Abstract
Background
Left atrial (LA) size and cardiorespiratory fitness (CRF) are predictors of future cardiovascular events in high‐risk populations. LA dilatation is a diagnostic criterion for left ventricular diastolic dysfunction. However, LA is dilated in endurance athletes with high CRF, but little is known about the association between CRF and LA size in healthy, free‐living individuals. We hypothesized that in a healthy population, LA size was associated with CRF and leisure‐time physical activity, but not with echocardiographic indexes of left ventricular diastolic dysfunction.
Methods and Results
In this cross‐sectional study from HUNT (Nord‐Trøndelag Health Study), 107 men and 138 women, aged 20 to 82 years, without hypertension, cardiovascular, pulmonary, or malignant disease participated. LA volume was assessed by echocardiography and indexed to body surface area LAVI (left atrial volume index). CRF was measured as peak oxygen uptake (VO 2peak) using ergospirometry, and percent of age‐ and‐sex‐predicted VO 2peak was calculated. Indexes of left ventricular diastolic dysfunction were assessed in accordance with latest recommendations. LAVI was >34 mL/m2 in 39% of participants, and LAVI was positively associated with VO 2peak and percentage of age‐ and‐sex‐predicted VO 2peak (β [95% CI], 0.11 [0.06–0.16] and 0.18 [0.09–0.28], respectively) and weighted minutes of physical activity per week (β [95% CI], 0.01 [0.003–0.015]). LAVI was not associated with other indexes of left ventricular diastolic dysfunction. There was an effect modification between age and VO 2peak/percentage of age‐ and‐sex‐predicted VO 2peak showing higher LAVI with advanced age and higher VO 2peak/percentage of age‐ and‐sex‐predicted VO 2peak as presented in prediction diagrams.
Conclusions
Interpretation of LAVI as a marker of diastolic dysfunction should be done in relation to age‐relative CRF. Studies on the prognostic value of LAVI in fit subpopulations are needed.
Keywords: echocardiography, endurance training, exercise, heart, physical activity
Subject Categories: Echocardiography, Exercise Testing, Exercise, Epidemiology, Physiology
Clinical Perspective
What Is New?
In previously healthy men and women participating in the HUNT (Nord‐Trøndelag Health Study), left atrial size was positively associated with higher cardiorespiratory fitness, but not with indexes of left ventricular diastolic dysfunction.
The association between cardiorespiratory fitness and left atrial enlargement was stronger with higher age.
What Are the Clinical Implications?
Cardiorespiratory fitness should be considered when left atrial size is included in clinical decision making.
Introduction
Left atrial (LA) volume is established as a strong prognostic marker of future cardiovascular events in high‐risk populations.1, 2, 3 The strong association between LA volume and left ventricular (LV) diastolic dysfunction4, 5 has resulted in LA volume becoming one of the diagnostic criteria for LV diastolic dysfunction, with a cutoff of 34 mL/m2 defining pathological enlargement.6
Contrary to this, LA enlargement is often observed among endurance athletes,7 in whom it is regarded a physiological adaptation.8 Similarly, LA enlargement has been observed in recreational runners,9 and higher lifetime training hours in nonelite athletes are linked to LA enlargement.10 LV diastolic dysfunction, however, is associated with low cardiorespiratory fitness (CRF)11; and low CRF has a well‐established link to mortality.12 Thus, enlarged LA in both patients with cardiac disease and endurance athletes represents a paradox as these are populations with different prognoses.
Although LA size has been studied thoroughly in athletes and patients with cardiac diseases, studies from healthy populations, and particularly studies on the associations between CRF and LA size in general free‐living populations, are scarce. Furthermore, as many patients examined by echocardiography do not have a well‐defined medical and cardiac history, a universal threshold of 34 mL/m2 defining LA enlargement may be unfavorable. Still, the current recommendations for assessment of LA volume and diastolic function only include a short precaution about the interpretation of LA volume in athletes.6, 13 However, it is likely that one should be cautious also when assessing LAVI and diastolic function in nonathlete subjects with high CRF and/or a long exercise training history. To avoid misinterpretation of normal LA as pathologically enlarged with following misdiagnosis, overtreatment, and unnecessary worry for patients, knowledge on the association between LA size, CRF, and diastolic function in healthy, free‐living, nonathletic subjects is needed.
Therefore, we aimed to investigate the association of LA volume with CRF and LV diastolic function in a healthy, free‐living population. Second, to better allow for generalization of the results to populations in whom measurements of CRF are not available, we aimed to assess the association of LA volume with leisure‐time physical activity (PA). We hypothesized that in a healthy, free‐living population, LA volume is associated with CRF and leisure‐time PA, but not with echocardiographic indexes of LV diastolic dysfunction.
Methods
The data from HUNT (Nord‐Trøndelag Health Study) used in this study are available on application to the HUNT Data Access Committee in accordance with the policy on data availability (further information and contact information: https://www.ntnu.edu/hunt/data).
Study Population
The subjects of this cross‐sectional study participated in the third wave of HUNT (HUNT3). HUNT3 was performed between October 2006 and June 2008, and all inhabitants of the county, aged ≥20 years, were invited, with 50 821 individuals (54%) participating. HUNT has been comprehensively described elsewhere.14 Subjects free from hypertension or use of hypertensive medications, pulmonary or cardiovascular disease, cancer, and sarcoidosis were invited to cardiopulmonary exercise testing as a part of the HUNT3 Fitness study, a substudy of HUNT3. The HUNT3 Echocardiography study15 was another substudy with similar inclusion criteria as the HUNT3 Fitness study, and 242 participants contributing in both the HUNT3 Echocardiography study and the HUNT3 Fitness study compose the population in this study. Data collection took place from June 9 to 19, 2008, in the town of Namsos, Norway.
Previously unknown minor pathological features were revealed in 6 study participants, including possible history of angina pectoris (n=2), aortic regurgitation (n=1), LV hypertrophy (n=2), and other (n=1). These individuals were not excluded from the analyses.
