ABSTRACT
Purpose
The purpose of this study was to investigate reductions of muscle stiffness induced by static stretching in older and younger men.
Methods
Twenty older (62–83 yr) and 20 younger (21–24 yr) men were recruited. Ankle dorsiflexion static stretching was consisted of 90 s × 5 repetitions. Before and after the stretching, the dorsiflexion range of motion (RoM), passive plantar flexion torque, and shear modulus (an index of stiffness) of the medial (MG) and lateral gastrocnemius and the soleus were measured.
Results
RoM, passive torque, and shear modulus of the triceps surae measured at the maximal dorsiflexion angle before stretching were significantly lower for the older group than the younger group. This suggests a weak stretching intensity for older compared with younger people. The stretching significantly improved RoM for both groups. For the older group, a significant reduction in passive torque was only observed at a 15° dorsiflexion angle, and the shear modulus was significantly decreased only for the distal region of MG. For the younger group, passive torque was significantly reduced for the entire RoM, and a significant decrease in shear modulus was found for the central and distal regions of MG and lateral gastrocnemius. A significant correlation between the muscle shear modulus measured at the maximal dorsiflexion angle before stretching and a stretching-induced decrease in muscle shear modulus was observed for older and younger participants. This indicates that the higher stretching intensity can reduce more muscle stiffness.
Conclusion
Static stretching can reduce muscle stiffness regardless of age, although the stretching effect on muscle stiffness was limited for older people. This might be due to a lower stretching intensity for older than younger people.
Key Words: FLEXIBILITY, RANGE OF MOTION, SHEAR MODULUS, ELASTOGRAPHY, GASTROCNEMIUS, SOLEUS
Populations around the world are aging rapidly. As a result, concern about maintaining the health of older people is increasing. Regular exercise is highly recommended for older people to maintain and/or improve physical (1) and mental health (2). However, it is difficult for some older people even to perform activities of daily living because of age-related loss of physical abilities. Flexibility is an essential physical ability. Reduced flexibility with age is well known (3), and this impairs body balance and functional ability for older people (4). This leads to an increased risk of falls (5) and interferes with activities of daily living. Therefore, regaining flexibility can be beneficial for older people.
Static stretching is a popular and safe exercise that improves flexibility. The effectiveness of static stretching to increase joint range of motion (RoM) and reduce joint resistance was demonstrated in young people using a dynamometer (6). For older people, static stretching can also improve RoM (7), although an 8-wk stretching program showed no reduction in joint resistance (8). As stretching is thought to change muscle tension perception, that is, stretch tolerance (9), and/or muscle stiffness (10), the effect of static stretching on muscle stiffness may be small for older people compared with younger people. Muscle stiffness is considered to influence joint flexibility (11), postural balance (12), and injury risk (13). Therefore, if static stretching reduces muscle stiffness, it could be beneficial in terms of fall prevention and quality of life improvement, especially for older people. However, because RoM and joint torque are also affected by factors other than muscle stiffness, for example, stretch tolerance and nonmuscular tissues, the effect of static stretching on muscle stiffness cannot be judged from the change in RoM and joint torque measured by a dynamometer. On the other hand, ultrasound shear wave elastography (SWE) is known as a quantitative and noninvasive method to assess the localized stiffness index (shear modulus) of biological tissues regardless of their size. The validity of stiffness measurements by means of this technique was confirmed by previous studies using an artificial phantom (14,15) and mammalian muscles (16), and the repeatability was ascertained by in vivo human muscle studies (17,18). Using this method, it was reported that static stretching could reduce the stiffness of plantar flexors (19,20) and knee flexors (21,22) in young people. However, the effect of stretching on muscle stiffness in older people has scarcely been explored.
The effect of stretching is influenced by its intensity. The increase in joint RoM and decrease in passive joint stiffness are greater when stretching is performed at the maximal tolerable joint angle rather than a submaximal angle (23). Similarly, a previous study revealed a reduction in muscle stiffness when stretching was conducted at 80% of RoM, but not at 60% or 40% RoM (24). It has also been reported that the stretching-induced reduction in muscle stiffness is more notable in stiffer muscles during stretching (20,22). Based on these studies, if muscle stiffness does not reach an adequate level during static stretching, muscle stiffness will not be reduced by the stretching. In previous studies, lower limb muscles were more compliant in older than younger counterparts (17,25) or were similar between them (26,27), despite poorer joint flexibility. This suggests that muscle stiffness in a stretching position in older people is lower than that in younger people and that the stretching effect on muscle stiffness could be age dependent. Furthermore, static stretching by older people could be less effective for regaining functional ability and/or reducing injury risk by reducing muscle stiffness as mentioned previously.
The aims of the present study were to assess 1) differences in the stiffness of each muscle of the triceps surae at the maximal dorsiflexion angle in a stretching position between older and younger men, and 2) changes in muscle stiffness induced by static stretching in older and younger men. We hypothesized that 1) stiffness of the triceps surae in older men would be lower than that in younger men in a stretching position, and 2) the stretching effect on muscle stiffness in older men would be negligible in contrast with younger men.
METHODS
Subjects
Twenty older men (age, 72 ± 5 yr; height, 167.3 ± 6.0 cm; weight, 68.5 ± 10.2 kg) and 20 younger men (age, 22 ± 1 yr; height, 172.5 ± 6.4 cm; weight, 67.1 ± 10.6 kg) participated voluntarily. The sample size was estimated to detect a stretching effect for a three-way repeated ANOVA (α error = 0.05, power = 0.80) using the G*Power statistical power analysis software. Effect size was predicted to be 0.54 based on the results of our previous study (22) that reported an acute stretching effect on hamstring muscles. The calculated sample size was 15. Therefore, 20 participants were recruited for each group. None of the participants had any apparent neurological or orthopedic disorders as confirmed by self-reporting. Participants were asked to refrain from strenuous exercise for 24 h before the testing. Written informed consent was obtained from each participant. The procedures were approved by the ethics committee of the Shibaura Institute of Technology and conducted in accordance with the Declaration of Helsinki.
