterate taught material, showcase clinical examples and provide practical image registration and review guidelines.
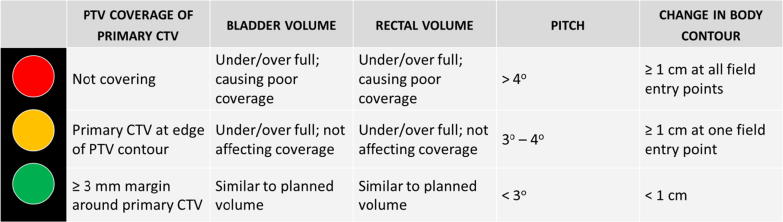
Fundamental to developing and evaluating RTT competence was standardisation of the cervical cancer soft-tissue review process. Stage one of the TCP focussed on offline verification and decision making. Assessment of PTV coverage, bladder and rectal volume, pelvic pitch and body contour was guided by a traffic-light decision support tool (Fig. 1). Wherein red, amber and green associated respectively to; a considerable deviation from planned position requiring urgent intervention, a deviation from planned position requiring monitoring and as planned. Decision choices comprised: seek advice, intervene before next fraction or no action.
Fig. 1.
Traffic light decision support tool, stage one.
Competency assessment
RTT soft-tissue review proficiency (after bony anatomy registration) was assessed against a clinician gold-standard from a database of 20 cervical cancer CBCT images.
Two image databases were created, necessary as the hospital has two radiotherapy departments split over two sites. One departmental site utilises Varian (Palo Alto, California, USA) and the other Elekta (Stockholm, Sweden) equipment. CBCT images were sampled from a retrospective frame of patients who received radical radiotherapy for locally advanced cervical cancer between March 2014 and March 2015; who gave prior consent for their images to be used for research. Database images were purposively selected by the MDIT to include a range of clinical situations. The Consultant Clinical Oncologist (CCO) at each site generated the gold-standard image assessment by reviewing the site specific database and completing a standardised image review document per image.
All reviews were graded pass or fail based on PTV coverage assessment and decision taken in concordance with the gold-standard. Parity was set at ≥80% agreement based on similar studies [12], [13]. Assuming the true rate-of-agreement is 80%, the required sample size was 280 image reviews, when a one-sided alpha of 0.05 and a statistical power of 85% are used. Calculations were completed using SPSS®. With 20 images in the database, a minimum of 14 RTTs needed to be recruited to the TCP.
Alongside the summative assessment, RTTs completed self-assessment proficiency questionnaires (Appendix A) immediately before commencement of the TCP and on submission of competency assessment. A Wilcoxon signed-rank test was implemented using SPSS® to test whether individuals’ post-TCP scores were significantly higher than pre-TCP scores. To enable this, answers ‘some/competent/expert’ were converted into 1/2/3 scores respectively.
RTT recruitment
Volunteers, of all grades, who had attained standard departmental image verification competencies, were requested to take part. Nineteen RTTs; composed of eleven junior RTTs and eight senior RTTs were recruited and provided written consent. RTT grade was recorded so a simple nonparametric correlation coefficient (Spearman’s rho) between grade and percentage concordance could be calculated using SPSS®.
On completion of taught sessions RTTs were given four weeks, within standard working hours, to complete the competency assessment.
