Abstract
Frailty is a pronounced symptom of aging associated with multiple comorbid states and adverse outcomes. The aim of this study was to evaluate the impact of 2 interventions, one based on prevention of falls and the other on prevention of loneliness, on total frailty and dimensions of frailty in urban community-dwelling elderly as well as associations with independent living.
This prospective interventional study followed up 410 persons aged 75 to 95. The participants of the control and intervention groups were monitored through a public health intervention programme. The level of frailty was measured by the Tilburg Frailty Indicator (TFI) questionnaire and the factors of independent living were analyzed using validated questionnaires.
After 1 year, physical frailty measured in the control group showed a statistically significant increase (r = −0.11), while in the intervention groups physical frailty did not increase (both P > .05). Psychological frailty measured after 1 year in the control group was significantly higher (r = −0.19), as well as in the group where the public health interventions to reduce loneliness were carried out (r = −0.19). Psychological frailty did not increase in the group in which public health interventions to prevent falls were carried out, and social frailty did not increase at all in the study period. The total level of frailty in the control group after 1 year was significantly increased (r = −0.19), while no increase was seen in the overall frailty in the intervention group. Multivariate analysis has shown that both interventions where independently associated with lower end frailty. Additionally, higher baseline frailty and visit to a physician in the last year were positively associated with higher end-study frailty level, while higher number of subjects in the household and higher total psychological quality of life (SF-12) were independently associated with lower end-study frailty. Only in the prevention of falls group there was no increase in restriction in the activities of daily living throughout study follow-up.
Public health interventions to prevent falls and to prevent loneliness have a positive effect on the frailty and independent living of the elderly living in their own homes in an urban community.
Keywords: elderly persons, frailty, independent living, public health interventions
1. Introduction
Frailty is perceived as a geriatric syndrome which is a reflection and consequence of the dysfunction of several organ systems.[1–3] While no common and universally accepted definition exists, it is most commonly defined as a state associated with increased vulnerability to adverse outcomes due to the decline in reserve and functions in multiple physiological systems.[4] Studies in Europe which examined overall (defined as physical or psychosocial) frailty or frailty defined as complex phenotype point to the category of “severely frail,” which includes between 1/3 and 1/2 of elderly persons living in the European states.[5,6] Two recent meta-analyses presented data on epidemiology of frailty. Meta-analysis by O’Caoimh et al[7] which analyzed data on frailty, defined using any definition, irrespective of the method of data collection or instrument used, from 68 unique datasets with data from 22 European countries showed that overall prevalence of frailty in the elderly population is 18%, being 12% in community-dwelling elderly and 45% in non-community based studies. The other meta-analysis by Siriwardhana et al[8] which examined the prevalence of frailty and prefrailty measured by any assessment method among community-dwelling older adults in low-income and middle-income countries showed that the prevalence of frailty varied from 3.9% in China to 51.4% in Cuba, while the prevalence of prefrailty ranged from 13.4% in Tanzania to 71.6% in Brazil. Additionally, demographic data on aging indicate that the number of elderly persons with frailty will increase, which is why frailty is defined as a priority in public health and health care system for the elderly.[9,10] In cohort studies, it was found that the prevalence of frailty defined by various methods ranges from 4% to 59% but there is a significant difference between various methodological approaches and there are ambiguities in comparing data from different geographic areas.[5,6]
The clinical picture of frailty in the elderly is characterized by an increased vulnerability caused by reduced functional abilities in all physiological systems, which results in the reduced ability to face the everyday or acute stressors.[11–14] Frail elderly persons are classified as vulnerable social groups because of the effects on their quality of life, the institutionalized care, and unwanted health and death outcomes. Especially vulnerable are elderly persons with concomitant chronic diseases, exposed to acute infections or acute confusion and those who were exposed to falls.[15–18]
In this study of frailty among the elderly, an integrative model of frailty based on a multidimensional approach was used, with an estimation of physical, psychological, and social dimensions of frailty.[19] Research shows that most of the elderly in European countries prefer to remain independent and continue to live in their own homes.[20,21] Numerous support programmes help elderly persons to stay in their homes and remain independent as long as possible,[21,22] because, according to the research, most of the elderly in Europe are still in good condition and capable of living independently.[23] However, according to the research data, to be capable to live independently at home an elderly person needs a certain state of mental health and satisfactory functional capacity.[24,25] Therefore, in this research of independent living of the elderly, focus has been placed on the analysis of the functional capacity of the elderly. The recognition of frailty in the elderly and an early intervention within the framework of primary health care are important for the care of the elderly. Interventions aiming to reduce frailty contribute to changes in the levels of frailty and affect the costs for the elderly persons’ health care. The rationale for designing and studying interventions aiming to prevent the frailty in the elderly has shown the efficacy of combined interventions.[4,26] However, while it has been shown that frailty is associated with higher risk of falls and more pronounced loneliness, there is still insufficient evidence of the effect of interventions aimed at decreasing risk of falls and level of loneliness on frailty. Faber et al[27] examined the effects of a 20-week moderate intensity group-exercise program on falls in nonfrail, pre-frail, and frail individuals. The randomized trial showed that frailty was a strong effect modifier and that, surprisingly, the intervention had opposite effects in different frailty classifications, non-significantly reducing fall risk in pre-frail subjects and significantly increasing fall risk in frail subjects and the study concluded that physical interventions to reduce falls should be targeted to nonfrail and pre-frail subjects and could be counterproductive and increase falls in frail persons. Moreover, there is a clear association between loneliness and physical and total frailty[28–30] and different activities have been shown to mediate the relationship between loneliness and frailty[31] so our hypothesis was that interventions aimed at loneliness and risk of falls reduce the level of frailty in community-dwelling elderly urban population.