The study was approved by the Regional Committee for Medical Research Ethics (2018/929) and conducted according to the second Declaration of Helsinki. Informed consent was obtained from all participants. The study participants could withdraw from the study at any time.
Self‐Reported Questionnaires and Clinical Measurements
Questionnaires on medical history, clinical examinations, and blood sampling for biochemical analyses were performed in the HUNT3 baseline examination, and detailed information on the sampling of these data has been reported earlier.14 Information on PA (frequency, duration, and intensity of leisure‐time PA) was gathered from validated questionnaires.16 PA was then calculated as volume of moderate‐to‐vigorous PA per week (PA volume), where relative vigorous intensity PA was weighted double in accordance with current recommendations.17 Information on PA intensity was given on the scale of rated perceived exertion, ranging from 6 (no exertion at all) to 20 (maximal exertion). Rated perceived exertion 12 and 13 were graded as moderate intensity, and rated perceived exertion >13 was graded as vigorous intensity. PA was also classified as adherence or nonadherence to PA guidelines17 on the basis of these calculations of minutes of PA per week.
Echocardiography
Transthoracic echocardiograms were recorded by one physician (H.D.) highly experienced in echocardiography. Participants were examined in the left‐lateral decubitus position using a Vivid 7 scanner with a phased‐array transducer (M3S and M4S) (version BT06; GE Ultrasound, Horten, Norway). All measurements were averaged over 3 cardiac cycles. Echocardiographic data were stored digitally and analyzed subsequently by the same physician echocardiographer.
For quantification of LA volume‐specific views, the LA was recorded from apical 4‐ and 2‐chamber views in end systole with tracing of the endocardial border (Figure 1).13 Mean difference between 4‐ and 2‐chamber length was 0.36 cm (SD, 0.28 cm). LA volume was calculated by the area‐length (A‐L) method and by the summation of disc method, and subsequently indexed per square meter body surface area LAVI (left atrial volume index). Mitral inflow peak early (E) and late velocity and early filling mitral deceleration time were assessed from apical 4‐chamber view by pulsed‐wave Doppler. Peak velocity tricuspid regurgitation was measured by continuous Doppler. Mitral annular peak systolic and peak early diastolic (e’) longitudinal velocities were assessed by pulsed‐wave tissue Doppler. The ratio of the early mitral inflow/the early diastolic mitral annular velocity (E/e’) was calculated.
Figure 1.
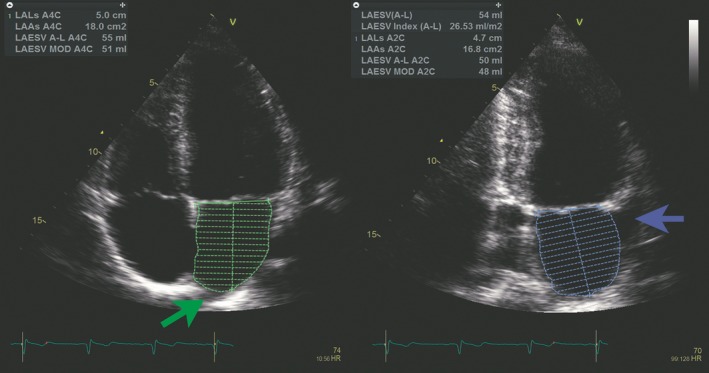
Left atrial (LA) assessment. LA volume was measured from B‐mode recordings in apical 4‐chamber view (left) and 2‐chamber view (right). Tracing was done from one side at the mitral annular level following the endocardial border around the atrium and to the opposite site at the mitral annular level. The contour was closed at the mitral annulus with a straight line. The area of the atria in the specific view is annotated LAAs in the figure. Pulmonary veins (green arrow) and LA appendage (blue arrow) were excluded from the tracings. LA length was measured in both views, illustrated by the central line in the 2 tracings (annotated as LALs in the figure). LA volume was measured by the area‐length method (annotated as LAESV A‐L in the figure) and the summation of disks method (annotated as LAESV MOD in the figure).13
Assessment of diastolic function was based on latest recommendations.6 The following parameters and corresponding cutoffs were used; mitral annular e’ (septal e’ <7 cm/s, lateral e’ <10 cm/s), E/e’ ratio >14, LAVI >34 mL/m2, and peak tricuspid regurgitation velocity >2.8 m/s. LV diastolic dysfunction was present if more than half of the available parameters met these cutoff criteria.
Data on the reliability of most of the measurements have been comprehensively described previously.15 Reproducibility for LAVI was calculated in a random subset of 145 study participants by separate analyses performed by 2 physicians experienced in echocardiography (H.D. and H.E.M‐H.). Shortly, coefficient of variation for LAVI was 12.1%, and the test‐retest coefficients of variation for separate echocardiographic data sets for E, e’ (average of septal and lateral), and E/e’ were 6.0%, 10.5%, and 7.9%, respectively.15
Cardiorespiratory Fitness
Peak oxygen uptake (VO2peak) was measured by ergospirometry during walking or running on a treadmill using an individualized protocol to voluntary exhaustion while wearing a tight face mask (Hans Rudolph, Germany) connected to a portable mixing chamber gas‐analysis system (MetaMax II; Cortex, Leipzig, Germany). Reliability of the cardiopulmonary exercise testing measurements has been published previously.18 Test‐retest correlation of oxygen uptake was 0.99 (P<0.001), and the coefficient of variation was 1.8%.