Evaluation
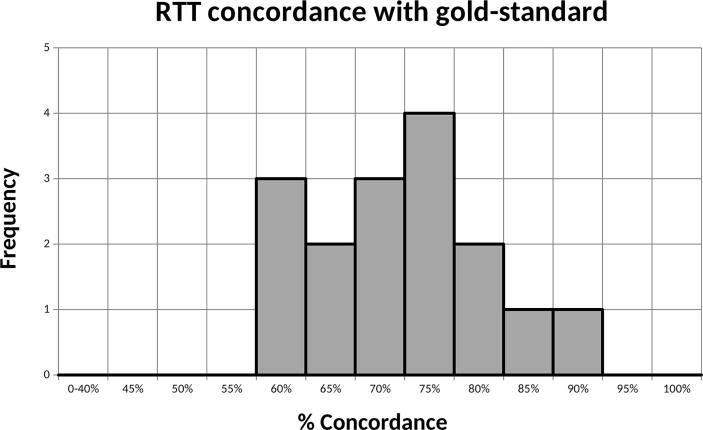
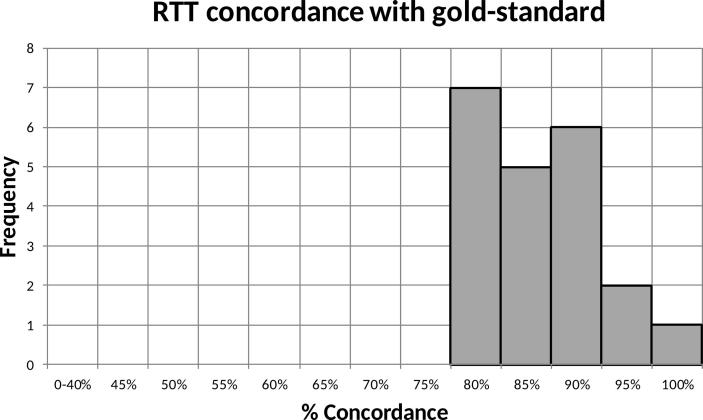
Sixteen RTTs completed the TCP in stage one. 231/320 (72%) image reviews concurred with the gold-standard. Individual concordance with gold-standard ranged from 60% to 90%, four achieved ≥80%, signifying parity (Fig. 2). This was not sufficient to support clinical implementation.
Fig. 2.
RTT concordance with gold-standard, stage one.
Correlation between RTT grade and percentage-concordance was low (r = 0.149); the two are not significantly correlated (p = 0.583).
RTTs’ self-assessments showed that the TCP significantly (p < 0.05) improved 12/16 RTTs’ scores. A trend for RTTs to have an inflated perception of their competence emerged. Fifteen of 16 RTTs deemed themselves competent to safely and correctly review cervical cancer CBCT images and make appropriate decisions while the summative competency assessment established only four as competent. This reinforced that summative competency assessment was crucial to proving safe practice.
Re-design
TCP stage one supported the principle that with advanced training parity with clinicians could be achieved in this task. Yet it only enabled four RTTs to achieve the pass threshold meaning it was ineffective in its objective to support clinical implementation of RTT-led cervical cancer IGRT. TCP redesign was deemed necessary to enable more RTTs to attain parity with clinicians.
TCP stage two
Development
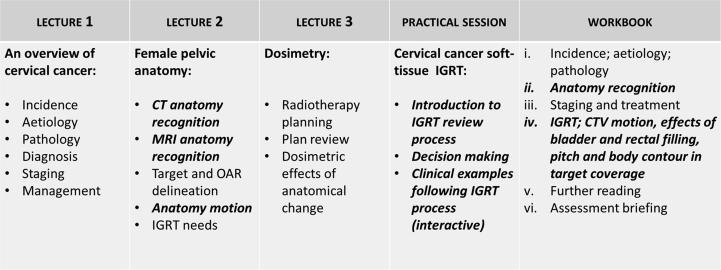
More stringent review guidelines and greater anatomy teaching was developed in advance of repeating the TCP. The TCP content, prepared by the MDIT, is presented in Fig. 3, topics expanded upon from TCP stage one are highlighted.
Fig. 3.
TCP content, stage two (sections updated from TCP stage one shown in bold italics).
