Abstract
BACKGROUND:
Morbid obesity is rising around the world. Surgery is a selective treatment intervention for it. Since most of the surgeons use weight loss for evaluating of the morbid obesity surgical outcomes and paying attention to the the quality of life (QOL) and body image evaluation are rare, this study aimed to assess the QOL and body image in pre- and postsurgery with other interventions.
MATERIALS AND METHODS:
This case–control study was done on 200 morbidly obese patients (n = 100 in each group) who referred to the obesity clinic in Shiraz. The data were collected by Body Image Concern Inventory and 12-item Short Form Survey. The data were analyzed by t-test, Pearson correlation coefficient test, analysis of variance, and regression analysis. P = 0.05 was considered as significant.
RESULTS:
The paired t-test showed a significant difference in mean scores of body image (P < 0.001) and all dimensions of the QOL (P < 0.001) in the case and control groups. In the case group, there was a significant difference between the mean scores of the QOL and the different categories of body mass index (BMI) in postsurgery (P < 0.05) and the different mean scores of body image and the different categories of BMI in pre- and postsurgery wasn’t significant (P > 0.05). Age was a predictor variable for the QOL of morbidly obese persons after surgery (P < 0.001). After surgery, men showed better QOL than women (P < 0.001).
CONCLUSION:
Final results indicated that body image and QOL defects caused by obesity could be more improvement after surgery. This study can promote health-care team's knowledge about holistic supporting of all dimensions’ QOL of obese individuals. It is suggested that supporting interventions should be done as effective methods of maintenance for effects of weight loss methods such as surgery.
Keywords: Body image, morbid obesity, quality of life, surgery
Introduction
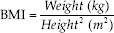
Obesity, as a chronic disease, causes physical problems such as cancers, cardiovascular disease (myocardial infarction and hypertension), musculoskeletal disorders, diabetes, and stroke.[1] It is usually classified by body mass index (BMI), and morbid obesity is defined as BMI ≥40 kg/m2.[2] Today, all types of obesity affected more than a third of the worldwide population.[3] In Iran, the overweight and obesity prevalence has been estimated 42.8% and 57% for men and women, respectively.[4]
There are different treatments for obesity such as diet, exercise, medication, and behavioral therapy, but morbidly obese people can often treat by surgery.[5] Morbidly obese people stated poor physical, psychological, and quality of life (QOL) for the cause of seeking treatment interventions.[6] Furthermore, they suffer from psychosocial problems such as stress, anxiety, depression, low self-confidence, negative body image, social judgment, and lack of social attractiveness.[7] Body dissatisfaction has been recognized as a stimulant to restart previous or new treatment again.[8]
Although QOL is often associated with the researches on the morbid obesity and morbid obesity has negative effects on the QOL,[9] the surgeons usually measure weight loss as a main surgeries outcome.[10] While health-care providers should be notified to the health promotion and obesity prevention as much as obesity treatment.[11] Despite the evaluation of the relationship between BMI and QOL in the studies, the effect of BMI modification on the QOL is not clear;[12,13] some studies also have revealed the role of unknown factors in this relationship.[14,15]
Today, bariatric surgery considers as a successful method for the treatment of severe obesity and has good effects on weight loss.[16] However, additional skin is a common complication of huge weight reduction after morbid obesity surgery on the upper arms, breasts, abdomen, and thighs.[17] This malformed skin has negative consequences on the QOL, self-confidence, physical activity, and body image.[18]
Despite the importance of the QOL and body image in the morbid obesity, they have not been accurately defined in some studies that whether surgery can improve or reduce them. Furthermore, regarding the increasing statistics of bariatric surgeries for morbid obesity in Iran and the limited attention paid to the QOL and body image in morbidly obese people under surgery, the present study aimed to study the QOL and body image of morbidly obese patients in pre- and postsurgery with other interventions.
