ABSTRACT
Background: After a potentially traumatic event (PTE), children often show symptoms of acute stress disorder (ASD), which may evolve into posttraumatic stress (PTS) disorder. A growing body of literature has employed latent class analysis (LCA) to disentangle the complex structure underlying PTS symptomatology, distinguishing between homogeneous subgroups based on PTS presentations. So far, little is known about subgroups or classes of ASD reactions in trauma-exposed children.
Objective: Our study aimed to identify latent classes of ASD symptoms in children exposed to a single-incident PTE and to identify predictors of class membership (gender, age, cultural background, parental education, trauma type, and trauma history).
Method: A sample of 2287 children and adolescents (5–18 years) was derived from the Prospective studies of Acute Child Trauma and Recovery (PACT/R) Data Archive, an international archive including studies from the USA, UK, Australia, and Switzerland. LCA was used to determine distinct subgroups based on ASD symptoms. Predictors of class membership were examined using a three-step approach.
Results: Our LCA yielded a three-class solution: low (42%), intermediate (43%) and high (15%) ASD symptom severity that differed in terms of impairment and number of endorsed ASD symptoms. Compared to the low symptoms class, children in the intermediate or high severity class were more likely to be of female gender, be younger of age, have parents who had not completed secondary education, and be exposed to a road traffic accident or interpersonal violence (vs. an unintentional injury).
Conclusions: These findings provide new information on children at risk for ASD after single-incident trauma, based on a unique set of international data. Classifying children based on latent symptom profiles helps to identify target groups for prevention and intervention after exposure to a PTE.
KEYWORDS: Single-Incident Trauma, early life adversity, childhood trauma, post-traumatic stress, latent class analysis
Antecedentes: después de un evento potencialmente traumático (EPT), los niños a menudo muestran síntomas de trastorno de estrés agudo (TEA), el cual, puede evolucionar a un trastorno de estrés postraumático (TEPT). Un creciente cuerpo de literatura ha empleado el análisis de clase latente (LCA por sus siglas en ingles) para desenredar la compleja estructura subyacente a la sintomatología de TEPT, distinguiendo entre subgrupos homogéneos basados en presentaciones de TEPT. Hasta ahora, se sabe poco sobre los subgrupos o clases de reacciones TEA en niños expuestos a traumas.
Objetivo: Nuestro estudio tuvo como objetivo identificar clases latentes de síntomas de TEA en niños expuestos a un solo incidente de EPT e identificar predictores de pertenencia a la clase (género, edad, antecedentes culturales, educación de los padres, tipo de trauma e historial de trauma).
Método: se obtuvo una muestra de 2287 niños y adolescentes (5–18 años) de los estudios Prospectivos del Archivo de Datos de recuperación y Trauma Infantil agudo (PACT/R, en sus siglas en inglés), un archivo internacional que incluye estudios de Estados Unidos, Reino Unido, Australia y Suiza. Se utilizó LCA para determinar distintos subgrupos basados en los síntomas de TEA. Los predictores de pertenencia a la clase se examinaron mediante análisis de regresión logística ponderada.
Resultados: Nuestro LCA arrojó una solución de tres clases: gravedad de los síntomas de TEA baja (42%), intermedia (43%) y alta (15%) que difería en términos de deterioro y número de síntomas de TEA atribuidos. En comparación con la clase baja e intermedia, los niños en la clase de gravedad alta tenían más probabilidades de ser de género femenino, de menor edad, tener padres que no habían completado la educación secundaria y estar expuestos a la violencia interpersonal (versus a eventos médicos no interpersonales). Pertenecer a una minoría étnica se asoció con la pertenencia a la clase de “síntomas intermedios“ en comparación con la clase de ”síntomas bajos”.
Conclusiones: Estos hallazgos brindan nueva información sobre los niños en riesgo de TEA después de un incidente traumático único, en base a un conjunto único de datos internacionales. La clasificación de los niños según los perfiles de síntomas latentes ayuda a identificar los grupos objetivo para la prevención e intervención después de la exposición a un EPT.
PALABRAS CLAVE: Incidente traumático único, adversidad de la vida temprana, trauma infantil, estres traumático, análisis de clases latente
背景:经历潜在创伤事件(PTE)之后,儿童常表现出急性应激障碍(ASD)的症状,这些症状可能演变成创伤后应激(PTS)障碍。越来越多的文献采用潜在类别分析(LCA)来理清PTS症状学潜在的复杂结构,从而根据PTS表现来区分同质亚组。到目前为止,对创伤暴露儿童ASD反应的亚组或类别知之甚少。
目标:我们的研究旨在确定暴露于单次PTE事件的儿童中ASD症状的潜在类别,并确定类别归属的预测因子(性别,年龄,文化背景,父母教育,创伤类型和创伤史)。
方法:从急性儿童创伤与康复前瞻性研究(PACT/ R)数据库中抽取2287名儿童和青少年样本(5–18岁),该国际档案库包括美国,英国,澳大利亚和瑞士的研究。根据ASD症状使用LCA确定不同的亚组。使用加权逻辑回归分析考查类别归属的预测因子。
结果:我们的LCA确定了三个类别:分别为低(42%),中等(43%)和高(15%)ASD症状严重程度类,即在损伤和记录的ASD症状数量方面有所不同。与低和中度症状类别相比,高症状类别的孩子更可能是女性,更年轻,父母更可能未完成中学教育并且更容易遭受人际暴力(相对于非人际医疗事件) 。相较于‘低症状’类别,属于少数民族与‘中等症状’的成员身份相关。
结论:这些发现基于一组独特的国际数据,为经历单次创伤后有急性应激障碍危险的儿童提供了新信息。根据潜在症状剖面对儿童进行分类有助于识别暴露于PTE后的预防和干预目标人群。
关键词: 单发性创伤, 早期逆境, 童年期创伤, 创伤后应激, 潜在类别分析
1. Introduction
Exposure to a potentially traumatic event (PTE) is relatively common. Lifetime prevalence rate in adults is 70% (Benjet et al., 2016) and 25% for children (Costello, Erkanli, Fairbank, & Angold, 2002). As a common psychological response during or in the aftermath of such an event, children often show acute stress reactions, such as intrusions, negative mood, and arousal. In most children, these symptoms decrease naturally within a short period of time (Copeland, Keeler, Angold, & Costello, 2007). However, a minority of children develops clinically relevant symptoms of acute stress disorder (ASD) or posttraumatic stress disorder (PTSD) (Alisic et al., 2014). In a study by Meiser-Stedman et al. (2017), approximately 14% of youth (8–17 years old) exposed to a single-incident trauma met criteria for ASD 2 weeks after trauma exposure.
ASD is a mental disorder that can occur in the first month after exposure to a PTE. ASD symptoms overlap with those for PTSD, including traumatic re-experiencing (e.g. flashbacks, recurring nightmares), avoidance, arousal (e.g. sleep disturbance, difficulties concentrating), and clinically significant distress (American Psychiatric Association, 2013). In DSM-5, the ASD diagnosis requires the presence of at least nine of 14 specified symptoms. A distinction from PTSD is that ASD symptoms must last at least 2 days but no more than 4 weeks after the traumatic event (American Psychiatric Association, 2013). Since ASD was found to be predictive of later development of PTSD (Shevlin, Hyland, & Elklit, 2014), its detection may be an important step in the prevention of PTSD.