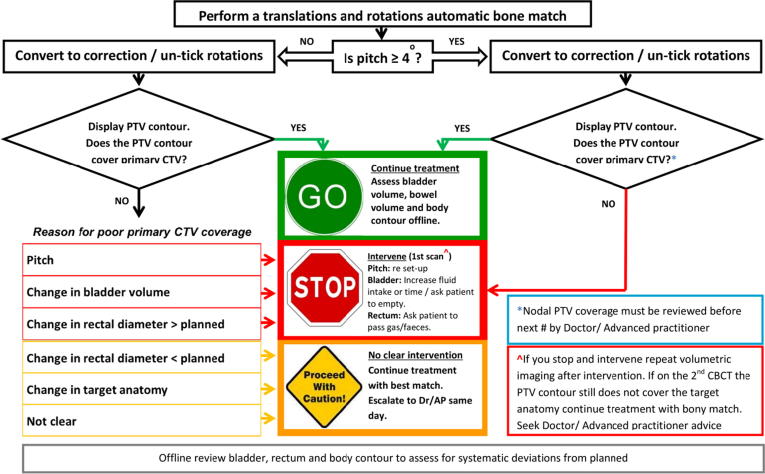
Stage two focussed on online verification and decision making. The move to online review was to align departmental protocol and national guidelines. Patients are standardly planned with Intensity Modulated Radiotherapy (IMRT), its steep dose gradients are less forgiving of geometrical inaccuracy hence daily online volumetric IGRT is advised [9]. The traffic-light decision support tool was replaced by a more prescriptive image review decision flowchart (Fig. 4). This flowchart directs the RTT to sequentially: assess pelvic pitch and PTV coverage, identify causes of sub-optimal primary clinical target volume (CTVp) coverage and resolve to deliver treatment or intervene before treatment.
Fig. 4.
Cervical cancer IGRT decision flowchart.
Competency assessment
As for stage one RTT soft-tissue review proficiency (after bony anatomy registration) was assessed against a CCO gold-standard database of 20 cervical cancer CBCT images. The same database images as for stage one were utilised for convenience. Both CCO’s re-reviewed the database images following the updated decision flowchart; answers were captured on a standardised image review assessment sheet and formed the new gold-standard.
Reviews were graded pass or fail based on CTVp coverage by PTV contour assessment (yes/no), decision taken (go/proceed with caution/stop) and intervention made in concordance with the gold-standard. Parity was set at ≥80% agreement.
Self-assessment competency was assessed pre and post TCP. These were used for self-reflection only and were not collected by the researcher.
RTT recruitment
As per stage one, volunteer RTTs of all grades were sought from across the hospitals two radiotherapy departments. Individuals who had not completed standard departmental image verification competencies were excluded as were those who participated in stage one; this was to avoid prior teaching biasing results. Twenty-one RTTs comprising nine junior RTTs and 12 senior RTTs were recruited and provided written consent.
On completion of taught sessions RTTs had four weeks to complete the competency assessment.
Evaluation
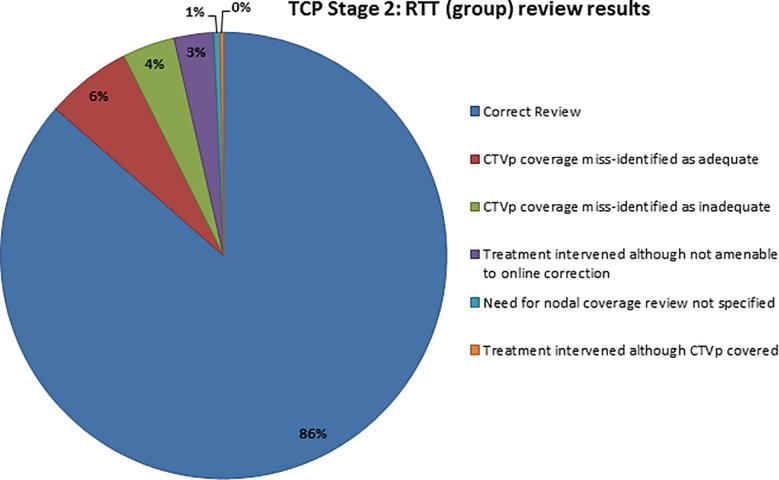
All 21 RTTs completed stage two. 363/420 (86%) image reviews concurred with the gold-standard. Individual concordance rates ranged from 80-100%; all achieved parity (Fig. 5).
Fig. 5.
RTT concordance with gold-standard, stage two.
Fig. 6 presents image review concordance for the cohort as a group. 42/57 non-concordant image reviews were the result of incorrect assessment of CTVp coverage by the PTV contour and subsequent inexact decision making. Inadequate CTVp coverage was missed by RTTs in 26/42 of these reviews and adequate CTVp coverage was incorrectly identified as inadequate in 16/42.
Fig. 6.
RTT (group) image review results, stage two.