Materials and Methods
A pilot case–control design was conducted from December 2017 to May 2018. In this study, the target population included all morbidly obese people who referred to the Obesity Clinics of Shiraz University of Medical Sciences, Iran. The sample size was based on the previous studies,[19]α = 0.05, and using Statistical Software Components (SSC) which is often called the Boston College Archive; the sample size was estimated about 200:
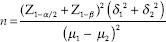
The samples divided into groups: the cases group that candidated for the surgery (n = 100) and the control group that gave other treatments (diet and exercise) (n = 100). The samples in each group were selected by simple random sampling method based on the table of random numbers. Since the researchers had a population of 200 and 200 was a three-digit number, they used the first three digits of the numbers listed on the chart based on the patient record number in the clinic. The researcher point to a spot on the chart randomly by closed eyes. Then, the researchers assumed that they selected a digit in the first column. After that, they went down to the next number. This method continued until we reached adequate sample size (n = 200). Inclusion criteria were individuals with BMI >35, from both genders (male and female), and age >18 years, having literacy and good mental and physical condition, and interesting to participate in the study. Patients who were diagnosed with serious chronic diseases or severe illness/injury (physical or mental) and if they were taking medications affecting weight and if they had a current or past severe psychiatric disorder were excluded from the study.
The study data were collected before and 3 months after surgery by a form including the demographic characteristics such as gender, age, weight, height, BMI, and two scales of the Body Image Concern Inventory (BICI) and Short Form-12 (SF-12) questionnaire. After receiving research approval, the researcher referred to the obesity clinics. The researcher asked the participants to fill informed consents form. After that, the researcher requested their demographic information and measured their weight and height. Then, she clarified how to answer two questionnaires about themselves. Finally, 100 questionnaires in each group were entered to the final analysis.
Weigh, height, and body mass index measurement
To measure weight, the researcher placed a standard and adjusted weight scale on a flat and firm surface. She asked the person to take off his shoes and heavy clothes and stand on the middle of the weight scale; then, the researcher recorded his weight.
To measure height, a meter was used perpendicular to a flat and rigid wall. The person was asked to stand in front of the meter without shoes. Then, we asked him to stick his/her legs and look straight, while the assessor flattened his hair with a ruler and recorded his height.[20] Furthermore, we calculated BMI by weight in kilograms divided by height in meters squared:[21]
Body Image Concern Inventory
The BICI included 19 items. It is scored using a 5-point Likert scale (1 = never, 2 = seldom, 3 = sometime, 4 = often, and 5 = always). To get a score of the body image, the items’ scores are combined together. The scores between 19–38, 38–57, and >57 in this test represent low, moderate, and severe body image concern, respectively.[22] The psychometric properties of this inventory were approved (α =0.88). In Iran, the Cronbach's alpha of the BICI was reported 0.95 and 0.89 in two researches.[23,24] In our study, content validity rate, content validity index, and the Cronbach's alpha coefficient were found 0.78, 0.90, and 0.87, respectively.
Short Form-12 questionnaire
This 12-item tool (12-item short form survey (Sf-12)) was designed to evaluate the QOL. This instrument was scored through a variable point Likert scale: ( Yes (Limited a lot) = 1 to No (Not limited at all) =3), (Yes = 1, No = 2), (Not at all = 5, Extremely = 1), and (All of the time (always) =1, None of the time (never) =6). Some of the questions (1, 8, 10, and 11) were scored revers. SF-12 consisted of 8 subscales: total self-concept of health, physical function, physical health, emotional problems, physical pain, social activity, vitality and vital energy, and mental health. To get a score of the QOL, items’ scores are combined together. The more score shows better the QOL. The scores between 12 and 24, 25 and 36, and 37 and 48 in this test represent weak, moderate, and good QOL, respectively. SF-12 was validated for the first time by test–retest reliability, and the Cronbach's alpha was reported 0.89 for physical dimension and 0.76 for mental dimension. Its validity was evaluated by the experimental validity and the construct validly that their results were acceptable.[25]
This questionnaire was validated in Iran. The Cronbach's alpha was reported 0.73 for physical dimension and 0.72 for mental dimension. Validity is evaluated by the convergent validity. Correlation between 4 subscales of physical component with total score and 3 subscales of mental component with total score were high.[26] In our study, the Cronbach's alpha coefficient was found 0.83.