People stress responses show high symptom heterogeneity, with diverse symptomatic manifestations (Armour, Mullerová, & Elhai, 2016; Steenkamp et al., 2012), which may not be fully captured by dichotomous taxonomy or population mean-based methods (Lenferink, de Keijser, van Denderen, & Boelen, 2018). In the last two decades, latent class analysis (LCA) has become one of the most established statistical techniques to disentangle the complex structure underlying mental disorders. LCA is a person-centred approach that identifies and distinguishes between homogeneous subgroups based on symptom presentations.
Prior studies that employed LCA in trauma-exposed adult samples distinguished three (Breslau, Reboussin, Anthony, & Storr, 2005; Horn et al., 2016; Lenferink et al., 2018) to four (Hebenstreit, Madden, & Maguen, 2014; Minihan, Liddell, Byrow, Bryant, & Nickerson, 2018; Rosellini, Coffey, Tracy, & Galea, 2014) different subgroups or classes of PTSD responses. Three studies across five samples showed that classes predominantly differed in terms of severity of PTSD symptom levels (i.e. low, intermediate, and high symptoms classes) (Breslau et al., 2005; Lenferink et al., 2018; Rosellini et al., 2014). Horn et al. (2016) described three PTSD classes (i.e. high, dysphoric, threat) that differ on symptom presentation rather than severity. Minihan et al. (2018) found four PTSD classes (i.e. high PTSD, high re-experiencing/avoidance, a moderate, and no PTSD class).
To the best of our knowledge, only one study conducted LCA in youths exposed to a PTE, which shows similar PTSD symptomatology classes as in adults. Ayer et al. (2011) investigated PTSD symptoms in a national sample of adolescents (aged 12–17 years) after lifetime exposure to diverse types of trauma and extracted three classes: no disturbance, intermediate disturbance, and pervasive disturbance. However, so far, hardly anything is known about immediate ASD reactions, let alone about subgroups of ASD symptoms, after a PTE in children. Increasing knowledge about diverging symptom profiles may help to identify target groups for prevention and intervention.
To identify subgroups at risk, it is important to better understand why different symptom classes emerge, e.g. if they indicate the presence of qualitatively different types of ASD, reflect certain sample differences or have a predictive impact on long-term mental health (Breslau et al., 2005). Prior research examining prevalence rates or mean PTSD symptom levels in people exposed to a PTE have identified several risk factors. PTSD diagnoses are more common among girls than boys (Alisic et al., 2014; Trickey, Siddaway, Meiser-Stedman, Serpell, & Field, 2012). Stress reactions following a PTE in children may vary with age (Dyregrov & Yule, 2006), usually with younger age as a risk factor for PTSD (Trickey et al., 2012). Regarding cultural background, several studies have found that abused children who belong to minorities experienced more severe symptomatology (Morrow & Sorell, 1989; Sanders-Phillips, Moisan, Wadlington, Morgan, & English, 1995; Stein, Golding, Siegel, Burnam, & Sorenson, 1988). Cultural differences in how sexuality (e.g. feeling guilty about losing virginity after sexual abuse) and interfamilial boundaries (e.g. fear of rejection from community when reporting abuse) are perceived and how (negative) emotions are expressed (e.g. shame for expressing negative emotions) may play an important detrimental role here (Cohen, Deblinger, Mannarino, & de Arellano, 2001; Sebre et al., 2004). A lower socioeconomic status has been identified as a risk factor for PTSD in children after trauma exposure (Kahana, Feeny, Youngstrom, & Drotar, 2006). As to trauma type, interpersonal trauma (e.g. abuse, assault) has been related to increased risk for PTSD in children compared with non-interpersonal trauma (e.g. accident, natural disaster) suggested (Alisic et al., 2014). Lastly, a history of trauma exposure has also been identified as a risk factor for stress in children (Finkelhor, Ormrod, & Turner, 2009).
In summary, research on ASD symptoms in children after exposure to a PTE is very limited. Moreover, LCA research on ASD symptoms is not yet available. Findings from previous LCA studies in PTSD suggest that three different classes can be distinguished in terms of symptom severity in adults and adolescents. The current study aimed to conduct an LCA on ASD symptoms within a sample of children derived from the Prospective studies of Acute Child Trauma and Recovery (PACT/R) Data Archive (Kassam-Adams, Kenardy, & Delahanty et al., in review). As a first step, we used LCA to examine subgroups of trauma-exposed children based on the endorsement of ASD symptoms. Secondly, we investigated whether formerly established predictors of stress reactions after exposure to a PTE, namely gender, age, cultural background, parental education (a commonly measured proxy for socioeconomic status in child trauma studies), trauma type, and trauma history predicted membership of the ASD classes.
Based on previous research in adult and adolescent samples (Ayer et al., 2011; Breslau et al., 2005; Horn et al., 2016; Lenferink et al., 2018) we expected that the LCA would result in at least three distinct ASD classes: a low, intermediate, and high symptom class. Furthermore, we expected that being a girl (vs. a boy), being younger of age, belonging to an ethnic minority, having low parental education, and being exposed to interpersonal or intentional trauma (vs. other trauma), and history of prior trauma were risk factors for belonging to classes with more severe ASD symptoms.
2. Method
2.1. Participants
Data on DSM-5 ASD symptoms, collected from children within 30 days after exposure to a PTE, were obtained from the international PTSD after Acute Child Trauma (PACT) Data Archive (Kassam-Adams et al., in review). This archive includes data of 30 longitudinal studies on acute traumatic stress symptoms after exposure to a PTE conducted in the USA, UK, Australia, and Switzerland. For the purpose of the present study, we included data from 21 studies in which self-reported ASD symptoms by children were assessed within 30 days after trauma. Nine studies did not meet these criteria and were therefore not included. Our sample consisted of 2287 children and adolescents between 5 and 18 years of age (Mage = 11.9, SD = 3.1). Table 1 demonstrates the sample characteristics. Just over half of participants resided in the USA. The most common type of PTE was unintentional injury (49.1%; e.g. fall, sports, and burns), followed by road traffic accidents requiring medical attention (RTAs; 34.3%; e.g. motor vehicle occupant, pedestrian, and bicycle), interpersonal violence (10.3%; e.g. violence by a (non-)family member or mass violence), and acute medical events (4.9%; e.g. ICU admission for severe illness).
Table 1.