15/57 non-concordant image reviews were the result of incorrect or incomplete decision making. RTTs misread poor CTVp coverage to be amenable to interventional improvement in 12/15 reviews whereas the gold-standard contributed poor CTVp coverage to anatomy changes not correctable through online intervention. The two clinical scenarios were; posterior displacement of the cervix due to the movement of a posterior bowel loop and distension of the uterus due to fluid build-up. In 2/15 reviews the need to assess nodal coverage offline was not documented and in 1/15 reviews the RTT intervened although the target was covered, rationale being to improve coverage further.
Correlation between RTT grade and percentage-concordance was low and not significant (r = −0.124; p = 0.593).
Stage two results supported the clinical implementation of RTT-led soft-tissue review under prospective audit conditions.
Prospective audit – implementation into clinical practice
A prospective audit of RTT-led cervical cancer soft-tissue review was approved by The Royal Marsden Hospital (NHS Foundation Trust) Clinical Audit Committee (RT81) in September 2016.
All patients commencing radical radiotherapy for un-operated cervical cancer within a six month period from March 2017 until August 2017, who had consented for their treatment associated images to be used for research, were included in this prospective study. Patients were treated with IMRT, receiving either 50.4 Gy or 45 Gy in 28 or 25 fractions respectively, as per radiotherapy departmental standard protocol. The CTVp to PTV margins were; 1–1.5 cm anterior/posterior, 1 cm laterally and 1.5–2 cm superiorly/inferiorly. A bladder filling protocol for planning CT and daily treatment was followed; empty bladder, drink 350 ml in 10minutes, wait 45minutes. No bowel preparation was routinely given.
Pre-treatment CBCT was acquired at each fraction. Six-dimensional (translations and rotations) registration to stable pelvic bony anatomy was performed initially to quantify pelvic tilt. Image registration was then re-set to account for translational shifts only. Daily online review of target anatomy (CTVp) coverage was performed by two trained RTTs, from the collective achieving parity in TCP stage two. Image review and decision making followed the workflow presented in Fig. 4; and was captured on a standardised image review assessment sheet.
The quality of the daily RTTs’ review and decision making skills were evaluated independently by the CCO at each site. The CCO reviewed 15 CBCT images per patient; the first five images from treatment fraction one to five and 10 further image reviews selected randomly over the treatment period. CCO review was performed offline at once weekly intervals over the course of a patient’s treatment; review of all imaging for every patient was not achievable due to CCO time limitations. To ensure reliability and comparability the CCO followed the workflow presented in Fig. 4 and completed the same documentation as the RTTs. The CCO was blinded to the decisions made by the RTTs. To avoid RTTs online decision making being influenced by CCO reviews they were blinded to CCO assessments until completion of the prospective audit.
Results
Thirteen patients (five from one department site and eight from the other) were included within this six month audit period. Online image review by two competent RTTs was achieved for all patients at all fractions.
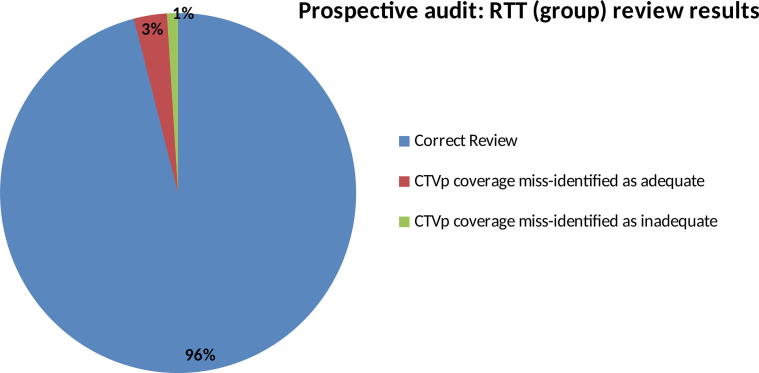
In total 200 images (mean per patient = 15; range; five to 20) were reviewed offline by the CCO. Of these; 180 were initial CBCT images and 20 were repeat CBCT images after intervention.
Image review concordance for the cohort was 192/200 (96%) (Fig. 7). Of the eight non-concordant image reviews, two resulted from adequate CTVp coverage being misidentified as inadequate. In both cases bladder volume was deemed greater than planned causing a CTVp partial-miss; treatment was stopped, the patient asked to re-prepare their bladder and treatment subsequently delivered with good target coverage. 6/8 (5 first image, 1 repeat image) were as the result of inadequate CTVp coverage being missed by RTT review. In all incidences the missed area was assessed as clinically insignificant by the CCO.
