Abstract
Purpose
The aim of this umbrella review is to determine the effectiveness of LLLT in the treatment of LET and to provide recommendations based on this evidence.
Methods
A comprehensive and systematic review was undertaken using Medline, EBSCO and EMBASE. Systematic reviews or meta-analysis were included if they compared Laser with at least one of the following: (i) placebo, (ii) no treatment, (iii) another treatment, conservative (physical therapy intervention or medical) or operative of LET. Principal outcomes included the assessment of short and long-term effect on functional status, pain, grip strength (pain-free or maximum) and a global measure (overall improvement).
Results
Seven papers met the inclusion criteria for the umbrella review, Five papers were of moderate and two of low methodological quality. All reviews reported benefits associated with laser therapy Vs other intervention or placebo, however the significance of the identified benefits differed between studies and reviews. No review reported negative effects of laser therapy or harm to patients. All reviews noted significant variance between included studies with 2 reviews citing statistically significant heterogeneity. It is essential to consider this in the interpretation of these data.
Conclusion
This umbrella review found poor results for the effectiveness of LLLT in the management of LET. Therefore, further research with well-designed RCTs is required to provide meaningful evidence on the effectiveness (absolute and relative) of LLLT for the management of LET.
Keywords: Low Level Laser Therapy, Lateral elbow tendinopathy, Functional status, pain, grip strength overall improvement, umbrella review
Introduction
Lateral elbow tendinopathy (LET) appears to be the most appropriate term to use in clinical practice because all the other terms such as lateral epicondylitis, lateral epicondylalgia, lateral epicondylosis and/or tennis elbow make reference to inappropriate aetiological, anatomical and pathophysiological terms 1). LET is one of the most common lesions of the arm work-related or sport-related pain disorder. The condition is usually defined as a syndrome of pain in the area of the lateral epicondyle 2) that may be degenerative or failed healing tendon response rather than inflammatory 3). Hence, the increased presence of fibroblasts, vascular hyperplasia, proteoglycans and glycosaminoglycans together with disorganized and immature collagen may all take place in the absence of inflammatory cells 4). The most commonly affected structure is the origin of the extensor carpi radialis brevis (ECRB) 4). The dominant arm is commonly affected, the peak prevalence of LET is between 30 and 60 years of age 2, 5) and the disorder appears to be of longer duration and severity in women 3, 6).
The main complaints of patients with LET are pain and decreased function 2, 3) both of which may affect daily activities. Diagnosis is simple, and a therapist should be able to reproduce this pain in at least one of three ways: (1) digital palpation on the facet of the lateral epicondyle, (2) resisted wrist extension and/or resisted middle-finger extension with the elbow in extension, and (3) by getting the patient to grip an object. 2, 3, 5)
Although the signs and symptoms of LET are clear and its diagnosis is easy, to date, no ideal treatment has emerged. Many clinicians advocate a conservative approach as the treatment of choice for LET 2, 3, 7, 8). Physiotherapy is a conservative treatment that is usually recommended for LET pat ients 2–9). A wide ar ray of physiotherapy treatments such as electrotherapeutic (ultrasound, ESWT, TENS, iontophoresis) and non-electrotherapeutic modalities (exercise programs, soft tissue manipulation, and acupuncture). have been recommended for the management of LET 10–13). These treatments have different theoretical mechanisms of action, but all have the same aim, to reduce pain and improve function. Such a variety of treatment options suggests that the optimal treatment strategy is not known, and more research is needed to discover the most effective treatment in patients with LET 10–13).
Low Level Laser Therapy (LLLT) has attracted much interest in the last 25-30 years as it has been effectively applied to common musculoskeletal conditions with the aim to reduce pain and elevate quality of life 14). Its effectiveness on LET has been evaluated in previously published systematic reviews 11, 15–18). To our knowledge, there has been no umbrella review of LLLT for the management of LET. Therefore, the aim of this umbrella review is to determine the effectiveness of LLLT in the treatment of LET and to provide recommendations based on this evidence. We assessed the potential for bias in this literature, supported by the most robust epidemiological evidence.
Methods
This review was conducted using the Preferred Reporting Items of Systematic Reviews Meta-Analyses (PRISMA) guidelines 19). A systematic review design was selected to limit any bias in the selection and reporting of evidence.
Search strategy
A comprehensive and systematic review was undertaken using Medline, EBSCO and EMBASE. The search strategy included a combination of free text and Medical Subject Heading (MeSH) terms (Table 1). Only peer reviewed systematic reviews published after 1980 were included. Secondary searching of the reference lists of retrieved papers was undertaken to identify any additional reviews that met the inclusion criteria.
Table 1: Concepts searched and the keywords related to these concepts.
| Concept | Keywords |
|---|---|
| Lateral epicondylitis | Lateral elbow tendinopathy OR Lateral epicondylitis OR Tennis elbow OR Extensor tendonitis OR Extensor tendinosis OR Extensor tendinopathy OR Lateral elbow OR Fathers of the Bride's elbow OR Enthesopathy OR Epicondylosis |
| Treatment | Light Therapy OR Therapeutic Laser OR Low Level Laser Therapy OR Low Power Laser Therapy OR Low Level Laser OR Low energy Laser OR Soft Laser OR Low intensity level laser OR Low intensity OR laser therapy OR photo biostimulation laser OR photobiomulation laser OR medical laser OR laser therapy OR biostimulation laser OR bioregulation laser |
| Systematic Review | Systematic review OR Meta-analysis |
Selection procedures
Papers were retrieved based on whether the title and abstract or, if required, the full manuscript met the inclusion criteria for this review. Papers identified through the search were assessed based on the inclusion and exclusion criteria by two independently reviewers (KP and IM). Where there was discrepancy, all the authors discuss the issues and reached consensus.
Inclusion criteria
Systematic reviews or meta-analysis were included if they met the following inclusion criteria. Firstly, the paper needed to report a systematic review or meta-analysis of original intervention studies. Articles that did not meet the PRISMA 19) definition of a systematic review or meta-analysis were excluded. Secondly, the review had to compare Laser with at least one of the following: (i) placebo, (ii) no treatment, (iii) another treatment, conservative (physical therapy intervention or medical) or operative. Finally, due to resource constraints and ease of access, reviews that were published in any other than English were excluded from the analysis.
Population of interest were patients diagnosed with lateral elbow tendinopathy, or lateral elbow increased by pressure on the lateral epicondyle and during resisted dorsiflexion of the wrist.
Data extraction
The data were extracted into a custom-build form based on tools used in other systematic reviews of reviews 20) by two reviewers (KP and IM). The form contained categories regarding the characteristics and results of the included reviews. All data was compared and where differences were identified, the authors discuss issues and reached a consensus decision.
Where the original reviews did not report a meta-analysis of results comparing only laser with any other comparator, we performed this ourselves where the data were available. The inverse variance method with random effects was used to obtain an estimate of the pooled mean difference.
