ABSTRACT
Objective
To examine the effect of age on procedural and clinical outcomes in patients undergoing percutaneous coronary intervention (PCI) of chronic total occlusion (CTO) lesions.
Methods
Literature search was conducted across PubMed, Google Scholar and Web of science, databases till March 2019.
Results
Seven studies including 7671 patients with an overall follow-up period of 1.5 to 5 years were included in our review. A total of 6299/1372 patients were included in non-elderly and elderly groups, respectively, with mean age and 67%/61% male patients. CTO-PCI was similarly successful in younger and older patients (82.8%, n = 5070 vs. 78.1%, n = 1010). The incidence of short-term outcomes was low across the studies and comparable between the two groups (all-cause mortality: 0.4% younger vs. 0.85% elderly, cerebrovascular accidents: 0.3% vs. 0.4%, major adverse cardiovascular events (MACE): 1.53% vs. 3.72% and major bleeding: 0.57% vs. 2.18%). Long-term outcomes including all-cause mortality (8.89% vs. 29.5%), cardiac mortality (3.72% vs. 15%) and MACE (24.9% vs. 40%) occurred with a higher incidence in elderly patients. When results were segregated according to the success of CTO-PCI, reduced clinical events were noted with successful revascularization in either age group.
Conclusion
Compared with the younger age group, CTO-PCI in elderly patients is safe and feasible with a comparable incidence of short-term outcomes. In either population, the incidence of long-term outcomes including survival remains a concern but when successful, CTO-PCI may be associated with improvement in terms of multiple patient-important clinical end-points.
KEYWORDS: Chronic total occlusion, percutaneous coronary intervention, age>75, review, angiography
1. Introduction
Chronic total occlusion (CTO) of coronary arteries is defined as complete obstruction of a native coronary artery for the duration of ≥3 months based on estimation from clinical symptoms [1]. The gravity of occlusion is defined by thrombolysis in myocardial infarction (TIMI) grade using angiography as true (TIMI flow grade 0) or functional (TIMI flow grade 1) [2]. Large clinical registries have reported a CTO prevalence of 16–18% in patients with CAD [3,4]. The traditional treatment for CTO has been optimal medical therapy while revascularization therapies, namely, coronary artery bypass graft (CABG) surgery and percutaneous coronary intervention (PCI) were utilized in a lesser proportion of patients (CABG, 22–26% and PCI, 10–22%) [4]. This was due to the uncertainty regarding the post-operative prognosis after revascularization, difficulty in performing CTO-PCI, and the morbidity related to CABG surgery.
With the advancement in treatment strategies, including the use of the hybrid algorithm for guiding crossing strategies and dedicated procedural equipment combined with increasing expertise of operators and availability of experienced centers, PCI has now become an accepted and valuable revascularization treatment option for CTO lesions as compared to the conservative era. As per a national report in 2013, CTO-PCI represented 4.8% of the total PCI volume in the US whereas a percentage of 5% to 10% was noted worldwide [5].
Studies have shown successful CTO-PCI can improve symptoms, angina, quality of life and left ventricular systolic function as well as reduce the need for repeat CABG [6]. However, most of these studies noted these benefits in a relatively younger patient population. With the improvement in life expectancy in the last few decades, we now have a greater proportion of elderly patients with CTO. However, there remains general reluctance towards revascularization therapy in the elderly, as most are being treated with medical management due to presumed complications, low technical success (60–70%) and lack of enough-published data to support aggressive revascularization [3].
Despite increasing evidence, that CTO-PCI improves survival in the elderly, these patients undergo PCI for CTO lesions less frequently as compared to younger individuals. In view of these conflicting practices, the aim of our study was to compare the short- and long-term outcomes of patients undergoing CTO-PCI in younger (<75) and older age groups (≥75).
2. Method
2.1. Search strategy
A comprehensive systematic literature search was performed across four databases (PubMed, Google Scholar, Web of Science and ScienceDirect) to identify all reports of clinical outcomes in elderly patients who underwent CTO-PCI. The search was conducted from the inception of these databases (till March 2019). To identify any additional studies, the references and footnotes of all retrieved articles were also manually searched to ensure that no studies were missed (Figure 1).
Figure 1.