Fig. 7.
RTT (group) image review results, clinical practice.
Discussion
We have successfully implemented RTT-led cervical cancer soft-tissue review by designing and reiterating a training model specific to cervical cancer IGRT. RTT-led cervical cancer soft-tissue review is now routine practice with CCO review reserved for complicated cases where RTTs seek guidance. Aside from the immediate purpose of improving accuracy of treatment delivery, RTT-led IGRT for cervix cancer has demonstrated other benefits. Less reliance on clinician availability results in improved workflow efficiency [14] and patient satisfaction. Additionally advanced RTT skills enable autonomy and increase engagement with patient involvement through real time feedback with regards to bladder preparation.
One other paper was found to present RTT education specific to cervical cancer IGRT [11]. The alternative training model describes two and a half hours of online self-education and seven hours of “hands on training” [11]. Specific themes covered within the taught component; disease and treatment of cervical cancer, female pelvic anatomy and inter-fractional challenges during EBRT, are comparable to those covered in the presented TCP advocating their pertinence. However, no competency component is directly discussed, making firm comparisons with our training difficult. They do reference prior experience presented by Boejen et al [15], stating their learning programme was similar to this work.
Boejen et al [15] presents training and competency assessment in an established virtual reality learning centre [15]. The advantage of virtual reality training is having a protected environment where new skills can be tested out on clinical cases without risk to the patient or interference to clinical workflow [16], the restriction being cost and space implications. RTTs’ competency in adaptive bladder plan selection was assessed in teams of two, each team reviewing 16 CBCT images [15]. A risk of assessing initial competency in pairs is that one RTT may dominate and less confident RTTs may not be identified. An advantage of this competency assessment was that it took place within the training session, expediting quicker transition from training to clinical implementation.
From delivery of our TCP stage two to clinical implementation within the prospective audit, a delay of eight weeks was incurred. Although RTTs were scheduled within work hours to attend training lectures finding time away from the treatment unit to complete the competency assessment was arranged within individuals working teams. Allowing a four week completion period proved achievable for most however the deadline was extended to six weeks to account for individuals’ unexpected periods of absence. Had competency assessment time also been assigned, the process may have been expedited. Assessment grading and feedback occurred within scheduled weekly review meetings and incurred a further delay of two weeks. The delay risked RTTs forgetting aspects of training or deskilling over time [12], this was managed by consolidation of training within the workbook, shown to increase clinical decision making [17]. The benefit of the delay was certainty and minimised resource waste; had competency not been achieved, as in stage one, modifications could have been implemented before going live.
The training model presented by Jensen et al [11] elicited similar results to ours. 89.7% of RTT reviews assessed target coverage correctly [11] compared with 96%. The percentage of CBCT reviews where the target was assessed as being inside the PTV although it was marginally outside was 0.7% versus 3%. Results presented by Jensen et al [11] reviewed 563 CBCT images, almost 10% of which could not be evaluated by RTTs due to poor image quality; the prospective audit presented here reviewed fewer images (200) but all were evaluable. Neither directly or systematically analyse CBCT image quality, it would be sensible to introduce a CBCT quality assessment scale if developing further IGRT training to ensure training database images represent all degrees of image quality encountered by RTTs in clinical practice.
A potential limitation of this study is that only a sample of RTT assessments were reviewed by the CCO offline, in contrast to the work by Jensen et al [11] where all RTT assessments were evaluated. The CCO’s busy workload demanded an efficient review process. It was felt that randomly sampling 15 images per patient, taken over the treatment duration, facilitated timesaving while maintaining sufficient representation of each patient.