Procedures
The participants lay prone on the bench of a dynamometer (CON-TREX MJ; PHYSIOMED, Schnaittach, Germany) with their hips and knees fully extended. The center of the lateral malleolus of the right foot was visually aligned to the dynamometer’s rotational axis. The right foot was firmly secured to the foot plate of the dynamometer with a nonelastic strap. Before the RoM measurement, five successive ankle joint rotations were performed at 5°·s−1 between 30° of plantar flexion (PF30) and 15° dorsiflexion (DF15; the neutral position [NP] was defined as 0°) to familiarize the participants with the passive dorsiflexion motion and to avoid any conditioning effect on muscle stiffness (20). Passive dorsiflexion at 1°·s−1 from PF30 to the maximal dorsiflexion angle determined based on the onset of pain for each participant was performed once to define the RoM. The ankle joint angle was returned immediately to the plantar flexed position to avoid a stretching effect on muscle stiffness. After the RoM measurement, the muscle stiffness was assessed by ultrasound SWE. Ten minutes later, static stretching was performed. Immediately after the stretching (POST), the RoM and muscle stiffness were reassessed in a similar manner to the measurements made before stretching (PRE). Lastly, maximal voluntary isometric contraction of the plantar flexors was performed for 3 s in NP to normalize electromyographic (EMG) signals during ultrasound SWE measurements. The ankle joint angle, passive torque, and EMG data were stored simultaneously on a personal computer using a 16-bit analog-to-digital converter (PowerLab 16/35; ADInstrument, Bella Vista, Australia). Sampling frequency was set at 1 kHz.
Static stretching
The static stretching involved five repetitions with no interval between repetitions. For each stretch, the right ankle was passively dorsiflexed from PF30 to the maximal dorsiflexion angle at 1°·s−1 and was fixed there for 90 s, and then returned to PF30 at 10°·s−1. The determination method of the maximal dorsiflexion angle was the same as for the RoM measurement (i.e., onset of pain). The present stretching protocol was decided to use referring previous studies (e.g., Ref. (22)), which reported clear effects of static stretching on RoM, passive joint torque, and muscle shear modulus.
Ultrasound SWE
An ultrasonic apparatus (ACUSON S2000; Siemens Medical Solutions, Ann Arbor, MI, USA) coupled with a linear transducer array (9 L4 Transducer, 4–9 MHz; Siemens Medical Solutions) was used to assess the shear wave speed for the shear modulus (an index of stiffness) calculation of the central region of the medial gastrocnemius (MGcentral), the distal region of the MG (MGdistal), the lateral gastrocnemius (LG), and the soleus (Fig. 1). Because MGdistal is the stiffest region among the lower leg muscles (28), a large stretching effect on MGdistal stiffness was expected. Hence, we assessed shear wave speed for not only MGcentral but also MGdistal. The shear wave speeds of MGcentral, LG and the soleus were measured at 30% of the lower leg length from the popliteal crease to the lateral malleolus, and that of MGdistal was measured slightly proximal to the distal myotendinous junction of MG. The mediolateral location of the probe was initially at the center of the tissue width. When intramuscular blood vessels and thick connective tissues were visible on an ultrasonographic image at the probe location, the position of the probe was moved mediolaterally to accurately assess the muscle shear wave speed. The ultrasound probe was placed with water-soluble transmission gel, and its orientation was carefully aligned to the fascicle direction of each muscle. The shear wave speed of each muscle was quantified before and after stretching at four joint angles, that is, PF30, NP, DF15, and RoM at PRE, in that order. The measurement order for muscles was random for each participant, although the order before and after the stretching was the same within participants. An elastographic image with a color map of shear wave speed was acquired once by an experienced examiner (>4 yr experience). The quality of the shear wave speed measurement was ensured using the ultrasonic apparatus system, which indicates the quality by displaying color-coded images. When green pixels, which indicate high-quality, occupied >75% of the area of a color-coded image within the shear wave speed color map region of interest, the elastographic image was stored.
FIGURE 1.
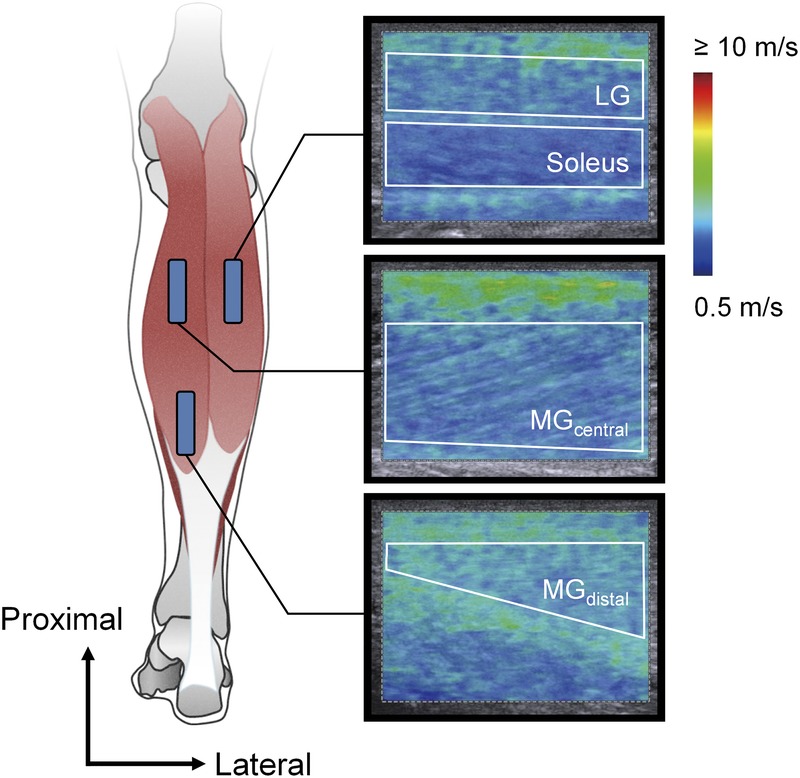
Schematic representation of ultrasound probe locations and typical examples of ultrasound shear wave elastographic images with a shear wave speed color scale. The area surrounded by the white line on each elastographic image represents the region of interest for shear modulus analysis.