Demographic characteristics.
| n (%) | ||
|---|---|---|
| Sex | Boys | 1455 (63.6) |
| Girls | 832 (36.4) | |
| Age (years) | 5–7 | 160 (7.3) |
| 8–11 | 828 (37.8) | |
| 12–14 | 708 (32.3) | |
| 15–17 | 493 (22.5) | |
| Country of residence | Australia | 456 (19.9) |
| Switzerland | 161 (7.0) | |
| UK | 441 (19.3) | |
| USA | 1229 (53.7) | |
| Ethnic minority in country of residence | Yes | 871 (41.2) |
| No | 1244 (58.8) | |
| Parent completed secondary education | Yes | 934 (78.9) |
| No | 250 (21.1) | |
| Trauma type | Unintentional injury | 1124 (49.8) |
| Acute medical event (non-injury) | 113 (5.0) | |
| RTA requiring medical attention | 784 (34.7) | |
| Interpersonal violence | 236 (10.5) | |
| Prior trauma history | Yes | 964 (62.0) |
| No | 591 (38.0) |
2.2. Procedure
Each of the original studies in which data were collected had approval from a local ethical committee. Table 2 shows the characteristics of the 21 studies included in the Data Archive, including the number of participants, primary trauma type, age range of participants, and country where and time when the study took place. Harmonizing ASD symptoms across studies consisted of several steps. Firstly, acute traumatic stress assessments 2 days to 30 days post-event were identified. Secondly, candidate congruent items were identified from each dataset and the core group of PACT Project Group researchers reached consensus on how to harmonize these items from different measures. An example of a harmonized item is the ASD symptom ‘Recurrent, involuntary, and intrusive distressing memories of the traumatic event(s)’ that has been assessed across studies using different measures, such as ‘Having upsetting thoughts or images about the event that came into your head when you didn’t want them to’ (Child PTSD Symptom Scale [CPSS]), ‘Do you think about it even when you don’t mean to?’ (Children’s Impact of Event Scales [CRIES]), and ‘Did you think about (event) even when you didn’t want to?’ (Clinician-Administered PTSD Scale for Children and Adolescents [CAPS-CA]). Thirdly, item responses were dichotomized based on the measures’ standard scoring rules for symptom presence. For a more detailed description of the harmonization process see (Kassam-Adams et al., 2012). For the purpose of the current study, we aimed to include 14 DSM-5 ASD symptoms and therefore the DSM-5 negative mood symptom was considered present if the child responded positively to either the ‘emotional numbing’ or the ‘detachment from other people’ item (both part of DSM-IV criteria).
Table 2.
Characteristics of included studies.
| PACT/R dataset number | Sample size | Type(s) of acute trauma exposure (index event) | Age range (years) | Country | Year(s) |
|---|---|---|---|---|---|
| 1001 | 219 | Injury/RTAa | 8–17 | US | 1999–2001 |
| 1002 | 90 | Injury/RTAb | 5–7 | US | 1999–2001 |
| 1003 | 164 | Injury/Medical/RTA/Violencec | 8–17 | US | 2002–2004 |
| 1004 | 38 | Violenced | 8–18 | US | 1999–2000 |
| 1006 | 363 | Injury/Medical/Violence/RTAe | 8–17 | US | 2007–2010 |
| 1007 | 88 | Injury/RTAf | 8–17 | US | 2007–2008 |
| 1008 | 53 | Injury/RTAg | 8–17 | US | 2005 |
| 1009 | 61 | Violenceh | 12–17 | US | 2001–2003 |
| 1010 | 132 | Injuryi | 6–16 | AUS | 2000–2002 |
| 1012 | 99 | Injuryj | 7–15 | AUS | 2003–2004 |
| 1014 | 49 | Injuryk | 7–15 | AUS | 2007 |
| 1020 | 79 | Violence/RTAl | 10–17 | UK | 2001–2002 |
| 1021 | 45 | RTAm | 6–11 | UK | 2004–2005 |
| 1022 | 121 | Injury/Medical/Violence/RTAn | 7–17 | AUS | 2004–2006 |
| 1023 | 50 | RTAo | 7–16 | SUI | 2004–2007 |
| 1025 | 91 | Injury/Violencep | 12–18 | US | 2002–2003 |
| 1026 | 55 | Injury/RTAq | 8–16 | AUS | 2013–2014 |
| 1032 | 111 | Injury/RTAr | 7–15 | SUI | 2016–2018 |
| 1036 | 62 | Injury/RTA/Violences | 8–17 | US | 2012–2014 |
| 1037 | 218 | Injury/Medical/RTA/Violencet | 8–17 | UK | 2010–2013 |
| 1038 | 99 | Injury/Medical/RTA/Violenceu | 6–13 | UK | 2014–2015 |
RTA = road traffic accident.
aKassam-Adams and Winston (2004).
bFeinberg (2004).
cKassam-Adams (2006).
dFein et al. (2002).
eKassam-Adams et al. (2013).
fKassam-Adams et al. (2011).
gMarsac, Donlon, Winston, and Kassam-Adams (2013).
hPailler, Kassam-Adams, Datner, and Fein (2007).
iLe Brocque, Hendrikz, and Kenardy (2010).
jKenardy, Thompson, Le Brocque, and Olsson (2008).
kCox, Kenardy, and Hendrikz (2010).
lMeiser-Stedman, Yule, Smith, Glucksman, and Dalgleish (2005).
mMeiser-Stedman, Smith, Glucksman, Yule, and Dalgleish (2008).
nNixon, Ellis, Nehmy, and Ball (2010).
oZehnder, Meuli, and Landolt (2010).
pZatzick et al. (2006).
qAlisic et al. (2015).
rde Haan, Tutus, Goldbeck, Rosner, and Landolt (2019).
sMarsac et al. (2017).
tMeiser-Stedman et al. (2017).
Hiller et al. (2018).
2.3. Predictors of class membership
Correlates of class membership included in the analyses comprised gender (0 = boys, 1 = girls), child age (in years), ethnic minority (0 = no, 1 = yes), parental education (0 = parent did not complete secondary education, 1 = parent completed secondary education), trauma type (i.e. unintentional injury, acute medical event, RTA, interpersonal violence, dummy coded with unintentional injury as reference group), and history of previous trauma (0 = no, 1 = yes). Ethnic minority status in the child’s country of residence was represented by a harmonized variable, based on available information from each study about the child’s race/ethnicity, e.g. for children in the UK samples, this would include those who reported their ethnicity as ‘Asian’, ‘Black’, or ‘Mixed’. Whether or not the parent completed secondary education was assessed through another harmonized variable, based on information about the parent’s highest level of education. Information on trauma type was categorized into unintentional injuries (not related to RTAs), acute medical events (non-injury), RTAs requiring medical attention, and interpersonal violence.
In order to examine to what extent the classes differed, on average, in the endorsement of ASD symptoms, the number of endorsed ASD symptoms was included as a correlate. Additionally, we examined the differences in impairment between the classes. Concurrent impairment was represented by a dichotomous variable (0 = no, 1 = yes) based on items assessing impairment in social, academic, or other functioning, which was included in the traumatic stress measures completed within 30 days post-trauma (cf., Kassam-Adams et al., 2012 for further information about this variable). For instance, the Acute Stress Checklist for Children (ASC-Kids) includes the following impairment item: ‘Since this happened, getting along with friends or family is harder for me.’
2.4. Statistical analyses
The 14 harmonized and dichotomized DSM-5 ASD symptoms (see Supplemental Table S1) were subjected to a LCA using Mplus 7.4 (Muthén & Muthén, 2012). Models with one up to seven classes were examined. Based on fit statistics and consistency with prior LCA research on ASD or PTSD symptoms, the preferred model was chosen. Model selection was based on the following fit statistics: Akaike’s information criterion (AIC) and Bayesian information criterion (BIC) values (with lower values indicating better fit), p-values of the Lo-Mendell-Rubin likelihood ratio test (LMR LRT) and bootstrapped likelihood ratio test (BLRT; with p < .05 indicating a better fit of the model under consideration than the model with one less class), and entropy R2 values (with values closer to 1 indicating better class separation Nylund, Asparouhov, & Muthén, 2007; van de Schoot, Sijbrandij, Winter, Depaoli, & Vermunt, 2017). Missing data on ASD symptoms varied between 0.3% and 46.7% per item (see Supplemental Table S1). Missing data on the ASD symptoms were accounted for with the Mplus missing data default option (Muthén & Muthén, 2012), i.e. full information maximum likelihood (FIML). To avoid solutions based on local maxima, 240 random sets of starting values and 60 final stage optimizations were used.