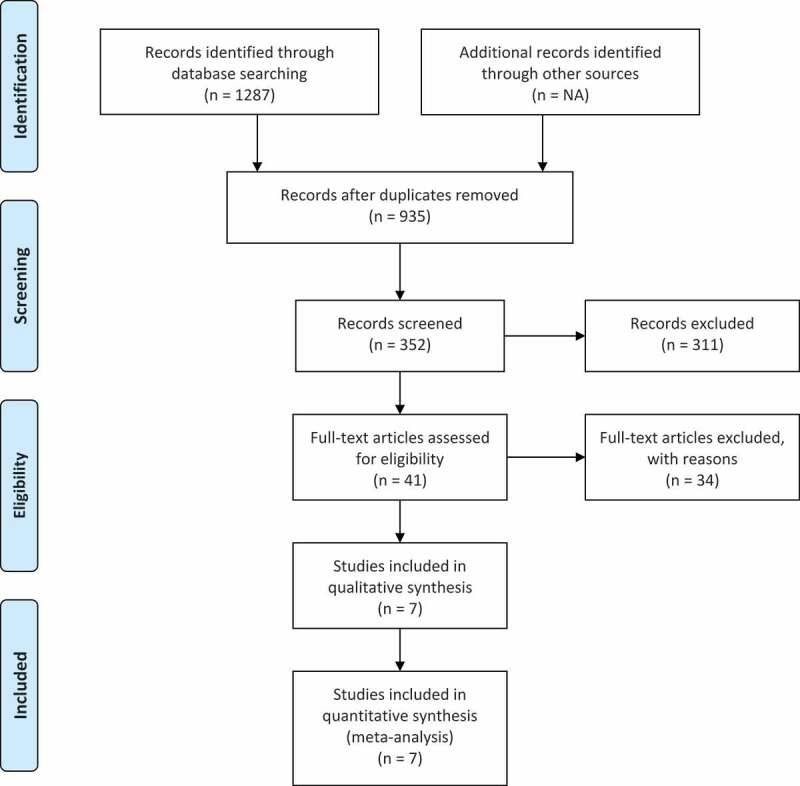
PRISMA flowsheet showing literature search and study selection details.
2.2. Inclusion and exclusion criteria
Studies were considered eligible if they reported clinical outcomes in elderly patients (age ≥ 75) who underwent PCI for CTO lesions with a younger population (age < 75) acting as a comparison group. Two authors independently screened the titles and abstracts of all citations obtained from the initial search. Any disagreement was resolved through discussion and consensus.
2.3. Data extraction
After deciding on the studies to be included, the data was extracted and verified by two authors. When provided, we extracted study design, the name of the first author, publication year, regions of study, study period, sample size, case size, duration of follow up, gender, mean age or age range, co-morbidities and concurrent pharmacological treatment and clinical outcomes.
3. Result
3.1. Baseline characteristics
A total of seven studies were included with 7671 patients [7–12, 14]. Two studies were prospective and five were retrospective. The overall follow-up period ranged from 1.5 to 5 years. The mean age ranged from 59 ± 9 to 80 ± 4. A total of 6184 patients were included in younger age group and 1538 patients were enrolled in older age group. In the younger age group, 67% (n = 4320) were males while 32% (n = 2009) were females. Among the elderly, 61% of patients were males (n = 839) while 39% (n = 549) were females. The BMI reported by only three studies [7,10,14] was higher in younger patients and showed a statistically significant difference (p < 0.01) between the two cohorts in these studies. Among other cardiovascular risk factors, younger patients had higher prevalence of current smoker status [30% (n = 1929) vs. 16% (n = 219)] and lower prevalence of hypertension (HTN) [76% (n = 4789) vs. 82% (n = 1166)], whereas the percentages of patients with diabetes mellitus type 2 and hyperlipidemia were comparable between the two groups.
In terms of past medical history, both the groups had a similar history of prior MI (38% in each group), whereas the higher prevalence of stroke was noted in the older age group [15% (n = 89) vs. 10% (n = 262)]. Similarly, in regards to previous cardiovascular interventions, both the groups had undergone PCI with a similar frequency (~43% in each group) but higher prevalence of prior CABG surgery was seen in older patients [29% (n = 350) vs. 22% (n = 1273)] (Table 1).
Table 1.