Ethical considerations
The study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (IR.AJUMS.REC. 10, 1395). The participants voluntarily filled out the questionnaire after signing written informed consent.
Statistical analysis
The study data were analyzed using the Statistical Package for the Social Sciences (SPSS) for Windows (version 17) United States; 2010. Descriptive statistics were used to summarize the demographic characteristics. Moreover, Pearson correlation coefficient test was used to determine the relationships between the test scores. The higher the absolute value of the coefficient, the stronger the relationship will be.[27] Furthermore, the paired and the independent t-test, the one-way analysis of variance, and linear regression were used. Besides, P = 0.05 was considered as statistically significant.
Results
The study population included 200 morbidly obese persons, who referred to the obesity clinic of Shiraz University of Medical Sciences from December 2017 to May 2018 in Shiraz, Iran. Most of the participants in the case group were women (61.40%) and housewives (39.60%) and had diploma degree (43.60%) [Table 1].
Table 1.
Demographic characteristics of the participants (n=200)
| Variable | Case group (n=100), n (%) | Control group (n=100), n (%) |
|---|---|---|
| Gender | ||
| Male | 38 (38) | 42 (42) |
| Female | 62 (62) | 58 (58) |
| Marital status | ||
| Single | 24 (24) | 30 (30) |
| Married | 72 (72) | 63 (72) |
| Divorced | 4 (4) | 7 (7) |
| Education level | ||
| <Diploma | 15 (15) | 14 (14) |
| Diploma | 43 (43) | 40 (40) |
| Associate degree | 12 (12) | 15 (15) |
| Bachelor | 20 (20) | 25 (25) |
| Master | 10 (10) | 6 (6) |
| Job status | ||
| Housewife | 40 (40) | 46 (46) |
| Employee | 29 (29) | 21 (21) |
| Business man | 21 (21) | 26 (26) |
| Unemployed | 10 (10) | 7 (7) |
| Total (%) | 100 (100) | 100 (100) |
*Descriptive statistics
According to the results, the participants in the case group were 19–64 years old and their mean age was 38.35 ± 10.18 years. According to descriptive statistics, the participants had a mean weight 117.56 ± 23.01 kg (presurgery) and 80.49 ± 14.78 kg (postsurgery), mean height of 166.69 ± 10.20 cm, and BMI of 42.13 ± 6.20 kg/m2 (presurgery) and 28.84 ± 3.93 kg/m2 (postsurgery). The data showed a normal distribution by one-sample Kolmogorov–Smirnov test (P > 0.05).
The paired t-test showed a significant differences in the mean scores of the QOL (t = 17.84, P < 0.001) and body image concern (t = −16.59, P < 0.001) of morbidly obese persons in pre- and postsurgery [Table 2]. Furthermore, the mean scores of the QOL (t = 5.71, P < 0.001) and the body image concern (t = 2.58, P = 0.01) of the control group in before and after 3 months were different significantly.
Table 2.
The comparison of difference mean scores of body image and all dimensions of quality of life morbidly obese persons in pre- and postsurgery
| Test variable | Mean±SD | Paired t-test | ||
|---|---|---|---|---|
| Before | After | t | P | |
| Control | ||||
| Body image concern | 57.23±11.65 | 55.21±11.56 | 2.58 | 0.01 |
| QOL | 36.96±5.29 | 34.84±4.92 | 5.71 | <0.001 |
| Case | ||||
| Body image concern | 71.66±18.64 | 38.09±10.55 | −16.59 | <0.001 |
| QOL | 25.21±6.68 | 44.06±9.62 | 17.84 | <0.001 |
| Total self-concept of health | 1.78±0.97 | 4.05±0.94 | 18.45 | <0.001 |
| Physical function | 3.04±1.12 | 6.27±2.18 | 13.93 | <0.001 |
| Physical health | 2.74±1.55 | 5.74±2.66 | 9.92 | <0.001 |
| Emotional problems | 2.70±0.85 | 5.85±2.70 | 11.20 | <0.001 |
| Physical pain | 2.52±1.17 | 4.32±0.97 | 12.47 | <0.001 |
| Social activity | 3.18±1.57 | 4.60±1.16 | 6.65 | <0.001 |
| Vitality and vital energy | 2.64±1.04 | 4.26±1.20 | 10.37 | <0.001 |
| Mental health | 6.61±2.18 | 8.97±1.96 | 8.74 | <0.001 |
| BMI | 41.84±4.29 | 28.84±3.93 | −28.34 | <0.001 |
QOL=Quality of life, BMI=Body mass index, SD=Standard deviation
The results revealed a significant difference in the mean scores of total self-concept of health, physical function, physical health, emotional problems, physical pain, social activity, vitality and vital energy, and mental health and BMI in pre- and postsurgery (P < 0.001) [Table 2].