The three-step approach in Mplus was used to examine the correlates of class-membership (Asparouhov & Muthén, 2014). Within this approach the classification error, resulting from assigning people to the class with the highest probability estimate, is taken into account when examining the associations between classes and correlates (Vermunt, 2010). Firstly, for descriptive reasons, we examined to what extent classes differed in (1) total number of endorsed ASD symptoms and (2) percentage of children that reported impairment (yes or no) because of ASD symptoms, separately. Secondly, differences between classes were examined regarding the background (i.e. gender, age, ethnic minority, and educational level of parent) and trauma characteristics (i.e. trauma type and trauma history) when entered to the model simultaneously. In total, 771 children provided data on all background and trauma characteristics. The relatively high proportion of missing data on correlates is due to the fact that some studies did not assess certain correlates. Therefore, these data could be considered to be missing completely at random. To avoid losing statistical power to detect effects, we imputed missing data on correlates by using multiple imputation; 100 datasets were generated. Lastly, we conducted a completers-only analysis by using listwise deletion when examining correlates of classes simultaneously.
3. Results
3.1. Latent class analysis
Table 3 shows the fit indices for the latent class models (one to seven classes). The three-class solution had the lowest BIC value, which is considered the preferred fit index to rely on according to an expert panel (van de Schoot et al., 2017). The entropy values were acceptable for the solution with two and three classes but were lower for models with four or more classes. The significant LMR-A p -value indicated that a three-class solution was preferred over a two-class solution. The BLRT p- value was indecisive. Based on the fit indices and accordance with prior research (cf., Lenferink et al., 2018), a three-class solution was chosen (following guidelines from van de Schoot et al. (2017) alternative class models are shown in Supplemental Figure S1).
Table 3.
Fit indices for 1–7 class solutions.
| Model | Loglikelihood | BIC | AIC | Entropy R2 | BLRt p-value | LMR-A p -value |
|---|---|---|---|---|---|---|
| 1 Class | −16,972.49 | 34,053.27 | 33,972.98 | |||
| 2 Class | −14,895.88 | 30,016.07 | 29,849.75 | 0.82 | <.001 | <.001 |
| 3 Class | −14,588.65 | 29,517.64 | 29,265.30 | 0.75 | <.001 | <.001 |
| 4 Class | −14,538.06 | 29,532.49 | 29,194.13 | 0.66 | <.001 | 0.12 |
| 5 Class | −14,493.49 | 29,559.37 | 29,134.98 | 0.67 | <.001 | 0.07 |
| 6 Class | −14,459.36 | 29,607.13 | 29,096.72 | 0.66 | <.001 | 0.24 |
| 7 Class | −14,429.88 | 29,664.20 | 29,067.76 | 0.68 | <.001 | 0.13 |
BIC = Bayesian Information Criterion; AIC = Akaike Information Criterion; BLRt = Bootstrap Likelihood Ratio test; LMR-A = Lo-Mendell Rubin adjusted loglikelihood ratio test.
In Table 4, probability rates per class are displayed, which represent the probability of symptom presence given the specific class (e.g. ‘distress at reminders’ was present in 91% of the children in class three). These rates are also shown in Figure 1. Based on previous specifications in the literature (Burstein et al., 2012), we labelled probability rates as high (≥0.60), moderate (≤0.59 and ≥0.15), and low (<0.15) probability that the symptom was present in the children within a particular class.
Table 4.
Probability of ASD symptom presence for three-class solution (N = 2287).
| |
Low symptoms class (N = 971, 42%) |
Intermediate symptoms class (N = 980, 43%) |
High symptoms class (N = 336, 15%) |
|||
|---|---|---|---|---|---|---|
| Prob. | SE | Prob. | SE | Prob. | SE | |
| Intrusive memories/thoughts | 0.07 | .01 | 0.51 | .03 | 0.91 | .02 |
| Distressing dreams | 0.02 | .01 | 0.16 | .02 | 0.52 | .04 |
| Flashbacks | 0.02 | .01 | 0.17 | .02 | 0.63 | .04 |
| Distress at reminders | 0.04 | .01 | 0.44 | .03 | 0.91 | .02 |
| Negative mood | 0.06 | .01 | 0.25 | .02 | 0.59 | .04 |
| Altered sense of reality | 0.16 | .02 | 0.41 | .03 | 0.73 | .04 |
| Inability to remember some parts | 0.16 | .02 | 0.30 | .02 | 0.49 | .04 |
| Avoid memories/thoughts/feelings | 0.17 | .01 | 0.65 | .03 | 0.89 | .02 |
| Avoid external reminders | 0.04 | .01 | 0.43 | .03 | 0.79 | .03 |
| Sleep disturbance | 0.12 | .02 | 0.30 | .02 | 0.78 | .03 |
| Irritable/angry | 0.05 | .01 | 0.27 | .02 | 0.71 | .03 |
| Hypervigilance | 0.11 | .02 | 0.48 | .03 | 0.87 | .03 |
| Concentration problems | 0.06 | .01 | 0.23 | .02 | 0.70 | .04 |
| Exaggerated startle | 0.04 | .01 | 0.27 | .02 | 0.69 | .03 |
Note. Prob = probability estimate; SE = standard error.
Figure 1.
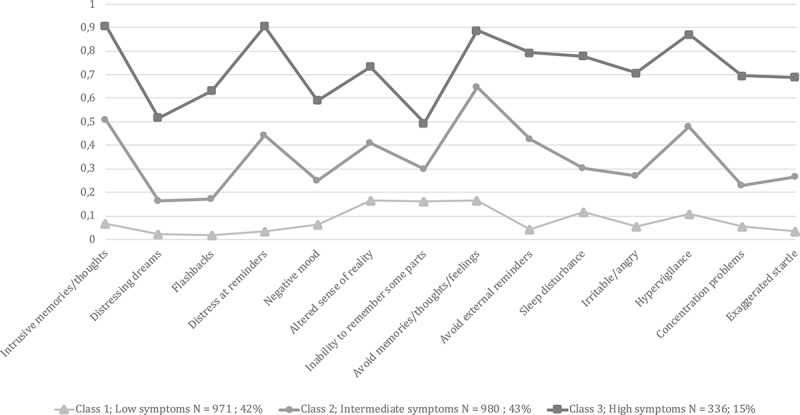
Three-class solution with estimated symptom probabilities per class (n = 2287).
Class 1 consisted of 971 children (42%) and was characterized by a generally low probability of the presence of ASD symptoms, except for ‘altered sense of reality’, ‘inability to remember some parts’, and ‘avoid memories/thoughts/feelings’, which showed a moderate probability. We labelled this class as ‘low symptoms class’. In class 2, 980 children (43%) showed a moderate probability of all ASD symptoms, except for ‘avoiding memories, thoughts, and feelings’, which showed a high probability. This class was named ‘intermediate symptoms class’. Class 3 constituted of 336 children (15%) and was characterized by a high probability of presence of all ASD symptoms, except for a moderate probability for the symptoms ‘distressing dreams’, ‘negative mood’, and ‘inability to remember some parts’. We labelled this class as ‘high symptoms class’. Due to the relatively high number of missing data on any of the ASD symptoms (i.e. n= 986 [43%] children provided complete data on all ASD symptoms), we repeated the LCA with the completers-only subsample. These analyses yielded similar results and conclusions, and are therefore not reported here.
