The concepts of stunned and hibernating myocardium were described and received considerable attention in the 1980s. These phenomena, related to myocardial ischemia (Figure 1), occur far more frequently than when they were initially described. This article defines these conditions, summarizes what has been learned about them since their original descriptions, and shows current importance of their understanding.
Figure 1.
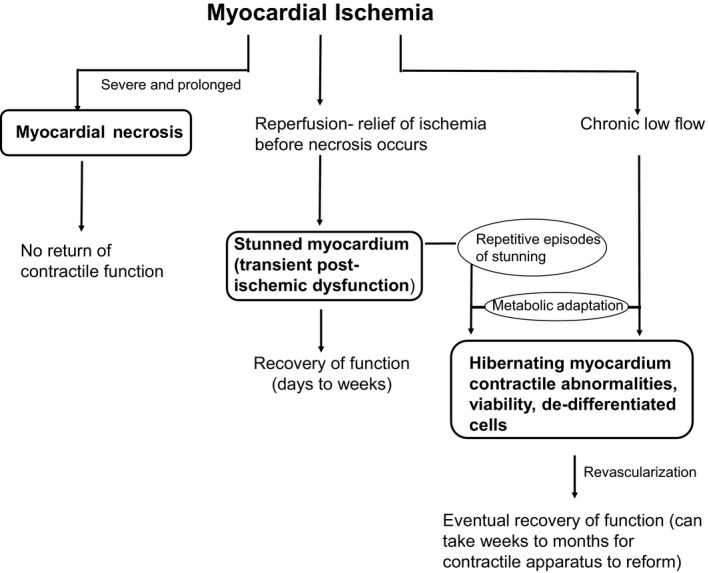
The schematic documents 3 possible outcomes of myocardial ischemia. On the left is the situation of severe and prolonged myocardial ischemia. The myocardial cells die resulting in a myocardial infarction, are replaced by scar tissue, and do not recover contractile function. In the middle is the scenario in which the duration and severity of myocardial ischemia are not long enough or severe enough to kill cells. When the ischemia is relieved by reperfusion, the myocardium is viable but stunned, exhibiting transient post‐ischemic contractile and biochemical dysfunction. Recovery of the stunned myocardium eventually occurs but may take days to weeks. The third scenario of ischemia is shown on the right. Chronic low blood flow results in metabolic adaptations allowing the cardiomyocytes to survive, but these cells do not contract at rest and exhibit typical morphology of dedifferentiation. Once revascularized, these hibernating myocardial cells eventually recover function, but this may require weeks to months as the contractile apparatus replenishes. In addition, another theory of hibernating myocardium is shown in which repetitive episodes of ischemic, stunned myocardium occur when coronary artery reserve cannot meet an increase in myocardial oxygen demand. These repetitive episodes of stunning lead to a chronic reduction in contractile function and metabolic adaptation to allow for cell survival.
Stunned Myocardium
Background
In 1982, Braunwald and Kloner1 described stunning as “prolonged, post‐ischemic ventricular dysfunction that occurs after brief periods of nonlethal ischemia.” They proposed that myocardial stunning may be thought of as a “hit” (an episode of severe ischemia), “run” (the relief of the ischemia before significant irreversible injury occurs), and “stun” (a relatively long period of post‐ischemic contractile dysfunction). The cardiac muscle eventually recovers fully, but during the phase of impaired function, it may require inotropic support. Stunned myocardium is also associated with prolonged biochemical abnormalities that may take days to resolve following initial resolution of ischemia. Delayed recovery following ischemia was first described in experimental animal studies in the 1970s and 1980s. Dogs were exposed to occlusions of a major coronary artery for up to 15 minutes, followed by reperfusion. This duration of ischemia causes largely “reversible” injury because it is not long enough to lead to detectable myocardial necrosis. (As described below, with more sensitive methods for detecting necrosis, evidence of apoptotic cell death has been identified.) Regional ventricular wall motion was measured with techniques such as ultrasonic crystals implanted in the walls of the ventricle.2, 3 The myocardium perfused by the occluded artery became akinetic or dyskinetic during ischemia. When blood flow was restored by removing the coronary artery clamp or ligation, contractile function remained depressed initially but then gradually recovered over the course of a few days. Cardiac ATP levels also demonstrated a biochemical stunning as levels were depressed within 15 minutes of coronary artery occlusion and gradually recovered toward normal by 72 hours of reperfusion.4 Histologic analysis revealed viable myocardial cells at 72 hours after reperfusion. Numerous laboratories demonstrated the phenomenon of stunned myocardium.5, 6 Whereas stunning was initially associated with brief periods of ischemia not associated with histologic evidence of cell death, other studies showed that this phenomenon occurred in models of myocardial infarction (MI), within the salvaged outer wall of the ventricle. In this case, the recovery of function following reperfusion of an experimental MI was even more prolonged, requiring days to weeks.7 Our research group showed that the contractile function of stunned myocardium could be supported with inotropes in the reperfused myocardial infarct models, without extending infarct size, as long as reperfusion had occurred and was complete.8, 9
There has been considerable interest in the mechanism(s) responsible for stunned myocardium. The 2 leading hypotheses are oxygen radical damage that occurs in the first few minutes of reperfusion and altered calcium flux with calcium overload that then desensitizes the myofilaments.10, 11 Zweier et al12 used spin trap techniques to show that there was a sizable burst of oxygen‐centered free radicals that occurs within the first 10 seconds of reperfusion. Oxygen free radicals are known to disrupt biologic systems including membranes and contractile apparatus. In an experimental model of 15 minutes of occlusion and 3 hours of reperfusion, Przyklenk et al13 showed that treatment with the oxygen free radical scavengers superoxide dismutase and catalase improved the contractility of stunned myocardium. Others also showed that oxygen radical scavengers were effective.10 The calcium blockers nifedipine14 and verapamil15 were shown to improve the recovery of stunned myocardium; the latter also partially preserved ATP levels. The calcium overload may result in decreased responsiveness of the myofilaments to calcium. More recently, it has been postulated that sarcoplasmic reticulum dysfunction may result in excitation‐contraction uncoupling as another component of the mechanism for stunning.16 In addition, a 2006 study showed that pretreatment of rabbits with ranolazine, an inhibitor of the late sodium channel current, also reduced stunning without any effect on hemodynamics, suggesting that the late sodium current may also play a role.17
Initial clinical evidence for stunned myocardium was substantiated by several observations: (1) the gradual return of regional function following thrombolytic therapy for acute MI, (2) prolonged left ventricular (LV) regional wall motion abnormalities in patients with unstable angina, (3) prolonged diastolic dysfunction following brief angioplasty balloon inflations and deflations, (4) persistent LV regional wall motion abnormalities following exercise‐induced ischemia, and (5) prolonged but reversible LV dysfunction following cardiac surgery1, 18, 19, 20 (Table 1). Stunned myocardium continues to be diagnosed in several different clinical scenarios.16
Table 1.
Clinical Evidence of Stunned Myocardium
|
Is Stunning Relevant in the PCI Era?