Methodological quality
A two-stage process was undertaken to evaluate both the type of evidence contained in each included review, and the quality of the review process used. In the first stage of this process, the level of evidence was graded using the Scottish Intercollegiate Guidelines Network (SIGN) hierarchy 21) (Table 2). In the second stage of this process, the quality of included systematic reviews and meta-analyses were assessed using the AMSTAR score 22), a tool to assess the methodological quality of systematic reviews. The AMSTAR score has been previously validated as a measure of quality in research reviews 22). Two reviewers independently scored each review using AMSTAR tool (KP and IM) and any disparities were discussed with a third reviewer (DL) until consensus was reached.
Table 2: SIGN hierarchy of evidence.
| Level of Evidence | Descriptor |
|---|---|
| 1++ | High quality meta-analyses, systematic reviews of RCTs, or RCTs with a very low risk of bias |
| 1+ | Well-conducted meta-analyses, systematic reviews, or RCTs with a low risk of bias |
| 1− | Meta-analyses, systematic reviews, or RCTs with a high risk of bias |
| 2++ | High quality systematic reviews of case control or cohort or studies High quality case control or cohort studies with a very low risk of confounding or bias and a high probabili-ty that the relationship is causal |
| 2+ | Well-conducted case control or cohort studies with a low risk of confounding or bias and a moderate proba-bility that the relationship is causal |
| 2− | Case control or cohort studies with a high risk of confounding or bias and a significant risk that the relation-ship is not causal |
| 3 | Non-analytic studies, e.g. case reports, case series |
| 4 | Expert opinion |
Outcomes
Principal outcomes included the assessment of short and long-termeffect on functional status, pain, grip strength (pain-free or maximum) and a global measure (overall improvement).
Results
Fourteen papers were identified by the search strategy and assessed against the umbrella review inclusion criteria 2,9–11,13,15–18,23–27) All reviewers agreed that seven papers met the inclusion criteria for the umbrella review 2, 10, 11, 15–18). Papers were excluded if they did not distinguish individuals with lateral elbow tendinopathy (tennis elbow), from those in other disease groups, the intervention did not involve the effects of laser therapy or did not report a formal systematic review. The flowchart in Figure 1 outlines the process for selecting the included systematic reviews.
Figure 1:
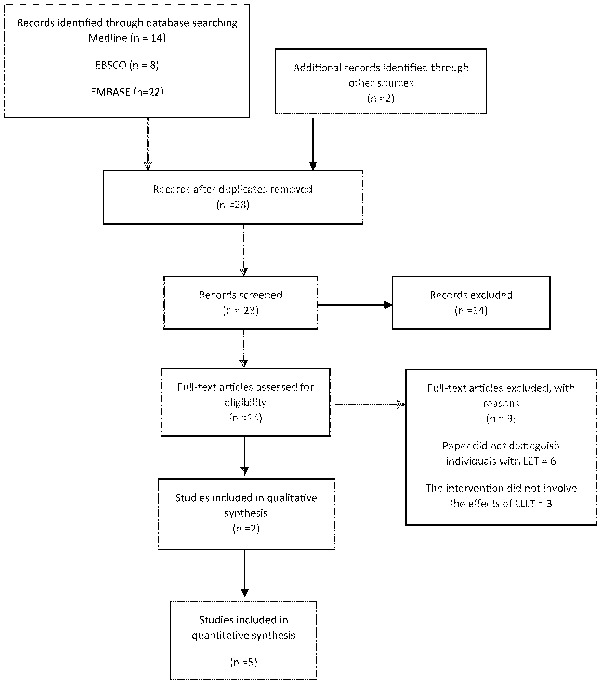
Study Selection
Studies included in quantitative synthesis
Five papers 2, 11, 15, 17, 18) were of moderate and two 10, 16) of low methodological quality, respectively. Table 3 provides details of the AMSTAR quality assessment, with explanations regarding the scoring decisions. The quality features of included systematic reviews are well or high quality meta-analyses or systematic reviews of RCTs with low or a very low risk of bias presented in SIGN grading system too.
Table 3: AMSTAR scores for the methodological quality of included reviews and SIGN hierarchy of the level of evidence of included reviews.
| AMSTAR | SIGN | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Was an ‘a priori’ design provided? | 2. Was there duplicate study selection and data extraction? | 3. Was a compre-hensive literature search performed? | 4. Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 5. Was a list of studies (included and excluded) provided? | 6. Were the characteris-tics of the included studies provided? | 7. Was the scientific quality of the included studies assessed and document-ed? | 8. Was the scientific quality of the included studies used appropri-ately in formulating conclu-sions? | 9. Were the methods used to combine the findings of studies appropri-ate? | 10. Was the likelihood of publication bias assessed? | 11. Was the conflict of interest included? | ||||
| Smidt, et al., 2003, [11] | Yes | X | X | X | X | X | X | X | 7 | 1++ | ||||
| No | X | X | X | |||||||||||
| Can't Answer | ||||||||||||||
| Not applicable | X | |||||||||||||
| Trudel, et al., 2004, [10] | Yes | X | X | X | X | 4 | 1+ | |||||||
| No | X | X | X | X | X | |||||||||
| Can't Answer | ||||||||||||||
| Not applicable | X | X | ||||||||||||
| Bjordal, et al., 2008, [15] | Yes | X | X | X | X | X | X | X | X | 8 | 1++ | |||
| No | X | X | ||||||||||||
| Can't Answer | ||||||||||||||
| Not applicable | X | |||||||||||||
| Sims, Miller and Elfar 2014, [16] | Yes | X | X | X | X | 4 | 1− | |||||||
| No | X | X | X | X | ||||||||||
| Can't Answer | ||||||||||||||
| Not applicable | X | X | X | |||||||||||
| Sayegh and Strauch, 2015, [18] | Yes | X | X | X | X | X | X | X | 7 | 1+ | ||||
| No | X | X | X | X | ||||||||||
| Can't Answer | ||||||||||||||
| Not applicable | ||||||||||||||
| Weber, et al., 2015, [17] | Yes | X | X | X | X | X | X | X | 7 | 1+ | ||||
| No | X | X | X | X | ||||||||||
| Can't Answer | ||||||||||||||
| Not applicable | ||||||||||||||
| Bisset, et al., 2015, [2] | Yes | X | X | X | X | X | X | X | X | 8 | 1+ | |||
| No | X | |||||||||||||
| Can't Answer | ||||||||||||||
| Not applicable | X | X | ||||||||||||
In some reviews it was possible to compare outcomes between various types of intervention, whilst in others various interventions were combined in the analysis. This variation is a reflection of the current state of the literature and the significant variety of operational definitions of laser therapy between studies included in the reviews.