Baseline participant characteristics.
| Author, Year, Study design | Groups | N | Age | Gender M/F | HTN | HLD | DM Type 2 | Current Smoker | Prior MI | Prior PCI | Prior CABG |
Prior stroke | CHF | CKD |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Toma, 2017, Retrospective |
<75 | 1593 | 61.5 ± 9 | 224/1369 | 1276 | 1369 | 461 | 377 | 390 | 241 | 221 | NA | 262 | 172 |
| ≥75 | 409 | 79.5 ± 4 | 108/301 | 371 | 340 | 129 | 24 | 103 | 69 | 71 | NA | 86 | 222 | |
| Karatasakis, 2017, Retropsective |
<75 | 1391 | 63.1 ± 6 | 1217/174 | 1244 | 1307 | 633 | 389 | 619 | 883 | 487 | 146 | 396 | NA |
| ≥75 | 253 | 80.1 ± 3 | 192/61 | 235 | 248 | 104 | 30 | 114 | 162 | 109 | 40 | 78 | NA | |
| Zhang, 2017, Retrospective |
<75 | 325 | 63 | 246/79 | 214 | NA | 111 | 200 | 72 | NA | NA | NA | 52 | NA |
| ≥75 | 120 | 78 | 81/39 | 87 | NA | 40 | 49 | 29 | NA | NA | NA | 24 | NA | |
| Iwentu, 2016, Retrospective |
<75 | 932 | 62.8 ± 5 | 805/127 | 824 | 899 | 444 | 299 | 405 | 599 | 312 | 97 | 269 | NA |
| ≥75 | 217 | 79.6 ± 4 | 168/49 | 219 | 227 | 97 | 34 | 102 | 145 | 106 | 40 | 71 | NA | |
| Andre, 2015, Prospective |
<75 | 263 | 60.6 ± 9 | 231/32 | 134 | 199 | 85 | 182 | 134 | 116 | 15 | 19 | 263 | 51 |
| ≥75 | 93 | 80.5 ± 4 | 68/25 | 70 | 59 | 37 | 34 | 50 | 44 | 17 | 9 | 93 | 39 | |
| Tanaka, 2013, Retrospective |
<75 | 217 | 63.1 ± 9 | 193/24 | 139 | 142 | 88 | 51 | 38 | NA | NA | NA | NA | 15 |
| ≥75 | 67 | 78.5 ± 3 | 44/23 | 46 | 45 | 23 | 6 | 12 | NA | NA | NA | NA | 1 | |
| Hobers, 2013, Prospective |
<75 | 1578 | 59.1 ± 9 | 1377/201 | 932 | 1032 | 369 | 431 | 775 | NA | 238 | NA | NA | 46 |
| ≥75 | 213 | 79 ± 3 | 166/47 | 138 | 120 | 37 | 42 | 115 | NA | 47 | NA | NA | 16 |
M, Male; F, Female; HTN, Hypertension; HLD, Hyperlipidemia; DM, Diabetes Mellitus; MI, Myocardial Infarction; PCI, Percutaneous coronary intervention; CABG, Coronary artery bypass grafting; CHF, Congestive heart failure; CKD, Chronic kidney disease; NA, Not available.
3.2. Angiographic and procedural characteristics
Regarding the coronary angiography results, CTO lesions were more frequently seen in the left anterior descending (LAD) artery in older patients (43% vs. 28%), whereas the prevalence of right circumflex artery and left circumflex artery disease was comparable between both groups. Sufficient data was not reported for single versus multivessel disease and location of left main disease in majority of the studies but the available data showed that single vessel disease was more prevalent in younger patients, 21% (n = 387) vs. 14% (n = 69). Six studies reported comparable volume of contrast used during the procedure ranging from a mean value of 176 ± 80 to 482 ± 23 ml in younger patients as compared to 164 ± 79 to 404 ± 197 ml in older patients. Procedural success was reported by five studies and it showed that CTO-PCI was successful in 82% (n = 4744) younger patients and 86% (n = 1039) older patients. Technical success was reported by seven studies and was achieved with a similar frequency in both age groups (76.7% versus 73.1%) (Table 2).
Table 2.