EMG
Muscle activities of MG, LG, and the soleus were measured using an EMG system (Bagnoli 8 EMG System, Delsys, Natick, MA, USA) to ensure that muscular activity during muscle stiffness measurements were not modulated before and after stretching. Preamplified bipolar active surface EMG electrodes (electrode shape, parallel bar; size, 1 mm width ×10 mm length; interelectrode distance, 10 mm; DE-2.1, Delsys) with band-pass filtering between 20 and 450 Hz were placed at the belly of each muscle after skin preparation by shaving, abrasion with sandpaper, and cleaning with alcohol. The EMG electrodes were placed along the fascicle direction. For MG and LG, the electrodes were located medially near the ultrasound probe location for MGcentral and LG, respectively. For the soleus, the electrode was placed just halfway between the distal muscle–tendon junction of the LG and that of the soleus. The locations of EMG electrodes were determined after deciding those of the ultrasound probe. A reference electrode was placed over the lateral malleolus of the left foot.
Data analyses
From the ultrasonic apparatus, elastographic images were exported in DICOM format. To calculate the muscle shear modulus, we processed the acquired elastographic images as follows. The region of interest on the elastographic image color map was selected to be as large as possible using image processing software (ImageJ; NIH, Bethesda, MD, USA). At this time, it was confirmed that tissues other than the target muscle (e.g., subcutaneous fat, aponeurosis, fascia, etc.) were not included in the selected area. Then, the RGB value of each pixel within the region of interest was converted into shear wave speed according to the RGB value–shear wave speed relation estimated from the color scale displayed on the elastographic image. The shear modulus (μ) of each pixel was calculated using the formula μ = ρν2, where ν is the shear wave speed and ρ is the tissue density. In this study, the muscle density was assumed to be 1.084 g·cm−3, which was the mean of the two values reported in a previous study (29). Thereafter, the muscle shear modulus of each elastographic image was calculated by averaging the shear modulus of all pixels within the region of interest.
For the passive joint torque and EMG data, the mean values and root mean square (EMG-RMS) values for each muscle were calculated over a 500-ms period at each joint angle (i.e., PF30, NP, DF15, and RoM at PRE) during the muscle stiffness measurements. In the present study, because the muscle stiffness was measured at four sites, there were four data items of passive torque and EMG-RMS at each joint angle. Therefore, to determine the representative values of passive torque and EMG-RMS at each joint angle, the four values calculated at each joint angle were averaged. The EMG-RMS values were normalized to those for 500 ms during maximal voluntary isometric contraction.
Statistical analyses
To compare the stretching intensity between the older and younger group, unpaired t-tests were conducted for RoM and maximal passive torque measured at PRE. For the maximal muscle shear modulus at PRE, two-way ANOVA (between factor: age (older, younger); within factor: muscle (MGcentral, MGdistal, LG, soleus)) was performed. To verify the stretching effect for each group, a paired t-test was conducted for RoM. For passive torque, two-way ANOVA (within factors: time (PRE, POST) and joint angle (PF30, NP, DF15)) was performed. For muscle shear modulus, three-way ANOVA (within factors: time (PRE, POST), muscle (MGcentral, MGdistal, LG, soleus), and joint angle (PF30, NP, DF15)) was used. For EMG-RMS, three-way ANOVA (within factors: time (PRE, POST), muscle (MG, LG, soleus), and joint angle (PF30, NP, DF15)) was used. When significant interactions were observed for ANOVA, additional multivariate ANOVA, and/or Bonferroni multiple comparison tests or paired/unpaired t-tests were performed. These analyses were conducted using statistical software (SPSS Statistics 25; IBM Japan, Tokyo, Japan). To test the association between stretching intensity and its effect on muscle stiffness, Pearson product–moment correlation analyses were performed between the muscle shear modulus measured at maximal dorsiflexion angle at PRE and the rate of change in muscle shear modulus by stretching in older, younger, and all participants.
Descriptive data are presented as means ± SDs. The significance level was set at α = 0.05. Effect size was estimated using Cohen’s d for paired/unpaired t-tests and Bonferroni multiple comparison tests, and partial η2 (ηp2) for ANOVA and multivariate ANOVA. The Pearson’s product–moment correlation coefficient (r) per se was regarded as the effect size for correlation analyses.
RESULTS
RoM
RoM at PRE was smaller for older participants than for younger ones (older: 23.9° ± 7.0°; younger: 29.7° ± 8.3°; P = 0.022, d = 0.755). Paired t-tests revealed that the static stretching improved RoM for both older (P < 0.001, d = 1.272) and younger participants (P < 0.001, d = 1.372; Figs. 2A, B, respectively).
FIGURE 2.