Statistical Analyses
VO2peak is expressed in milliliters of oxygen consumed per kg body weight per minute and as percentage of predicted from age and sex (VO2%pred). Age‐ and sex‐predicted VO2peak was calculated by previously published sex‐specific regression equations of age (men: VO2peak=63.6–0.393×age; women: VO2peak=55.6–0.328×age)19 based on a larger sample of the HUNT Fitness study.18 VO2%pred was calculated by dividing measured VO2peak by predicted VO2peak and multiplying by 100. We included VO2peak and VO2%pred in a multiple regression model in addition to other echocardiographic variables shown to be independent predictors of LAVI10, 20 to assess if CRF improved prediction. Furthermore, linear regression was used to assess associations between LAVI and VO2peak, VO2%pred, PA volume, and age. We tested between‐group differences of LAVI for sexes and for adherence or nonadherence to PA guidelines using an ANCOVA. We used multiple regression to predict LAVI on the basis of VO2peak and VO2%pred, age, and sex, and explored for statistical interaction. The Akaike information criterion was used to assess model performance. The resulting regression models were used to predict LAVI on the basis of the mentioned variables. Linear regression was also performed to assess associations between LAVI and other echocardiographic indexes of diastolic function, as well as between VO2peak/VO2%pred and diastolic function indexes. Sensitivity analyses were performed with exclusion of measurements from those with 1‐plane LAVI measurements only and for those with difference between 4‐ and 2‐chamber atrial length of >0.5 cm. P<0.05 was considered statistically significant, and P values and CIs are based on robust SEs. Analyses were conducted using R Studio Version 1.2.1335 (R Foundation for Statistical Computing, Vienna, Austria) and STATA 15.1 (StataCorp, TX).
Results
General characteristics of participants are presented in Table 1 and demonstrate the low cardiovascular risk profile of the population, as well as the normal profile of echocardiographic parameters of LV structure and systolic function. VO2peak was 10% lower than predicted by age and sex, and adherence to PA guidelines was high (40.3%). Echocardiographic LV diastolic function indexes are shown in Table 2. By the A‐L method, LAVI was a mean of 32.6 mL/m2 (SD, 6.7 mL/m2), and 39% of participants had LAVI above the cutoff of 34 mL/m2. Three participants (1.2%) met criteria of diastolic dysfunction. Men had significantly higher LAVI compared with women (mean difference, 2.9 [95% CI, 1.1–4.6] mL/m2; P=0.001), but not after adjusting for VO2peak (mean difference, 1.4 [95% CI, −0.6 to 3.4] mL/m2; P=0.17). VO2peak independently predicted LAVI in a multiple regression model including LV mass index, LV end‐diastolic volume, E/e’, sex, and age (model: R 2=0.16, P<0.0001; VO2peak β=0.16 [95% CI, 0.04–0.28], P=0.02).
Table 1.
Baseline Characteristics of the 242 Participants by Sex
| Characteristics | Men | Women | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Clinical characteristics | ||||
| n | 107 | … | 135 | … |
| Age, y | 49 | 13 | 48 | 14 |
| Waist circumference, cm | 93 | 8 | 87 | 10 |
| Waist/hip ratio | 0.91 | 0.05 | 0.86 | 0.07 |
| Weight, kg | 85 | 11 | 71 | 12 |
| BMI, kg/m2 | 26.4 | 3.1 | 25.6 | 3.9 |
| Body surface area, m2 | 2.05 | 0.14 | 1.79 | 0.14 |
| Systolic BP, mm Hg | 129 | 13 | 122 | 15 |
| Diastolic BP, mm Hg | 76 | 9 | 70 | 10 |
| Resting HR, bpm | 66 | 10 | 69 | 10 |
| Current smoker, % | 21.7 | … | 19.2 | … |
| Physical activity adherence, % | 43.7 | … | 40.3 | … |
| Total cholesterol, mmol/L | 5.5 | 0.9 | 5.4 | 1.1 |
| HDL cholesterol, mmol/L | 1.3 | 0.3 | 1.5 | 0.3 |
| Glucose, mmol/L | 5.6 | 1.1 | 5.2 | 0.8 |
| Cardiopulmonary exercise testing variables | ||||
| Peak oxygen uptake, mL/kg per min | 43.8 | 7. 7 | 33.3 | 7.0 |
| VO2%pred | 99 | 18 | 83 | 14 |
| Peak RER | 1.14 | 0.07 | 1.13 | 0.07 |
| Peak HR, bpm | 181 | 13 | 181 | 14 |
| General echocardiographic indexes | ||||
| LV end‐diastolic volume, mL | 110 | 22 | 85 | 18 |
| LV end‐diastolic diameter, mm | 52 | 5 | 49 | 5 |
| LV ejection fraction, % | 57 | 6 | 58 | 6 |
| Mitral annular S’, cm/s | 8.6 | 1.4 | 8.2 | 1.4 |
| TAPSE, cm | 2.9 | 0.5 | 2.8 | 0.4 |
| Tricuspid annular S’, cm/s | 13.1 | 2.2 | 12.8 | 2.1 |
| Global longitudinal LV end‐systolic strain, % | −17.1 | 2.1 | −18.5 | 2.1 |
BMI indicates body mass index; BP, blood pressure; bpm, beats per minute; HDL, high‐density lipoprotein; HR, heart rate; LV, left ventricular; RER, respiratory exchange ratio; S’, peak mitral annular systolic velocity (by pulsed‐wave tissue Doppler); TAPSE, tricuspid annular plane systolic excursion; VO2%pred, percentage of age‐ and sex‐predicted peak oxygen uptake.
Table 2.