The mean number of ASD symptoms differed between the classes, such that children in the high symptoms class endorsed the highest number of ASD symptoms, followed by the children in the intermediate symptoms class, and thereafter the children in the low symptoms class. Impairment resulting from ASD symptoms was also associated with class membership, such that high symptoms class > intermediate symptoms class > low symptoms class (see Table 5).
Table 5.
Correlates of class membership.
| Total sample | Class 1: low symptoms N = 971 (42%) | Class 2: intermediate symptoms n = 980 (43%) | Class 3: high symptoms n = 336 (15%) | Pairwise comparisons based on multivariate model (N = 2287) |
|
|---|---|---|---|---|---|
| Child gender, N (%) | |||||
| Girl | 832 (36.4%) | 322 (33.2%) | 348 (35.5%) | 162 (48.2%) | 1 = 2 < 3 |
| Boy | 1455 (63.6%) | 649 (66.8%) | 632 (64.5%) | 174 (51.8%) | |
| Age (in years), M (SD) | 11.88 (3.05) | 12.31 (3.01) | 11.54 (3.03) | 11.68 (3.03) | 1 > 2 = 3 |
| Ethnic minority, N (%) | |||||
| Yes | 871 (41.2%) | 345 (37.9%) | 390 (43.8%) | 136 (43.3%) | 1 = 2 = 3 |
| No | 1244 (58.8%) | 566 (62.1%) | 500 (56.2%) | 178 (56.7%) | |
| Parent completed secondary education, N (%) | |||||
| Yes | 934 (78.9%) | 469 (83.3%) | 363 (75.9%) | 102 (71.3%) | 1 > 2 = 3 |
| No | 250 (21.1%) | 94 (16.7%) | 115 (24.1%) | 41 (28.7%) | |
| Trauma typea, N (%) | |||||
| Unintentional injury | 1124 (49.8%) | 526 (54.7%) | 480 (49.5%) | 118 (36.2%) | |
| Acute medical eventa (non-injury) | 113 (5.0%) | 56 (5.8%) | 44 (4.5%) | 13 (4.0%) | 1 = 2 = 3 |
| RTA requiring medical attentiona | 784 (34.7%) | 323 (33.6%) | 329 (34.0%) | 132 (40.5%) | 1 = 2 < 3 |
| Interpersonal violencea | 236 (10.5%) | 57 (5.9%) | 116 (12.0%) | 63 (19.3%) | 1 < 2 < 3 |
| Trauma history, N (%) | |||||
| Yes | 964 (62.0%) | 481 (63.7%) | 374 (61.6%) | 109 (56.6%) | 1 = 2 = 3 |
| No | 591 (38.0%) | 274 (36.3%) | 233 (38.4%) | 84 (43.5%) | |
| Pairwise comparisons based on univariate model (N = 2287) |
|||||
| Number of ASD symptoms endorsed, M (SD) | 3.72 (3.29) | .90 (.89) | 4.47 (1.62) | 9.63 (2.05) | 1 < 2 < 3 |
| Impairment, N (%) | |||||
| Yes | 591 (37.8%) | 146 (20.4%) | 268 (43.4%) | 177 (76.6%) | 1 < 2 < 3 |
| No | 973 (62.2%) | 569 (79.6%) | 350 (56.6%) | 54 (23.4%) |
aUnintentional injury is reference group. Ethnic minority in country of residence; ASD = acute stress disorder; RTA = road traffic accident.
3.2. Predictors of class membership
Table 5 displays the observed means and frequencies for each correlate and the multivariate associations between predictors and probability of class membership (see Supplemental Table S2 for detailed results). Child gender (i.e. being a girl), age (i.e. being younger), parental education (i.e. no completion of secondary education), and trauma type (i.e. having experienced a RTA or interpersonal violence vs. unintentional injuries) were associated with membership of the high symptoms class (vs. low symptoms class), after accounting for the effects of other predictors. Child age (i.e. younger), parental education (i.e. no completion of secondary education), and trauma type (i.e. having experienced interpersonal violence vs. unintentional injuries) were associated with a higher likelihood of being in the intermediate symptoms class (vs. low symptoms class). Child gender (i.e. being a girl) and trauma type (i.e. having experienced a RTA or interpersonal violence vs. unintentional injuries) were associated with a higher probability of membership of the high symptoms class compared with the intermediate symptoms class.
Repeating the multivariate analysis including children with complete data on all predictors (N = 771) showed no meaningful differences in the results, when compared with the imputed data; the same predictors were significantly or not significantly related to classes. Except that for one of the dummies of trauma type (i.e. RTA vs. unintentional injury), the effect was no longer significant for the difference between the high vs. low symptoms class and high vs. intermediate symptoms class. The effect also disappeared for the dummy coded trauma type (i.e. interpersonal violence vs. unintentional injury) for the intermediate vs. low symptoms class (see Supplemental Table S3).
4. Discussion
The aim of our study was to identify latent classes (i.e. homogeneous subgroups) of children exposed to a single-incident PTE based on the presentation of DSM-5 ASD symptoms. Moreover, we examined whether certain factors (gender, age, cultural background, parental education, trauma type, and trauma history) predict membership of ASD classes.
As expected, our LCA resulted in a three-class solution, distinguished based on the number of symptoms endorsed. The vast majority of trauma-exposed children would be classified into a low symptoms class (42%) or an intermediate symptoms class (43%), with a relatively low or moderate probability of endorsement of most ASD symptoms, respectively. In keeping with prior LCA findings in adult PTS, the smallest class (15%) was the high symptoms class, including children with a high probability of endorsement of most ASD symptoms. Further evidence for the clinical meaningfulness of these classes is that they differed significantly regarding functional impairment, with classes endorsing more ASD symptomatology being at higher risk for impairment.
Our finding of a three-class solution based on endorsed amount of ASD symptoms, rather than types of symptoms presented, accords with previous LCA studies on PTSD symptoms in adult populations (Breslau et al., 2005; Hebenstreit et al., 2014; Lenferink et al., 2018; Rosellini et al., 2014). We did not find evidence for qualitative different ASD symptom subtypes in children. Interestingly, the intermediate and high symptoms classes appear to follow almost identical symptom patterns, which supports a dimensional, severity-based conceptualization of mental disorders, such as ASD. An exception is the symptom ‘sleep disturbance’ that showed a tendency towards divergence potentially indicative of different symptom profiles. Here, the high symptoms subgroup depicted a high probability (78%) to report sleep disturbances, which diverged substantially from the intermediate group (30%). As poor sleep quality is known to contribute to increased stress sensitivity and hampered daytime coping (Brewin, Andrews, & Valentine, 2000), it is not surprising if high sleep disturbance in traumatized children concurs with other clinically significant ASD symptoms, while lower sleep disturbance could act as protective factor in the intermediate symptoms class. Overall, the current LCA supports the ASD diagnostic criteria proposed by the DSM-5 (American Psychiatric Association, 2013). According to the DSM-5, symptom requirements are fulfilled when (1) nine out of 14 ASD symptoms are present within the first month following the traumatic incident and (2) the symptoms cause significant distress/impairment in daily life. Thus, congruent with the lack of evidence for qualitatively different symptom profiles, the resulting heterogeneity of possible symptom combinations reflects the conceptualization of ASD as a comprehensive, severity-based diagnosis (Kassam-Adams et al., 2012).