A diverse range of outcomes was measured across the reviews. As can be seen in Table 4 and 5, four reviews investigated short-term effect of pain 2, 11, 15, 17), and three focused on long-term effect of pain 2, 11, 15). Pain scores for both short-term and long-term effect were measured in most of the studies using either a continuous visual analogue scale (PVAS) or an ordinal points system. Four reviews investigated short effect of function 2, 11, 15, 18) and three focused on long effect of function 2, 11, 15) (Table 6 and 7). They reported the dichotomous rating of success through a global improvement or patient satisfaction scale either short-term or/and long-term effect. Grip strength was reported in most reviews as either maximum grip strength (MGS) 2, 17) or pain-free grip strength (PFGS) 2, 15) (Table 8 and 9). The number of studies synthesized in the included reviews varied between 3 and 13 studies 7, 28–41).
Table 4: Summary table of included reviews - short term effect on pain.
| Study | Included Studies | N | Mean | SD | N | Mea | SD | WMD (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Bjordal, et al., 2008 | Tendon Application 904nm | |||||||
| Palimieri, 37) | 15 | 45 | 14 | 15 | 15.3 | 11 | 29.70 (20.69, 38.71) | |
| Vasselijen, et al. 40) | 15 | 16 | 12 | 15 | 6 | 12 | 10.00 (1.41, 17.59) | |
| Løgdberg-Andersson, Mutzell and Hazel, 34) | 73 | 10 | 25 | 69 | −1 | 25.8 | 11.00 (2.64, 19.36) | |
| Stergioulas, 39) | 15 | 29.3 | 25.2 | 15 | 11.54 | 24.88 | 17.76 (−0.16, 25.68) | |
| Lam and Cheing, 33) | 21 | 20.9 | 26.2 | 18 | 2.2 | 29 | 18.70 (1.23, 36.17) | |
| Tendon Application 820nm and 1064nm | ||||||||
| Krasheninnikoff, et al. 32) | 18 | 19 | 36 | 18 | 14 | 35 | 5.00 (−18.20, 28.20) | |
| Papadopoulos, et al. 38) | 15 −1 | 20.5 | 16 | 14 | 21.2 −15.00 (−29.68. −0.32) | |||
| Basford, Sheffield and Cieslak, 28) | 23 | 13.4 | 29.9 | 24 | 17 | 36.8 | −3.60 (−25.57, 18.37) | |
| Acupoint application technique 904nm | ||||||||
| Lundeberg, Haker and Thomas, 35) | 38 | 26 | 20 | 19 | 22 | 20 | 4.00 (−7.01, 15.01) | |
| Tendon Application 632nm versus brace | ||||||||
| Oken, et al., 36) | 20 | 28 | 12 | 20 | 14 | 9 | 14.00 (7.43, 20.57) | |
| Total: 10.24 (3.04, 17.45) | ||||||||
| Weber, et al., 2015 | Basford, et al. 28) | 23 | 47.7 | 45 | 23 | 34.3 | 28 | 13.40 (−8.26, 35.06) |
| Stergioulas, 39) | 31 | 52.5 | 20.82 | 25 | 23.2 | 14.8 | 29.30 (20.10, 38.50) | |
| Total: 24.45 (10.24, 38.65)1 | ||||||||
| Smidt, et al., 2003 | SMD(95% CI) | |||||||
| Laser Vs Placebo | ||||||||
| Vasseljen, et al. 40) | - | - | - | - | - | - | −0.25 (−0.96, 0.47) | |
| Laser versus US + Friction Massage | ||||||||
| Vasseljen, et al. 40) | - | - | - | - | - | - | 0.92 (0.17, 1.67) | |
| Bisset, et al., 2015 | Laser v placebo (NdYAG 204 mW/cm2) | |||||||
| Basford, Sheffield and Cieslak, 28) | - | - | - | - | - | - | 0.37 (−0.21 to 0.94) | |
| Laser v placebo (GaAs 30 mW/830 nm) | ||||||||
| Krasheninnikoff, et al. 32) | - | - | - | - | - | - | 0.08 (−0.58 to 0.73) | |
Calculate on a Random effect model - Mean Difference using Review Manager V. 5.0, I2 = 42% P=0.19
Table 5: Summary table of included reviews - long term effect on pain.
| Study | Included Studies | N | Mean | SD | N | Mea | SD | WMD (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Bjordal, et al., 2008 | Tendon Application 904nm | |||||||
| Vasselijen, et al. 41) | 15 | 16 | 12 | 16 | 6 | 12 | 10 (1.41, 18.59) | |
| Stergioulas, 39) | 15 | 42 | 22.9 | 16 | 20.46 | 23.8 | 21.54 (4.83, 38.25) | |
| Lam and Cheing, 33) | 21 | 36.6 | 23.2 | 18 | 13.3 | 29.3 | 23.3 (6.52, 40.08) | |
| Tendon Application 632nm versus brace | ||||||||
| Oken, et al. 36) | 20 | 28 | 12 | 20 | 14 | 9 | 14 (7.43, 20.57) | |
| Acupoint application 904nm | ||||||||
| Lundeberg, Haker and Thomas, 35) | 38 | 26 | 20 | 19 | 22 | 20 | 4 (−7.01, 15.01) | |
| Tendon Application 1064 nm | ||||||||
| Basford, Sheffiled and Cieslak, 28) | 23 | 31.4 | 36 | 24 | 32.5 | 28 | −1.10 (−19.59, 17.39) | |
| Total: 11.80 (7.54, 16.07) | ||||||||
| Smidt, et al., 2003 | SMD(95% CI) | |||||||
| Laser Vs Placebo | ||||||||
| Vasselijen, et al. 41) | - | - | - | - | - | - | −0.46 (−1.19, 0.27) | |
| Lundeberg, Haker and Thomas, 35) | - | - | - | - | - | - | −2 (−2.77, −1.22) | |
| SMD(95% CI) | ||||||||
| Laser versus US + Friction Massage | ||||||||
| Vasselijen, et al. 41) | - | - | - | - | - | - | 0.84 (0.09, 1.58) | |
| SMD(95% CI) | ||||||||
| Laser versus laser | ||||||||
| Lundeberg, Haker and Thomas, 35) | - | - | - | - | - | - | −1.00 (−1.67, −0.33) | |
| Bisset, et al., 2015 | SMD(95% CI) | |||||||
| Laser v placebo (NdYAG 204 mW/cm2) | ||||||||
| Basford, Sheffiled and Cieslak, 28) | - | - | - | - | - | - | 0.58 (−0.01 to 1.17) | |
| SMD(95% CI) | ||||||||
| Laser v placebo (GaAs 30 mW/830 nm) | ||||||||
| Krasheninnikoff, et al. 32) | - | - | - | - | - | - | 0.03 (−0.62 to 0.69) | |
| Laser v placebo (HeNe 632.8 nm, 1.56 mW; GaAs 904 nm, 0.07 mW) | ||||||||
| Lundeberg, Haker and Thomas, 35) | - | - | - | - | - | - | 0.98 (0.30 to 1.66) | |
Table 6: Summary table of included reviews - short term effect on overall improvement.