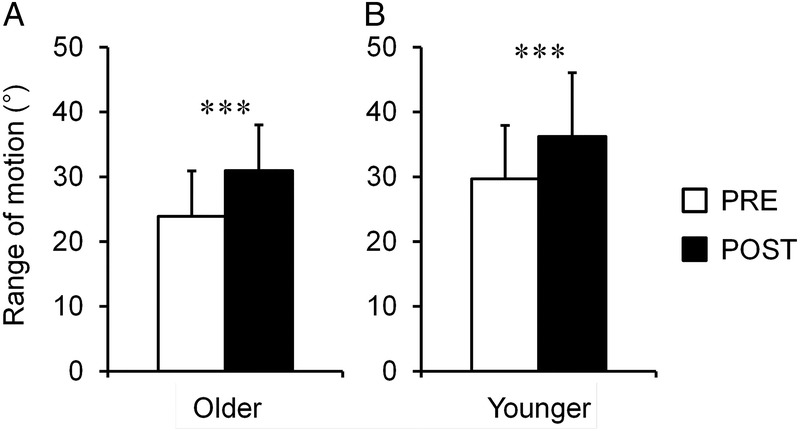
Dorsiflexion range of motion before (PRE) and after (POST) static stretching for older (A) and younger (B) participants. ***Significant difference between PRE and POST, P < 0.001. Values are means and SDs.
Passive joint torque
Maximal passive joint torque at PRE for older participants was smaller than that for younger ones (older: 19.8 ± 10.2 N·m; younger: 28.6 ± 12.1 N·m; P = 0.018, d = 0.786). Two-way ANOVA (time–joint angle) for submaximal passive joint torque showed a significant interaction (older: P < 0.001, ηp2 = 0.485; younger: P < 0.001, ηp2 = 0.748), and post hoc paired t-tests revealed a significant stretching-induced decrease in passive joint torque for older participants at DF15 (P = 0.001, d = 0.833) and that for younger participants at PF30 (P = 0.039, d = 0.503), NP (P < 0.001, d = 1.610), and DF15 (P < 0.001, d = 2.127; Figs. 3A, B, respectively).
FIGURE 3.
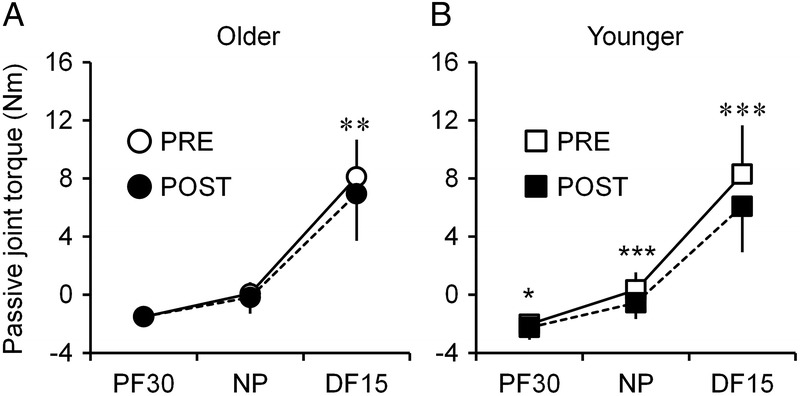
Passive plantar flexion torque measured at a submaximal dorsiflexion angle before (PRE) and after (POST) static stretching for older (A) and younger (B) participants. Significant difference between PRE and POST: *P < 0.05, **P < 0.01, ***P < 0.001. Values are means and SDs.
Shear modulus
For maximal shear modulus at PRE, two-way ANOVA (age–muscle) showed significant main effects of age (P = 0.027, ηp2 = 0.122) and muscle (P < 0.001, ηp2 = 0.775) with no significant interaction (P = 0.131, ηp2 = 0.052). Post hoc Bonferroni comparisons revealed that maximal shear modulus was significantly lower for older participants than for younger ones and was significantly higher in the order MGdistal, MGcentral, LG, and soleus (P < 0.001, d > 3.046; Fig. 4). For older participants, three-way ANOVA (time–muscle–joint angle) for submaximal muscle shear modulus showed a significant second-order interaction (P = 0.006, ηp2 = 0.232), and post hoc analyses revealed a significant decrease induced by stretching only for MGdistal at DF15 (P = 0.003, d = 0.753; Fig. 5A). For younger participants, three-way ANOVA (time–muscle–joint angle) showed a significant second-order interaction (P = 0.006, ηp2 = 0.224), and post hoc analyses revealed a significant decrease induced by stretching for MGcentral at NP (P = 0.010, d = 0.637) and DF15 (P < 0.001, d = 1.065), MGdistal at NP (P = 0.034, d = 0.511) and DF15 (P = 0.003, d = 0.767), and LG at DF15 (P = 0.004, d = 0.730; Fig. 5B). Pearson’s product–moment correlation analyses revealed that the maximal shear modulus at PRE was significantly negatively correlated with the stretching-induced changes in shear modulus measured at DF15 expressed as a percentage for older, younger, and all (older + younger) participants (Figs. 6A–C, respectively).
FIGURE 4.
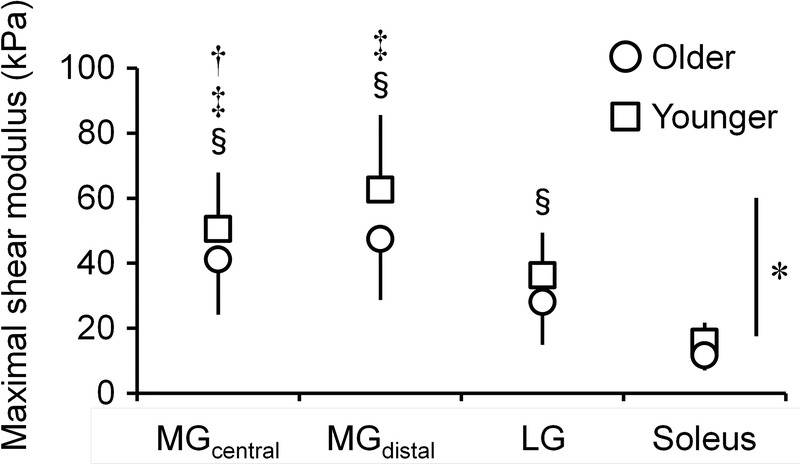
Muscle shear modulus measured at the maximal dorsiflexion angle before stretching for older and younger participants. *Significant main effect of age, P < 0.05. Significant difference: †vs MG distal, ‡vs LG, §vs the soleus (P < 0.001). Values are means and SDs.