There was no significant difference between the mean scores of the QOL and the different categories of BMI in the presurgery, but in the postsurgery, it was significant (P < 0.05) and there was no significant between the mean scores of the body image concern and the different categories of BMI both in pre- and postsurgery (P > 0.05) [Table 3].
Table 3.
The difference between the mean scores of the quality of life and the mean scores of body image concern in the different categories of body mass index
| Time | Test | BMI categories | Mean±SD | Statistical test* | |
|---|---|---|---|---|---|
| F | P | ||||
| Before surgery | QOL | 35-40 | 25.31±6.43 | 1.091 | 0.34 |
| 40.01-50 | 24.93±6.83 | ||||
| >50 | 32.00±4.24 | ||||
| The body image concern | 35-40 | 72.37±17.55 | 0.261 | 0.77 | |
| 40.01-50 | 71.00±19.56 | ||||
| >50 | 80.00±2.82 | ||||
| After surgery | QOL | 18-25 | 42.89±9.61 | 3.13 | 0.04 |
| 25.01-30 | 42.89±9.61 | ||||
| >30 | 44.74±9.67 | ||||
| The body image concern | 18-25 | 39.10±11.38 | 0.94 | 0.39 | |
| 25.01-30 | 39.15±10.54 | ||||
| >30 | 35.73±10.45 | ||||
*The one-way ANOVA=Analysis of variance, QOL=Quality of life, BMI=Body mass index, SD=Standard deviation
The study finding showed that age and gender were not a significant predictor variable of the body image concern and the QOL pre- and postsurgery (P > 0.05), but in the postsurgery, age was a predictor variable of the QOL (P < 0.001) [Table 4]. The results revealed that there was no significant difference between the mean scores of the QOL and the body image concern between men and women in the pre- and postsurgery (P > 0.05), but in after surgery, the mean score of the QOL showed a significant difference between men and women (P < 0.001) [Table 5].
Table 4.
The regression analysis of the body image concern and quality of life based on age and gender pre- and postsurgery
| Time | Dependent variable | Predictors variable | β | Statistical test* | ||
|---|---|---|---|---|---|---|
| t | F | P** | ||||
| Before surgery | Body image concern | Age | −1.89 | −1.89 | 1.83 | 0.06 |
| Gender | 0.03 | 0.36 | 0.71 | |||
| QOL | Age | 0.05 | 0.50 | 0.74 | 0.61 | |
| Gender | −0.11 | −1.12 | 0.26 | |||
| After surgery | Body image concern | Age | −1.82 | −1.83 | 2.33 | 0.06 |
| Gender | −0.10 | −1.06 | 0.29 | |||
| QOL | Age | 0.008 | 0.08 | 7.77 | <0.001 | |
| Gender | −0.37 | −3.94 | 0.93 | |||
*Linear regression, **P=0.05. QOL=Quality of life
Table 5.