Echocardiographic Indexes of LV Diastolic Function by Sex
| Variables | Men | Women | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| LAESV index (A‐L), mL/m2 | 34.2 | 7.1 | 31.3 | 6.1 |
| LAESV index (MOD), mL/m2 | 31.2 | 6.5 | 28.2 | 5.6 |
| Mitral E‐wave, cm/s | 67 | 16 | 72 | 16 |
| Mitral A‐wave, cm/s | 50 | 16 | 56 | 18 |
| Mitral E/A | 1.5 | 0.5 | 1.4 | 0.6 |
| Mitral E/e’ | 6.4 | 2.2 | 6.5 | 2.0 |
| Lateral e’, cm/s | 12.5 | 3.5 | 13.2 | 3.6 |
| Septal e’, cm/s | 9.6 | 2.6 | 10.1 | 2.9 |
| Mitral deceleration time, ms | 214 | 69 | 208 | 68 |
| Pulmonary vein S, cm/s | 55 | 12 | 61 | 12 |
| Pulmonary vein D, cm/s | 50 | 12 | 49 | 12 |
| Pulmonary vein S/D ratio | 1.2 | 0.4 | 1.3 | 0.3 |
| TRV maximum, m/s | 2.3 | 0.3 | 2.3 | 0.4 |
A indicates late diastolic (atrial) mitral inflow; A‐L, area‐length; D, peak diastolic velocity; E, early diastolic mitral inflow; e’, peak early diastolic mitral annular velocity; LAESV, left atrial end‐systolic volume; LV, left ventricular; MOD, summation of disc method; S, peak systolic velocity; TRV, tricuspid regurgitant velocity.
CRF and LA Volume
Figure 2 shows the positive correlation of LAVI with VO2%pred, and Table 3 shows the positive association with VO2peak and PA volume as well. Participants adhering to PA guidelines had borderline significantly higher LAVI (age‐ and sex‐adjusted mean difference, 1.7 [95% CI, −0.1 to 3.5]; P=0.06). In multiple regression analyses, introducing an interaction term between age and VO2peak/VO2%pred improved the predictions, but other or higher‐order interaction terms did not. VO2peak, age, and the interaction of age and VO2peak predicted LAVI (model 1: LAVI~VO2peak+Age+VO2peak×Age, P<0.0001, R 2=0.09). The linear regression with VO2%pred, age, sex, and the interaction of age and VO2%pred (model 2: LAVI~VO2%pred+Age+VO2%pred×Age+Sex, P<0.0001, R 2=0.10) performed similarly. Sex did not contribute significantly in the prediction equation with VO2peak. The resulting regression equations were used to predict LAVI on the basis of age and VO2peak/VO2%pred. In sex‐specific models, the same model 2 (omitting the sex term) had the lowest Akaike information criterion for men (P<0.002; R 2=0.11), whereas none of the tested models for women significantly predicted LAVI (a model with splines for VO2peak at 25, 35, and 45 mL/kg had the lowest Akaike information criterion; R 2=0.06; P=0.06). The higher predicted LAVI with advanced age and higher VO2peak/VO2%pred is presented in Figure 3A and 3B, as well as the male‐only VO2%pred model in Figure 3C. Predicted LAVI by VO2%pred with associated 95% CIs and 95% prediction intervals by sex for age 40 and 70 years is shown in Figure S1.
Figure 2.
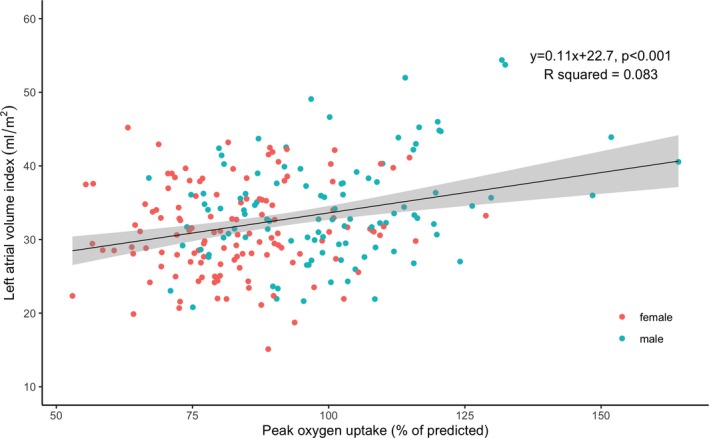
Scatterplot of the relationship between left atrial volume index (mL/m2) and percentage of age‐ and sex‐predicted peak oxygen uptake (n=229).
Table 3.
Linear Regression Analyses With LA Volume Index (A‐L Method) as Dependent Variable
| Variable | n | Univariate Model | Age‐ and Sex‐Adjusted Model | ||||
|---|---|---|---|---|---|---|---|
| β (95% CI) | R 2 | P Value | β (95% CI) | R 2 | P Value | ||
| VO2peak | 229 | 0.18 (0.09–0.28) | 0.06 | <0.001 | 0.20 (0.08–0.33) | 0.07 | 0.002 |
| VO2%pred | 229 | 0.11 (0.06–0.16) | 0.08 | <0.001 | 0.09 (0.04–0.14) | 0.08 | 0.001 |
| PA volume | 225 | 0.01 (0.003–0.015) | 0.04 | 0.006 | 0.009 (0.003–0.015) | 0.08 | 0.005 |
| Age | 229 | 0.03 (−0.03 to 0.01) | 0.004 | 0.34 | N/A | N/A | N/A |
A‐L indicates area‐length; LA, left atrial; PA volume, minutes of physical activity per week with high‐intensity activity weighted 2:1; VO2%pred, percentage of age‐ and sex‐predicted VO2peak; VO2peak, peak oxygen consumption; N/A, not applicable.
Figure 3.
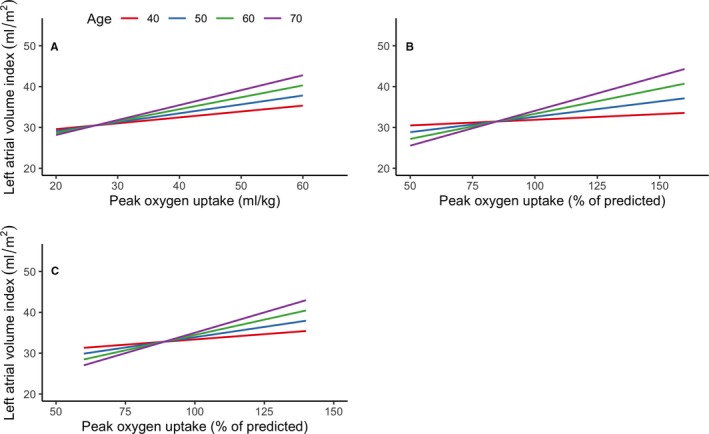
Prediction diagrams of left atrial volume index for ages 40, 50, 60, and 70 years by peak oxygen uptake (VO2peak) (n=229) (A), percentage of age‐ and sex‐predicted VO 2peak (n=229) (B), and percentage of age‐ and sex‐predicted VO 2peak in men only (n=103) (C).