FIGURE 5.
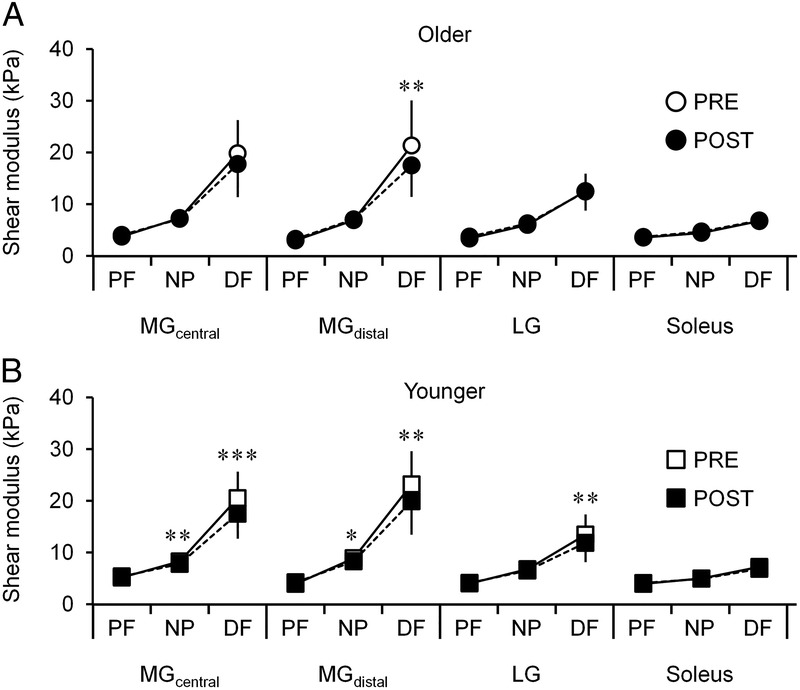
Muscle shear modulus measured at a submaximal dorsiflexion angle (30° of plantar flexion [PF], neutral position [NP] and 15° of dorsiflexion [DF]) before (PRE) and after (POST) static stretching for older (A) and younger (B) participants. Significant reduction from PRE: *P < 0.05, **P < 0.01, ***P < 0.001. Values are means and SDs.
FIGURE 6.
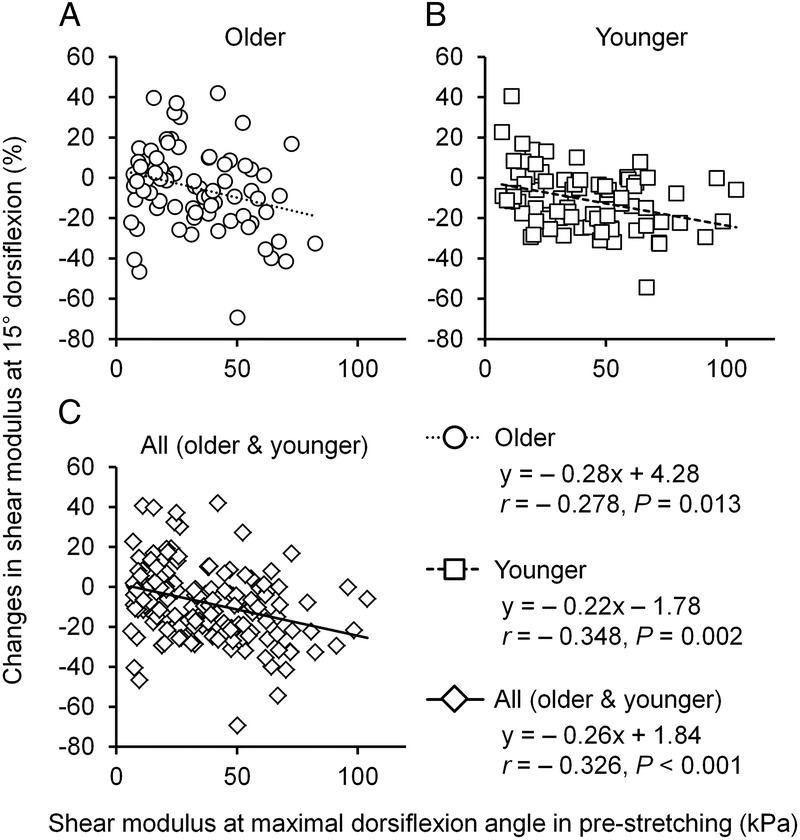
Correlations between the muscle shear modulus measured at the maximal dorsiflexion angle before stretching and the stretching-induced changes in muscle shear modulus measured at DF15 for older (A), younger (B), and all (C) participants. Regression lines are shown for older (dotted line), younger (broken line), and all (solid line).
EMG-RMS
For older participants, three-way ANOVA (time–muscle–joint angle) for EMG-RMS showed no significant interactions (P > 0.193, ηp2 < 0.085) and no significant main effect of time (P = 0.123, ηp2 = 0.121). For younger participants, three-way ANOVA (time–muscle–joint angle) did not show any interactions (P > 0.459, ηp2 < 0.040) or main effect of time (P = 0.113, ηp2 = 0.127).