The comparison of difference mean score of quality of life and body image concern between morbidly obese men and women pre- and postsurgery
| Time | Test | |||||||
|---|---|---|---|---|---|---|---|---|
| QOL | Body image concern | |||||||
| Mean±SD | Independent t-test | Mean±SD | Independent t-test | |||||
| Male | Female | t | P | Male | Female | t | P | |
| Before | 26.15±7.60 | 24.62±6.04 | 1.11 | 0.26 | 70.97±17.68 | 72.08±19.33 | −0.28 | 0.77 |
| After | 48.60±9.74 | 41.27±8.48 | 3.96 | <0.001 | 39.60±12.63 | 37.16±9.04 | 1.12 | 0.26 |
SD=Standard deviation, QOL=Quality of life
Discussion
The study findings showed that the mean score of the QOL and the body image concern in the morbidly obese patients were different in pre- and postsurgery, which confirms our hypothesis. When the patients had a good feeling about their QOL and did not concern about the body shape, they satisfied by the surgery. It means that the improvement of the QOL and the body image caused by the surgery, so clinician should focus on them. This finding is consistent with the results of a descriptive study which shows that the body image should be considered as an important factor in the obesity management strategies. The study shows that targeting BMI only is not sufficient to improve the QOL of overweight and obese individuals, and those other variables, including perceptual factors, should be considered.[28]
These results were significant in the control group too, but their improvement in the scores of the QOL and the body image was not very highlighted and showed moderate the QOL and the body image. It is probably because of the control group didn’t give any supportive interventions during the study.
In the case group, the results showed that respondents judged to have improved their all dimension of the QOL and health after surgery. They experienced a better feeling about their health, physical and social function, and physical, emotional, and mental health. These results can help to the planning of nursing care before and after obesity surgery for health education and coping with any complications. Physical and chronic pain decreased after surgery. Several studies showed the same results.[29,30,31]
Another research has shown that obese people were not happy with their bodies, did not enjoy from going out, and received unkind nicknames.[32] In this study, participants had not good mental and emotional health before surgery, but after surgery, all participants satisfied with having more vitality and energy and social relationship improvement. Our results showed that participants reported lower concerns about their body after surgery, but in another research, obese people had not good body image because of loose and hanging skin following surgery.[33] This difference could be related to the supporting and regular following up patients after surgery in obesity clinics of Shiraz.
Our results indicated no difference between the mean scores of the body image in none of the different categories of BMI pre- and postsurgery. It consisted with result of a the study that showed no linear relationship between the body image and BMI.[34] However, some of the researchers found a one-way significant relationship between satisfaction with the body image and BMI in obese people, and overweight and obese participants reported significantly higher levels of negative body image than normal and underweight participants.[35] It is related to the type of this study's samples that had BMI >35, because of when the body weight is greater than a certain amount, body appearance becomes unpleasant and amount of dissatisfaction is the same in all of the morbid obesity categories.
Several studies have shown that a decrease in BMI is not necessarily associated with an improvement in the QOL.[12,13] However, the results of another study found individuals’ variability in the relationship between BMI and QOL.[36] These results are consisted with our finding that showed a difference between the mean scores of the QOL in different categories of BMI in postsurgery. These could be related to individuals with higher weight, lost weight faster or higher, and reported better QOL.
Furthermore, the role of confounding variables (age and gender) was evaluated, and the results of this study showed that age and gender were not a significant predictor variable for the QOL and the body image concern. This finding was consistent with part of findings of a cross-sectional study that indicated no significant relationship between the body image and gender, but age could be one of the main factors in decreasing body image.[37] Contrarily, another study found that satisfaction of boys is more than girls.[38] These differences could be related to the difference in the type of studied samples, because our samples were in adult age and fairly homogeneous.
In postsurgery, age was a predictor variable for the QOL in this study. It is Probably because the age is an important factor to influence on the persons’ responding to the surgical and anesthetic conditions. It means that the younger people had better situation than older people for surgery, so they experience better QOL.
The results revealed no difference of body image concern between men and women in pre- and postsurgery, but another study found that women are more influenced by all types of feedback than men, which can lead to body weight dissatisfaction and excessive attention paid to body image.[39] Furthermore, based on our results, the mean score of the QOL had a significant difference between men and women in after surgery and men had better QOL than women. In this regard, other researches showed that the body-related QOL perception in men is better than women because, moreover, women feel pressed by the media, peers, and couples to look slimmer and younger, and this is a transcultural phenomenon.[40]
This study has several limitations. Importantly, the current study performed only in Shiraz and on the morbidly obese people with small sample size, which means that the results are more likely to be generalizable to other cities and other types of obesity. Therefore, it is suggested that future studies could be done in other city and rural areas with larger sample size. Another limitation was that men participants were less than women. It was related to more prevalence of obesity in women population in the real world and also men less tented to participate in the study. Despite the limitations, this study improves the holistic evaluating of surgery outcomes including mental and physical health, physical and social activity, physical pain, and feeling of vitality and energy. Furthermore, our selected patients were from different genders, marital statuses, social classes, and education degrees.