Diastolic Function
There were no statistically significant associations between LAVI and e’, E/e’, and tricuspid regurgitation (Table S1) as well as other indexes of diastolic dysfunction (pulmonary vein systolic and diastolic velocities and their ratio, transmitral flow early and late velocities and their ratio, and mitral deceleration time; data not shown). Septal e’ showed a positive association to VO2%pred, but no other association was found in age‐ and sex‐adjusted multiple regression analyses with echocardiographic indexes of diastolic function as dependent variable and VO2peak and VO2%pred as independent variables (Table S2).
Sensitivity Analyses
Excluding those with only single‐plane measurement of LAVI, those with >0.5‐cm difference between 2‐ and 4‐chamber measurements, and those with diastolic dysfunction (n=3), did not make notable changes to the main results. LAVI was systematically lower when measured by the biplane method of discs compared with the A‐L method (LAVI [summation of disc method] mean, 29.5 mL/m2; mean difference, 3.3 [95% CI, 3.1–3.5] mL/m2; P<0.0001; n=209), and 22% had LAVI >34 mL/m2 when measured by the summation of disc method. Predicted LAVI based on model 1 and model 2 was therefore also lower, and higher VO2peak/VO2%pred was needed to reach thresholds for enlarged LAVI (Figure S2). The same effect modification between VO2peak/VO2%pred and age was seen when using LAVI measured by the biplane method of discs.
Using a different approach fitting a restricted cubic spline model for the prediction of LAVI by VO2%pred showed similar results as model 2 (Data S1, Figure S3). Allowing for different β coefficients at different levels of VO2%pred, this model showed an effect on LAVI when VO2%pred was >100%.
We also fitted spline models allowing different β coefficients at different ages, with similar findings as in the main models (Data S1, Figure S4).
Discussion
Our main finding is that higher CRF is associated with higher LAVI in a healthy, free‐living general population sample, and the effect is modified by age. In fact, participants aged ≥60 years with VO2peak as expected by age and sex were predicted to have LAVI at the threshold for pathological enlargement of 34 mL/m2 (A‐L method). Higher LAVI was not associated with other indexes of diastolic dysfunction. The main findings are summarized in Figure 4.
Figure 4.
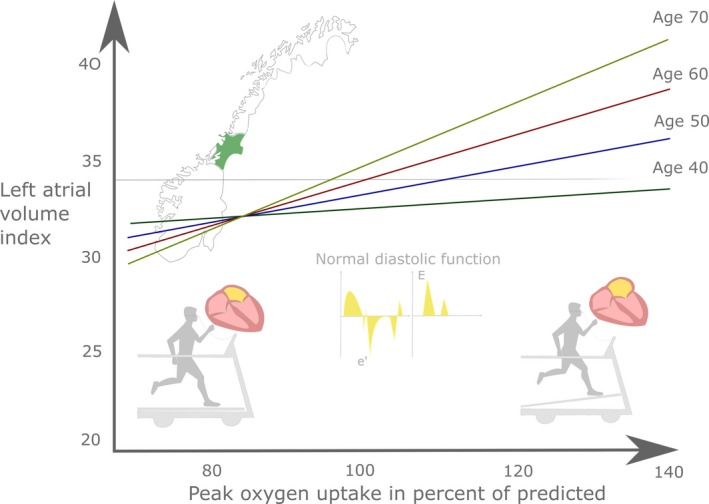
Take‐home figure. Indexed left atrial volume was positively associated with cardiorespiratory fitness in healthy adults, and the effect was more pronounced with advanced age. Left atrial volume was not associated with other indexes of left ventricular diastolic dysfunction.
CRF, Diastolic Function, and LA Size
Although evidence on the associations between LAVI and CRF in healthy populations is lacking, the main finding from this study is supported by studies showing enlarged LAVI in competitive endurance athletes7, 8 and recreational runners.9 Authors from a study comparing athletes and normal subjects argued that LAVI appears to be determined by a complex interplay between LV end‐diastolic volume, PA level, and LV mass.20 Sex was not an independent predictor in the latter study, which is in line with our results showing that LAVI was not different between sexes after adjusting for VO2peak, a proxy of LV size. An interventional study randomizing adults to high‐intensity exercise or yoga control showed that LA volume increased significantly more in the high‐intensity exercise group,21 although another study based on the same exercise intervention showed that LA mechanical remodeling was more prominent than LV mechanical remodeling in the high‐intensity exercise group.22
A modest proportion of the LAVI variance was explained by the VO2peak/VO2%pred models. However, the mean VO2%pred of the study population was 10% lower than expected by age and sex, and few subjects had high VO2%pred values, especially in women. In fact, only 16% of women had VO2%pred higher than expected by age and sex, compared with 47% of the men. It is likely that this contributed largely to the lack of significant associations between LAVI and VO2peak/VO2%pred in women. The differences by sex for the association between CRF and LAVI should be investigated further.
Higher LAVI was not associated with diastolic dysfunction in our study, which is supported by a study from a US preventive health clinic showing that the association between LAVI and LV diastolic filling pressures measured by E/e’ differs by CRF level.11 Another study also showed that E/e’ was associated with LAVI among normal subjects, but not among athletes.20 In patients with LV diastolic dysfunction, low CRF is associated with enlarged LAVI,23 and therefore it seems to be a U‐ (or at least J‐) shaped relationship between LAVI and CRF, where enlarged LAVI and low CRF are associated with diastolic dysfunction and a poor prognosis, whereas enlarged LAVI and high CRF probably are associated with a favorable prognosis. Higher prognostic value of diastolic dysfunction compared with enlarged LAVI has been shown in a study from the general population,24 supporting that enlarged LAVI may convey other information than just as a marker of chronically elevated filling pressures.