DISCUSSION
The present results showed that the maximal shear modulus of the triceps surae at PRE for older participants was significantly lower than for younger participants. This suggests that the stretching intensity for older participants was weaker compared with younger participants, in line with our hypothesis. The present stretching exercise improved RoM for both groups; however, significant decreases in muscle shear modulus for older participants were only found in MGdistal at DF15. In contrast, for younger participants, muscle shear modulus was significantly decreased for MGcentral, MGdistal, and LG. These results indicate that effect of stretching on muscle stiffness was limited for older participants, supporting our hypothesis. Collectively, the present results suggest that although static stretching improves flexibility regardless of age, its effect on muscle stiffness in older people is marginal. This might be due to insufficient stretching intensity for older people.
In the present study, stretching intensity for older participants was considered to be lower than for younger participants. The results showed that RoM and the maximal passive joint torque measured at PRE for older participants were narrower and smaller than those for younger participants, respectively. These results agree with a previous study (30). It was suggested that the difference in maximal passive joint resistance between age groups is due to age-related loss of muscle mass. On the other hand, the maximal shear modulus of the triceps surae measured at PRE was also lower for older than for younger participants (Fig. 4). As the shear modulus of the lower limb muscles assessed at a submaximal joint angle was comparable between older and younger people (26,27) or was lower for older people than younger people (17,25) with an age-related decrease in RoM, the difference in maximal shear modulus between age groups observed in the present study is reasonable. Muscle shear modulus is suggested to have little association with size, for example, anatomical cross-sectional area (31) and thickness (32), and also to be unchanged by 6-wk resistance training, despite a significant increase in muscle thickness (33). Hence, aging changes in the maximal joint resistance to external force induced by passive stretch are attributable to not only changes in muscle size but also other factors. Possible factors could be stretch tolerance (9) and/or nonmuscular structures such as nerves and fasciae (34). These reduce the RoM resulting in suppression of maximal joint resistance in older people. Most older people cannot rotate their joints passively until they reach higher joint resistance and muscle stiffness compared with younger people. This means that static stretching intensity weakens with age.
In this study, static stretching improved the RoM for older and younger participants as reported previously (35). Muscle shear modulus was also reduced by stretching in both groups. However, although a significant reduction in shear modulus was found in MG (MGcentral and MGdistal) and LG for younger participants in accordance with a previous study (36), it was only found in MGdistal for older participants (Fig. 5). This can be explained by the muscle- and age-specific differences in the shear modulus at the joint angle during stretching, because it is thought that stiffer muscles reduce the shear modulus more distinctly by stretching (20,22). In the present study, the muscle shear modulus measured at RoM at PRE was significantly higher in the order MGdistal, MGcentral, LG, and the soleus (Fig. 4) as reported previously (28). In addition, the maximal muscle shear modulus was lower for older than younger participants (Fig. 4). Based on these results, the significant decrease in muscle shear modulus induced by stretching observed in the present study was considered to be reasonable. Furthermore, the maximal shear modulus measured at PRE was significantly negatively correlated with the percentage changes in the shear modulus measured at DF15 before and after stretching for older, younger, and all participants (Fig. 6). These associations indicate that the muscle shear modulus decreases more when muscles are stiffer in a stretching position, even for older people. Based on our results, static stretching could reduce muscle stiffness regardless of age, although its effect was limited for older people because of low stretching intensity.
The effect of static stretching on muscle stiffness may vary by not only age but also sex. In fact, a previous study reported that 5 min of static stretching can reduce the shear modulus of the gastrocnemii to the same extent for older and younger women (35). However, this discrepancy between the present and previous results would be caused by differences in stretching intensity (i.e., muscle stiffness in the stretching position) rather than a sex difference. For instance, the MG shear modulus at NP before stretching reported in the aforementioned study (older women: 15.2 ± 3.7 kPa; younger women: 18.3 ± 6.0 kPa; Ref. (35)) was much higher than that of the present study (older men: 7.3 ± 1.4 kPa; younger men: 8.3 ± 1.0 kPa), whereas the RoM and stretching maneuvers were comparable. This implies a considerable difference in stretching intensity between the previous and present studies. Based on the stretching intensity–dependent decrease in muscle stiffness revealed in the present study (Fig. 6), the stretching effect on muscle stiffness is also expected to vary between studies. Although the suggested sex difference in the shear modulus of the triceps surae has been controversial (11,17,37,38), it may be crucial for providing a stretching effect and reducing muscle stiffness if stretching is performed at higher than a certain intensity regardless of sex or age.
The present results indicate that static stretching performed at a joint angle determined by the onset of pain is less effective in reducing muscle stiffness in older people. Health care practitioners should bear in mind the age-related difference in the stretching effect on muscle stiffness. On the other hand, stretching could reduce muscle stiffness even in older people if done at sufficient intensity. Generally, the stretching effect on flexibility parameters (e.g., RoM, passive joint torque, and muscle stiffness, etc.) is dependent on the stretching duration (39), stretching intensity (24), and rest duration between sets of stretching (40). The present stretching time of 7.5 min seemed long enough, although the interval before reaching stretching position between repetitions was also long (about 1 min). Because performing stretching at extremely high intensity may be risky, especially for older people, a resting period will be useful to safely improve flexibility parameters in older people. These points need to be explored in future studies.
Lastly, we have to mention about an applicability of the present findings. The present stretching duration (i.e., 7.5 min) is much longer compared with a practical stretching duration; for example, stretching as a warm-up before an exercise may be usually performed for about ~30 s. It is presumed that the stretching effect on muscle stiffness can become smaller than observed in this study, when stretching is performed in a shorter duration compared with the present settings. In particular, stretching for several tens of seconds might possibly not reduce muscle stiffness for older people. Because it is unknown whether the present results can be also true when stretching is performed in a short duration, future study is warranted to explore this point.