On the other hand, one of the common problems in morbidly obese people is changing their size and shape and had physical, mental, and social problems which can reduce their QOL. Since the obese patients feel better about their life and body image after surgery, we recommended the clinicians to promote the QOL as the main aims of bariatric treatment. Therefore, further studies on the longitudinal effects of the QOL and the body image improvement in postsurgery are recommended. This study can help nurses, nutritionists, surgeons, and psychologists who provide holistic care for education and health promotion of morbidly obese patients. Furthermore, our findings highlight the QOL measurement as a suitable index for evaluation of treatment interventions of morbid obesity and comparison of their outcomes.
Conclusion
Since surgery can improve mental, physical, and social health of morbidly obese people, the QOL can be a good scale for surgeon and patients to understand health status in postsurgery period. Furthermore, the QOL and the body image improvement can motivate morbidly obese persons to maintain their weight loss. This research can verify helpful in improving health clinician, service provision, health-care costs, and public health policy knowledge, mental supporting of morbidly obese people, and their QOL. Furthermore, the present study is the basis for future research in providing evaluation of all of the surgery outcomes and not only amount of weight loss. Therefore, we emphasize the public awareness and health-care providers that obesity management should focus more on the monitoring and promotion of the patient's health and all of the QOL aspects, instead of the treatment of their obesity.
Financial support and sponsorship
This study was financially supported by Ahvaz Jundishapur University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The study is a part of Ph. D. thesis (NCRCCD-9416) of Negar Yazdani. The authors appreciate Ahvaz Jundishapur and Shiraz Universities of Medical Sciences for supporting the research, Nursing Care Research Center in Chronic diseases, and Colorectal Research Center. The authors also would acknowledge the Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance and also study’ participants.
References
- 1.Smith KB, Smith MS. Obesity statistics. Prim Care. 2016;43:121–35, ix. doi: 10.1016/j.pop.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Hruby A, Hu FB. The epidemiology of obesity: A big picture. Pharmacoeconomics. 2015;33:673–89. doi: 10.1007/s40273-014-0243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stevens GA, Singh GM, Lu Y, Danaei G, Lin JK, Finucane MM, et al. National, regional, and global trends in adult overweight and obesity prevalences. Popul Health Metr. 2012;10:22. doi: 10.1186/1478-7954-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarrafzadegan N, Kelishadi R, Siadat ZD, Esmaillzadeh A, Solhpour A, Shirani S, et al. Obesity and cardiometabolic risk factors in a representative population of Iranian adolescents and adults in comparison to a western population: The Isfahan healthy heart programme. Public Health Nutr. 2010;13:314–23. doi: 10.1017/S1368980009991029. [DOI] [PubMed] [Google Scholar]
- 5.Skyrud RV, Aaseth J, Birketvedt GS. Outpatient, multidisciplinary treatment of morbidly obese patients: A two-year retrospective study. Open Behav Sci J. 2011;5:28–32. Available on Jan 2019 from: https://www.benthamopen.com/DOWNLOAD-PDF/TOBSJ-5-28/ [Google Scholar]
- 6.Jepsen R, Aadland E, Robertson L, Kolotkin RL, Andersen JR, Natvig GK, et al. Physical activity and quality of life in severely obese adults during a two-year lifestyle intervention programme. J Obes. 2015;2015:314194. doi: 10.1155/2015/314194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Verhagen M. Body Image of Patients with Morbid Obesity before and After Bariatric Surgery. Clinical and Health Psychology (Master thesis) 2016 Jun;:5–16. [Google Scholar]