The negative prognostic influence of LAVI is shown in high‐risk populations, such as patients with type 2 diabetes mellitus and myocardial infarction.1, 2 However, longitudinal studies on the prognostic value of enlarged LAVI in fit populations are lacking, which should be evaluated in future studies. An interventional study did show LA mechanical remodeling in response to high‐intensity exercise without significant electrical remodeling,22 further supporting this notion.
A study investigating exercise capacity and LAVI in normal and diseased subjects showed that exercise capacity was negatively correlated to LAVI in systolic and diastolic dysfunction, but positively correlated to LAVI in normal subjects, supporting our findings,25 as the population in our study was previously healthy.
It is likely that the physiological high blood flow obtained during PA may trigger LA remodeling in fit individuals in a similar way as the high‐pressure states found in relation to LV pathological features. The number of years of endurance exercise training has been shown to be an independent predictor of enlarged LAVI in athletes,10 which is supportive of our finding of an effect modification between age and CRF on LAVI showing higher predicted LAVI by CRF with advanced age. Cumulative PA volume over years may therefore be an important stimulus to enlarged LAVI in healthy subjects from the general population as well. Animal models showing increased LA fibrosis in response to exercise training further support the possibility of cumulative, and possibly irreversible, changes to the LA over time.26 Although data on cumulative PA over many years were not available in our study, it may be argued that LA enlargement caused by this stimulus may be less harmful as PA behavior generally is associated with lower cardiovascular risk. Thus, it may be hypothesized that LAVI is not a good marker of risk in a healthy and fit population.
Clinical Implications
Our study indicates that CRF should be considered when assessing LAVI, and as previously discussed it may be argued that LAVI is not a marker of risk in healthy and fit subpopulations. As Nistri et al previously stated,20 a dichotomous classification of normal/pathological LAVI without taking variables such as athletic status into account increases risk of misclassification, further suggesting that specific cutoffs based on sporting activity should be proposed. Our study supports these findings and further implies that CRF or exercise training status should be considered when assessing LAVI also in nonathletes. Our findings indicate that making such precautions is especially important among fit individuals of advanced age. In fact, one metabolic equivalent task (metabolic equivalent task=3.5 mL/kg per minute) higher VO2peak translated to ≈1.3 mL higher predicted LAVI in 70‐year‐old patients in our study. Our results also suggest that briefly assessing patients’ leisure‐time PA could help clinicians in interpreting findings of enlarged LAVI. Another alternative to the somewhat resource‐demanding ergospirometry is estimating CRF through nonexercise equations, which could be a feasible alternative in clinical practice.12, 19
Strengths and Limitations
The study has several methodological strengths. CRF was measured by ergospirometry during incremental symptom‐limiting exercise, dedicated echocardiographic recordings were obtained to assess LA volume, and leisure‐time PA was measured by a validated questionnaire.
Although mean VO2peak values were lower in our study population than in the reference population, CRF reference values from Norwegian populations in general are somewhat higher than in other populations.27 Given the relationship between LAVI and CRF found in this study, this may partly explain the high LAVI values found in this study compared with a recent meta‐analysis.28 Another potentially important cause may be the inclusion of LAVI from studies assessing LAVI on the basis of one view only, and the meta‐analyses did not take difference in length between 4‐ and 2‐chamber view into account. The discrepancy between the recommendations, the large meta‐analyses, and the present results reflects the need for high‐quality echocardiographic studies from different populations. The A‐L method for LA volume evaluation is known to yield higher values for LAVI compared with the summation of disc method, and the discrepancy in our material was similar to what was expected.29 However, sensitivity analyses showed the same associations to CRF regardless of method of LAVI quantification.
The cross‐sectional design limits conclusions about causation, and the selection of healthy individuals made echocardiographic diastolic dysfunction practically absent. Furthermore, we did not follow specific guidelines for examination of diastolic dysfunction when ejection fraction was reduced,6 as the number of participants with reduced ejection fraction was negligible. Data on fat‐free body mass were not available, and it is reasonable that fit individuals have a lower proportion of body fat that may influence the indexed LA volume. Obesity may also affect LAVI30; and although it is strongly related to CRF, it is possible that the presented associations could be different in populations of different body composition. As all participants were in sinus rhythm, the results should not be generalized to individuals with arrhythmias. However, although the participants answered to be free of any cardiovascular disease, it is possible that some participants may have had undiagnosed asymptomatic paroxysmal atrial fibrillation. This is especially important as previous studies have shown increased atrial fibrillation prevalence in populations with a long history of endurance exercise training,31 and atrial fibrillation is associated with enlarged atria. However, it is less likely that subjects with high CRF are asymptomatic from their atrial fibrillation compared with subjects with low CRF. Furthermore, self‐reported diagnoses of atrial fibrillation in HUNT3 have been validated, showing a negative predictive value of 98.4% for the self‐reported questionnaire.32 Thus, it is unlikely that confounding from atrial fibrillation has significantly affected the presented results.
Conclusions
In a healthy population, LA volume was positively associated with CRF, but not with diastolic dysfunction. On the basis of this study from a healthy population and earlier studies from diseased populations, there seems to be a U‐ or J‐shaped relationship between CRF and LA size. Age‐relative CRF should be considered when LA volume is included in clinical decision making. Enlarged LA volume may not be a marker of risk in fit subpopulations, which should be further studied.
Sources of Funding
The study was funded by The Liaison Committee for Education, Research and Innovation in Central Norway, the K.G. Jebsen Foundation, and the Norwegian University of Science and Technology, Trondheim, Norway.
Disclosures
None.
Supporting information
Data S1. Supplemental methods and results.