Whereas initial descriptions supporting the concept of stunned myocardium in humans occurring after reperfusion for acute MI came from the thrombolytic therapy literature,21 is there evidence for myocardial stunning in the percutaneous coronary intervention (PCI) era? Wdowiak‐Okrojek et al22 recently evaluated 97 patients with acute MI who were treated successfully with PCI and followed their cardiac function with serial 2‐dimensional echocardiographic speckle tracking following revascularization. They observed the greatest improvement in regional systolic function occurring between day 1 and 2 of reperfusion. On days 3 to 180 there was further improvement in systolic function but not as marked as during the first 2 days. Recovery of diastolic function took longer with the most significant improvement occurring very gradually over the first 7 days of reperfusion. This study showed that systolic and diastolic stunning is noted in 2019, despite the most up‐to‐date reperfusion strategies. In another study of PCI‐treated acute MIs, gated single‐photon emission computed tomography myocardial perfusion imaging was performed before hospital discharge and 6 months after hospital discharge in 120 patients. LV ejection fraction (LVEF) just before discharge was 47% and late EF was 51%; 54 patients showed an increase in EF of >5 units. Recovery of LVEF correlated to the amount of salvaged myocardium.23 Other studies have shown that myocardial stunning occurs following PCI for ST‐segment–elevation MI.24
Recent reports have confirmed that stunned myocardium occurs after even brief inflations of an angioplasty balloon in the coronary artery of patients undergoing elective PCI. McCormick et al25 studied 20 patients with preserved LV function and single vessel coronary artery disease (CAD) who were undergoing elective PCI. They placed a conductance catheter into the LV cavity and measured hemodynamics and pressure‐volume loops at baseline, during balloon inflation (coronary artery occlusion) and at 30 minutes of recovery (after balloon deflation). LV dysfunction was observed both during balloon inflation as well as at 30 minutes after deflation. At 30 minutes of reperfusion, cardiac output, EF, dP/dT max remained reduced and Tau remained elevated, consistent with stunning. Of note, pretreatment with glucagon‐like peptide‐1 protected the patients against ischemic LV dysfunction and stunning.
Although experimental studies showed that oxygen free radical scavengers, calcium blockers, and late sodium current inhibitors could improve the function of stunned myocardium, a recent clinical study suggested that the heart rate slowing drug, ivabradine, can prevent stunned myocardium associated with exercise inducible ischemia in coronary artery patients. In 15 patients with CAD, echocardiography was used to assess stunning. LV longitudinal strain was impaired during exercise at peak stress and for several minutes of recovery. After 2 weeks of ivabradine therapy, repeated stress echocardiograms showed that the drug prevented the impairment of LV function during recovery.26
Conditions That May Be Caused By Stunned Myocardium
Several recent reports have suggested that certain conditions whose exact cause remains to be determined, may be a manifestation of stunned myocardium. While the original description of stunned myocardium describes prolonged return of function after relief of a discrete episode of ischemia, these conditions may, but have not been unequivocally shown to, reflect ischemia followed by relief of ischemia. Therefore, it is safer at this point to state that these conditions may be, rather than definitively are, manifestations of stunning.
Stress cardiomyopathy or Takotsubo cardiomyopathy (Table 2) is one such example. This entity is characterized by chest pain, dyspnea, signs of ischemia on ECG (including transient ST‐segment–elevation and T‐wave inversion), elevated cardiac enzymes, transient LV apical ballooning with sparing of the basal portion of the left ventricle, and exclusion of significant organic stenosis in the coronary arteries. The circumferential nature of the transient LV wall motion abnormalities extend beyond the distribution of a single epicardial coronary artery, suggesting that, unlike most acute MIs, an occlusion in a single coronary artery cannot explain the extent of the wall motion abnormality.27 Takotsubo cardiomyopathy often occurs in postmenopausal women and is preceded by emotional stress. This disease may account for up to 1% to 2% of all patients hospitalized with the initial diagnosis of acute ST‐segment–elevation MI. Because the LV dysfunction usually resolves in about 2 to 5 weeks, an element of stunned myocardium has been implicated.28, 29 However, as Takotsubo cardiomyopathy is usually associated with elevations of cardiac enzymes, it is likely that once the acute episode is resolved, there is a mix of irreversibly injured cells (that die) as well as reversibly injured cells that survive. The cause of the apical ballooning is likely ischemia, but the exact mechanism is still debated. Coronary angiography usually does not show classic atherosclerotic narrowing. The arteries are often patent, suggesting elements of coronary artery vasospasm, perhaps microvascular spasm, or plaque rupture with spontaneous thrombolysis. Adrenergic hyperactivity or a sympathetic storm following stress may play a role and contribute to coronary artery spasm, damage cardiomyocytes by calcium overload, cause disorders of myocardial fatty acid metabolism, and contribute to atherosclerotic plaque rupture with subsequent spontaneous thrombolysis.30 Postmenopausal low estrogen levels have also been implicated. That Takotsubo cardiomyopathy is often associated with emotional stress is exemplified by recent reports linking it to the emotional stress associated with earthquakes.31 In experimental models, the administration of high doses of isoproterenol (to mimic adrenergic hyperactivity/sympathetic storm) has been used to study Takotsubo cardiomyopathy. In one study, our group observed that rats exposed to isoproterenol exhibited LV apical akinesis, with preservation of contractile motion in the basal portion of the left ventricle. Histologic and ultrastructural analysis at 24 hours exhibited a mix of necrotic cells plus reversibly injured myocytes showing vacuolization, lipid droplets, damaged mitochondria, and edema. Mononuclear cell infiltration was also observed. On day 8 after exposure, the apical akinesis fully resolved by echocardiographic analysis. Histologic analysis at day 8 revealed foci of both necrosis and fibrosis plus areas of viable tissue in the apical regions.32 Thus, the fact that viable tissue in the apex is present at 8 days and the function of the apex largely recovered after the initial insult on day 1 supports the concept that stunned myocardium plays a major role in Takotsubo cardiomyopathy.
Table 2.
Takotsubo (Stress) Cardiomyopathy
|
Neurogenic Stunned Myocardium
Another relatively recently recognized phenomenon is “neurogenic stunned myocardium.” While the term stunned myocardium is used to describe this phenomenon, whether it really represents true stunned myocardium as originally described and occurs following relief of a discrete episode of myocardial ischemia remains to be determined. Neurogenic events such as stroke, subarachnoid hemorrhages, or seizures cause a sympathetic storm that has also been associated with LV dysfunction. Some investigators categorize Takotsubo stress cardiomyopathy as a type of “neurogenic stunned myocardium.”33 The clinical findings may present similarly to acute MI with ischemic ECG changes (transient ST‐segment elevations and T‐wave inversions,34 QTc prolongation),35 LV wall motion abnormalities, decreased overall cardiac function, and elevated cardiac troponin levels. Angiography typically shows no mechanical obstruction of the coronary arteries and coronary vasospasm may contribute. The phenomenon is thought to be related to a surge in catecholamines after areas of the brain related to the autonomic nervous system have been damaged.36
The entity of neurogenic stunned myocardium does appear similar to Takotsubo cardiomyopathy but shows more global hypokinesis rather than the regional wall motion abnormality of apical ballooning. Improvement in function is observed within 2 to 5 days after the neurologic event, again suggesting that stunned myocardium was a prominent feature of this entity. Biso et al36 postulated that free radical release and calcium entry into the cells with contraction band formation, cardiac enzyme release, and myocytolysis play a role in the pathophysiology of neurogenic stunned myocardium.