Procedural and angiographic characteristics.
| Overall result | Andre, 2015 | Toma, 2017 | Iwentu, 2016 | Tankana, 2013 | Karatasakis, 2017 | Zhang, 2017 | Hobers, 2013 | ||
|---|---|---|---|---|---|---|---|---|---|
| Procedural characteristics | |||||||||
| Procedural success | <75 | 2073 (89.2%) |
– | – | 863 (89.7%) |
– | 1210 (87%) |
– | – |
| ≥75 | 396 (84.2%) |
– | – | 191 (82.8%) |
– | 205 (81%) |
– | – | |
| Technical success | < 75 | 5070 (82.8%) |
226 (78%) |
1355 (85%) |
874 (90.9%) |
189 (79%) |
1231 (88.5%) |
105 (82.7%) |
1090 (69%) |
| ≥75 | 1010 (78.1%) |
75 (74.3%) |
307 (75%) |
199 (85.7%) |
57 (77%) |
213 (84%) |
23 (69.7%) |
136 (63.9%) |
|
| Angiographic characteristics | |||||||||
| LAD | <75 | 1680 (27.6%) |
– | 431 (27%) |
214 (22%) |
68 (31.3%) |
327 (23.5%) |
99 (30.5%) |
541 (34.3%) |
| ≥75 | 564 (43.4%) |
– | 125 (30.6%) |
231 (97.5%) |
25 (37.3%) |
71 (28%) |
35 (29.2%) |
77 (36.2%) |
|
| LCX | <75 | 1904 (30%) |
78 (29.7%) |
765 (48%) |
204 (20.8%) |
59 (27.2%) |
313 (22.5%) |
116 (35.7%) |
369 (23.4%) |
| ≥75 | 386 (27.8%) |
29 31.2%) |
166 (40.6%) |
45 (19%) |
17 (25.4%) |
45 (18%) |
46 (38.3%) |
38 (17.8%) |
|
| RCA | <75 | 2171 (44.8%) |
152 (57.8%) |
388 (24.4%) |
561 (57%) |
111 (51.2%) |
765 (55%) |
163 (50.2%) |
31 (42%) |
| ≥75 | 603 (42.8%) |
42 (45.2%) |
112 (27.4%) |
127 (53.6%) |
32 (47.8%) |
139 (55%) |
54 (45%) |
97 (42%) |
|
LAD, Left anterior descending; LCX, Left circumflex; RCA, Right coronary artery.
3.3. Short-term outcomes
The overall clinical outcomes are summarized in Table 3. The all-cause mortality was reported by three studies and neither of them found any statistically significant differences between the two groups. It occurred in 0.4% (n = 14) younger patients and 0.85% (n = 7) in elderly patients. Major adverse cardiovascular events (MACE), reported by four studies, was lower in the younger group: 1.53% (n = 65) vs. 3.72% (n = 37). Similarly, major bleeding events or drop-in Hemoglobin level >3 g/dl that required transfusion were lower in younger patients (0.57%, n = 20) compared to older patients (2.18%, n = 18). Overall, the incidence of short-term outcomes in the two age groups was low across all studies.
Table 3.
Short and long-term outcomes.
| Outcomes | Groups | Overall result | Andre, 2015 | Toma, 2017 | Iwentu, 2016 | Tankana, 2013 | Karatasakis, 2017 | Zhang, 2017 | Hobers, 2013 |
|---|---|---|---|---|---|---|---|---|---|
| Short-term outcomes | |||||||||
| All-cause mortality | <75 | 14 (0.4%) |
1 (0.4%) |
7 (0.4%) |
– | 0 | 6 (0.5%) |
– | – |
| ≥75 | 7 (0.8%) |
2 (2.2%) |
2 (0.5%) |
– | 1 (1.5%) |
2 (0.8%) |
– | – | |
| MACE | <75 | 65 (1.5%) |
1 (0.4%) |
15 (0.9%) |
19 (1.9%) |
– | 30 (2.2%) |
– | – |
| ≥75 | 37 (3.7%) |
5 (5.4%) |
4 (0.9%) |
12 (5.1%) |
– | 16 (6.3%) |
– | – | |
| TVR | <75 | 10 (0.3%) |
0 (0%) |
5 (0.3%) |
– | 1 (0.5%) |
4 (0.3%) |
– | – |
| ≥75 | 6 (0.7%) |
2 (2.2%) |
3 (0.7%) |
– | 0 | 1 (0.4%) |
– | – | |
| CVA | <75 | 16 (0.3%) |
0 | 1 (0.7%) |
3 (0.3%) |
0 | 12 (0.8%) |
– | – |
| ≥75 | 4 (0.4%) |
0 | 1 (0.2%) |
1 (0.4%) |
1 (1.4%) |
1 (0.4%) |
– | – | |
| Cardiac tamponade | <75 | 22 (0.5%) |
– | 8 (0.5%) |
3 (0.7%) |
4 (1.7%) |
7 (1.1%) |
– | – |
| ≥75 | 14 (1.4%) |
– | 2 (0.5%) |
5 (2.2%) |
0 | 7 (2.8%) |
– | – | |
| Major bleeding | <75 | 20 (0.6%) |
1 (0.4%) |
3 (0.2%) |
– | 4 (1.8%) |
12 (0.9%) |
– | – |
| ≥75 | 18 (2.2%) |
5 (5.4%) |
9 (2.2%) |
– | 0 | 4 (1.4%) |
– | – | |