In conclusion, this study aimed to investigate differences in the stiffness of the triceps surae in the stretching position and the stretching-induced decrease in muscle stiffness in older and younger men. The shear modulus measured at the RoM before stretching was higher in the following order: MGdistal, MGcentral, LG, and the soleus for both age groups, and was lower for older than for younger men. Static stretching reduced only the shear modulus of MGdistal, the stiffest region, in older men. Conversely, a decrease in the shear modulus induced by stretching was found in MGdistal, MGcentral, and LG in young men. Regardless of age, a stretching-induced reduction in the muscle shear modulus was correlated with the muscle shear modulus at the RoM before stretching. These results indicate that static stretching can reduce muscle stiffness regardless of age; however, the stretching effect on muscle stiffness in older men is suggested to be limited compared with younger men because older men cannot stretch their muscles sufficiently.
Acknowledgments
This work was supported by JSPS KAKENHI Grant Number JP18J00400 (to K. H.). The authors declare no conflict of interest. The results of the present study do not constitute endorsement by the American College of Sports Medicine.
K. H. and R. A. conceived and designed the research. K. H. and R. Y. performed the experiments. K. H. and R. Y. analyzed the data. K. H., R. Y., and R. A. interpreted the data. K. H. drafted the manuscript. R. Y. and R. A. edited and revised the manuscript. All authors approved the final version of the manuscript.
REFERENCES
- 1.Eyigor S, Karapolat H, Durmaz B. Effects of a group-based exercise program on the physical performance, muscle strength and quality of life in older women. Arch Gerontol Geriatr. 2007;45(3):259–71. [DOI] [PubMed] [Google Scholar]
- 2.Penninx BW, Rejeski WJ, Pandya J, et al. Exercise and depressive symptoms: a comparison of aerobic and resistance exercise effects on emotional and physical function in older persons with high and low depressive symptomatology. J Gerontol B Psychol Sci Soc Sci. 2002;57(2):124–32. [DOI] [PubMed] [Google Scholar]
- 3.Harris ML. Flexibility. Phys Ther. 1969;49(6):591–601. [DOI] [PubMed] [Google Scholar]
- 4.Mecagni C, Smith JP, Roberts KE, O’Sullivan SB. Balance and ankle range of motion in community-dwelling women aged 64 to 87 years: a correlational study. Phys Ther. 2000;80(10):1004–11. [PubMed] [Google Scholar]
- 5.Campbell AJ, Reinken J, Allan BC, Martinez GS. Falls in old age: a study of frequency and related clinical factors. Age Ageing. 1981;10(4):264–70. [DOI] [PubMed] [Google Scholar]
- 6.Kay AD, Blazevich AJ. Moderate-duration static stretch reduces active and passive plantar flexor moment but not Achilles tendon stiffness or active muscle length. J Appl Physiol (1985). 2009;106(4):1249–56. [DOI] [PubMed] [Google Scholar]
- 7.Johnson E, Bradley B, Witkowski K, et al. Effect of a static calf muscle–tendon unit stretching program on ankle dorsiflexion range of motion of older women. J Geriatr Phys Ther. 2007;30(2):49–52. [DOI] [PubMed] [Google Scholar]
- 8.Gajdosik RL, Vander Linden DW, McNair PJ, Williams AK, Riggin TJ. Effects of an eight-week stretching program on the passive-elastic properties and function of the calf muscles of older women. Clin Biomech (Bristol, Avon). 2005;20(9):973–83. [DOI] [PubMed] [Google Scholar]
- 9.Weppler CH, Magnusson SP. Increasing muscle extensibility: a matter of increasing length or modifying sensation? Phys Ther. 2010;90(3):438–49. [DOI] [PubMed] [Google Scholar]
- 10.Magnusson SP, Simonsen EB, Aagaard P, Boesen J, Johannsen F, Kjaer M. Determinants of musculoskeletal flexibility: viscoelastic properties, cross-sectional area, EMG and stretch tolerance. Scand J Med Sci Sports. 1997;7(4):195–202. [DOI] [PubMed] [Google Scholar]
- 11.Miyamoto N, Hirata K, Miyamoto-Mikami E, Yasuda O, Kanehisa H. Associations of passive muscle stiffness, muscle stretch tolerance, and muscle slack angle with range of motion: individual and sex differences. Sci Rep. 2018;8(1):8274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nelson AG, Kokkonen J, Arnall DA, Li L. Acute stretching increases postural stability in nonbalance trained individuals. J Strength Cond Res. 2012;26(11):3095–100. [DOI] [PubMed] [Google Scholar]
- 13.Kumagai H, Miyamoto-Mikami E, Hirata K, et al. ESR1 rs2234693 polymorphism is associated with muscle injury and muscle stiffness. Med Sci Sports Exerc. 2019;51(1):19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yoshitake Y, Takai Y, Kanehisa H, Shinohara M. Muscle shear modulus measured with ultrasound shear-wave elastography across a wide range of contraction intensity. Muscle Nerve. 2014;50(1):103–13. [DOI] [PubMed] [Google Scholar]
- 15.Miyamoto N, Hirata K, Kanehisa H, Yoshitake Y. Validity of measurement of shear modulus by ultrasound shear wave elastography in human pennate muscle. PLoS One. 2015;8(10,4):e0124311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eby SF, Song P, Chen S, Chen Q, Greenleaf JF, An KN. Validation of shear wave elastography in skeletal muscle. J Biomech. 2013;46(14):2381–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akagi R, Yamashita Y, Ueyasu Y. Age-related differences in muscle shear moduli in the lower extremity. Ultrasound Med Biol. 2015;41(11):2906–12. [DOI] [PubMed] [Google Scholar]
