Abstract
Background
A straight line–based model is often used to calculate the distance between an out‐of‐hospital cardiac arrest (OHCA) and the location of an automated external defibrillator (AED). This model may be inaccurate as it overlooks any obstacles between the OHCA and AED. This study aimed to elucidate the effect of the straight line–based and walking route–based calculation on the average distance between an historical OHCA and the closest AED and the coverage rate of AEDs, ie, the proportion of historical OHCAs that were within 100 meters of an AED. It is hoped that the findings will help policy makers in deploying AEDs in optimal urban settings.
Methods and Results
This was an observational study conducted in Hong Kong. The average distance between an historical OHCA and its closest AED and the coverage rate of AEDs were calculated with both the straight line–based and walking route–based model. A total of 1637 AEDs and 5119 cases of OHCA were included for analysis. The average distances calculated by the straight line–based and walking route–based model were 230.8 and 545.3 meters, respectively. The coverage rate calculated by the straight line–based model was 30.04%, while that by the walking route–based model was 11.17%.
Conclusions
The straight line–based model may underestimate the average distances and overestimate the coverage rate in an urban setting. The walking route–based model may be more useful for studies of AED deployment in urban cities.
Keywords: automated external defibrillator, sudden cardiac arrest, deployment
Subject Categories: Sudden Cardiac Death, Ventricular Fibrillation, Cardiopulmonary Arrest, Health Services
Clinical Perspective
What Is New?
There could be significant differences in the average distance between an out‐of‐hospital cardiac arrest and the closest automated external defibrillator (AED) and the coverage rate of AED between the calculations by the straight line–based and walking route–based model.
The straight line–based model tends to underestimate the average distance between an out‐of‐hospital cardiac arrest and the closest AED and overestimate the coverage rate of AEDs.
What Are the Clinical Implications?
The walking route–based model is preferred to a straight line–based model in planning AED deployment in urban settings.
Public access defibrillation programs are useful to improve the survival rate of out‐of‐hospital cardiac arrest (OHCA).1 One critical factor that leads to the success of such programs is shortened time to first defibrillation. In respect to this, existing guidelines recommend that an automated external defibrillator (AED) should be placed such that a bystander can get to it within 100 meters of a cardiac arrest.2, 3, 4 How to ensure that an AED is available within 100 meters of an OHCA has been a focus of investigations. Different mathematical models aimed at optimizing AED deployment have been developed and tested.5, 6, 7, 8, 9 These models have used either the average distance between an OHCA and its closest AED or coverage rate, ie, the proportion of historical OHCAs that are within 100 meters of an AED as a measure of whether AED deployment is optimal. One commonality of these models is that the calculation of the distance was based on a straight line radius distance on a map. However, in an urban setting, streets and alleys twist around buildings. A study by Bryan10 used a walking route–based calculation to optimize the AED locations. The OHCA and candidate AED locations in their study, however, lacked representativeness in terms of the OHCA they chose and the candidate locations for placing additional AEDs. The target samples of OHCAs were extracted from ambulance calls, and only 48 calls were real OHCAs. The candidate locations for placing the new AEDs were 212 restaurants. They did not consider other locations where OHCAs more commonly occur, eg, sports grounds and transport stations. The present study aimed to elucidate the effect of the straight line– and walking route–based calculation on the average distance between an historical OHCA and the closest AED and the coverage rate of AEDs in an urban setting. The findings should bring more insight to policy makers when they are planning for AED deployment in their localities.
Methods
All data and materials used in this study have been made publicly available and can be accessed at https://github.com/Cainefm/maxcovr. This was an observational study conducted in Hong Kong from July 1, 2015, to December 31, 2016. Hong Kong is a highly urbanized city with a population of 7.4 million and an area of 1100 square kilometers. The incidence of OHCA was estimated to be 72 cardiac arrests per 100 000 people.11 There is no AED registry in Hong Kong. The use and placement of AEDs is unregulated and unguided. A public accessible defibrillator in this study was defined as an AED that was reachable by any person in the community. Sources of data of the publicly accessible AEDs in this study were the major AED suppliers in Hong Kong, government offices, the Leisure and Cultural Services Department (LCSD), the Department of Health, St. John Brigade, Hong Kong Red Cross, major mall owners, public utilities corporations such as the Mass Transit Railway, and the Heart‐Safe School Project.12 Each AED identified during the study period was recorded with an exact postal address. Data accuracy was ensured by door‐to‐door verification and direct contact with the individuals in charge of the premises or facilities where the AEDs were housed.