| Study | Included Studies | Treatment Group (n/N) | Control Group (n/N) | RR (95% CI) Fixed |
|---|---|---|---|---|
| Sayegh, Robert and Strauch, 2015 | Haker and Lundeberg 42) | 12/18 | 13/22 | 1.13 (0.70, 1.82) |
| Haker and Lundeberg 7) | 18/23 | 9/19 | 1.65 (0.98, 2.78) | |
| Total = 1.35 (0.93, 1.96)1 | ||||
| Smidt, et al., 2003 | Laser Vs Placebo | |||
| Vasseljen, 41) | - | - | 0.81 (0.61, 1.06) | |
| Haker and Lundeberg 7) | - | - | 1.45 (0.96, 2.20) | |
| Haker and Lundeberg 31) | - | - | 0.87(0.65, 1.16) | |
| Krasheninnikoff, et al. 32) | - | - | 1.07 (0.82, 1.39) | |
| Gudmundsen and Vikne, 29) | - | - | 0.72 (0.60, 0.87) | |
| Laser versus US + Friction Massage | ||||
| Vasseljen, 41) | 1.09 (0.73, 1.62) | |||
| Bjordal, et al., 2008 | Tendon Application 904nm | |||
| Palimieri, 37) | 14/15 | 9/15 | 1.56 (1.01, 2.40) | |
| Gudmundsen and Vikne, 29) | 42/47 | 18/45 | 2.23 (1.54, 3.24) | |
| Haker and Lundeberg 31) | 16/29 | 12/29 | 1.33 (0.77, 2.30) | |
| Vasseljen, 41) | 12/15 | 8/15 | 1.5 (0.88, 2.57) | |
| Løgdberg-Andersson, Mutzell and Hazel, 34) | 47/74 | 35/68 | 1.23 (0.92, 1.65) | |
| Tendon Application 820nm (+/−40) | ||||
| Krasheninnikoff, et al. 32) | 11/18 | 10/18 | 1.10 (0.63, 1.91) | |
| Acupoint application technique 904nm | ||||
| Haker and Lundeberg 77) | 10/23 | 17/26 | 0.66 (0.39, 1.15) | |
| Total = 1.36 (1.16, 1.60) | ||||
| Bisset, et al., 2015 | Laser v placebo (GaAs 30 mW/830 nm) | |||
| Krasheninnikoff, et al. 32) | - | - | 1.10 (0.63 to 1.91) | |
Calculate on a Random effect model - Mean Difference using Review Manager V. 5.0, I2 = 12% P=0.29
Table 7: Summary table of included reviews - long term effect on overall improvement.
| Study | Included Studies | Treatment Group (n/N) | Control Group (n/N) | RR (95% CI) Fixed |
|---|---|---|---|---|
| Smidt, et al., 2003 | Laser Vs Placebo | |||
| Vasseljen, 41) | - | - | 0.67 (0.39, 1.14) | |
| Haker and Lundeberg 7) | - | - | 0.95 (0.51, 1.75) | |
| Haker and Lundeberg 31) | - | - | 0.93 (0.56, 1.53) | |
| Lundeberg, Haker and Thomas, 35) | - | - | 1.00 (0.63, 1.59) | |
| Laser versus US + Friction Massage | ||||
| Vasseljen, 41) | - | - | 1.60 (0.68, 3.77) | |
| Bjordal, et al., 2008 | Tendon Application 904nm | |||
| Haker and Lundeberg 7) | 42/47 | 18/45 | 2.23 (1.54, 3.24) | |
| Vasseljen, 41) | 12/16 | 8/15 | 1.5 (0.88, 2.57) | |
| Acupoint application technique 904nm | ||||
| Haker and Lundeberg 7) | 17/23 | 17/26 | 1.13 (0.78, 1.64) | |
| Total: 1.68 (1.32, 2.13) | ||||
| Bisset, et al., 2015 | Laser v placebo (GaAs 30 mW/830 nm) | |||
| Krasheninnikoff, et al. 32) | - | - | 1.10 (0.63 to 1.91) | |
Table 8: Summary table of included reviews - Maximum handgrip strength.
| Study | Included Studies | Experimental - LLLT - Contro |
||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Total | Mean | SD | Total | Mean Difference (95% CI) | ||
| Weber, et al., 2015 | Basford, Sheffiled and Cieslak, 28) | 32.1 | 33.6 | 23 | 34.5 | 37 | 24 | −2.40 (−22.59, 17.79) |
| Lam and Cheing, 33) | 25.29 | 8.26 | 21 | 19.56 | 9.75 | 18 | 5.73 (0.01, 11.45) | |
| Bisset, et al., 2015 | Laser v placebo (NdYAG 204 mW/cm2) | |||||||
| Basford, Sheffiled and Cieslak, 28) | - | - | - | - | - | - | −0.07 (−0.64 to 0.51) | |
Table 9: Summary table of included reviews - Pain free grip strength.
| Study | Included Studies | Mean | SD | Total | Mean | SD | Total | Mean Difference (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Bisset, et al., 2015 | Laser v placebo (HeNe 632.8 nm, 5 mW; GaAs 904 nm, 4 mW) | |||||||
| Haker and Lundeberg, 7) | - | - | - | - | - | - | −0.37 (−0.89 to 0.15) | |
| Laser v placebo (GaAs 904 nm, 12 mW) | ||||||||
| Haker and Lundeberg, 30) | - | - | - | - | - | - | 0.47 (−0.10 to 1.04) | |
| Bjordal, et al., 2008 | Tendon Application 904nm | |||||||
| Haker and Lundeberg 7) | 25 | 34.3 | 25 | 0 | 33.6 | 24 | 0.72 (0.14, 1.30) | |
| Vasseljen, 41) | 50 | 20.1 | 15 | −20 | 20.10 | 15 | 3.39 (2.22, 4.55) | |
| Stergioulas, 39) | 7.2 | 12.9 | 15 | 1.84 | 11.6 | 15 | 0.43 (−0.3, 1.15) | |
| Lam and Cheing, 33) | 49.10 | 11.9 | 21 | 13 | 13.5 | 18 | 2.79 (1.89. 3.7) | |
| Tendon Application 820nm and 1064nm | ||||||||
| Papadopoulos, et al. 38) | −1 | 11 | 14 | 9 | 10 | 15 | −0.93 (−1.7, −0.15) | |
| Acupoint application technique 904nm | ||||||||
| Lundeberg, Haker and Thomas, 35) | 41.5 | 26 | 38 | 38.2 | 23 | 19 | 0.13 (−0.42, 0.68) | |
| Haker and Lundeberg 7) | 17 | 18 | 23 | 10 | 18 | 26 | 0.38 (−0.18, 0.95) | |
| Tendon Application 632nm versus brace | ||||||||
| Oken, et al. 36) | 10.5 | 18 | 20 | −7,5 | 14 | 20 | 1.09 (0.42, 1.76) | |
| Total : 0.66 (0.42, 0.90) | ||||||||
All reviews reported benefits associated with laser therapy Vs other intervention or placebo, however the significance of the identified benefits differed between studies and reviews. No review reported negative effects of laser therapy or harm to patients. All reviews noted significant variance between included studies with 2 reviews 17, 18) citing statistically significant heterogeneity. It is essential to consider this in the interpretation of these data.