Table S1. Linear Regression Analyses With Left Atrial Volume Index as the Dependent Variable and Indices of Diastolic Dysfunction as Independent Variables
Table S2. Linear Regression Analyses With Indices of Diastolic Dysfunction as Dependent Variable and VO2peak/VO2%pred as Independent Variable
Figure S1. Prediction diagrams of left atrial volume index (A‐L method) for ages 40 and 70 years for men and women by percent of age and sex predicted VO2peak with confidence (blue dotted line) and prediction (red dotted line) intervals based on main results model 2 (n=229).
Figure S2. Prediction diagrams of left atrial volume index measured by biplane method of discs for different ages by (A) VO2peak (n=209), (B) percent of age and sex predicted VO2peak (n=209), and (C) percent of age and sex predicted VO2peak in men only (n=96).
Figure S3. Prediction of left atrial volume index (A‐L method) based on a restricted cubic spline model for percent of age and sex predicted VO2peak (n=229).
Figure S4. Prediction of left atrial volume index (A‐L method) by percent of age and sex‐predicted VO2peak based on a restricted cubic spline model for age.
Acknowledgments
The HUNT (Nord‐Trøndelag Health Study) is a collaboration between the HUNT Research Centre (Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology), Nord‐Trøndelag County Council, Central Norway Regional Health Authority, and the Norwegian Institute of Public Health.
(J Am Heart Assoc. 2020;9:e014682 DOI: 10.1161/JAHA.119.014682.)
References
- 1. Møller JE, Hillis GS, Oh JK, Seward JB, Reeder GS, Wright RS, Park SW, Bailey KR, Pellikka PA. Left atrial volume: a powerful predictor of survival after acute myocardial infarction. Circulation. 2003;107:2207–2212. [DOI] [PubMed] [Google Scholar]
- 2. Poulsen MK, Dahl JS, Henriksen JE, Hey TM, Høilund‐Carlsen PF, Beck‐Nielsen H, Møller JE. Left atrial volume index: relation to long‐term clinical outcome in type 2 diabetes. J Am Coll Cardiol. 2013;62:2416–2421. [DOI] [PubMed] [Google Scholar]
- 3. Tsang TSM, Abhayaratna WP, Barnes ME, Miyasaka Y, Gersh BJ, Bailey KR, Cha SS, Seward JB. Prediction of cardiovascular outcomes with left atrial size. J Am Coll Cardiol. 2006;47:1018–1023. [DOI] [PubMed] [Google Scholar]
- 4. Tsang TSM, Barnes ME, Gersh BJ, Bailey KR, Seward JB. Left atrial volume as a morphophysiologic expression of left ventricular diastolic dysfunction and relation to cardiovascular risk burden. Am J Cardiol. 2002;90:1284–1289. [DOI] [PubMed] [Google Scholar]
- 5. Abhayaratna WP, Seward JB, Appleton CP, Douglas PS, Oh JK, Tajik AJ, Tsang TSM. Left atrial size. J Am Coll Cardiol. 2006;47:2357–2363. [DOI] [PubMed] [Google Scholar]
- 6. Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Alexandru Popescu B, Waggoner AD. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016;17:1321–1360. [DOI] [PubMed] [Google Scholar]
- 7. Iskandar A, Mujtaba MT, Thompson PD. Left atrium size in elite athletes. JACC Cardiovasc Imaging. 2015;8:753–762. [DOI] [PubMed] [Google Scholar]
- 8. Pelliccia A, Maron BJ, Di Paolo FM, Biffi A, Quattrini FM, Pisicchio C, Roselli A, Caselli S, Culasso F. Prevalence and clinical significance of left atrial remodeling in competitive athletes. J Am Coll Cardiol. 2005;46:690–696. [DOI] [PubMed] [Google Scholar]
- 9. Zilinski JL, Contursi ME, Isaacs SK, Deluca JR, Lewis GD, Weiner RB, Hutter AM, D'Hemecourt PA, Troyanos C, Dyer KS, Baggish AL. Myocardial adaptations to recreational marathon training among middle‐aged men. Circ Cardiovasc Imaging. 2015;8:1–10. [DOI] [PubMed] [Google Scholar]
- 10. D'Andrea A, Riegler L, Cocchia R, Scarafile R, Salerno G, Gravino R, Golia E, Vriz O, Citro R, Limongelli G, Calabrò P, Di Salvo G, Caso P, Russo MG, Bossone E, Calabrò R. Left atrial volume index in highly trained athletes. Am Heart J. 2010;159:1155–1161. [DOI] [PubMed] [Google Scholar]
- 11. Brinker SK, Pandey A, Ayers CR, Barlow CE, DeFina LF, Willis BL, Radford NB, Farzaneh‐Far R, de Lemos JA, Drazner MH, Berry JD. Association of cardiorespiratory fitness with left ventricular remodeling and diastolic function. JACC Heart Fail. 2014;2:238–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ross R, Blair SN, Arena R, Church TS, Després J‐P, Franklin BA, Haskell WL, Kaminsky LA, Levine BD, Lavie CJ, Myers J, Niebauer J, Sallis R, Sawada SS, Sui X, Wisløff U. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134:e653–e699. [DOI] [PubMed] [Google Scholar]
- 13. Lang RM, Badano LP, Mor‐Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt J‐U. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015;16:233–271. [DOI] [PubMed] [Google Scholar]
- 14. Krokstad S, Langhammer A, Hveem K, Holmen T, Midthjell K, Stene T, Bratberg G, Heggland J, Holmen J. Cohort profile: the HUNT study, Norway. Int J Epidemiol. 2013;42:968–977. [DOI] [PubMed] [Google Scholar]
- 15. Thorstensen A, Dalen H, Amundsen BH, Aase SA, Stoylen A. Reproducibility in echocardiographic assessment of the left ventricular global and regional function, the HUNT study. Eur J Echocardiogr. 2010;11:149–156. [DOI] [PubMed] [Google Scholar]