An historical cohort of nontrauma OHCA cases was used in the calculation of the average distance between an OHCA and its closest AED and the coverage rate. The data of the OHCA cases were from the database prospectively collected by the local emergency medical service, which is run by the Hong Kong Fire Services Department of the Hong Kong Government, from August 1, 2012, to July 31, 2013. In this database, the locations of cardiac arrests attended by the emergency medical service were recorded as longitude and latitude.
To facilitate quantification of the spatial relationship with the historical cases of OHCA, the addresses of the AEDs identified in the study period were first converted to longitude and latitude by Python 2.7 with pygeocoder packages (Python Software Foundation) and Google's Geocoding API. These geographical information system data, together with those of OHCA, were then converted into Universal Transverse Mercator format. When the distances between points on a map are calculated, the Universal Transverse Mercator coordinate system allows the distances based on meters constantly rather than considering degrees and minutes. R for Windows 3.2.5 (package “rgdal,” “raster,” “rgeos,” and “ggplot2”) was used to perform the geographical information system analysis and visualization. To quantify the spatial relationship, 2 computations were then performed. First, the average distance between an OHCA with its closest AED was calculated. Second, the coverage rate was obtained by calculating the proportion of historical OHCAs occurring within 100 meters of an AED. The straight line–based and walking route–based distances, which did not include elevation, were used in the calculation of these 2 measures. The straight line distances were calculated by Haversine formula. The walking route distances were calculated by the Open Source Routing Machine, which is designed as a routing engine for the shortest path in road networks.13 The back end was built on Ubuntu 19.04 x64 (Canonical Ltd.). Chi‐square and t tests were used to verify the statistical difference where appropriate. The study was approved by the institutional review board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster and informed consent was waived.
Results
During the study period, 1637 AEDs were identified across all districts of Hong Kong. The number of AEDs per 10 000 population and per kilometer squared were 2.23 and 1.48, respectively. The majority (49.4%) of AEDs were installed at educational institutions. Deployment at recreational facilities came second (29.3%). These recreational facilities were mostly manned by the LCSD and included sports centers, parks, swimming pools, beaches, museums, and libraries (Table 1).
Table 1.
Distribution of Existing AEDs
| Location | Frequency, No. (%) |
|---|---|
| Educational institutions | 809 (49.4) |
| Recreational facilities | 479 (29.3) |
| Mass transit railway stations | 216 (13.2) |
| Malls and commercial buildings | 74 (4.5) |
| Government buildings | 56 (3.4) |
| Others | 3 (0.2) |
AEDs indicates automated external defibrillators.
There were 5154 nontrauma OHCA cases from the database from August 1, 2012, to July 31, 2013. Thirty‐five cases were excluded because of wrong or absent geographical information system information. Therefore, 5119 cases were analyzed. The most common location was patients’ home (51.8%). Approximately 13% of cardiac arrests occurred in public locations (including streets) (Table 2).
Table 2.
Locations of Historical OHCAs
| Location | Frequency, No. (%) |
|---|---|
| Home | 2654 (51.8) |
| Public places (excluding streets) | 528 (10.3) |
| Streets | 154 (3) |
| Residential care homes for the elderly | 1564 (30.6) |
| En route to hospital | 219 (4.3) |
OHCAs indicates out‐of‐hospital cardiac arrests.
Table 3 shows the spatial relationship between the AED identified during the study period and the historical cases of OHCA. The results given by straight line–based and walking route–based calculation are different. If calculated by the walking route–based model, the coverage rate is one third of those calculated by the straight line–based model, while the average distance is more than double of the latter. Histograms of the straight line and walking route distances (Figure 1) and scatterplots of one distance versus the other, indicating the regions where either metric indicates being >100 meters from the nearest AED unit, are also given (Figure 2).
Table 3.