| Long-term outcomes | |||||||||
| All-cause mortality | <75 | 208 (6.6%) |
– | 133 (8.3%) |
– | – | – | – | 75 (4.8%) |
| ≥75 | 155 (24.9%) |
– | 109 (26.7%) |
– | – | – | – | 46 (21.6%) |
|
| Cardiac mortality | <75 | 18 (3.7%) |
– | – | – | 3 (1.4%) |
– | 15 (5.6%) |
– |
| ≥75 | 27 (15%) |
– | – | – | 9 (13.4%) |
– | 18 (5.6%) |
– | |
| MACE | <75 | 730 (21.5%) |
– | 457 (28.6%) |
– | 50 (23%) |
– | – | 223 (14.13%) |
| ≥75 | 252 (36.5%) |
– | 162 (39.6%) |
– | 22 (32.8%) |
– | – | 68 (32%) |
|
MACE, Major Adverse Cardiovascular Events; TVR, Target vessel revascularization; CV, Cerebrovascular accident.
3.4. Long-term outcomes
Although not reported by all studies, the long-term mortality was lower in the younger age group. In the younger age group, the all-cause mortality was 8.89% (n = 282) and cardiac mortality was 3.72% (n = 18). These adverse clinical events had a much higher incidence in the older age group with an all-cause mortality of 29.5% (n = 211) and cardiac mortality of 15% (n = 27). Regarding long-term MACE, 24.9% (n = 844) younger patients experienced MACE as compared to 40% (n = 276) of elderly patients.
3.5. Successful vs. failed PCI
Comparison of outcomes between patients with successful versus failed PCI was reported by five studies, with the study by Andre et al. reporting outcomes in the elderly age group only (Table 4). In the younger age group, studies report a lower incidence of all-cause mortality, MI, MACE and cardiac mortality in those with successful PCI than those with failed PCI (2% vs. 4.8%, 2.6% vs. 3.4%, 6.5% vs. 15.1% and 2.1% vs. 6.8%, respectively). On the other hand, a higher incidence of TVR was seen in successful vs. failed PCI patients (2.1% vs. 1%).
Table 4.
Comparison of outcomes between successful vs. failed CTO-PCI in both young and elderly patients.
| Age <
75 |
Age >
75 |
||||
|---|---|---|---|---|---|
| Study | Outcomes | Successful PCI | Failed PCI | Successful PCI | Failed PCI |
| Andre, 2016 | – | – | N = 71 | N = 22 | |
| Mortality | – | – | 15 (21.1) | 2 (9.1) | |
| MI | – | – | 2 (2.8) | 4 (18.2) | |
| Unstable Angina | – | – | 1 (1.4) | 1 (4.5) | |
| Cardiogenic shock | – | – | 2 (2.8) | 1 (4.5) | |
| Angina CCS >2 | – | – | 4 (5.6) | 7 (31.8) | |
| TVR | – | – | 2 (2.8) | 5 (22.7) | |
| Hoebers, 2013 | N = 1090 | N = 488 | N = 136 | N = 77 | |
| MACE | 123 (11.2) | 102 (20.8) | 35 (25.8) | 33 (42.3) | |
| CABG | 40 (3.6) | 62 (12.7) | 0 (0) | 16 (20.4) | |
| MI | 56 (5.1) | 25 (5.1) | 16 (11.5) | 6 (8) | |
| Mortality | 48 (4.4) | 30 (6.1) | 27 (19.6) | 19 (24.6) | |
| Toma, 2017 | N = 1355 | N = 238 | N = 307 | N = 102 | |
| MACE | 10 (0.7) | 5 (2.1) | 3 (1) | 1 (1) | |
| Mortality | 2 (0.1) | 5 (2.1) | 3 (1) | 1 (1) | |
| MI | 7 (0.5) | 0 (0) | 2 (0.7) | 0 (0) | |
| TVR | 3 (0.2) | 0 (0) | 1 (0.2) | 0 (0) | |
| CVA | 0 (0) | 1 (0.4) | 1 (0.3) | 1 (1) | |
| Zhang, 2017 | N = 90 | N = 177 | N = 20 | N = 94 | |
| Cardiac mortality | 1 (1.1) | 14 (7.9) | 3 (15) | 15 (16) | |
| 3-year primary end-point* | 12 (13.3) | 66 (37.3) | 5 (25) | 31 (33) | |
| Tanaka, 2013 | N = 189 | N = 28 | N = 57 | N = 10 | |
| Cardiac mortality | 5 (2.4) | 0 (0) | 1 (2.4) | 2 (23.1) | |
| MACE | 39 (20.8) | 7 (25.3) | 20 (35.6) | 3 (30.8) | |
| TVR | 30 (15.9) | 5 (17.6) | 8 (14.4) | 1 (8.3) | |
*For Zhang, 2017 – 3-year primary end-point was the combined incidence of hospitalization from angina, reinfarction, heart failure or repeat revascularization and cardiac death.