The need for summative competency assessment to prove safe and compliant practice [18] was demonstrated by considerable inter-RTT variability and over-estimation of self-competence in TCP stage one. The utilisation of a gold-standard imaging database proved a successful tool to determine competence in TCP stage two, as supported within similar bladder and lung cancer IGRT studies [11], [19] and recommended by national guidance [9]. Inter-RTT concordance variability was evidently reduced from TCP stage one to two; 60–90% versus 80–100%. TCP stage two introduced a prescriptive image review flowchart, reduced RTT variability supports that this tool aided more consistent image review and decision making. Radiographers work in an environment that demands adherence to process and protocols and they are generally stronger at perceiving information in a concrete manner and processing this actively [20]. As such, flowcharts likely suit RTTs’ learning style and professional conditioning. This study’s finding reflect previous USA-based research identifying Radiography students as task-orientated and purposeful learners where task-orientation was characterised by structure and results, whilst purposeful learning involved persistent integration of theory and practice[21]. However, the previous research comprised pre-registration learners whereas our study involved work-based learning in post-registration RTTs.
Considerably greater concordance with the gold-standard was appreciated when two RTTs reviewed the images online compared to individual review within TCP stage two; 96% versus 86%. This trend was also appreciated by McNair et al [12] who reported inflation in RTT concordance with gold-standard from 76% to 91% with two trained observers. This is not surprising and supports safe practice guidance that radiotherapy is delivered by two competent RTTs [22]. To further support RTT learning from practice, on completion of the prospective audit, results including reflections on incorrect assessments were displayed in a PowerPoint presentation and circulated to all participants. Whilst a lone observer does not reflect clinical practice, assessing individuals’ competency has proved an effective education tool. It appears reasonable, based on both these studies, to have a lower threshold of acceptability for a single observer compared to two [12].
No statistically significant link between RTT grade and concordance was established, reinforcing this advanced training should be open to all grades. This is supported by Jereczek-Fossa et al [23] who determined satisfactory agreement between senior and junior RTTs, in prostate-verification [23]. The RTT demographics examined within this research cannot however rule out the influence of RTTs’ clinical-experiences on concordance. Greater examination of RTT demographics, including CBCT experience; pre-treatment experience; and years of experience may have elicited reasons behind score variably; this may enable more tailored education.
As TCP stage two proved a successful training tool facilitating excellent RTT concordance with the gold-standard online, it has since been used to develop the skills and competency of 55 further RTTs across the hospitals two radiotherapy departments. The continuous development of staff is essential to sustain daily online cervical cancer soft-tissue review through; staff turnaround, annual leave, sickness and department rotations. The availability of recorded sessions has enhanced the convenience of TCP delivery as individual RTTs can be trained as required rather than waiting for larger group sessions which require; space, trainee time and extended RTT time away from clinical practice.
Presently the MDIT are further developing this training programme to introduce cervical cancer adaptive plan-of-the-day (POD) radiotherapy. The current training programme provides RTTs with the target motion knowledge underpinning the rationale for POD [24]; having achieved this standard already should expedite the training requirements for POD. Buy-in from the MDIT has, at every stage and continues to be, imperative. The heterogeneity of skills and knowledge offered by this team brought different perspectives to each task, improving effectiveness and patient safety and fuelling creative solutions [25], [26], [27]. It also ensured TCP content validity.
In addition to the MDIT, working within the directives of clinical audit also helped secure clinical success for this project. As with similar projects [12], the first iteration of the training programme was not fully successful but the cyclical nature of clinical audit enabled initial failings of TCP stage one to be established, evaluated and reflected on. This provided invaluable information to the MDIT, allowing them to make more effective decisions [28] during TCP redesign and clinical implementation.
Conclusion
RTT-led cervical cancer soft-tissue IGRT was successfully clinically implemented with the use of a training programme and summative competency assessment. Efforts to ensure the quality of a new training programme are essential, multidisciplinary input and audit conditions help to ensure this.
Advancing RTTs’ knowledge of cervical cancer anatomy, motion and treatment also provides a firm theoretical basis upon which further training can be build, such as adaptive plan selection skills. We propose this programme could be transferred to other departments or modified to other tumour sites
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This article represents independent research [part] funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at the Royal Marsden NHS Foundation Trust and the Institute of Cancer Research. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Contributor Information
S.E. Alexander, Email: sophie.alexander@rmh.nhs.uk.
N. Hopkins, Email: naomi.hopkins@rmh.nhs.uk.
S. Lalondrelle, Email: susan.lalondrelle@rmh.nhs.uk.
A. Taylor, Email: alexandra.taylor@rmh.nhs.uk.
H.A. McNair, Email: helen.mcnair@rmh.nhs.uk.