Our second main finding that female gender, younger age, lower parental education, and exposure to interpersonal violence or RTA predicted membership of the high or intermediate symptoms class are in line with earlier studies both in adults (Brewin et al., 2000; Bryant, 2011, 2019; Olff, 2017) and children (Alisic et al., 2014; Trickey et al., 2012). This is especially notable in that these previous studies focused on prevalence rates or mean symptom levels of ASD or PTSD, instead of latent classes of individuals based on ASD symptoms. Prior work found that female gender is related to increased likelihood of ASD in adults as well as in children (Dai et al., 2018). This may be related to observed gender differences in expression of internalizing behaviours, self-blaming thoughts, and threat appraisal and/or in sensitization of the hypothalamus-pituitary-axis (Alisic et al., 2014; Olff, 2017; Tolin & Foa, 2006). Being younger when exposed to a PTE has also been identified earlier as a risk factor (Trickey et al., 2012), potentially related to developmental differences in cognitive capabilities, including knowledge and language, and in emotion-regulation skills (Salmon & Bryant, 2002), which impact the ability to process a PTE (Ehlers & Clark, 2000). The protective effect of parental education in dealing with effects of exposure to PTEs may be understood from the same cognitive theories and also as a marker for socioeconomic class and the accompanying greater resources when a child or family is experiencing stress. Higher educated parents may have the resources that allow them to provide more social support to their child, which has been identified as one of the most important protective factors after trauma (Olff, 2017). Interpersonal trauma (vs. non-interpersonal trauma) has often been associated with greater PTS severity in children, and our findings support this. Interpersonal trauma, more often than non-interpersonal trauma, may lead to negative cognitions about the self (e.g. self-blame), others (e.g. general mistrust in people), and the world (e.g. shattered world assumptions), which in turn impedes functioning (Alisic et al., 2014). RTAs can involve not only negative cognitions, subjective life threat and intense sensory experiences during the PTE, but also the potential involvement of family members in the same PTE with implications for the availability of social support.
This study was based on data from an international data archive (Kassam-Adams et al., in review). The substantial sample size renders it unlikely that the discovered latent symptom profiles are based on low statistical power. Further strengths include the assessment of ASD symptoms within 30 days after trauma exposure at multiple sites and various trauma types. Moreover, the current study focused on the most recent conceptualizations of ASD in the DSM-5. However, findings should be interpreted in the light of several limitations. First, a common difficulty when conducting analysis in large data archives is the handling of missing data. We used FIML to account for missing data on the ASD symptoms in our sample and multiple imputations to account for missing data on predictors. We also conducted analyses on completers, which yielded similar results. Second, the current study did not include longitudinal measures, it remains to be seen if the extracted classes are predictive of long-term symptom disturbance, e.g. if those in the high-symptom-burden ASD class are more likely to develop symptomatic PTSD, a question that is still under debate (Bryant, 2011; Hansen, Hyland, & Armour, 2016; Maercker et al., 2013). Third, we relied on data from child self-report (rather than a parental-proxy report). While this is generally the gold standard for internalizing symptoms such as PTS symptoms, the parental report might provide an additional, and valuable perspective on child ASD symptoms, especially in younger subjects. Further, including parents’ own distress as a predictor for class membership and the children’s long-term development could be a valuable addition in the future research. Fourth, all data were derived from studies conducted in Western high-income countries which might impede generalization of the results in lower-income countries or different cultural backgrounds. Fifth, most single-incident traumas in the current sample were medically related; thus, our study does not cover the full range of single-incident PTEs such as natural disasters or sudden death of a close person.
The current findings may have important clinical implications. To start with, our findings are in line with prior work showing the human capacity to thrive after experiencing PTEs, while only a minority develops severe complaints after a PTE (Galatzer-Levy, Huang, & Bonanno, 2018). The majority of children confronted with a PTE therefore probably do not need treatment for ASD. However, refraining from intervention for children with intermediate or high amount of ASD symptoms within 1 month after trauma exposure may maintain or even exacerbate symptoms over time, since ASD symptoms in children and adolescents after a RTA were found to predict PTSD after 6 months (Dalgleish et al., 2008). Identifying risk factors for ASD for early detection of children at risk for developing (long-lasting) complaints therefore seems to be of clinical importance. Based on our findings, extra attention should be paid to younger and/or female children exposed to a RTA or interpersonal trauma and have parents with a low educational level, as these children seem to have a higher chance of developing ASD symptoms. These results can help hospital staff or mental health professionals in improving screening protocols and detecting children at-risk for ASD for prevention purposes. Furthermore, the intermediate and the high symptoms classes depict similar symptom profiles with elevated symptom peaks for intrusions, distress at reminders, avoidance, and hypervigilance. This might indicate that children who experience these ASD symptoms can benefit from similar treatment. This accords with a meta-analysis indicating similar treatment effects in children with ‘full-blown’ and ‘partial’ PTSD within the first month after exposure to a single-incident trauma (Kramer & Landolt, 2011).
In conclusion, to our knowledge, this is the first study that examined latent classes of DSM-5 ASD symptoms in children after exposure to a PTE. We examined this in a unique sample of over 2,000 acutely traumatized children derived from an international data archive. Our findings support a three class grouping of ASD symptoms based on symptom severity in children who experienced a single-incident PTE. Moreover, predictors of PTS (child gender, age, socioeconomic status, and trauma type) found in prior studies using mean-based methods were supported in these analyses based on latent classes. These findings contribute to a body of work that suggests factors that could help identify children at risk for developing ASD after PTEs.
Funding Statement
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) [R03HD092720].
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed here.