Stunned Myocardium Associated With Dialysis
LV dysfunction has now been described during and after hemodialysis, and this has been attributed by some investigators to stunned myocardium. Mahmoud et al37 examined serial echocardiograms of 11 patients undergoing hemodialysis. All patients developed ≥2 new regional wall motion abnormalities during dialysis; these contractile abnormalities persisted for at least 30 minutes after dialysis. Global longitudinal strain, a measure of global LV contractility, was also impaired during and after dialysis.37 Penny et al38 showed that exercise preconditioning during dialysis could reduce the extent of stunning associated with dialysis, determined by echocardiography.
Biomarker Release Associated With Stunned Myocardium
There is ongoing controversy regarding the meaning of biomarker release of creatine kinase–myocardial band and cardiac troponin I and T associated with stunned myocardium. Release of these markers, typically associated with MI, into the blood stream have been well documented in experimental models of brief ischemia and reperfusion, not usually associated with MI.39, 40 Cardiac troponin has also been detected in the circulation after exercise or pacing‐induced ischemia,41 as well as after vigorous bouts of exercise not necessarily associated with known ischemia. It is unknown whether this biomarker is leaking from many cardiac cells that are reversibly injured or a few cells that are irreversibly injured. A recent investigation by Weil et al42 used a pig model of myocardial stunning, induced by a 10‐minute coronary artery occlusion and reperfusion. They observed a pathologic elevation of cardiac troponin I by 60 minutes after reperfusion and continued elevation at 24 hours. Although tissue staining with triphenyltetrazolium chloride and histologic analysis did not demonstrate classic ischemic necrosis, sections obtained 1 hour after reperfusion showed a 6‐fold increase in terminal deoxynucleotidyl transferase dUTP nick end labeling–positive cardiomyocytes in the region of ischemia/reperfusion. Therefore, their study suggests that the elevation of troponin I after a period of stunning is not associated with classic ischemic necrosis but with some cells that undergo apoptosis (programmed cell death). The clinical significance of this finding remains to be determined.42
Diagnosing Stunned Myocardium
How is stunned myocardium diagnosed? In some cases, the diagnosis will be retrospective with the observation that, after an episode of ischemia is relieved, there is a gradual improvement in LV function over time. In some cases, the diagnosis can be made prospectively by finding evidence of a “flow‐function mismatch,” which usually would be discovered by various imaging techniques. For example, the finding of a contractile dysfunction (by ventriculography, echocardiography, nuclear, or other imaging technique) after relief of a discrete episode of ischemia in the same area as normal perfusion (by thallium scintigraphy, positron emission tomography [PET], echocardiography contrast) is suggestive of stunning, especially if the region is shown to be viable (normal/enhanced glucose metabolism by PET; Figure 2). Nuclear imaging techniques have documented the presence of stunned myocardium following episodes of unstable angina.43 Recent studies suggest that adding a measure of wall thickening in addition to EF measure on single‐photon emission computed tomography imaging, improved the ability to diagnose stunned myocardium.44, 45 Viability is also suggested if the region that demonstrates contractile dysfunction shows improved function with inotropic stimulation.
Hibernating Myocardium
Background
The concept of hibernating myocardium (Figure 2, Table 3) was first proposed by Dr George Diamond in 197846 and then popularized by Dr Shahbudin Rahimtoola in 1989.47 The initial concept was that a region of the myocardium was supplied by an atherosclerotic coronary artery in which enough blood supply was present to maintain viability but not enough to maintain normal contractility of the region. In the setting of low blood flow (reduced oxygen supply), there was an adaptive downregulation of function (reduced oxygen demand) and metabolism to minimize ischemia and prevent myocardial necrosis.48 Rahimtoola's description of a typical case of hibernating myocardium reported the LV angiographic results of a patient who preoperatively had a single vessel occlusion (left anterior artery descending) with an EF of 37% and pronounced anteroapical akinesis of the left ventricle. However, after nitroglycerin, the EF improved to 51% and there was improved regional wall motion of the anteroapical region of the left ventricle, demonstrating active contraction (and viability) in regions that were not moving before nitroglycerin. Eight months after coronary artery bypass surgery to the left anterior descending artery, the EF was 76% and the anteroapical region of the left ventricle exhibited normal wall motion. Thus, a region of the myocardium that initially appeared akinetic, but was shown to be viable after nitroglycerin challenge and was therefore “hibernating,” had eventually recovered full function after revascularization.49 The regional wall motion abnormality caused by hibernating was present chronically, was related to low blood flow, without MI, and demonstrated the potential to recover (wake up out of hibernation) once blood flow was restored. The downregulation of function and metabolism would counter the reduced perfusion and could even prevent ischemia, and certainly prevent painful ischemia. In contrast to stunning, which is a result of a discrete episode of ischemia (lasting minutes to hours), followed by impaired ventricular performance that might persist for hours to days, hibernating myocardium results from months to years of reduced perfusion. The contractile dysfunction lasts until blood flow is re‐established and then slowly recovers.50
Figure 2.
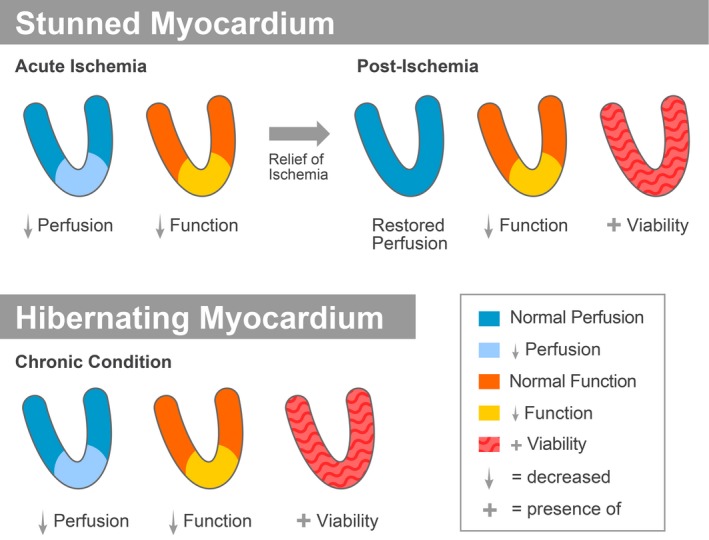
Schematic representation of imaging findings in stunned and hibernating myocardium. Top panel: The heart is shown as a conical structure with the base at the top and the apex at the bottom with the ventricular cavity in the middle. Stunned myocardium occurs after relief of a discreet episode of ischemia. During ischemia, imaging studies (such as nuclear studies using thallium or other tracers, echocardiographic contrast agents, magnetic resonance contrast imaging) will show reduced perfusion. During active ischemia, reduced perfusion of the apex is associated with reduced cardiac function (contractility) in the same apical region. Cardiac function can be measured by a variety of techniques, including real‐time nuclear imaging, echocardiography, and magnetic resonance imaging. After restoration of flow (angioplasty, stenting, thrombolysis, relief of coronary vasospasm), perfusion is restored but there is a persistent region of reduced cardiac function. The functional abnormality may last hours to days to weeks but eventually does recover. The myocardium shows positive viability (usually performed with positron emission tomography such as fluorodeoxyglucose uptake showing active metabolism and therefore viable metabolizing cells). Bottom panel: Hibernating myocardium is shown. At the apex there is eventually an area of reduced perfusion. In the early phase, this area may be characterized by normal resting flow with reduced coronary reactivity. Repetitive stunned myocardium may contribute as described in the text. The chronically (months to years) reduced perfusion is matched by a chronic reduction in cardiac function at the apex. The myocardium is viable as shown by studies such as positron emission tomography.