Appendix A.
| Clinical Competency | Some | Competent | Expert | Comments | |
|---|---|---|---|---|---|
| 1 | Knowledge of female pelvic CT anatomy. | ||||
| 2 | Knowledge of female pelvic MRI anatomy. | ||||
| 3 | Underpinning knowledge of cervical cancer, rationale for treatment and treatment technique. | ||||
| 4 | Ability to review and identify changes in bladder and rectal volume on CBCT images. | ||||
| 5 | Ability to review and identify changes in vagina, cervix and uterus position on CBCT images. | ||||
| 6 | Ability to review and identify pitch on CBCT images. | ||||
| 7 | Ability to review and identify changes in patient contour on CBCT images. | ||||
| 8 | Ability to review and identify changes in PTV coverage on CBCT images. | ||||
| 9 | Ability to safely and correctly analyse cervical CBCTs and make appropriate decisions. | ||||
References
- 1.McNair H.A., Hansen V.N., Parker C.C., Evans P.M., Norman A., Miles E. A comparison of the use of bony anatomy and internal markers for offline verification and an evaluation of the potential benefit of online and offline verification protocols for prostate radiotherapy. Int J Radiat Oncol Biol Phys. 2008;71(1):41–50. doi: 10.1016/j.ijrobp.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 2.Taylor A., Powell M.E.B. An assessment of interfractional uterine and cervical motion: Implications for radiotherapy target volume definition in gynaecological cancer. Radiother Oncol. 2008;8;88(2):250–257. doi: 10.1016/j.radonc.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 3.Bondar L., Hoogeman M., Mens J.W., Dhawtal G., de Pree I., Ahmad R. Toward an individualized target motion management for IMRT of cervical cancer based on model-predicted cervix–uterus shape and position. Radiother Oncol. 2011;5;99(2):240–245. doi: 10.1016/j.radonc.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 4.Collen C, Engels B, Duchateau M, Tournel K, De Ridder M, Bral S, et al. Volumetric imaging by megavoltage computed tomography for assessment of internal organ motion during radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys 2010 8/1;77(5):1590–1595. https://doi.org/10.1016/j.ijrobp.2009.10.021. [DOI] [PubMed]
- 5.Lim K., Kelly V., Stewart J., Xie J., Cho Y., Moseley J. Pelvic radiotherapy for cancer of the cervix: is what you plan actually what you deliver? Int J Radiat Oncol Biol Phys. 2009;5/1;74(1):304–312. doi: 10.1016/j.ijrobp.2008.12.043. [DOI] [PubMed] [Google Scholar]
- 6.Tyagi N., Lewis J.H., Yashar C.M., Vo D., Jiang S.B., Mundt A.J. Online cone beam computed tomography to assess interfractional motion in patients with intact cervical cancer. Int J Radiat Oncol Biol Phys. 2011;5/1;80(1):273–280. doi: 10.1016/j.ijrobp.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Mundt A., Yashar C., Mell L. 2nd ed. Demos Medical; New York, USA: 2011. Gynecologic Cancer. [Google Scholar]
- 8.Dawson L.A., Jaffray D.A. Advances in image-guided radiation therapy. J. Clin Oncol. 2007;25(8):938–946. doi: 10.1200/JCO.2006.09.9515. [DOI] [PubMed] [Google Scholar]
- 9.National Radiotherapy Implementation Group. Image Guided Radiotherapy: Guidance for implementation and use; 2012.