MI, Myocardial infarction; TVR, Target vessel revascularization; MACE, Major Adverse Cardiovascular Events; CABG, Coronary artery bypass grafting; CVA, Cerebrovascular accident.
In the older age group patients, a lower incidence of outcomes including MI, MACE, TVR, cardiac mortality and all-cause mortality was seen in patients with successful PCI as compared to those with failed PCI (3.9% vs. 5%, 1.2% vs. 2%, 2.5% vs. 4.4%, 5.2% vs. 16.3% and 8.8% vs. 10.9%, respectively).
4. Discussion
The results of our review show: (1) similar procedural and technical success rates in elderly and younger age group patients, (2) comparable frequency of short-term outcomes with the overall incidence being low between the two age groups and (3) higher incidence of long-term outcomes in the elderly group.
Elderly patients are more likely to have complex coronary artery lesions and extensive CAD. This combined with the comorbidity burden accounts for the perception of poor outcomes and subsequent reluctance of physicians towards performing complex PCI in this high-risk group [8]. However, in recent years’ multiple factors such as the use of hybrid algorithms, including antegrade versus retrograde approach and true lumen strategy versus dissection re-entry, improved wire designs, use of drug-eluting stents and increased skills of operating physicians have significantly improved the success rates of CTO-PCI [13]. In line with this, the combined result of these studies in our review showed a comparable technical success rate between the two age groups (76.7% vs 73.1%).
This is in contrast to the report from the NCDR (National Cardiovascular Data Registry) which reported a success rate of 59% and identified older age as an independent predictor of technical failure [5]. However, the same study also reported high success rate with participation of more experienced high volume operators as was the case in the studies by Iwentu et al. and Tanaka et al. Similarly, the study by Karatasakis et al. was also performed in a high CTO volume center but it showed greater odds of technical failure in patients >75 years of age (odds ratio [OR], 2.28; 95% confidence interval [CI], 1.20–4.28). However, residual confounding from examined variables (such as previous CABG, PAD) and unexamined variables (such as frailty) was a concern with this study.
Even though the incidence of short-term outcomes was low in both the age groups, these events occurred with relatively higher frequency in elderly patients. This can be related to the higher prevalence of comorbid conditions such as HTN, prior stroke, CABG and angiographic risk such as more severe coronary calcification in elderly patients in most of our studies. Despite this, with the recent technological advances, the advent of drug-eluting stents and more prolonged antithrombotic medications, the incidence of short-term outcomes after CTO-PCI has decreased as noted in the report from NCDR which did not reveal an association between age and in-hospital MACEs [5,15,16].
In regards to long-term outcomes, a much higher incidence of hard end-points was noted in the elderly group as compared to younger patients. These findings resonate with the results of large observational studies performed by Tomasello et al. and Jang et al. which primarily included patients aged <75 and reported a decreased incidence of cardiac death and MACEs with CTO revascularization [17,18]. However, results from randomized controlled trials have been ambiguous. DECISION-CTO and EUROCTO trials evaluated angina relief and quality of life with EUROCTO trial reporting improvement in health status assessed via Seattle Angina Questionnaire in the CTO-PCI group. However, both the studies reported no difference in regards to MACEs [19,20]. In contrast, the recently published REVASC trial including 205 patients showed reduced MACEs with CTO-PCI at 12 months [21]. Hence, based on our studies, there may be a trend towards better long-term outcomes in younger age populations, however, convincing proof of survival benefit in either age group remains elusive. This is also in congruence with current guidelines that recommend considering PCI for CTO lesions in patients with angina burden and for improving LV function and degree of ischemia as compared to mortality benefit [22,23].