Table 3.
Clinical Evidence of Hibernating Myocardium
|
What is New and Controversial?
In the article by Braunwald and Kloner describing stunned myocardium, the authors postulated that the myocardium could become chronically stunned as a consequence of repetitive episodes of myocardial ischemia. In retrospect, this description may have actually described the situation of hibernating myocardium.1 There has been controversy regarding the issue of whether hibernating myocardium is the result of chronically reduced resting coronary flow or whether hibernation is caused by repeated episodes of ischemia/stunning48 as observed in a validated swine model.51 This latter concept would suggest that repetitive episodes of stunning1 lead to hibernating myocardium.52 With this theory of hibernating, the key problem is one of inadequate coronary flow reserve, such that resting flow is normal, but the coronaries cannot accommodate an increase in oxygen demand, resulting in repeated episodes of supply‐demand imbalance, with development of reduced ventricular function and adaptation of metabolism to reduce active ischemia. Using a chronic ameroid constrictor model in pigs, Canty and Fallavollita53, 54 showed that repetitive episodes of stunning over time also resulted in a downregulation of myocardial blood flow that reduced the mismatch between function and flow. They showed that there is a continuum from stunning that originally is associated with normal return of flow to repetitive stunning and then hibernating with reduced resting flow, thus reconciling the 2 theories regarding flow in hibernating myocardium. Clinical studies have also suggested varying degrees of flow‐function mismatch in patients with wall motion abnormalities.55 That altered coronary flow reserve is a key component of hibernating myocardium in patients and animal models has now been described in several studies.56, 57, 58, 59, 60
Phenotype of the Hibernating Myocyte
Whichever the exact mechanism, there is evidence that the myocardium can adapt to a low flow state. Experimental studies by Fedele et al61 showed that a partial stenosis in an animal model resulted in metabolic adaptation by the heart to minimize or reverse metabolic characteristics of ischemia. In the early minutes of placing a stenosis on the coronary artery, myocardial lactate consumption had turned to lactate production, but by 20 minutes to 1 hour after placing the stenosis, the degree of lactate production had fallen and by 2 hours after stenosis, metabolism had reverted to lactate consumption.61 In addition, at 5 minutes after coronary stenosis, regional venous pH had fallen to acidic levels, but by 1 to 3 hours after stenosis, pH returned to baseline. Histopathologic and electron microscopy of areas thought to be hibernating were assessed after obtaining biopsies during coronary artery bypass surgery.62, 63 These hibernating myocardial cells typically show a loss of contractile filaments with sarcomeres often confined to the periphery of the cells. Large spaces toward the center of cells show excess glycogen granules in the cytosol, small mitochondria, and loss of sarcoplasmic reticulum and transverse tubules. The cells also stain positively for excess glycogen on periodic acid–Schiff staining. The myocardial cells appear “dedifferentiated” in that they appear to have switched to a fetal phenotype. A possible analogy is what happens if you break your arm and your arm is placed into a cast. The muscles are not being used and therefore atrophy. In hibernating myocardium, the heart muscle cells are also not contracting, so a degree of atrophy or even dedifferentiation is not unexpected. Revascularization would therefore not expect to return function to normal immediately; rather, there would need to be time for the muscle cells to replenish their sarcomeres and regrow. Indeed, in an experimental study, a chronic stenosis of the left anterior descending artery was created in swine to produce hibernating myocardium. By 3 months there was depressed wall thickening in the left anterior descending region without infarction. While revascularization normalized blood flow, there was no immediate improvement in wall thickening of the left anterior descending region. Rather, wall thickening gradually improved but remained depressed at 1 month after revascularization. Following revascularization myocardial cells re‐entered the growth phase of the cell cycle and increased myocyte nuclear density, with new formation of protein.64
A study by Lionetti et al65 examined the histological and molecular features of hearts from patients undergoing transplantation for ischemic cardiomyopathy compared with hearts of patients with dilated cardiomyopathy. Histologic and molecular features associated with hibernating myocardium were observed in both hearts of patients with ischemic cardiomyopathy and hearts of patients with dilated cardiomyopathy (despite patent coronary arteries and less fibrosis in the dilated cardiomyopathy cohort).65 These findings suggest that some of the pathophysiology associated with hibernating myocardium may apply to dilated cardiomyopathy as well.
Imaging of Hibernating Myocardium
Various imaging techniques have been used to diagnose hibernating myocardium in patients. A perfusion‐metabolism mismatch showing absent or reduced perfusion in a region that is not contracting, but demonstrates active metabolism (such as fluorodeoxyglucose uptake), suggests hibernation.66 Hibernating myocardium has also been diagnosed by assessing contractile reserve, usually using echocardiography or magnetic resonance imaging (MRI) and low‐dose dobutamine. A region of the myocardium not initially contracting may contract when stimulated inotropically by low‐dose dobutamine. High‐dose dobutamine may make contraction worse, presumably by inducing ischemia. The fact that a region of the ventricle initially responds to the low‐dose inotrope proves that the region is not dead and has contractile reserve. Ruling out MI or scar is also part of the imaging workup of hibernating myocardium and can be achieved by MRI (ruling out late gadolinium enhancement) or scarring by echo or identifying LV wall thickness >5 to 6 mm, which would be unlikely in a transmural infarction. Gunning et al67 compared several techniques for predicting hibernation and assessed biopsies of the ventricle for myocyte volume fraction. In this study, true hibernating myocardium was assessed by determining improvement in postoperative function. Thallium was the most sensitive imaging technique for predicting hibernating myocardium, whereas MRI was the most specific. Myocyte volume fraction assessed upon biopsies was higher in those segments predicted to be hibernating rather than scar and was higher when both thallium and MRI predicted hibernation.