Pain
Short-Term effect
Four reviews which investigated laser therapy and pain relief reported short-term effect of pain as an outcome measure 2, 11, 15, 17). There was some variation in finding of “laser” use between reviews. Bjordal, et al. 15) reported continuous data for pain relief from 10 trials in a way, which made possible the statistical pooling of the results. At the first observation after the end of the treatment period, LLLT was significantly better than controls with a WMD of 10.2 mm [95% CI: 3.0 to 17.5] in favour of LLLT on a 100 mm VAS (p = 0.005). In a subgroup of five trials 33, 34, 37, 39, 41) where 904 nm LLLT was administered directly to the tendon, LLLT reduced pain by 17.2 mm [95% CI: 8.5 to 25.9] more than placebo (p = 0.0001). One trial 36) with 632 nm LLLT, showed significantly better results for LLLT than a wrist brace and ultrasound therapy, but none of the results from trials with wavelengths of 820 nm or 1064 nm 28, 32, 38), or acupoint application technique 35) were significantly different from placebo. Weber, et al. 17) reported two LLLT studies 28, 39), one low frequency electrical stimulation study and one PEMF study reported sufficient data to be analyzed. Combined treatment groups gained 24.45 [95% CI = 10.24, 38.65) (I2 = 42%) units of pain relief (difference from baseline). Finally Smidt, et al. 11) and Bisset, et al. 2) from 2 trials each 28, 32, 40, 41), showed no statistically significant pains' effects on Short-term follow-up (≤ 6 weeks). The results are summarized in Table 4.
Long-Term effect
Three reviews which investigated laser therapy and pain relief reported long-term effect on pain as an outcome measure 2, 11, 15). Bjordal, et al. 15) reported six trials providing continuous follow-up data on a 100 mm VAS measured between 3 and 8 weeks after the end of treatment 28, 33, 35, 36, 39, 41). The combined WMD was 11.80 mm [95% CI: 7.5 to 16.1] in favour of LLLT. Contradictory results were reported for intermediate (6 weeks to 6 months) and longterm follow-up (≥ 6 months) assessments in Smidt, et al. 11) review, and for comparisons with other physiotherapeutical modalities 35, 40, 41). Based on the best evidence synthesis there is insufficient evidence to demonstrate either benefit or lack of effect of laser for lateral epicondylitis. On long term follow up of six months and one year, Bisset, et al 2), found no evidence of an effect seen with pooled data in laser over other or non-therapy 28, 32, 35). The results are summarized in Table 5.
Overall Improvement
Short-Term effect
Four reviews which investigated laser therapy and overall improvement reported short term effect, as an outcome measure 2, 11, 15, 18). Sayegh, Robert and Strauch 18) assessed the overall improvement and found that neither laser therapy nor nonsurgical treatment was favored (RR = 1.35, 0.93–1.96); p = 0.12; I2 = 12%). Smidt, et al. 11) reported no statistically significant effects on short-term follow-up (< 6 weeks) in overall improvement. Bjordal, et al. 15) included seven trials 29, 31, 32, 34, 37, 40, 42) presented data in a way which allowed us to pool data for global improvement. LLLT was significantly better than placebo with an overall relative risk for improvement equal to 1.36 [95% CI: 1.16 to 1.60] (p = 0.002). In a subgroup analysis of five trials 29, 34, 37, 40, 42) where 904 nm LLLT was used to irradiate the symptomatic tendon, the relative risk for global improvement was significantly higher for LLLT that than placebo [RR 1.53, 95% CI 1.28 to 1.83] (p < 0.0001). In the remaining two trials 31, 32) where LLLT was administered to acupoints or with 820 nm wavelength, the relative risk for global improvement was not significantly different from placebo [RR 0.80, 95% CI 0.50 to 1.22]. Bisset, et al 2) included only one study 32) investigated overall improvement with a null treatment effect. The results are summarized in Table 6.
Long Term effect
Three reviews which investigated laser therapy and overall improvement reported long term effect as an outcome measure 2, 11, 15). Smidt, et al. 11) reported no statistically significant effects for intermediate (6 weeks to 6 months) and long-term follow-up (≥ 6 months) on overall improvement. For global improvement, Bjordal, et al. 15) included three trials 29, 31, 40) providing data suitable for statistical pooling, and the pooled RR was calculated to 1.68 [95% CI: 1.32 to 2.13] in favour of LLLT. Bisset, et al 2) included only one study 32) investigated overall improvement with a null treatment effect. The results are summarized in Table 7.
Grip Strength
Maximum handgrip strength
Two reviews investigated laser therapy effect and Maximum handgrip strength, as an outcome measure 2, 17). Weber, et al. 17) included two LLLT studies which reported maximum grip strength 28, 33). Comparison between treatment and control groups at the end of studies showed a non-significant result. Bisset, et al. 2) included only one study investigated Maximum handgrip strength with a null treatment effect 28). The results are summarized in Table 8.
Pain free grip strength
Two reviews investigated laser therapy effect and Pain free grip strength, as an outcome measure 2, 15). Bisset, et al. 2) included two studies investigated pain free grip strength with no statistically significant results 7, 30). Bjordal, et al. 15) reported significantly better results for LLLT in comparison to placebo with SMDs of 0.66 [95% CI: 0.42 to 0.90] [p < 0.0001). When trials were subgrouped by application technique and wavelengths, only trials with irradiation of tendons and wavelengths 632 nm 36) or 904 nm 33, 39, 43, 44), showed positive results versus control with SMDs at 1.09 [95% CI: 0.42 to 1.76] and 1.30 [95% CI: 0.91 to 1.68], respectively. The results are summarised in Table 9.
Studies included in qualitative synthesis
The extensive search for relative reviews revealed two more reviews 10, 16) which could not be used for further meta-analysis. The reason was the lack of additional information in the tables and the result sessions of those papers. Both reviews concluded to ambiguous results after comparing active LLLT treatment with placebo treatment.
In more detail, Trudel, et al. 10) appraised the 8 studies included using the Sackett's Level of Evidence 45) and separated them in two groups; level 1a and 2a (6 studies of higher level of evidence) 28, 30, 32, 35, 38, 43, 45) and level 2b (2 studies of lower level of evidence) 7, 44) (Table 10). All studies included at least three of the following outcome measures: a) grip strength, b) pain severity, c) an incremental lifting test. Results of higher level studies showed that the active LLLT was not significantly better than the placebo laser for any of these outcomes in the treatment of lateral epicondylitis. On the other hand lower level evidence indicated that there was a significant short-and long-term improvement on pain, grip strength and incremental lifting.