- 8.Abolhassani S, Irani MD, Sarrafzadegan N, Rabiei K, Shahrokhi S, Pourmoghaddas Z, et al. Barriers and facilitators of weight management in overweight and obese people: Qualitative findings of TABASSOM project. Iran J Nurs Midwifery Res. 2012;17:205–10. [PMC free article] [PubMed] [Google Scholar]
- 9.Charalampakis V, Seretis C, Daskalakis M, Fokoloros C, Karim A, Melissas J, et al. The effect of laparoscopic sleeve gastrectomy on quality of life: A prospective cohort study with 5-years follow-up. Surg Obes Relat Dis. 2018;14:1652–8. doi: 10.1016/j.soard.2018.06.016. [DOI] [PubMed] [Google Scholar]
- 10.Douglas IJ, Bhaskaran K, Batterham RL, Smeeth L. Bariatric surgery in The United Kingdom: A Cohort study of weight loss and clinical outcomes in routine clinical care. PLoS Med. 2015;12:e1001925. doi: 10.1371/journal.pmed.1001925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vine M, Hargreaves MB, Briefel RR, Orfield C. Expanding the role of primary care in the prevention and treatment of childhood obesity: A review of clinic- and community-based recommendations and interventions. J Obes. 2013;2013:172035. doi: 10.1155/2013/172035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laxy M, Holle R, Döring A, Peters A, Hunger M. The longitudinal association between weight change and health-related quality of life: The KORA S4/F4 cohort study. Int J Public Health. 2014;59:279–88. doi: 10.1007/s00038-013-0506-x. [DOI] [PubMed] [Google Scholar]
- 13.Döring N, de Munter J, Rasmussen F. The associations between overweight, weight change and health related quality of life: Longitudinal data from the stockholm public health cohort 2002-2010. Prev Med. 2015;75:12–7. doi: 10.1016/j.ypmed.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 14.Cox TL, Ard JD, Beasley TM, Fernandez JR, Howard VJ, Affuso O, et al. Body image as a mediator of the relationship between body mass index and weight-related quality of life in black women. J Womens Health (Larchmt) 2011;20:1573–8. doi: 10.1089/jwh.2010.2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hayward J, Millar L, Petersen S, Swinburn B, Lewis AJ. When ignorance is bliss: Weight perception, body mass index and quality of life in adolescents. Int J Obes (Lond) 2014;38:1328–34. doi: 10.1038/ijo.2014.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schigt A, Gerdes VE, Cense HA, Berends FJ, van Dielen FM, Janssen I, et al. Bariatric surgery is an effective treatment for morbid obesity. Neth J Med. 2013;71:4–9. [PubMed] [Google Scholar]
- 17.Colwell AS. Current concepts in post-bariatric body contouring. Obes Surg. 2010;20:1178–82. doi: 10.1007/s11695-010-0120-4. [DOI] [PubMed] [Google Scholar]
- 18.de Zwaan M, Georgiadou E, Stroh CE, Teufel M, Köhler H, Tengler M, et al. Body image and quality of life in patients with and without body contouring surgery following bariatric surgery: A comparison of pre – And post-surgery groups. Front Psychol. 2014;5:1310. doi: 10.3389/fpsyg.2014.01310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moraes JM, Caregnato RC, Schneider DS. Quality of life before and after bariatric surgery. Acta Paul Enferm. 2014;27:157–64. [Google Scholar]
- 20.Streur WJ, Hurlburt WB, Birch S. Measuring Height/Weight and Calculating BMI Guidelines for School. State of Alaska: Alaska Department of Health and Social Services/Division of Public Health. 2011 [Google Scholar]
- 21.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA. 2010;303:242–9. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 22.Littleton HL, Axsom D, Pury CL. Development of the body image concern inventory. Behav Res Ther. 2005;43:229–41. doi: 10.1016/j.brat.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 23.Basaknejad S, Ghafari M. The relationship between body image concern and psychological disorders in students. JBS. 2008;1:179–87. [Google Scholar]