References
- Alisic, E., Barrett, A., Bowles, P., Babl, F. E., Conroy, R., McClure, R. J., … Mehl, M. R. (2015, February 1). Ear for recovery: Protocol for a prospective study on parent–child communication and psychological recovery after paediatric injury. BMJ Open, 5(2), e007393–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alisic, E., Zalta, A. K., Van Wesel, F., Larsen, S. E., Hafstad, G. S., Hassanpour, K., & Smid, G. E. (2014). Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: Meta-analysis. The British Journal of Psychiatry, 204(5), 335–340. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th). Washington, DC: Author. doi: 10.1176/appi.books.9780890423349 [DOI] [Google Scholar]
- Armour, C., Mullerová, J., & Elhai, J. D. (2016). A systematic literature review of PTSD’s latent structure in the diagnostic and statistical manual of mental disorders: DSM-IV to DSM-5. Clinical Psychology Review, 44, 60–74. [DOI] [PubMed] [Google Scholar]
- Asparouhov, T., & Muthén, B. (2014). Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Structural Equation Modeling: A Multidisciplinary Journal, 21(3), 329–341. [Google Scholar]
- Ayer, L., Danielson, C. K., Amstadter, A. B., Ruggiero, K., Saunders, B., & Kilpatrick, D. (2011). Latent classes of adolescent posttraumatic stress disorder predict functioning and disorder after 1 year. Journal of the American Academy of Child & Adolescent Psychiatry, 50(4), 364–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjet, C., Bromet, E., Karam, E. G., Kessler, R. C., McLaughlin, K. A., Ruscio, A. M., … Koenen, K. C. (2016). The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychological Medicine, 46(2), 327–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau, N., Reboussin, B. A., Anthony, J. C., & Storr, C. L. (2005). The structure of posttraumatic stress disorder: Latent class analysis in 2 community samples. Archives of General Psychiatry, 62(12), 1343–1351. [DOI] [PubMed] [Google Scholar]
- Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for post-traumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68, 748–766. [DOI] [PubMed] [Google Scholar]
- Bryant, R. A. (2011). Acute stress disorder as a predictor of posttraumatic stress disorder: A systematic review. The Journal of Clinical Psychiatry, 72(2), 233–239. [DOI] [PubMed] [Google Scholar]
- Bryant, R. A. (2019). Post-traumatic stress disorder: A state-of-the-art review of evidence and challenges. World Psychiatry, 18(3), 259–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burstein, M., Georgiades, K., Lamers, F., Swanson, S. A., Cui, L., He, J.-P., … Merikangas, K. R. (2012). Empirically derived subtypes of lifetime anxiety disorders: Developmental and clinical correlates in U.S. Adolescents. Journal of Consulting and Clinical Psychology, 80(1), 102–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. A., Deblinger, E., Mannarino, A. P., & de Arellano, M. A. (2001). The importance of culture in treating abused and neglected children: An empirical review. Child Maltreatment, 6(2), 148–157. [DOI] [PubMed] [Google Scholar]
- Copeland, W. E., Keeler, G., Angold, A., & Costello, E. J. (2007). Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry, 64(5), 577–584. [DOI] [PubMed] [Google Scholar]
- Costello, E. J., Erkanli, A., Fairbank, J. A., & Angold, A. (2002). The prevalence of potentially traumatic events in childhood and adolescence. Journal of Traumatic Stress, 15(2), 99–112. [DOI] [PubMed] [Google Scholar]
- Cox, C., Kenardy, J., & Hendrikz, J. K. (2010). A randomized controlled trial of a web-based early intervention for children and their parents following unintentional injury. Journal of Pediatric Psychology, 35, 581–592. [DOI] [PubMed] [Google Scholar]
- Dai, W., Liu, A., Kaminga, A. C., Deng, J., Lai, Z., Yang, J., & Wen, S. W. (2018). Prevalence of acute stress disorder among road traffic accident survivors: A meta-analysis. BMC Psychiatry, 18(1), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalgleish, T., Meiser-Stedman, R., Kassam-Adams, N., Ehlers, A., Winston, F., Smith, P., … Yule, W. (2008). Predictive validity of acute stress disorder in children and adolescents. The British Journal of Psychiatry, 192(5), 392–393. [DOI] [PubMed] [Google Scholar]
- de Haan, A., Tutus, D., Goldbeck, L., Rosner, R., & Landolt, M. A. (2019). Do dysfunctional posttraumatic cognitions play a mediating role in trauma adjustment? Findings from interpersonal and accidental trauma samples of children and adolescents. European Journal of Psychotraumatology, 10(1), 1596508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyregrov, A., & Yule, W. (2006). A review of PTSD in children. Child and Adolescent Mental Health, 11(4), 176–184. [DOI] [PubMed] [Google Scholar]
- Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. [DOI] [PubMed] [Google Scholar]
- Fein, J., Kassam-Adams, N., Gavin, M., Huang, R., Blanchard, D., & Datner, E. M. (2002). Persistence of posttraumatic stress in violently injured youth seen in the emergency department. Archives of Pediatrics & Adolescent Medicine, 156(8), 836–840. [DOI] [PubMed] [Google Scholar]
- Feinberg, M. (2004). Demographic and psychological concomitants of ASD and PTSD: An analysis of children after traffic injury (ProQuest. Paper AAI3125815). Graduate School of Education, University of Pennsylvania. Retrieved from http://repository.upenn.edu/dissertations/AAI3125815 [Google Scholar]
- Finkelhor, D., Ormrod, R. K., & Turner, H. A. (2009). Lifetime assessment of poly-victimization in a national sample of children and youth. Child Abuse & Neglect, 33(7), 403–411. [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy, I. R., Huang, S. H., & Bonanno, G. A. (2018). Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clinical Psychology Review, 63(May), 41–55. [DOI] [PubMed] [Google Scholar]
- Hansen, M., Hyland, P., & Armour, C. (2016). Does highly symptomatic class membership in the acute phase predict highly symptomatic classification in victims 6 months after traumatic exposure? Journal of Anxiety Disorders, 40(2016), 44–51. [DOI] [PubMed] [Google Scholar]
- Hebenstreit, C., Madden, E., & Maguen, S. (2014). Latent classes of PTSD symptoms in Iraq and Afghanistan female veterans. Journal of Affective Disorders, 166(2014), 132–138. [DOI] [PubMed] [Google Scholar]
- Hiller, R. M., Meiser-Stedman, R., Lobo, S., Creswell, C., Fearon, P., Ehlers, A., … Halligan, S. L. (2018). A longitudinal investigation of the role of parental responses in predicting children’s post-traumatic distress. Journal of Child Psychology and Psychiatry, 59(7), 781–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn, S. R., Pietrzak, R. H., Schechter, C., Bromet, E. J., Katz, C. L., Reissman, D. B., … Feder, A. (2016). Latent typologies of posttraumatic stress disorder in world trade center responders. Journal of Psychiatric Research, 83(2016), 151–159. [DOI] [PubMed] [Google Scholar]
- Kahana, S. Y., Feeny, N. C., Youngstrom, E. A., & Drotar, D. (2006). Posttraumatic stress in youth experiencing illnesses and injuries: An exploratory meta-analysis. Traumatology, 12(2), 148–161. [Google Scholar]
- Kassam-Adams, N. (2006). The Acute Stress Checklist for Children (ASC-Kids): Development of a child self-report measure. Journal of Traumatic Stress, 19(1), 129–139. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams, N., Garcia-Espana, J., Marsac, M. L., Kohser, K. L., Baxt, C., Nance, M., & Winston, F. (2011). A pilot randomized controlled trial assessing secondary prevention of traumatic stress integrated into pediatric trauma care. Journal of Traumatic Stress, 24(3), 252–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam-Adams, N., Gold, J., Montaño, Z., Kohser, K. L., Cuadra, A., Muñoz, C., & Armstrong, F. D. (2013). Development and psychometric evaluation of child acute stress measures in Spanish and English. Journal of Traumatic Stress, 26(1), 19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam-Adams, N., Kenardy, J. A., Delahanty, D. L., Marsac, M. L., Meiser-Stedman, R., Nixon, R. D. V., ... Palmieri, P. A. (in review). Development of an international data repository and research resource: The Prospective studies of Acute Child Trauma and Recovery (PACT/R) data archive. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam-Adams, N., Palmieri, P. A., Rork, K., Delahanty, D. L., Kenardy, J., Kohser, K. L., … McGrath, C. (2012). Acute stress symptoms in children: Results from an international data archive. Journal of the American Academy of Child & Adolescent Psychiatry, 51(8), 812–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam-Adams, N., & Winston, F. K. (2004). Predicting child PTSD: The relationship between acute stress disorder and PTSD in injured children. Journal of the American Academy of Child and Adolescent Psychiatry, 43(4), 403–411. [DOI] [PubMed] [Google Scholar]