- 18.Saeki J, Ikezoe T, Nakamura M, Nishishita S, Ichihashi N. The reliability of shear elastic modulus measurement of the ankle plantar flexion muscles is higher at dorsiflexed position of the ankle. J Foot Ankle Res. 2017;10:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akagi R, Takahashi H. Acute effect of static stretching on hardness of the gastrocnemius muscle. Med Sci Sports Exerc. 2013;45(7):1348–54. [DOI] [PubMed] [Google Scholar]
- 20.Hirata K, Miyamoto-Mikami E, Kanehisa H, Miyamoto N. Muscle-specific acute changes in passive stiffness of human triceps surae after stretching. Eur J Appl Physiol. 2016;116(5):911–8. [DOI] [PubMed] [Google Scholar]
- 21.Le Sant G, Ates F, Brasseur JL, Nordez A. Elastography study of hamstring behaviors during passive stretching. PLoS One. 2015;10(9):e0139272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miyamoto N, Hirata K, Kanehisa H. Effects of hamstring stretching on passive muscle stiffness vary between hip flexion and knee extension maneuvers. Scand J Med Sci Sports. 2017;27(1):99–106. [DOI] [PubMed] [Google Scholar]
- 23.Kataura S, Suzuki S, Matsuo S, et al. Acute effects of the different intensity of static stretching on flexibility and isometric muscle force. J Strength Cond Res. 2017;31(12):3403–10. [DOI] [PubMed] [Google Scholar]
- 24.Freitas SR, Andrade RJ, Larcoupaille L, Mil-homens P, Nordez A. Muscle and joint responses during and after static stretching performed at different intensities. Eur J Appl Physiol. 2015a;115(6):1263–72. [DOI] [PubMed] [Google Scholar]
- 25.Yoshida K, Itoigawa Y, Maruyama Y, et al. Application of shear wave elastography for the gastrocnemius medial head to tennis leg. Clin Anat. 2017;30(1):114–9. [DOI] [PubMed] [Google Scholar]
- 26.Debernard L, Robert L, Charleux F, Bensamoun SF. Analysis of thigh muscle stiffness from childhood to adulthood using magnetic resonance elastography (MRE) technique. Clin Biomech (Bristol, Avon). 2011;26(8):836–40. [DOI] [PubMed] [Google Scholar]
- 27.Domire ZJ, McCullough MB, Chen Q, An KN. Feasibility of using magnetic resonance elastography to study the effect of aging on shear modulus of skeletal muscle. J Appl Biomech. 2009;25(1):93–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Le Sant G, Nordez A, Andrade R, Hug F, Freitas S, Gross R. Stiffness mapping of lower leg muscles during passive dorsiflexion. J Anat. 2017;230(5):639–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ward SR, Lieber RL. Density and hydration of fresh and fixed human skeletal muscle. J Biomech. 2005;38:2317–20. [DOI] [PubMed] [Google Scholar]
- 30.Gajdosik RL, Vander Linden DW, Williams AK. Influence of age on length and passive elastic stiffness characteristics of the calf muscle–tendon unit of women. Phys Ther. 1999;79(9):827–38. [PubMed] [Google Scholar]
- 31.Hirata K, Miyamoto-Mikami E, Kimura N, Miyamoto N. No association between passive material property and cross-sectional area in human hamstring. J Phys Fitness Sports Med. 2018;7(1):35–40. [Google Scholar]
- 32.Chino K, Ohya T, Kato E, Suzuki Y. Muscle thickness and passive muscle stiffness in elite athletes: implications of the effect of long-term daily training on skeletal muscle. Int J Sports Med. 2018;39(3):218–24. [DOI] [PubMed] [Google Scholar]
- 33.Akagi R, Shikiba T, Tanaka J, Takahashi H. A six-week resistance training program does not change shear modulus of the triceps brachii. J Appl Biomech. 2016;32(4):373–8. [DOI] [PubMed] [Google Scholar]
- 34.Nordez A, Gross R, Andrade R, et al. Non-muscular structures can limit the maximal joint range of motion during stretching. Sports Med. 2017;47(10):1925–9. [DOI] [PubMed] [Google Scholar]
- 35.Nakamura M, Ikezoe T, Nishishita S, Umehara J, Kimura M, Ichihashi N. Acute effects of static stretching on the shear elastic moduli of the medial and lateral gastrocnemius muscles in young and elderly women. Musculoskelet Sci Pract. 2017;32:98–103. [DOI] [PubMed] [Google Scholar]
- 36.Taniguchi K, Shinohara M, Nozaki S, Katayose M. Acute decrease in the stiffness of resting muscle belly due to static stretching. Scand J Med Sci Sports. 2015;25(1):32–40. [DOI] [PubMed] [Google Scholar]
- 37.Chino K, Takahashi H. Measurement of gastrocnemius muscle elasticity by shear wave elastography: association with passive ankle joint stiffness and sex differences. Eur J Appl Physiol. 2016;116(4):823–30. [DOI] [PubMed] [Google Scholar]
- 38.Saeki J, Ikezoe T, Yoshimi S, Nakamura M, Ichihashi N. Menstrual cycle variation and gender difference in muscle stiffness of triceps surae. Clin Biomech (Bristol, Avon). 2019;61:222–6. [DOI] [PubMed] [Google Scholar]
- 39.Caliskan E, Akkoc O, Bayramoglu Z, et al. Effects of static stretching duration on muscle stiffness and blood flow in the rectus femoris in adolescents. Med Ultrason. 2019;21(2):136–43. [DOI] [PubMed] [Google Scholar]
- 40.Freitas SR, Vaz JR, Bruno PM, Valamatos MJ, Andrade RJ, Mil-Homens P. Are rest intervals between stretching repetitions effective to acutely increase range of motion? Int J Sports Physiol Perform. 2015c;10(2):191–7. [DOI] [PubMed] [Google Scholar]