Viability Testing of Revascularization Therapy
How important is viability testing before going forward with a revascularization procedure? The issue of viability testing remains controversial.48 A 2002 meta‐analysis by Allman et al68 suggested that there was a close association between testing for viability and improved survival following revascularization therapy versus medical therapy alone. While, if there was an absence of viability, then there was no difference in survival outcome between revascularization therapy versus medical therapy. In this analysis of >3000 patients with CAD and LV dysfunction (EF 32%), viability testing was assessed using thallium perfusion, fluorodeoxyglucose metabolic imaging, or dobutamine echocardiography. In patients showing areas of viability, revascularization resulted in an annual mortality rate of 3.2% over an average of 25 months compared with 16% with the medical treatment alone (no revascularization) groups (P<0.0001). Thus, there was a 79.6% reduction in annual mortality by revascularizing areas of viability compared with no revascularization. In patients without viability, there was no difference in annual mortality between revascularizing (7.7%) or medical therapy (6.2%). This analysis would therefore favor the use of viability testing. A recent subanalysis of the PARR‐2 (PET and Recovery Following Revascularization‐2) study analyzed 182 patients with LV dysfunction and CAD who underwent assessment for PET mismatch between perfusion and active metabolism. Patients with larger amounts of mismatch (and therefore larger amounts of hibernating myocardium) had better clinical outcomes (less cardiac death, MI, or cardiac hospitalization) with revascularization therapy.69 However, the STICH (Surgical Treatment for Ischemic Heart Failure) trial called into question the importance of viability testing. Among 1212 patients enrolled in the trial who had severe CAD and an LVEF <35%, 610 had viability testing (single‐photon emission computed tomography and/or dobutamine echocardiography) and were randomized to medical therapy plus coronary artery bypass grafting (CABG) or medical therapy alone. There was no significant interaction between viability status and treatment with respect to mortality. The assessment of viability did not identify patients with a different survival benefit from CABG.70 Of note, at 5 years, there was no significant reduction in mortality with CABG versus medical therapy.71 There was a modest 8% reduction in mortality with revascularization compared with medical therapy alone reported at 10 years of follow‐up.72 Did this trial spell the end to viability testing for the issue of revascularization? There were a number of criticisms regarding the viability issue in the STICH trial including the following: tests such as MRI or PET may have been more accurate for viability than single‐photon emission computed tomography or dobutamine echocardiography performed in the STICH trial, with only less than half of the total patients enrolled in STICH having viability testing; 40% of the patients enrolled were asymptomatic; patients were not assessed for ischemia; postoperative LV volumes were not reported; and other weaknesses continue to be debated.73, 74, 75, 76, 77, 78 A follow‐up article by the STICH group monitored patients out to >10 years and again concluded that myocardial viability testing did not help delineate the benefits of revascularization with CABG versus medical therapy in patients with ischemic cardiomyopathy.79 However, this study did show that increases in LVEF were only observed in those patients who had evidence for viability, irrespective of whether the patients received CABG plus medical therapy or medical therapy alone, suggesting that at least the diagnosis of viability was associated with eventual recovery of some degree of function. Another fairly recent study failed to show an overall benefit of PET imaging for management of patients with CAD and LV dysfunction, although some subpopulations may benefit.80 Arora et al81 also observed mixed results when assessing usefulness of PET imaging to predict recovery of LV perfusion and EF following CABG. However, a more recent study showed that viability testing using MRI (low‐dose dobutamine for contractile reserve and late gadolinium enhancement for visualization of scar) could predict improvement in long‐term functional recovery of the left ventricle, although this improvement in function was considerably delayed and required up to 35 months. In this study, the presence of contractile reserve best predicted earlier ventricular functional improvement.82 Thus, debate continues about the usefulness of viability testing as a management tool for whether to go forward with revascularization procedures.
Another Approach to Treating Hibernating Myocardium
The therapy of choice for the treatment of hibernating myocardium is revascularization, which can take the form of PCI (angioplasty and/or stenting) or coronary artery bypass surgery. However, as mentioned, revascularization may not lead to immediate recovery of function, and delay in return of function should be expected as myocardial muscle cells may go through a phase of stunning and may take considerable time to rebuild their contractile machinery. Another approach has recently been described in the experimental literature. This concept involves injecting stem cells (mesenchymal stem cells and mononuclear cells) into models of myocardial ischemia, which in several studies improved cardiac function and improved coronary perfusion.83 Weil,84 Canty,53,54 and others assessed the efficacy of intracoronary‐delivered allogeneic mesenchymal stem cells and cardiosphere‐derived cells using a swine model of hibernating myocardium. Pigs were subjected to a chronic left anterior descending coronary artery stenosis. Three months after instrumentation, when the percent wall thickening of the anterior wall was reduced (38% versus 83% in control nonischemic tissue), treatment with one of the stem cell types was initiated and compared with vehicle. The pigs were immunosuppressed with cyclosporine to avoid a rejection phenomenon. Four weeks after cell therapy, the percent wall thickening of the anterior LV wall remained depressed (34%) in the vehicle group, whereas it recovered to 51% in both the allogeneic mesenchymal stem cell group and also to 51% in the cardiosphere‐derived cell group. Both therapies improved myocyte nuclear density and reduced cell hypertrophy in both the ischemic and remote regions of the left ventricle. The stem cell therapies did not increase tissue perfusion in this study. The authors concluded that both stem cell types had similar therapeutic efficacy in improving regional function of hibernating myocardium in this large animal model.84 Thus, another approach to the treatment of hibernating myocardium, besides simply revascularizing the myocardium, is to consider regenerative techniques such as some types of stem cell therapy.
Summary
The phenomena of stunned myocardium and hibernating myocardium were first described decades ago but they remain clinically relevant problems. Stunned myocardium remains an issue following contemporary reperfusion therapy for acute MI and can contribute to post‐MI LV dysfunction and heart failure. Exercise‐induced stunning is now well recognized. Recently, 3 conditions have been described that may also involve an element of stunning: stress cardiomyopathy (Takotsubo), “neurogenic stunned myocardium,” and LV abnormalities associated with dialysis. One clinical study showed that the heart rate–slowing drug, ivabradine, was effective in reducing exercise‐induced stunning. Hibernating myocardium is still a condition that can contribute to heart failure and ischemic cardiomyopathy. Hibernating myocardium may begin as repetitive episodes of stunning with normal resting coronary blood flow between episodes but eventually result in a chronic wall motion abnormality with reduced resting blood flow. There is a characteristic phenotype of the hibernating cardiomyocyte that includes sparse contractile elements located at the periphery of cells with central cytoplasm containing abundant glycogen granules and small mitochondria. Hibernating myocardium can be diagnosed by a variety of imaging techniques. While revascularization of hibernating myocardium improves cardiac function, there is still controversy regarding the importance of viability testing. Experimental studies suggest that a novel therapy for hibernating myocardium involves stem cell therapy.
Disclosures
None.
Acknowledgments
The author thanks Dr Eugene Braunwald for advice and guidance in preparing this article.