- 16. Kurtze N, Rangul V, Hustvedt B‐E. Reliability and validity of the international physical activity questionnaire in the Nord‐Trøndelag Health Study (HUNT) population of men. BMC Med Res Methodol. 2008;8:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, George SM, Olson RD. The physical activity guidelines for Americans. JAMA. 2018;320:2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Loe H, Rognmo Ø, Saltin B, Wisløff U. Aerobic capacity reference data in 3816 healthy men and women 20–90 years. PLoS One. 2013;8:e64319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nes BM, Vatten LJ, Nauman J, Janzky I, Wisløff U. A simple nonexercise model of cardiorespiratory fitness predicts long‐term mortality. Med Sci Sports Exerc. 2014;46:1159–1165. [DOI] [PubMed] [Google Scholar]
- 20. Nistri S, Galderisi M, Ballo P, Olivotto I, D'Andrea A, Pagliani L, Santoro A, Papesso B, Innelli P, Cecchi F, Mondillo S. Determinants of echocardiographic left atrial volume: implications for normalcy. Eur J Echocardiogr. 2011;12:826–833. [DOI] [PubMed] [Google Scholar]
- 21. Opondo MA, Aiad N, Cain MA, Sarma S, Howden E, Stoller DA, Ng J, van Rijckevorsel P, Hieda M, Tarumi T, Palmer MD, Levine BD. Does high‐intensity endurance training increase the risk of atrial fibrillation? Circ Arrhythm Electrophysiol. 2018;11:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McNamara DA, Aiad N, Howden E, Hieda M, Link MS, Palmer D, Samels M, Everding B, Ng J, Adams‐Huet B, Opondo M, Sarma S, Levine BD. Left atrial electromechanical remodeling following 2 years of high‐intensity exercise training in sedentary middle‐aged adults. Circulation. 2019;139:1507–1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ratanasit N, Karaketklang K, Chirakarnjanakorn S, Krittayaphong R, Jakrapanichakul D. Left atrial volume as an independent predictor of exercise capacity in patients with isolated diastolic dysfunction presented with exertional dyspnea. Cardiovasc Ultrasound. 2014;12:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pritchett AM, Mahoney DW, Jacobsen SJ, Rodeheffer RJ, Karon BL, Redfield MM. Diastolic dysfunction and left atrial volume. J Am Coll Cardiol. 2004;45:87–92. [DOI] [PubMed] [Google Scholar]
- 25. Arruda ALM, Pellikka PA, Olson TP, Johnson BD. Exercise capacity, breathing pattern, and gas exchange during exercise for patients with isolated diastolic dysfunction. J Am Soc Echocardiogr. 2007;20:838–846. [DOI] [PubMed] [Google Scholar]
- 26. Guasch E, Benito B, Qi X, Cifelli C, Naud P, Shi Y, Mighiu A, Tardif J‐C, Tadevosyan A, Chen Y, Gillis M‐A, Iwasaki Y‐K, Dobrev D, Mont L, Heximer S, Nattel S. Atrial fibrillation promotion by endurance exercise. J Am Coll Cardiol. 2013;62:68–77. [DOI] [PubMed] [Google Scholar]
- 27. Paap D, Takken T. Reference values for cardiopulmonary exercise testing in healthy adults: a systematic review. Expert Rev Cardiovasc Ther. 2014;12:1439–1453. [DOI] [PubMed] [Google Scholar]
- 28. D'Ascenzi F, Piu P, Capone V, Sciaccaluga C, Solari M, Mondillo S, Henein M. Reference values of left atrial size and function according to age: should we redefine the normal upper limits? Int J Cardiovasc Imaging. 2019;35:41–48. [DOI] [PubMed] [Google Scholar]
- 29. Surkova E, Badano LP, Genovese D, Cavalli G, Lanera C, Bidviene J, Aruta P, Palermo C, Iliceto S, Muraru D. Clinical and prognostic implications of methods and partition values used to assess left atrial volume by two‐dimensional echocardiography. J Am Soc Echocardiogr. 2017;30:1119–1129. [DOI] [PubMed] [Google Scholar]
- 30. Stritzke J, Markus MRP, Duderstadt S, Lieb W, Luchner A, Döring A, Keil U, Hense H‐W, Schunkert H. The aging process of the heart: obesity is the main risk factor for left atrial enlargement during aging. J Am Coll Cardiol. 2009;54:1982–1989. [DOI] [PubMed] [Google Scholar]
- 31. Myrstad M, Løchen M‐L, Graff‐Iversen S, Gulsvik AK, Thelle DS, Stigum H, Ranhoff AH. Increased risk of atrial fibrillation among elderly Norwegian men with a history of long‐term endurance sport practice. Scand J Med Sci Sports. 2014;24:e238–e244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Malmo V, Langhammer A, Bønaa KH, Loennechen J, Ellekjaer H. Validation of self‐reported and hospital‐diagnosed atrial fibrillation: the HUNT‐study. Clin Epidemiol. 2016;8:185. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supplemental methods and results.
Table S1. Linear Regression Analyses With Left Atrial Volume Index as the Dependent Variable and Indices of Diastolic Dysfunction as Independent Variables
Table S2. Linear Regression Analyses With Indices of Diastolic Dysfunction as Dependent Variable and VO2peak/VO2%pred as Independent Variable
Figure S1. Prediction diagrams of left atrial volume index (A‐L method) for ages 40 and 70 years for men and women by percent of age and sex predicted VO2peak with confidence (blue dotted line) and prediction (red dotted line) intervals based on main results model 2 (n=229).
Figure S2. Prediction diagrams of left atrial volume index measured by biplane method of discs for different ages by (A) VO2peak (n=209), (B) percent of age and sex predicted VO2peak (n=209), and (C) percent of age and sex predicted VO2peak in men only (n=96).
Figure S3. Prediction of left atrial volume index (A‐L method) based on a restricted cubic spline model for percent of age and sex predicted VO2peak (n=229).
Figure S4. Prediction of left atrial volume index (A‐L method) by percent of age and sex‐predicted VO2peak based on a restricted cubic spline model for age.