Spatial Relationship of Existing AED and OHCA
| Straight Line–Based Model | Walking Route–Based Model | |
|---|---|---|
| OHCAs within 100 m of an AED, No. | 1544 | 574 |
| Coverage rate, % | 30.04 | 11.17 |
| Average distance, mean±SD, m | 230.8±360.8 | 545.3±727.8 |
AED indicates automated external defibrillator; OHCA, out‐of‐hospital cardiac arrest.
Figure 1.
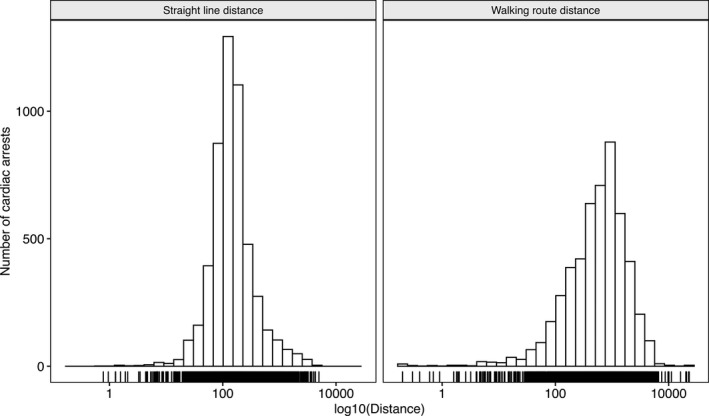
Histograms showing the distribution of the historical out‐of‐hospital cardiac arrests with reference to an automated external defibrillator as calculated by the straight line–based model (left) and walking route–based model (right).
Figure 2.
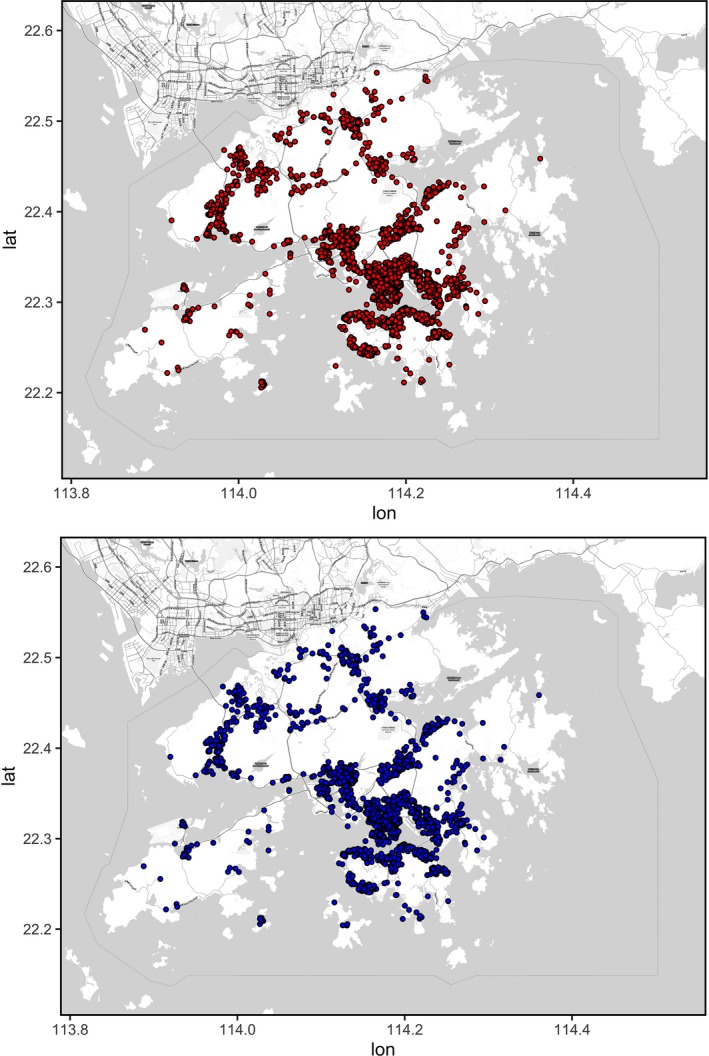
Scatterplots of one distance vs the other, indicating the regions where either metric indicates being >100 meters (upper: by straight line–based calculation; lower: by walking route–based calculation) from the nearest automated external defibrillator.