- 24.Esmaeil Riahi M. Gender Differences in the Level of Body Image Satisfaction. 2012;9(3):5–33. (In press) [Google Scholar]
- 25.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Montazeri A, Vahdaninia M, Mousavi SJ, Omidvari S. The Iranian version of 12-item short form health survey (SF-12): Factor structure, internal consistency and construct validity. BMC Public Health. 2009;9:341. doi: 10.1186/1471-2458-9-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Polit DF, Beck CT. 9th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams and Wilkins; 2012. Nursing Research: Generating and Assessing Evidence for Nursing Practice. [Google Scholar]
- 28.Pétré B, Scheen AJ, Ziegler O, Donneau AF, Dardenne N, Husson E, et al. Body image discrepancy and subjective norm as mediators and moderators of the relationship between body mass index and quality of life. Patient Prefer Adherence. 2016;10:2261–70. doi: 10.2147/PPA.S112639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Melo IT, São-Pedro M. Musculoskeletal pain in lower limbs in obese patients before and after bariatric surgery. Arq Bras Cir Dig. 2012;25:29–32. doi: 10.1590/s0102-67202012000100007. Available on Jan 2019 from:http://www.scielo.br/pdf/abcd/v25n1/07.pdf . [DOI] [PubMed] [Google Scholar]
- 30.Grans R, Warth CF, Farah JF, Bassitt DP. Quality of life and prevalence of osteoarticular pain in patients submitted to bariatric surgery. Einstein. 2012;10:415–21. doi: 10.1590/s1679-45082012000400004. [DOI] [PubMed] [Google Scholar]
- 31.Wijhoven H, De Vet H, Picavet S. Explaining sex differences in chronic musculoskeletal pain in general population. Pain. 2006;124:158–66. doi: 10.1016/j.pain.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 32.Serrano AQ, Vasconcelos MG, Silva GA, Cerqueira MM, Pontes CM. Obese adolescents’ perceptions about the repercussions of obesity on their health. Rev Esc Enferm USP. 2010;44:25–31. [PubMed] [Google Scholar]
- 33.Klassen AF, Cano SJ, Scott A, Johnson J, Pusic AL. Satisfaction and quality-of-life issues in body contouring surgery patients: A qualitative study. Obest Surg. 2012;22:1527–34. doi: 10.1007/s11695-012-0640-1. [DOI] [PubMed] [Google Scholar]
- 34.Ghai A, Milosevic I, Laliberte M, Taylor VH, McCabe RE. Body image concerns in obese women seeking bariatric surgery. Ethn Inequal Health Soc Care. 2014;7:96–107. [Google Scholar]
- 35.Watkins JA, Christie C, Chally P. Relationship between body image and body mass index in college men. J Am Coll Health. 2008;57:95–100. doi: 10.3200/JACH.57.1.95-100. [DOI] [PubMed] [Google Scholar]
- 36.Cox TL, Zunker C, Wingo B, Thomas DM, Ard JD. Body image and quality of life in a group of African American women. Soc Indicator Res. 2010;99:531–40. [Google Scholar]
- 37.Sabeti F, Gorjian Z. The Relationship between the satisfaction of body image and self-esteem among obese Adolescents in Abadan, Iran. IJDO. 2013;5:126–31. [Google Scholar]
- 38.van den Berg PA, Mond J, Eisenberg M, Ackard D, Neumark-Sztainer D. The link between body dissatisfaction and self-esteem in adolescents: Similarities across gender, age, weight status, race/ethnicity, and socioeconomic status. J Adolesc Health. 2010;47:290–6. doi: 10.1016/j.jadohealth.2010.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Befort CA, Rickard KM. Gender similarities in response to figure-size feedback in a selected non-clinical population. Sex Roles. 2003;49:71–80. [Google Scholar]
- 40.van der Beek ES, Geenen R, de Heer FA, van der Molen AB, van Ramshorst B. Quality of life long-term after body contouring surgery following bariatric surgery: Sustained improvement after 7 years. Plast Reconstr Surg. 2012;130:1133–9. doi: 10.1097/PRS.0b013e318267d51d. [DOI] [PubMed] [Google Scholar]