References
- 1. Braunwald E, Kloner RA. The stunned myocardium: prolonged, postischemic ventricular dysfunction. Circulation. 1982;66:1146–1149. [DOI] [PubMed] [Google Scholar]
- 2. Heyndrickx GR, Millard RW, McRitchie RJ, Maroko PR, Vatner SF. Regional myocardial functional and electrophysiological alterations after brief coronary artery occlusion in conscious dogs. J Clin Invest. 1975;56:978–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kloner RA, Ellis SG, Carlson NV, Braunwald E. Coronary reperfusion for the treatment of acute myocardial infarction: postischemic ventricular dysfunction. Cardiology. 1983;70:233–246. [DOI] [PubMed] [Google Scholar]
- 4. DeBoer LW, Ingwall JS, Kloner RA, Braunwald E. Prolonged derangements of canine myocardial purine metabolism after a brief coronary artery occlusion not associated with anatomic evidence of necrosis. Proc Natl Acad Sci USA. 1980;77:5471–5475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ambrosio G, Zweier JL, Jacobus WE, Weisfeldt ML, Flaherty JT. Improvement of postischemic myocardial function and metabolism induced by administration of deferoxamine at the time of reflow: the role of iron in the pathogenesis of reperfusion injury. Circulation. 1987;76:906–915. [DOI] [PubMed] [Google Scholar]
- 6. Charlat ML, O'Neill PG, Hartley CJ, Roberts R, Bolli R. Prolonged abnormalities of left ventricular diastolic wall thinning in the “stunned” myocardium in conscious dogs: time course and relation to systolic function. J Am Coll Cardiol. 1989;13:185–194. [DOI] [PubMed] [Google Scholar]
- 7. Ellis SG, Henschke CI, Sandor T, Wynne J, Braunwald E, Kloner RA. Time course of functional and biochemical recovery of myocardium salvaged by reperfusion. J Am Coll Cardiol. 1983;1:1047–1055. [DOI] [PubMed] [Google Scholar]
- 8. Arnold JM, Braunwald E, Sandor T, Kloner RA. Inotropic stimulation of reperfused myocardium with dopamine: effects on infarct size and myocardial function. J Am Coll Cardiol. 1985;6:1026–1034. [DOI] [PubMed] [Google Scholar]
- 9. Ellis SG, Wynne J, Braunwald E, Henschke CI, Sandor T, Kloner RA. Response of reperfusion‐salvaged, stunned myocardium to inotropic stimulation. Am Heart J. 1984;107:13–19. [DOI] [PubMed] [Google Scholar]
- 10. Bolli R, Marban E. Molecular and cellular mechanisms of myocardial stunning. Physiol Rev. 1999;79:609–634. [DOI] [PubMed] [Google Scholar]
- 11. Kloner RA, Przyklenk K, Patel B. Altered myocardial states. The stunned and hibernating myocardium. Am J Med. 1989;86:14–22. [DOI] [PubMed] [Google Scholar]
- 12. Zweier JL, Flaherty JT, Weisfeldt ML. Direct measurement of free radical generation following reperfusion of ischemic myocardium. Proc Natl Acad Sci USA. 1987;84:1404–1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Przyklenk K, Kloner RA. Superoxide dismutase plus catalase improve contractile function in the canine model of the “stunned myocardium”. Circ Res. 1986;58:148–156. [DOI] [PubMed] [Google Scholar]
- 14. Przyklenk K, Ghafari GB, Eitzman DT, Kloner RA. Nifedipine administered after reperfusion ablates systolic contractile dysfunction of postischemic “stunned” myocardium. J Am Coll Cardiol. 1989;13:1176–1183. [DOI] [PubMed] [Google Scholar]
- 15. Przyklenk K, Kloner RA. Effect of verapamil on postischemic “stunned” myocardium: importance of the timing of treatment. J Am Coll Cardiol. 1988;11:614–623. [DOI] [PubMed] [Google Scholar]
- 16. Guaricci AI, Bulzis G, Pontone G, Scicchitano P, Carbonara R, Rabbat M, De Santis D, Ciccone MM. Current interpretation of myocardial stunning. Trends Cardiovasc Med. 2018;28:263–271. [DOI] [PubMed] [Google Scholar]
- 17. Hale SL, Kloner RA. Ranolazine, an inhibitor of the late sodium channel current, reduces postischemic myocardial dysfunction in the rabbit. J Cardiovasc Pharmacol Ther. 2006;11:249–255. [DOI] [PubMed] [Google Scholar]
- 18. Kloner RA, Allen J, Cox TA, Zheng Y, Ruiz CE. Stunned left ventricular myocardium after exercise treadmill testing in coronary artery disease. Am J Cardiol. 1991;68:329–334. [DOI] [PubMed] [Google Scholar]
- 19. Kloner RA, Przyklenk K. Stunned and hibernating myocardium. Annu Rev Med. 1991;42:1–8. [DOI] [PubMed] [Google Scholar]
- 20. Patel B, Kloner RA, Przyklenk K, Braunwald E. Postischemic myocardial “stunning”: a clinically relevant phenomenon. Ann Intern Med. 1988;108:626–628. [DOI] [PubMed] [Google Scholar]
- 21. Touchstone DA, Beller GA, Nygaard TW, Tedesco C, Kaul S. Effects of successful intravenous reperfusion therapy on regional myocardial function and geometry in humans: a tomographic assessment using two‐dimensional echocardiography. J Am Coll Cardiol. 1989;13:1506–1513. [DOI] [PubMed] [Google Scholar]
- 22. Wdowiak‐Okrojek K, Wejner‐Mik P, Kasprzak JD, Lipiec P. Recovery of regional systolic and diastolic myocardial function after acute myocardial infarction evaluated by two‐dimensional speckle tracking echocardiography. Clin Physiol Funct Imaging. 2019;39:177–181. [DOI] [PubMed] [Google Scholar]
- 23. Calabretta R, Castello A, Linguanti F, Tutino F, Ciaccio A, Giglioli C, Sciagra R. Prediction of functional recovery after primary PCI using the estimate of myocardial salvage in gated SPECT early after acute myocardial infarction. Eur J Nucl Med Mol Imaging. 2018;45:530–537. [DOI] [PubMed] [Google Scholar]
- 24. Sharif D, Matanis W, Sharif‐Rasslan A, Rosenschein U. Doppler echocardiographic myocardial stunning index predicts recovery of left ventricular systolic function after primary percutaneous coronary intervention. Echocardiography. 2016;33:1465–1471. [DOI] [PubMed] [Google Scholar]
- 25. McCormick LM, Hoole SP, White PA, Read PA, Axell RG, Clarke SJ, O'Sullivan M, West NE, Dutka DP. Pre‐treatment with glucagon‐like Peptide‐1 protects against ischemic left ventricular dysfunction and stunning without a detected difference in myocardial substrate utilization. JACC Cardiovasc Interv. 2015;8:292–301. [DOI] [PubMed] [Google Scholar]
- 26. Maranta F, Tondi L, Agricola E, Margonato A, Rimoldi O, Camici PG. Ivabradine reduces myocardial stunning in patients with exercise‐inducible ischaemia. Basic Res Cardiol. 2015;110:55. [DOI] [PubMed] [Google Scholar]
- 27. Richard C. Stress‐related cardiomyopathies. Ann Intensive Care. 2011;1:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chen W, Dilsizian V. Exploring the pathophysiology of takotsubo cardiomyopathy. Curr Cardiol Rep. 2017;19:53. [DOI] [PubMed] [Google Scholar]
- 29. Ranieri M, Finsterer J, Bedini G, Parati EA, Bersano A. Takotsubo syndrome: clinical features, pathogenesis, treatment, and relationship with cerebrovascular diseases. Curr Neurol Neurosci Rep. 2018;18:20. [DOI] [PubMed] [Google Scholar]