Discussion
Different geographic tools and mathematical models have been used to describe or optimize AED deployment. For example, hotspot plot can identify the locations with insufficient AEDs in a small space. A weakness of this kind of plot is lack of objectivity. In a crowded urban city center, it is impossible to differentiate patients located in or out of range of an AED from a plot (Figure 3). Other tools or models have relied on the calculation of the average distance or coverage rate by measuring the straight line distance between an OHCA and an AED.5, 6 As shown in this study, however, straight line–based calculations may be inherently inaccurate.
Figure 3.
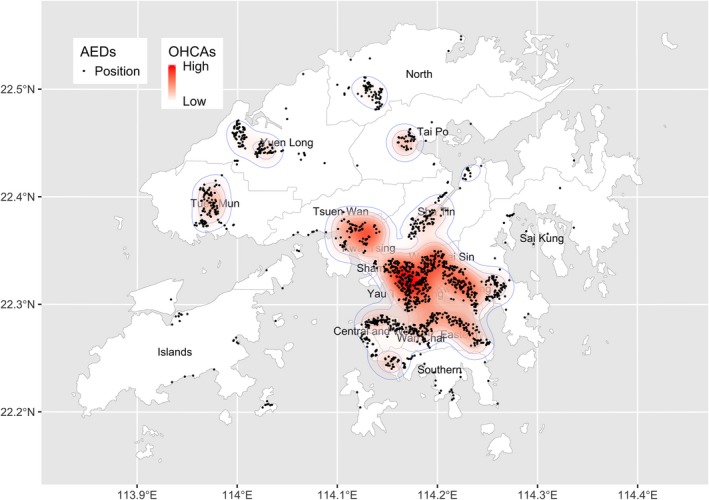
Hotspot map by kernel‐density estimation of out‐of‐hospital cardiac arrests (OHCAs) and the locations of automated external defibrillators (AEDs) of Hong Kong.
Time to defibrillation is a known predictor of survival in cases of OHCA. The calculation of the distance a bystander has to travel to get to an AED should be as precise as possible. Miscalculation may unnecessarily influence the judgement of policy makers. However, this study has shown that there is significant difference in the results of the spatial relationship of AEDs and OHCA between straight line–based and walking route–based calculation. The walking route distance should be closer to the actual distance between an OHCA and an AED in an urban setting. Using the straight line–based model would overestimate the coverage rate and underestimate the average distance between an OHCA and the closest AED. This is obviously because the straight line–based model does not take into account the obstacles between the OHCA and the AED in an urban setting. It is therefore recommended that deployment of AEDs in urban settings should be based on the walking route–based model.
Study Limitations
There are several limitations in this study. Because of the lack of compulsory registration of AEDs in Hong Kong, the list of AEDs recruited in this study may be incomplete. Further, the use of the AED found in this study might be limited by temporal inaccessibility.7 This is because not all AEDs were 24/7 accessible. As a result, the coverage rate may be hampered and it would adversely affect the timeliness of AED application on a patient with OHCA. The distances calculated by both models were on a horizontal level. In urban cities such as Hong Kong, multistory buildings dominate. The distance between an OHCA and the nearest AED may be underestimated if either the AED or an OHCA occurs in a high‐rise building. In fact, studies have shown that patients with an OHCA that occurs in high‐rise buildings might experience delays in emergency medical service response. This would, in turn, undermine their probability of survival.14, 15 In future studies of AED deployment, incorporation of vertical distances in the calculation is recommended. Historical cases of OHCA were used in the calculation in this study. In theory, the location of an OHCA is unpredictable. The results of calculation on a different set of OHCAs may show diverse findings.
Conclusions
The widely used straight line–based calculation of the spatial relationship of AED and OHCA may be inaccurate. A walking route–based model is recommended for studies of optimization of AED deployment.
Disclosures
None.
(J Am Heart Assoc. 2020;9:e014398 DOI: 10.1161/JAHA.119.014398.)