An important consideration here is the comparison of outcomes between successful versus failed CTO revascularization. A meta-analysis of 25 studies including more than 28,000 CTO-PCI patients with a median follow-up of 3 years showed that successful PCI was associated with improved clinical outcomes including overall survival (odds ratio (OR), 0.52), angina burden (OR 0.38), stroke (OR 0.72) and need for subsequent bypass surgery (OR 0.18) [24]. Similarly, compared with failed PCI, combined results from studies included in our review showed better outcomes with successful CTO revascularization in both elderly and younger age group patients.
Following are the limitations of our study: first, five out of the seven included studies were retrospective analysis and are thus subject to selection bias. Second, given heterogeneity for several clinical end-points and success rates, a pooled analysis was not possible, hence, the reported results should only be considered suggestive and hypothesis-generating. Third, only the study by Andre et al. assessed myocardial viability. As expected, whether CTO supplies viable or non-viable myocardium has significant clinical importance as it correlates with the burden of ischemia and might dictate benefit achieved post-CTO recanalization. Fourth, only the study by Iwentu et al. reported definitions for technical and procedural success which can partly explain the observed varied success rates. Fifth, four out of the seven studies were performed at single centers which questions the generalizability of results of these studies.
5. Summary
In conclusion, when compared with the younger age group, CTO-PCI in elderly patients is safe and feasible with a comparable incidence of short-term outcomes. However, there seems to be a trend towards better long-term outcomes in younger patients requiring further research to convincingly establish proof of survival in either age group.
Author contributions
Noman Lateef conceptualized and designed the review; Noman Lateef, Muhammad Junaid Ahsan carried out the analysis; Noman Lateef, Muhammad Junaid Ahsan and Hafiz Muhammad Fazeel, Abdul Haseeb and Omar Kousa drafted the initial manuscript; Mohsin Mirza, Mark Holmberg reviewed and approved the final manuscript as submitted.
Disclosure statement
A conflict-of-interest statement is required for all articles and study types. In the interests of transparency and helping reviewers to assess any potential bias in a study’s design, interpretation of its results, or presentation of its scientific/medical content, the BPG requires all authors of each paper to declare on the title page any conflicting interests (including but not limited to commercial, personal, political, intellectual or religious interests) that are related to the work submitted for consideration of publication.
References
- [1].Di Mario C, Werner GS, Sianos G, et al. European perspective in the recanalisation of chronic total occlusions (CTO): consensus document from the EuroCTO club. EuroIntervention. 2007;3(1):30–43. [PubMed] [Google Scholar]
- [2].Schumacher SP, Stuijfzand WJ, Opolski MP, et al. Percutaneous coronary intervention of chronic total occlusions: when and how to treat. Cardiovasc Revascularization Med. 2019; Jun;20(6):513–522. [DOI] [PubMed] [Google Scholar]
- [3].Fefer P, Knudtson ML, Cheema AN, et al. Current perspectives on coronary chronic total occlusions: the canadian multicenter chronic total occlusions registry. J Am Coll Cardiol. 2012;59(11):991–997. [DOI] [PubMed] [Google Scholar]
- [4].Råmunddal T, Hoebers LP, Henriques JPS, et al. Chronic total occlusions in Sweden–a report from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR). PLoS One. 2014;9(8):e103850–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Brilakis ES, Banerjee S, Karmpaliotis D, et al. Procedural outcomes of chronic total occlusion percutaneous coronary intervention: a report from the NCDR (National Cardiovascular Data Registry). JACC Cardiovasc Interv. 2015;8(2):245–253. [DOI] [PubMed] [Google Scholar]