- 30. Said SM, Saygili E, Rana OR, Genz C, Hahn J, Bali R, Varshney S, Albouaini K, Prondzinsky R, Braun‐Dullaeus RC. Takotsubo cardiomyopathy: what we have learned in the last 25 years? (a comparative literature review). Curr Cardiol Rev. 2016;12:297–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kloner RA. Lessons learned about stress and the heart after major earthquakes. Am Heart J. 2019;215:20–26. [DOI] [PubMed] [Google Scholar]
- 32. Sachdeva J, Dai W, Kloner RA. Functional and histological assessment of an experimental model of Takotsubo's cardiomyopathy. J Am Heart Assoc. 2014;3:e000921 DOI: 10.1161/JAHA.114.000921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Medina de Chazal H, Del Buono MG, Keyser‐Marcus L, Ma L, Moeller FG, Berrocal D, Abbate A. Stress cardiomyopathy diagnosis and treatment: JACC state‐of‐the‐art review. J Am Coll Cardiol. 2018;72:1955–1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Akutsu Y, Kaneko K, Kodama Y, Li HL, Suyama J, Toshida T, Kayano H, Shinozuka A, Gokan T, Kobayashi Y. Reversible T‐wave inversions and neurogenic myocardial stunning in a patient with recurrent stress‐induced cardiomyopathy. Ann Noninvasive Electrocardiol. 2014;19:285–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Murthy SB, Shah S, Rao CP, Bershad EM, Suarez JI. Neurogenic stunned myocardium following acute subarachnoid hemorrhage: pathophysiology and practical considerations. J Intensive Care Med. 2015;30:318–325. [DOI] [PubMed] [Google Scholar]
- 36. Biso S, Wongrakpanich S, Agrawal A, Yadlapati S, Kishlyansky M, Figueredo V. A review of neurogenic stunned myocardium. Cardiovasc Psychiatry Neurol. 2017;2017:5842182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mahmoud H, Forni LG, McIntyre CW, Selby NM. Myocardial stunning occurs during intermittent haemodialysis for acute kidney injury. Intensive Care Med. 2017;43:942–944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Penny JD, Salerno FR, Brar R, Garcia E, Rossum K, McIntyre CW, Bohm CJ. Intradialytic exercise preconditioning: an exploratory study on the effect on myocardial stunning. Nephrol Dial Transplant. 2019;34:1917–1923. [DOI] [PubMed] [Google Scholar]
- 39. Wu AH. Release of cardiac troponin from healthy and damaged myocardium. Front Lab Med. 2017;1:144–150. [Google Scholar]
- 40. Jaffe AS, Wu AH. Troponin release–reversible or irreversible injury? Should we care? Clin Chem. 2012;58:148–150. [DOI] [PubMed] [Google Scholar]
- 41. Turer AT, Addo TA, Martin JL, Sabatine MS, Lewis GD, Gerszten RE, Keeley EC, Cigarroa JE, Lange RA, Hillis LD, de Lemos JA. Myocardial ischemia induced by rapid atrial pacing causes troponin T release detectable by a highly sensitive assay: insights from a coronary sinus sampling study. J Am Coll Cardiol. 2011;57:2398–2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Weil BR, Young RF, Shen X, Suzuki G, Qu J, Malhotra S, Canty JM Jr. Brief myocardial ischemia produces cardiac troponin I release and focal myocyte apoptosis in the absence of pathological infarction in swine. JACC Basic Transl Sci. 2017;2:105–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gerber BL, Wijns W, Vanoverschelde JL, Heyndrickx GR, De Bruyne B, Bartunek J, Melin JA. Myocardial perfusion and oxygen consumption in reperfused noninfarcted dysfunctional myocardium after unstable angina: direct evidence for myocardial stunning in humans. J Am Coll Cardiol. 1999;34:1939–1946. [DOI] [PubMed] [Google Scholar]
- 44. Bestetti A, Cuko B, Decarli A, Galli A, Lombardi F. Additional value of systolic wall thickening in myocardial stunning evaluated by stress‐rest gated perfusion SPECT. J Nucl Cardiol. 2019;26:833–840. [DOI] [PubMed] [Google Scholar]
- 45. Bestetti A, Cuko B, Gasparini M, De Servi S. Better characterization of dipyridamole‐induced myocardial stunning by systolic wall thickening. A gated perfusion SPECT study. J Nucl Cardiol. 2018. Available at: 10.1007/s12350-018-1340-6. [DOI] [PubMed] [Google Scholar]
- 46. Diamond GA, Forrester JS, deLuz PL, Wyatt HL, Swan HJ. Post‐extrasystolic potentiation of ischemic myocardium by atrial stimulation. Am Heart J. 1978;95:204–209. [DOI] [PubMed] [Google Scholar]
- 47. Rahimtoola SH. The hibernating myocardium. Am Heart J. 1989;117:211–221. [DOI] [PubMed] [Google Scholar]
- 48. Ryan MJ, Perera D. Identifying and managing hibernating myocardium: what's new and what remains unknown? Curr Heart Fail Rep. 2018;15:214–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Rahimtoola SH. Coronary bypass surgery for chronic angina—1981. A perspective. Circulation. 1982;65:225–241. [DOI] [PubMed] [Google Scholar]
- 50. Braunwald E, Rutherford JD. Reversible ischemic left ventricular dysfunction: evidence for the “hibernating myocardium”. J Am Coll Cardiol. 1986;8:1467–1470. [DOI] [PubMed] [Google Scholar]
- 51. Kim SJ, Peppas A, Hong SK, Yang G, Huang Y, Diaz G, Sadoshima J, Vatner DE, Vatner SF. Persistent stunning induces myocardial hibernation and protection: flow/function and metabolic mechanisms. Circ Res. 2003;92:1233–1239. [DOI] [PubMed] [Google Scholar]
- 52. Depre C, Vatner SF. Mechanisms of cell survival in myocardial hibernation. Trends Cardiovasc Med. 2005;15:101–110. [DOI] [PubMed] [Google Scholar]
- 53. Canty JM, Fallavollita JA. Chronic hibernation and chronic stunning: a continuum. J Nucl Cardiol. 2000;7:509–527. [DOI] [PubMed] [Google Scholar]
- 54. Canty JM, Fallavollita JA. Lessons from experimental models of hibernating myocardium. Coron Artery Dis. 2001;374–380. [DOI] [PubMed] [Google Scholar]
- 55. Nihoyannopoulos P, Vanoverschelde JL. Myocardial ischaemia and viability: the pivitol role of echocardiography. Eur Heart J. 2011;32:810–819. [DOI] [PubMed] [Google Scholar]
- 56. Burton JO, Jefferies HJ, Selby NM, McIntyre CW. Hemodialysis‐induced repetitive myocardial injury results in global and segmental reduction in systolic cardiac function. Clin J Am Soc Nephrol. 2009;4:1925–1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Marzullo P, Parodi O, Sambuceti G, Giorgetti A, Picano E, Gimelli A, Salvadori P, L'Abbate A. Residual coronary reserve identifies segmental viability in patients with wall motion abnormalities. J Am Coll Cardiol. 1995;26:342–350. [DOI] [PubMed] [Google Scholar]
- 58. Rinaldi CA, Masani ND, Linka AZ, Hall RJ. Effect of repetitive episodes of exercise induced myocardial ischaemia on left ventricular function in patients with chronic stable angina: evidence for cumulative stunning or ischaemic preconditioning? Heart. 1999;81:404–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Vanoverschelde JL, Wijns W, Depre C, Essamri B, Heyndrickx GR, Borgers M, Bol A, Melin JA. Mechanisms of chronic regional postischemic dysfunction in humans. New insights from the study of noninfarcted collateral‐dependent myocardium. Circulation. 1993;87:1513–1523. [DOI] [PubMed] [Google Scholar]