- Kenardy, J., Thompson, K., Le Brocque, R., & Olsson, K. (2008). Information provision intervention for children and their parents following pediatric accidental injury. European Child & Adolescent Psychiatry, 17(5), 316–325. [DOI] [PubMed] [Google Scholar]
- Kramer, D. N., & Landolt, M. A. (2011). Characteristics and efficacy of early psychological interventions in children and adolescents after single trauma: A meta-analysis. European Journal of Psychotraumatology, 2(1), 7858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Brocque, R., Hendrikz, J., & Kenardy, J. (2010). The course of posttraumatic stress in children: Examination of recovery trajectories following traumatic injury. Journal of Pediatric Psychology, 35, 637–645. [DOI] [PubMed] [Google Scholar]
- Lenferink, L. I. M., de Keijser, J., van Denderen, M. Y., & Boelen, P. A. (2018). Latent classes of posttraumatic stress symptoms in two samples of bereaved people. International Journal of Stress Management. doi: 10.1037/str0000121 [DOI] [Google Scholar]
- Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., van Ommeren, M., Jones, L. M., & Reed, G. M. (2013). Diagnosis and classification of disorders specifically associated with stress: Proposals for ICD-11. World Psychiatry, 12(3), 198–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsac, M., Donlon, K., Winston, F., & Kassam-Adams, N. (2013). Child coping, parent coping assistance, and posttraumatic stress following pediatric physical injury. Child: Care, Health & Development, 39(2), 171–177. [DOI] [PubMed] [Google Scholar]
- Marsac, M., Kassam-Adams, N., Delahanty, D., Ciesla, J., Weiss, D., Widaman, K. F., & Barakat, L. P. (2017). An initial application of a bio-psycho-social framework to predict posttraumatic stress following pediatric injury. Health Psychology, 36(8), 787–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meiser-Stedman, R., McKinnon, A., Dixon, C., Boyle, A., Smith, P., & Dalgleish, T. (2017). Acute stress disorder and the transition to posttraumatic stress disorder in children and adolescents: Prevalence, course, prognosis, diagnostic suitability, and risk markers. Depression and Anxiety, 34(4), 348–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meiser-Stedman, R., Smith, P., Glucksman, E., Yule, W., & Dalgleish, T. (2008). The posttraumatic stress disorder diagnosis in preschool- and elementary school-age children exposed to motor vehicle accidents. American Journal of Psychiatry, 165, 1326–1337. [DOI] [PubMed] [Google Scholar]
- Meiser-Stedman, R., Yule, W., Smith, P., Glucksman, E., & Dalgleish, T. (2005). Acute stress disorder and posttraumatic stress disorder in children and adolescents involved in assaults or motor vehicle accidents. American Journal of Psychiatry, 162, 1381–1383. [DOI] [PubMed] [Google Scholar]
- Minihan, S., Liddell, B. J., Byrow, Y., Bryant, R. A., & Nickerson, A. (2018). Patterns and predictors of posttraumatic stress disorder in refugees: A latent class analysis. Journal of Affective Disorders, 232, 252–259. [DOI] [PubMed] [Google Scholar]
- Morrow, K. B., & Sorell, G. T. (1989). Factors affecting self-esteem, depression, and negative behaviors in sexually abused female adolescents. Journal of Marriage and the Family, 51(3), 677–686. [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (2012). Mplus user’s guide (Vol. 7). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nixon, R., Ellis, A., Nehmy, T., & Ball, S. (2010). Screening and predicting posttraumatic stress and depression in children following single-incident trauma. Journal of Clinical Child & Adolescent Psychology, 39(4), 588–596. [DOI] [PubMed] [Google Scholar]
- Nylund, K. L., Asparouhov, T., & Muthén, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4), 535–569. [Google Scholar]
- Olff, M. (2017). Sex and gender differences in post-traumatic stress disorder: An update. European Journal of Psychotraumatology, 8(sup4), 1351204. [Google Scholar]
- Pailler, M., Kassam-Adams, N., Datner, E., & Fein, J. (2007). Depression, acute stress and behavioral risk factors in violently injured adolescents. General Hospital Psychiatry, 29, 357–363. [DOI] [PubMed] [Google Scholar]
- Rosellini, A. J., Coffey, S. F., Tracy, M., & Galea, S. (2014). A person-centered analysis of posttraumatic stress disorder symptoms following a natural disaster: Predictors of latent class membership. Journal of Anxiety Disorders, 28(1), 16–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon, K., & Bryant, R. A. (2002). Posttraumatic stress disorder in children: The influence of developmental factors. Clinical Psychology Review, 22, 163–188. [DOI] [PubMed] [Google Scholar]
- Sanders-Phillips, K., Moisan, P. A., Wadlington, S., Morgan, S., & English, K. (1995). Ethnic differences in psychological functioning among black and latino sexually abused girls. Child Abuse & Neglect, 19(6), 691–706. [DOI] [PubMed] [Google Scholar]
- Sebre, S., Sprugevica, I., Novotni, A., Bonevski, D., Pakalniskiene, V., Popescu, D., … Lewis, O. (2004). Cross-cultural comparisons of child-reported emotional and physical abuse : Rates, risk factors and psychosocial symptoms. Child Abuse & Neglect, 28, 113–127. [DOI] [PubMed] [Google Scholar]
- Shevlin, M., Hyland, P., & Elklit, A. (2014). Different profiles of acute stress disorder differentially predict posttraumatic stress disorder in a large sample of female victims of sexual trauma. Psychological Assessment, 26(4), 1155–1161. [DOI] [PubMed] [Google Scholar]
- Steenkamp, M. M., Nickerson, A., Maguen, S., Dickstein, B. D., Nash, W. P., & Litz, B. T. (2012). Latent classes of PTSD symptoms in Vietnam veterans. Behavior Modification, 36(6), 857–874. [DOI] [PubMed] [Google Scholar]
- Stein, J. A., Golding, J. M., Siegel, J. M., Burnam, M. A., & Sorenson, S. B. (1988). Long-term psychological sequelae of child sexual abuse: The Los Angeles epidemiologic catchment area study. In Wyatt G. E. & Powell G. J. (Eds.), Lasting effects of child sexual abuse (Vol. 100, Sage focus ed., pp. 135–154). Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- Tolin, D. F., & Foa, E. B. (2006). Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin, 132(6), 959–992. [DOI] [PubMed] [Google Scholar]
- Trickey, D., Siddaway, A. P., Meiser-Stedman, R., Serpell, L., & Field, A. P. (2012). A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review, 32(2), 122–138. [DOI] [PubMed] [Google Scholar]
- van de Schoot, R., Sijbrandij, M., Winter, S. D., Depaoli, S., & Vermunt, J. K. (2017). The GRoLTS-checklist: Guidelines for reporting on latent trajectory studies. Structural Equation Modeling: A Multidisciplinary Journal, 24(3), 451–467. [Google Scholar]
- Vermunt, J. K. (2010). Latent class modeling with covariates: Two improved three-step approaches. Political Analysis, 18(4), 450–469. [Google Scholar]
- Zatzick, D., Grossman, D. C., Russo, J., Pynoos, R., Berliner, L., Jurkovich, G., … Rivara, F. P. (2006). Predicting posttraumatic stress symptoms longitudinally in a representative sample of hospitalized injured adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 45, 1188–1195. [DOI] [PubMed] [Google Scholar]
- Zehnder, D., Meuli, M., & Landolt, M. A. (2010). Effectiveness of a single-session early psychological intervention for children after road traffic accidents: A randomised controlled trial. Child and Adolescent Psychiatry and Mental Health, 4, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