Sims, et al., 16) examined non-surgical treatment in lateral epicondylitis. Among other treatment, they also researched active laser treatment versus different types of laser and placebo laser. Authors reported the results of nine studies and separated them in two categories; early studies (studies from 1987 to 1996) 32, 35, 38, 43, 44) and later studies (studies from 2000 to 2010) 28, 33, 39, 46). The outcome measures used were different for each study with most dominant the improvement in pain, grip strength and functional assessment (Table 10). The results showed that early studies of laser therapy did not show an effect of treatment whereas more recent investigations did show substantial improvement for patients treated with laser therapy over those who received placebo therapy. In more detail, Lundeberg, et al. 35) studied two different types of laser (pulsed Ga-As and continuous He-Ne), with no difference between treatment and placebo groups up to 3 months after treatment. Four more RCTs studied the effect of either a Ga-As or Ga-Al-As laser versus sham laser therapy. Varying levels of energy were delivered per point in each study, and follow-up periods ranged from 7 weeks to 1 year. Three of those studies 32, 38, 42) did not report significant difference in results between laser therapy and placebo whereas a fourth study 40) did.
Table 10: Results from studies included in qualitative synthesis.
| Study | Studies included | Outcome measures | Results |
|---|---|---|---|
| Trudel et al., 2004 |
1a+2a studies Lundeberg, Haker and Thomas, 35) Haker and Lundeberg, 31) Krasheninnikoff, et al. 32) Basford, Sheffield and Cieslak, 28) Haker and Lundeberg, 42) Papadopoulos, et al. 38) 2b studies Vasseljen, 41) Haker and Lundeberg, 42) |
Grip strength, pain severity and an incremental lifting test All studies included at least these 3 outcomes |
6 level 1a and 2a studies (Sackett's Level of Evidence) examined a total of 294 subjects and scores ranging between 29 to 44 out of 48 suggested that active laser is not significantly better than placebo laser for any of these outcomes in the treatment of lateral epicondylitis. Alternatively, two level 2b studies examined a total of 30 participants with a total of 93 subjects and scores ranging from 31 to 39 out of 48 indicated that there was significant short- and long-term improvement on pain, grip strength, and incremental lifting. |
| Sims et al., 2014 |
Early studies Lundeberg, Haker and Thomas, 35) Haker and Lundeberg 42) Krasheninnikoff, et al. 32) Papadopoulos, et al. 38) Vasseljen, 41) Later studies Basford, Sheffield and Cieslak, 28) Stergioulas, 39) Lam and Cheing, 33) Emanet, et al. 46) |
Improvement in pain, grip strength, and functional assessment Different outcomes for each study |
Early Studies Three studies did not demonstrate a difference in results between laser therapy and placebo (although one of these studies did not include 25 % of subjects lost to follow-up) whereas a fourth study did. Later studies Three studies reported significant positive long and short-term results of active LLLT versus placebo. One study showed no significant short-term difference between active LLLT versus placebo |
Results of more recent studies conflict with those found previously. Basford et al. 28) conducted a double-blind RCT with a Nd-YAG laser and placebo which did not demonstrate a difference in outcome at 4 weeks. However, a study by Stergioulas, 39) combined plyometric exercise with Ga-As laser or placebo laser and found a significant (p < 0.05) improvement in VAS and strength at 8 and 16 weeks in the active treatment group. A similar study by Lam and Chein, 33) looking only at short-term outcomes of Ga-As laser treatment at 3 weeks found comparable results (p < 0.0125). Emanet et al., 46) also found positive results of LLLT in their double-blind RCT using a Ga-As laser and additional physical therapy for both groups with a statistically significant (p < 0.05) difference with respect to improved pain, grip strength, and functional assessment in favor of the treatment group at 12 weeks.
Discussion
In this umbrella review, the effectiveness of LLLT was assessed by searching databases in combination with reference checking for systematic reviews and meta analyses. It is the first umbrella review to assess the effectiveness of LLLT in the management of LET. Poor results for LLLT in LET were found. LLLT has attracted much interest as it is applied to common musculoskeletal conditions such as LET 14). Helium-neon (HeNe) and gallium arsenide (GaAs) are the two most common types of LLLT. It is primarily used in practice for pain alleviation, assisting tissue healing at cellular level, and improvement of function by inference. However, Gam, et al. 47) concluded that LLLT has no effect on pain in musculoskeletal syndromes and Mulcahy, et al. 48) concluded that LLLT acts primarily as a placebo.
Although results showed poor LLLT effectiveness in the LET management, the LLLT cannot be ruled out from the list of LET treatment. The reason is that LLLT is a dose-response modality, 7, 49) and the optimal treatment dose has obviously not yet have been identified. Analysis of the dose response was difficult to be tested, because of poor reporting of parameters and a dearth of clinical studies comparing the effectiveness of different treatment modality variables 47).
LLLT is the form of light therapy that is usually recommended as a supplement to the exercise program in the management of tendinopathies 49). LLLT has been shown to have potential to modulate the degenerative process. It is known that LET, is a degenerative process and not inflammatory one. In addition, the biostimulatory effects of LLLT have been shown to reduce cell apoptosis 50) and promote collagen fiber synthesis within a low-range therapeutic window of 0.4-4 J = cm2 51, 52) there were methodological shortcomings in the included systematic reviews. Many of the studies failed to provide adequate long-term follow-up, blinding, and power calculations. The use of standardized outcome measures was also lacking. Finally, the protocol of the intervention was not described in full detail, making replication difficult. Therefore, well designed RCTs are needed to investigate the effectiveness of LLLT in the management of LET.
Our umbrella review relied on results reported within the previously published systematic reviews and meta-analyses. There was a considerable clinical and methodological heterogeneity in terms of populations evaluated, doses, comparators, outcome measures, lengths of follow-ups, etc. The searches were restricted in published English language papers, thereby omitting some potentially important unpublished reviews in languages other than English. We did not evaluate whether there was evidence for small-study effects using funnel plot asymmetry, because of insufficient data. Another one limitation is that the definition of groups and intervention that employed by each systematic review, may not be entirely accurate.
Conclusion
This umbrella review found poor results for the effectiveness of LLLT in the management of LET. However, LLLT cannot be ruled out, as it is a dose-response modality, and the optimal treatment dose needs yet to be discovered. The current review recommends that practitioners do not use LLLT as sole treatment for LET but can be used in combination with other suggested treatments. In addition, the included studies had methodological shortcomings. Therefore, further research with well-designed RCTs is required to provide meaningful evidence on the effectiveness (absolute and relative) of LLLT for the management of LET.