- 60. Verheyen F, Racz R, Borgers M, Driesen RB, Lenders MH, Flameng WJ. Chronic hibernating myocardium in sheep can occur without degenerating events and is reversed after revascularization. Cardiovasc Pathol. 2014;23:160–168. [DOI] [PubMed] [Google Scholar]
- 61. Fedele FA, Gewirtz H, Capone RJ, Sharaf B, Most AS. Metabolic response to prolonged reduction of myocardial blood flow distal to a severe coronary artery stenosis. Circulation. 1988;78:729–735. [DOI] [PubMed] [Google Scholar]
- 62. Borgers M. Hibernating myocardium: programmed cell survival or programmed cell death? Exp Clin Cardiol. 2002;7:69–72. [PMC free article] [PubMed] [Google Scholar]
- 63. Borgers M, Thone F, Ausma J, Shevalkar B, Flameng WJ. Structural correlates of regional myocardial dysfunction in patients with critical coronary artery stenosis: chronic hibernation? Cardiovasc Pathol. 1993;2:237–245. [Google Scholar]
- 64. Page BJ, Banas MD, Suzuki G, Weil BR, Young RF, Fallavollita JA, Palka BA, Canty JM Jr. Revascularization of chronic hibernating myocardium stimulates myocyte proliferation and partially reverses chronic adaptations to ischemia. J Am Coll Cardiol. 2015;65:684–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Lionetti V, Matteucci M, Ribezzo M, Di Silvestre D, Brambilla F, Agostini S, Mauri P, Padeletti L, Pingitore A, Delsedime L, Rinaldi M, Recchia FA, Pucci A. Regional mapping of myocardial hibernation phenotype in idiopathic end‐stage dilated cardiomyopathy. J Cell Mol Med. 2014;18:396–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Taegtmeyer H, Dilsizian V. Imaging myocardial metabolism and ischemic memory. Nat Clin Pract Cardiovasc Med. 2008;5(suppl 2):S42–S48. [DOI] [PubMed] [Google Scholar]
- 67. Gunning MG, Kaprielian RR, Pepper J, Pennell DJ, Sheppard MN, Severs NJ, Fox KM, Underwood SR. The histology of viable and hibernating myocardium in relation to imaging characteristics. J Am Coll Cardiol. 2002;39:428–435. [DOI] [PubMed] [Google Scholar]
- 68. Allman KC, Shaw LJ, Hachamovitch R, Udelson JE. Myocardial viability testing and impact of revascularization on prognosis in patients with coronary artery disease and left ventricular dysfunction: a meta‐analysis. J Am Coll Cardiol. 2002;39:1151–1158. [DOI] [PubMed] [Google Scholar]
- 69. D'Egidio G, Nichol G, Williams KA, Guo A, Garrard L, deKemp R, Ruddy TD, DaSilva J, Humen D, Gulenchyn KY, Freeman M, Racine N, Benard F, Hendry P, Beanlands RS. Increasing benefit from revascularization is associated with increasing amounts of myocardial hibernation: a substudy of the PARR‐2 trial. JACC Cardiovasc Imaging. 2009;2:1060–1068. [DOI] [PubMed] [Google Scholar]
- 70. Bonow RO, Maurer G, Lee KL, Holly TA, Binkley PF, Desvigne‐Nickens P, Drozdz J, Farsky PS, Feldman AM, Doenst T, Michler RE, Berman DS, Nicolau JC, Pellikka PA, Wrobel K, Alotti N, Asch FM, Favaloro LE, She L, Velazquez EJ, Jones RH, Panza JA. Myocardial viability and survival in ischemic left ventricular dysfunction. N Engl J Med. 2011;364:1617–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Velazquez EJ, Lee KL, Deja MA, Jain A, Sopko G, Marchenko A, Ali IS, Pohost G, Gradinac S, Abraham WT, Yii M, Prabhakaran D, Szwed H, Ferrazzi P, Petrie MC, O'Connor CM, Panchavinnin P, She L, Bonow RO, Rankin GR, Jones RH, Rouleau JL. Coronary‐artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011;364:1607–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Velazquez EJ, Lee KL, Jones RH, Al‐Khalidi HR, Hill JA, Panza JA, Michler RE, Bonow RO, Doenst T, Petrie MC, Oh JK, She L, Moore VL, Desvigne‐Nickens P, Sopko G, Rouleau JL. Coronary‐artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med. 2016;374:1511–1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Athanasuleas C, Buckberg G, Conte J. The STICH trial data: keep it simple. J Thorac Cardiovasc Surg. 2015;149:1682–1683. [DOI] [PubMed] [Google Scholar]
- 74. Cortigiani L, Bigi R, Sicari R. Is viability still viable after the STICH trial? Eur Heart J Cardiovasc Imaging. 2012;13:219–226. [DOI] [PubMed] [Google Scholar]
- 75. Daggubati R, Arumugham P, Ferguson TB Jr. The world post STICH: is this a “game changer?” A surgeon's perspective–revascularization is still the treatment of choice. Prog Cardiovasc Dis. 2013;55:470–475. [DOI] [PubMed] [Google Scholar]
- 76. Gramze NL, Shah DJ. Is there a need to assess myocardial viability in patients presenting with heart failure? Curr Opin Cardiol. 2016;31:501–509. [DOI] [PubMed] [Google Scholar]
- 77. Shah BN, Khattar RS, Senior R. The hibernating myocardium: current concepts, diagnostic dilemmas, and clinical challenges in the post‐STICH era. Eur Heart J. 2013;34:1323–1336. [DOI] [PubMed] [Google Scholar]
- 78. Srichai MB, Jaber WA. Viability by MRI or PET would have changed the results of the STICH trial. Prog Cardiovasc Dis. 2013;55:487–493. [DOI] [PubMed] [Google Scholar]
- 79. Panza JA, Ellis AM, Al‐Khalidi HR, Holly TA, Berman DS, Oh JK, Pohost GM, Sopko G, Chrzanowski L, Mark DB, Kukulski T, Favaloro LE, Maurer G, Farsky PS, Tan RS, Asch FM, Velazquez EJ, Rouleau JL, Lee KL, Bonow RO. Myocardial viability and long‐term outcomes in ischemic cardiomyopathy. N Engl J Med. 2019;381:739–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Beanlands RS, Nichol G, Huszti E, Humen D, Racine N, Freeman M, Gulenchyn KY, Garrard L, deKemp R, Guo A, Ruddy TD, Benard F, Lamy A, Iwanochko RM. F‐18‐fluorodeoxyglucose positron emission tomography imaging‐assisted management of patients with severe left ventricular dysfunction and suspected coronary disease: a randomized, controlled trial (PARR‐2). J Am Coll Cardiol. 2007;50:2002–2012. [DOI] [PubMed] [Google Scholar]
- 81. Arora Y, Singh RS, Sampath S, Sood A, Singh P, Singh H, Mishra AK, Parmar M. Impact of hibernating and viable myocardium on improvement in perfusion and left ventricular ejection fraction after coronary artery bypass graft. Nucl Med Commun. 2019;40:325–332. [DOI] [PubMed] [Google Scholar]
- 82. Glaveckaite S, Valeviciene N, Palionis D, Puronaite R, Serpytis P, Laucevicius A. Prediction of long‐term segmental and global functional recovery of hibernating myocardium after revascularisation based on low dose dobutamine and late gadolinium enhancement cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2014;16:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Giordano C, Kuraitis D, Beanlands RS, Suuronen EJ, Ruel M. Cell‐based vasculogenic studies in preclinical models of chronic myocardial ischaemia and hibernation. Exp Opin Biol Ther. 2013;13:411–428. [DOI] [PubMed] [Google Scholar]
- 84. Weil BR, Suzuki G, Leiker MM, Fallavollita JA, Canty JM Jr. Comparative efficacy of intracoronary allogeneic mesenchymal stem cells and cardiosphere‐derived cells in swine with hibernating myocardium. Circ Res. 2015;117:634–644. [DOI] [PMC free article] [PubMed] [Google Scholar]