- [6].Tong J, Yu Q, Li C, et al. Successful revascularization of noninfarct related artery with chronic total occlusion among acute myocardial infarction patients: a systematic review and meta-analysis. Medicine (Baltimore). 2018;97(3):e9655–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Toma A, Gebhard C, Gick M, et al. Survival after percutaneous coronary intervention for chronic total occlusion in elderly patients. EuroIntervention. 2017;13(2):e228–e35. [DOI] [PubMed] [Google Scholar]
- [8].Tanaka Y, Takeshita S, Takahashi S, et al. Comparison of short- and long-term outcomes of percutaneous coronary intervention for chronic total occlusions between patients aged ≥75 years and those aged <75 years. Am J Cardiol. 2013;112(6):761–766. [DOI] [PubMed] [Google Scholar]
- [9].Karatasakis A, Iwnetu R, Danek BA, et al. The impact of age and sex on in-hospital outcomes of chronic total occlusion percutaneous coronary intervention. J Invasive Cardiol. 2017;29(4):116–122. [PubMed] [Google Scholar]
- [10].Zhang H-P, Ai H, Zhao Y, et al. Effect of chronic total occlusion percutaneous coronary intervention on clinical outcomes in elderly patients. Am J Med Sci. 2018;355(2):174–182. [DOI] [PubMed] [Google Scholar]
- [11].Hoebers LP, Claessen BE, Dangas GD, et al. Long-term clinical outcomes after percutaneous coronary intervention for chronic total occlusions in elderly patients (≥75 years). Catheterization Cardiovasc Interventions. 2013;82(1):85–92. [DOI] [PubMed] [Google Scholar]
- [12].Iwnetu R. Impact of age on technical and in-hospital outcomes of percutaneous coronary intervention for chronic total occlusions. Fort Worth, Tx:University of North Texas Health Science Center; 2016. Available from: http://digitalcommons.hsc.unt.edu/theses/927. [Google Scholar]
- [13].Shah A. Chronic total occlusion coronary intervention: in search of a definitive benefit. Methodist Debakey Cardiovasc J. 2018. Jan–Mar;14(1):50–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].André R, Dumonteil N, Lhermusier T, et al. In-hospital and long-term outcomes after percutaneous coronary intervention for chronic total occlusion in elderly patients: a consecutive, prospective, single-centre study. Arch Cardiovasc Dis. 2016;109(1):13–21. [DOI] [PubMed] [Google Scholar]
- [15].Vasaiwala S, Forman DE, Mauri L.. Drug-eluting stents in the elderly. Curr Treat Options Cardiovasc Med. 2010. January;12(1):76–83. [DOI] [PubMed] [Google Scholar]
- [16].Oqueli E, Dick R. Percutaneous coronary intervention in very elderly patients. In-hospital mortality and clinical outcome. Heart Lung Circ. 2011. October;20(10):622–628. [DOI] [PubMed] [Google Scholar]
- [17].Tomasello SD, Boukhris M, Giubilato S, et al. Management strategies in patients affected by chronic total occlusions: results from the Italian registry of chronic total occlusions. Eur Heart J. 2015;36:3189–3198. [DOI] [PubMed] [Google Scholar]
- [18].Jang WJ, Yang JH, Choi SH, et al. Long‐term survival benefit of revascularization compared with medical therapy in patients with coronary chronic total occlusion and well‐developed collateral circulation. JACC Cardiovasc Interv. 2015;8:271–279. [DOI] [PubMed] [Google Scholar]
- [19].Lee SW, Lee PH, Ahn JM, et al. Randomized trial evaluating percutaneous coronary intervention for the treatment of chronic total occlusion. Circulation. 2019. April 2;139(14):1674–1683. [DOI] [PubMed] [Google Scholar]
- [20].Werner GS, Martin-Yuste V, Hildick-Smith D, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J. 2018;39:2484–2493. [DOI] [PubMed] [Google Scholar]
- [21].Mashayekhi K, Nührenberg TG, Toma A, et al. A randomized trial to assess regional left ventricular function after stent implantation in chronic total occlusion: the REVASC trial. J Am Coll Cardiol Intv. 2018;11. [DOI] [PubMed] [Google Scholar]
- [22].Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. EuroIntervention. 2019. February 20;14(14):1435–1534. [DOI] [PubMed] [Google Scholar]
- [23].Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American college of cardiology foundation/American heart association task force on practice guidelines and the society for cardiovascular angiography and interventions. Catheter Cardiovasc Interv. 2013;82(4):E266–355. [DOI] [PubMed] [Google Scholar]
- [24].Christakopoulos GE, Christopoulos G, Carlino M, et al. Meta‐analysis of clinical outcomes of patients who underwent percutaneous coronary interventions for chronic total occlusions. Am J Cardiol. 2015;115:1367–1375. [DOI] [PubMed] [Google Scholar]