References
- 1. Weisfeldt ML, Kerber RE, McGoldrick RP, Moss AJ, Nichol G, Ornato JP, Palmer DG, Riegel B, Smith SC Jr. Public access defibrillation. A statement for healthcare professionals from the American Heart Association Task Force on Automatic External Defibrillation. Circulation. 1995;92:2763. [DOI] [PubMed] [Google Scholar]
- 2. Gratton M, Lindholm DJ, Campbell JP. Public‐access defibrillation: where do we place the AEDs? Prehosp Emerg Care. 1999;3:303–305. [DOI] [PubMed] [Google Scholar]
- 3. Folke F, Lippert FK, Nielsen SL, Gislason GH, Hansen ML, Schramm TK, Sørensen R, Fosbøl EL, Andersen SS, Rasmussen S, Køber L, Torp‐Pedersen C. Location of cardiac arrest in a city center: strategic placement of automated external defibrillators in public locations. Circulation. 2009;120:510–517. [DOI] [PubMed] [Google Scholar]
- 4. Mao RD, Ong ME. Public access defibrillation: improving accessibility and outcomes. Br Med Bull. 2016;118:25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chan TC, Li H, Lebovic G, Tang SK, Chan JY, Cheng HC, Morrison LJ, Brooks SC. Identifying locations for public access defibrillators using mathematical optimization. Circulation. 2013;127:1801–1809. [DOI] [PubMed] [Google Scholar]
- 6. Hansen CM, Lippert FK, Wissenberg M, Weeke P, Zinckernagel L, Ruwald MH, Karlsson L, Gislason GH, Nielsen SL, Køber L, Torp‐Pedersen C, Folke F. Temporal trends in coverage of historical cardiac arrests using a volunteer‐based network of automated external defibrillators accessible to laypersons and emergency dispatch centers. Circulation. 2014;130:1859–1867. [DOI] [PubMed] [Google Scholar]
- 7. Sun CL, Demirtas D, Brooks SC, Morrison LJ, Chan TC. Overcoming spatial and temporal barriers to public access defibrillators via optimization. J Am Coll Cardiol. 2016;68:836–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Huang CY, Wen TH. Optimal installation locations for automated external defibrillators in Taipei 7‐Eleven stores: using GIS and a genetic algorithm with a new stirring operator. Comput Math Methods Med. 2014;2014:241435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tierney NJ, Reinhold HJ, Mira A, Weiser M, Burkart R, Benvenuti C, Auricchio A. Novel relocation methods for automatic external defibrillator improve out‐of‐hospital cardiac arrest coverage under limited resources. Resuscitation. 2018;125:83–89. [DOI] [PubMed] [Google Scholar]
- 10. Bryan BD. Optimal placement of public‐access AEDs in urban environments. Comput Ind Eng. 2015;90:269–280. [Google Scholar]
- 11. Fan KL, Leung LP, Siu YC. Out‐of‐hospital cardiac arrest in Hong Kong: a territory‐wide study. Hong Kong Med J. 2017;23:48–53. [DOI] [PubMed] [Google Scholar]
- 12. The Jockey Club ‘Heart‐Safe School’ Project. Hong Kong: Hong Kong College of Cardiology; 2012. Available at: http://www.heartsafeschool.org.hk/eng/plan.aspx. Accessed April 2, 2019. [Google Scholar]
- 13. Luxen D, Vetter C. Real‐time routing with open street map data. Proceedings of the 19th ACM SIGSPATIAL International Conference on Advances in Geographic Information Systems; Chicago, IL. 2094062: ACM, 513‐516 (2011).
- 14. Morrison LJ, Angelini MP, Vermeulen MJ, Schwartz B. Measuring the EMS patient access time interval and the impact of responding to high‐rise buildings. Prehosp Emerg Care. 2005;9:14–18. [DOI] [PubMed] [Google Scholar]
- 15. Drennan IR, Strum RP, Byers A, Buick JE, Lin S, Cheskes S, Hu S, Morrison LJ. Out‐of‐hospital cardiac arrest in high‐rise buildings: delays to patient care and effect on survival. CMAJ. 2016;188:413–419. [DOI] [PMC free article] [PubMed] [Google Scholar]