References
- 1: Stasinopoulos D., Johnson M.I., “Lateral elbow tendinopathy” is the most appropriate diagnostic term for the condition commonly referred-to as lateral epicondylitis", Med. Hypotheses. 67 (2006) 1400-1402. 10.1016/j.mehy.2006.05.048. [DOI] [PubMed] [Google Scholar]
- 2: Bisset L.M., Vicenzino B., Physiotherapy management of lateral epicondylalgia, J. Physiother. 61 (2015) 174-181. 10.1016/j.jphys.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 3: Coombes B.K., Bisset L., Vicenzino B., Management of Lateral Elbow Tendinopathy: One Size Does Not Fit All, J. Orthop. Sport. Phys. Ther. 45 (2015) 938-949. 10.2519/jospt.2015.5841. [DOI] [PubMed] [Google Scholar]
- 4: Kraushaar B., Nirschl R., Current concepts review: tendinosis of the elbow (tennis elbow), J Bone Jt. Surg. 81-A (1999) 259-278. 10.1197/j.jht.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 5: Vicenzino B., Wright A., Lateral epicondylalgia I: epidemiology, pathophysiology, aetiology and natural history, Phys. Ther. Rev. 1 (1996) 2334. 10.1179/ptr.1996.1.1.23. [DOI] [Google Scholar]
- 6: Waugh E.J., Jaglal S.B., Davis A.M., Tomlinson G., Verrier M.C., Factors Associated with Prognosis of Lateral Epicondylitis after 8 Weeks of Physical Therapy, Arch. Phys. Med. Rehabil. 85 (2004) 308-318. 10.1016/S0003-9993(03)00480-5. [DOI] [PubMed] [Google Scholar]
- 7: Haker E., Lundeberg T., Lateral epicondylalgia: report of noneffective midlaser treatment., Arch. Phys. Med. Rehabil. 72 (1991) 984-8. http://www.ncbi.nlm.nih.gov/pubmed/1953322 [PubMed] [Google Scholar]
- 8: Hong Q.N., Durand M.-J., Loisel P., Treatment of lateral epicondylitis: where is the evidence?, Joint. Bone. Spine. 71 (2004) 369-73. 10.1016/j.jbspin.2003.05.002. [DOI] [PubMed] [Google Scholar]
- 9: Luk J.K.H., Tsang R.C.C., Leung H.B., Lateral epicondylalgia: Midlife crisis of a tendon, Hong Kong Med. J. 20 (2014) 145-151. 10.12809/hkmj134110. [DOI] [PubMed] [Google Scholar]
- 10: Trudel D., Duley J., Zastrow I., Kerr E.W., Davidson R., MacDermid J.C., Rehabilitation for patients with lateral epicondylitis: a systematic review., J. Hand Ther. 17 (2004) 243-266. 10.1197/j.jht.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 11: Smidt N., Assendelft W.J.J., Arola H., Malmivaara A., Greens S., Buchbinder R., van der Windt D.A.W.M., Bouter L.M., Green S., Buchbinder R., Van Der Windt D., Effectiveness of physiotherapy for lateral epicondylitis: a systematic review., Ann. Med. 35 (2003) 51-62. 10.1080/07853890310004138. [DOI] [PubMed] [Google Scholar]
- 12: Labelle H., Guibert R., Joncas J., Newman N., Fallaha M., Rivard C.H., Lack of scientific evidence for the treatment of lateral epicondylitis of the elbow. An attempted meta-analysis., J. Bone Joint Surg. Br. 74 (1992) 646-651. http://www.ncbi.nlm.nih.gov/pubmed/1388172. [DOI] [PubMed] [Google Scholar]
- 13: Bisset L., Paungmali A., Vicenzino B., Beller E., A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia., Br. J. Sports Med. 39 (2005) 411-22-22. 10.1136/bjsm.2004.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14: Cotler H.B., Chow R.T., Hamblin M.R., Carroll J., The Use of Low Level Laser Therapy (LLLT) For Musculoskeletal Pain, MOJ Orthop. Rheumatol. 116 (2015) 1477-1490. 10.15406/mojor.2015.02.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15: Bjordal, J.M., Lopes-Martins R.A., Joensen J., Couppe C., Ljunggren A.E., Stergioulas A., Johnson M.I., A systematic review with procedural assessments and meta-analysis of low level laser therapy in lateral elbow tendinopathy (tennis elbow)., BMC Musculoskelet. Disord. 9 (2008) 75. 10.1186/1471-2474-9-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16: Sims S.E.G., Miller K., Elfar J.C., Hammert W.C., Non-surgical treatment of lateral epicondylitis: a systematic review of randomized controlled trials, Hand. 9 (2014) 419-446. 10.1007/s11552-014-9642-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17: Weber C., Thai V., Neuheuser K., Groover K., Christ O., Efficacy of physical therapy for the treatment of lateral epicondylitis: a meta-analysis., BMC Musculoskelet. Disord. 16 (2015) 223. 10.1186/s12891-015-0665-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18: Sayegh E.T., Strauch R.J., Does Nonsurgical Treatment Improve Longitudinal Outcomes of Lateral Epicondylitis Over No Treatment? A Meta-analysis, Clin. Orthop. Relat. Res. 473 (2014) 1093-1107. 10.1007/s11999-014-4022-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19: Moher J A.D., Liberati A, Tetzlaff J, PRISMA 2009 Flow Diagram, Prism. Statement. 6 (2009) 1000097. 10.1371/journal.pmed1000097. [DOI] [Google Scholar]
- 20: Smith V., Devane D., Begley C.M., Clarke M., Methodology in conducting a systematic review of systematic reviews of healthcare interventions, BMC Med. Res. Methodol. 11 (2011). 10.1186/1471-2288-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21: Harbour R., Miller J., A new system for grading recommendations in evidence based guidelines, BMJ. 323 (2001) 334-336. 10.1136/bmj.323.7308.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22: Shea B.J., Hamel C., Wells G.A., Bouter L.M., Kristjansson E., Grimshaw J., Henry D.A., Boers M., AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews, J. Clin. Epidemiol. 62 (2009) 1013-1020. 10.1016/j.jclinepi.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 23: Alberta F., CORR Insights®: Does Nonsurgical Treatment Improve Longitudinal Outcomes of Lateral Epicondylitis Over No Treatment? A Meta-analysis, Clin. Orthop. Relat. Res. 473 (2015) 1108-1110. 10.1007/s11999-014-4085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24: Boisaubert B., Brousse C., Zaoui A., Montigny J.P., Les traitements non chirurgicaux de la tendinopathie des ??picondyliens, Ann. Readapt. Med. Phys. 47 (2004) 346-355. 10.1016/j.annrmp.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 25: Borkholder C.D., Hill V.A., Fess E.E., The efficacy of splinting for lateral epicondylitis: a systematic review, J. Hand Ther. 17 (2004) 181-199. 10.1197/j.jht.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 26: Gebremariam L., Hay E.M., van der Sande R., Rinkel W.D., Koes B.W., Huisstede B.M.A., Subacromial impingement syndrome--effectiveness of physiotherapy and manual therapy., Br. J. Sports Med. 48 (2014) 1202-1208. 10.1136/bjsports-2012-091802. [DOI] [PubMed] [Google Scholar]