- 10.Lim K, Stewart J, Kelly V, Xie J, Brock KK, Moseley J, et al. Dosimetrically triggered adaptive intensity modulated radiation therapy for cervical cancer. Int J Radiat Oncol Biol Phys 2014 9/1;90(1):147–154. https://doi.org/10.1016/j.ijrobp.2014.05.039. [DOI] [PubMed]
- 11.Jensen N.B., Assenholt M.S., Fokdal L.U., Vestergaard A., Schouboe A., Kjaersgaard E.B. Cone beam computed tomography-based monitoring and management of target and organ motion during external beam radiotherapy in cervical cancer. Phys Imag Radiat Oncol. 2019;1(9):14–20. doi: 10.1016/j.phro.2018.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McNair H., Hafeez S., Taylor H., Lalondrelle S., McDonald F., Hansen V. Radiographer-led plan selection for bladder cancer radiotherapy: initiating a training programme and maintaining competency. Br J Radiol. 2015;88(1048):20140690. doi: 10.1259/bjr.20140690. [DOI] [PubMed] [Google Scholar]
- 13.Boston S., Scrase C., Hardy V. 140 Implementation of radiographer led planning target delineation for prostate cancer. Radiother Oncol. 2005;1(76):S73. [Google Scholar]
- 14.Royal College of Radiologists. Guide to job planning in clinical oncology; 2012.
- 15.Boejen A., Vestergaard A., Hoffmann L., Ellegaard M.B., Rasmussen A.M., Møller D. A learning programme qualifying radiation therapists to manage daily online adaptive radiotherapy. Acta Oncol. 2015;54(9):1697–1701. doi: 10.3109/0284186X.2015.1062914. [DOI] [PubMed] [Google Scholar]
- 16.Boejen A., Grau C. Virtual reality in radiation therapy training. Surg Oncol. 2011;20(3):185–188. doi: 10.1016/j.suronc.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Nisbet H., Matthews S. The educational theory underpinning a clinical workbook for VERT. Radiography. 2011;17(1):72–75. [Google Scholar]
- 18.Franklin N., Melville P. Competency assessment tools: an exploration of the pedagogical issues facing competency assessment for nurses in the clinical environment. Collegian. 2015;22(1):25–31. doi: 10.1016/j.colegn.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 19.Hudson J., Doolan C., McDonald F., Locke I., Ahmed M., Gunapala G. Are therapeutic radiographers able to achieve clinically acceptable verification for stereotactic lung radiotherapy treatment (SBRT)? J Radiother Pract. 2015;14(1):10–17. [Google Scholar]
- 20.Fowler P. Learning styles of radiographers. Radiography. 2002;8(1):3–11. [Google Scholar]
- 21.Ward P., Makela C. Radiography students’ clinical learning styles. Radiol Technol. 2010;81(6):527–537. [PubMed] [Google Scholar]
- 22.Donaldson SR. Towards safer radiotherapy. British Institute of Radiology, Institute of Physics and Engineering in Medicine, National Patient Safety Agency, Society and College of Radiographers, The Royal College of Radiologists, London; 2007.
- 23.Jereczek-Fossa B., Pobbiati C., Santoro L., Fodor C., Fanti P., Vigorito S. Prostate positioning using cone-beam computer tomography based on manual soft-tissue registration. Strahlenther Onkol. 2014;190(1):81–87. doi: 10.1007/s00066-013-0387-1. [DOI] [PubMed] [Google Scholar]
- 24.Heijkoop ST, Langerak TR, Quint S, Bondar L, Mens JW, Heijmen BJ, Hoogeman MS. Clinical implementation of an online adaptive plan-of-the-day protocol for nonrigid motion management in locally advanced cervical cancer IMRT. Int J Radiat Oncol Biol Phys 2014;90(3):673–9. https://doi.org/10.1016/j.ijrobp.2014.06.046. [DOI] [PubMed]
- 25.Borrill C.S., Carletta J., Carter A., Dawson J.F., Garrod S., Rees A. University of Aston in Birmingham; Birmingham: 2000. The effectiveness of health care teams in the National Health Service. [Google Scholar]
- 26.Prades J., Remue E., Van Hoof E., Borras J.M. Is it worth reorganising cancer services on the basis of multidisciplinary teams (MDTs)? A systematic review of the objectives and organisation of MDTs and their impact on patient outcomes. Health Policy. 2015;119(4):464–474. doi: 10.1016/j.healthpol.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 27.Kane B., Luz S. “Do no harm”: Fortifying MDT collaboration in changing technological times. Int J Med Inf. 2013;82(7):613–625. doi: 10.1016/j.ijmedinf.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 28.Tabrizi J.S., Farahsa S. How evaluation and audit is implemented in educational organizations? A systematic review. Res Dev Med Educ. 2015;4(1):3. [Google Scholar]