- 27: Pfefer M.T., Cooper S.R., Uhl N.L., Chiropractic Management of Tendinopathy: A Literature Synthesis, J. Manipulative Physiol. Ther. 32 (2009) 41-52. 10.1016/j.jmpt.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 28: Basford J.R., Sheffield C.G., Cieslak K.R., Laser therapy: a randomized, controlled trial of the effects of low intensity Nd:YAG laser irradiation on lateral epicondylitis., Arch. Phys. Med. Rehabil. 81 (2000) 1504-10. 10.1053/apmr.2000.17812. [DOI] [PubMed] [Google Scholar]
- 29: Gudmundsen J.V.J., Vikne J., Laserbehandling av epicondylitis humerie og rotatorcuffsyndrom, Nor Tidskr Idrettsmed. 2 (1987) 6-15. [Google Scholar]
- 30: Haker E., Lundeberg T., Pulsed ultrasound treatment in lateral epicondylalgia, Laser. 12 (1991) 7 https://www.ncbi.nlm.nih.gov/pubmed/1962154 [PubMed] [Google Scholar]
- 31: Haker E., Lundeberg T., Is low-energy laser treatment effective in lateral epicondylalgia?, J. Pain Symptom Manage. 6 (1991) 241-6. http://www.ncbi.nlm.nih.gov/pubmed/2030299 [DOI] [PubMed] [Google Scholar]
- 32: Krasheninnikoff M., Ellitsgaard N., Rogvi-Hansen B., Zeuthen A., Harder K., Larsen R., Gaardbo H., No effect of low power laser in lateral epicondylitis., Scand. J. Rheumatol. 23 (1994) 260-3. http://www.ncbi.nlm.nih.gov/pubmed/7973480 [DOI] [PubMed] [Google Scholar]
- 33: Lam L.K.Y., Cheing G.L., Effects of 904-nm low-level laser therapy in the management of lateral epicondylitis: a randomized controlled trial., Photomed. Laser Surg. 25 (2007) 65-71. 10.1089/pho.2006.2047. [DOI] [PubMed] [Google Scholar]
- 34: Lögdberg-Andersson M., Mützell S., Hazel Å., Low level laser therapy (LLLT) of tendinitis and myofascial pains-a randomized, double-blind, controlled study, LASER Ther. 9 (1997) 79-85. 10.5978/islsm.9.79. [DOI] [Google Scholar]
- 35: Lundeberg T., Haker E., Thomas M., Effect of laser versus placebo in tennis elbow., Scand. J. Rehabil. Med. 19 (1987) 135-8. http://www.ncbi.nlm.nih.gov/pubmed/3441775 [PubMed] [Google Scholar]
- 36: Oken O., Kahraman Y., Ayhan F., Canpolat S., Yorgancioglu Z.R., Oken O.F., The short-term efficacy of laser, brace, and ultrasound treatment in lateral epicondylitis: a prospective, randomized, controlled trial., J. Hand Ther. 21 (2008) 63-7; quiz 68. 10.1197/j.jht.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 37: Palmieri B., Stratified double blind crossover study on tennis elbow in young amateur athletes using infrared lasertherapy., Med. Laser Rep. 1 (1984). [Google Scholar]
- 38: Papadopoulos E., Smith R., Cawley M., Mani R., Low-level laser therapy does not aid the management of tennis elbow, Clin. Rehabil. 10 (1996) 9-11. 10.1177/026921559601000103. [DOI] [Google Scholar]
- 39: Stergioulas A., Effects of low-level laser and plyometric exercises in the treatment of lateral epicondylitis., Photomed. Laser Surg. 25 (2007) 205-13. 10.1089/pho.2007.2041. [DOI] [PubMed] [Google Scholar]
- 40: Vasseljen O., Høeg N., Kjeldstad B., Johnsson a, Larsen S., Low level laser versus placebo in the treatment of tennis elbow., Scand. J. Rehabil. Med. 24 (1992) 37-42. http://www.ncbi.nlm.nih.gov/pubmed/1604260. [PubMed] [Google Scholar]
- 41: Vasseljen O., Low-level Laser versus Traditional Physiotherapy in the Treatment of Tennis Elbow, Physiotherapy. 78 (1992) 329-334. 10.1016/S0031-9406(10)61481-2. [DOI] [Google Scholar]
- 42: Haker E., Lundeberg T., Laser treatment applied to acupuncture points in lateral humeral epicondylalgia. A double-blind study, Pain. 43 (1990) 243-247. 10.1016/0304-3959(90)91078-W. [DOI] [PubMed] [Google Scholar]
- 43: Haker E., Lundeberg T., Laser treatment applied to acupuncture points in lateral humeral epicondylalgia. A double-blind study., Pain. 43 (1990) 243-7. http://www.ncbi.nlm.nih.gov/pubmed/2087335 [DOI] [PubMed] [Google Scholar]
- 44: Vasseljen O., Høeg N., Kjeldstad B., Johnsson A., Larsen S., Low level laser versus placebo in the treatment of tennis elbow., Scand. J. Rehabil. Med. 24 (1992) 37-42. http://www.ncbi.nlm.nih.gov/pubmed/1604260 [PubMed] [Google Scholar]
- 45: Sackett D.L., Rules of evidence and clinical recommendations on the use of antithrombotic agents., Chest. 95 (1989) 2S-4S. http://www.ncbi.nlm.nih.gov/pubmed/2914516 [PubMed] [Google Scholar]
- 46: Emanet S.K., Altan L.I., Yurtkuran M., Investigation of the effect of GaAs laser therapy on lateral epicondylitis., Photomed. Laser Surg. 28 (2010) 397-403. 10.1089/pho.2009.2555. [DOI] [PubMed] [Google Scholar]
- 47: Gam A.N., Thorsen H., Lønnberg F., The effect of low-level laser therapy on musculoskeletal pain: a meta-analysis., Pain. 52 (1993) 63-6. 10.1016/0304-3959(93)90114-5. [DOI] [PubMed] [Google Scholar]
- 48: Mulcahy D., McCormack D., McElwain J., Wagstaff S., Conroy C., Low level laser therapy: a prospective double blind trial of its use in an orthopaedic population, Injury. 26 (1995) 315-317. 10.1016/0020-1383(95)00048-E. [DOI] [PubMed] [Google Scholar]
- 49: Bjordal J.M., Couppe C., Ljunggren A.E., Low Level Laser Therapy for Tendinopathy. Evidence of A Dose-Response Pattern, Phys. Ther. Rev. 6 (2001) 91-99. 10.1179/ptr.2001.6.2.91. [DOI] [Google Scholar]
- 50: Carnevalli C.M.M., Soares C.P., Zângaro R.A., Pinheiro A.L.B., Silva N.S., Laser Light Prevents Apoptosis on Cho K-1 Cell Line, J. Clin. Laser Med. Surg. 21 (2003) 193-196. 10.1089/104454703768247756. [DOI] [PubMed] [Google Scholar]
- 51: Loevschall H., Arenholt-Bindslev D., Effect of low level diode laser irradiation of human oral mucosa fibroblasts in vitro., Lasers Surg. Med. 14 (1994) 347-354. [DOI] [PubMed] [Google Scholar]
- 52: Reddy G.K., Stehno-Bittel L., Enwemeka C.S., Laser photostimulation of collagen production in healing rabbit Achilles tendons, Lasers Surg. Med. 22 (1998) 281-287. . [DOI] [PubMed] [Google Scholar]