2. Methods
2.1. Study design and participants
Enrolment for this prospective interventional study was conducted between January 2015 and September 2017. Study was conducted in city of Rijeka which is an urban environment in Primorje-Gorski Kotar County with a population of some 128,000 of which 19.74% over 65 years of age and an aging index of 169.8 (data from Croatian Bureau of Statistics). Pilot site Rijeka was 1 of 5 pilot sites included in the project Urban Health Centres Europe (UHCE) for testing preventive integrated health and social care approach for community-dwelling elderly persons. According to last census data, aging index of Rijeka (169.8) is higher than that of state capital Zagreb (111.6) and also Croatia (116.3). According to latest Eurostat data the aging index of 28 members of European Union is 125.8 (data from: https://ec.europa.eu/eurostat). This higher aging index makes Rijeka an especially suitable location for testing interventions aimed at elderly population. However, the same interventions carried here are equally implementable in other urban communities with different ageing indices.
This study was approved by the Ethical Committee - Faculty of Medicine University of Rijeka (IRB No:07–04–2014; 2170–24–01–14–02). All subjects provided informed consent. The study included 410 elderly persons living in their own homes, 283 women and 127 men aged median 80 years (min–max range 75–95). Inclusion criteria were: age 75 years or older, independent living, expected to be able to participate in the study for at least 6 months according to the assessment of their community nurse. The following exclusion criteria were defined: permanent residence outside the urban community, dementia or psychosis, accommodation in an institution for old and helpless persons, persons who are not able to comprehend the basic information on the study or not able to cognitively evaluate the risks and benefits of participation and are not expected to be able to make an informed decision regarding participation in the study. At the beginning of the study frailty, multiple morbidity, polypharmacy, visits to doctors, and the hospitalization of the elderly were evaluated. Upon these data the clinical profile, pathological risk, and residual skills of the elderly were determined. Participants gave their informed consent to participate in the research for the period of 1 year. Before and after the public health intervention programme was conducted the visiting nurses interviewed participants in the control and the intervention group. Physicians, physiatrists, and physiotherapists were involved in the implementation of the public health intervention programme to prevent falls. Along with the visiting nurses, also medical and health professionals of the Department for Social Medicine of the Faculty of Medicine of the University and Rijeka and the Department for Public Health of the Faculty of Health Studies of the University of Rijeka participated in the public health intervention to reduce loneliness.
2.2. Measurement
Frailty was measured with the Tilburg Frailty Indicator (TFI) questionnaire, which was developed and validated for primary health care use.[32,33] TFI measures physical frailty (including components: perception of physical health, inexplicable weight loss, walking difficulties, difficulty in maintaining balance, hearing impairments, visual impairments, lack of strength in the arms, and physical fatigue), psychological frailty (including components: memory problems, the feeling of being lost, nervous or anxious, inability to deal with problems), and social frailty (including components: perception of life, lack of social relationships, and lack of social support). The independent living analysis is based on measurements with the Groningen Activity Restriction Scale which includes activities of daily living (ADL) items on everyday life activities such as clothing, feeding, hygiene, and instrumental activities from daily living (IADL). The instrument on everyday life activities essential to maintaining a certain quality of life such as driving, communication management, financial management, preparing meals, going shopping, and in addition the total restriction of activities /GARS.[34]
2.3. Interventions
The public health intervention “fall prevention” consisted of 2 activities: determining and eliminating the risk of falls in the intervention participants home and organized custom exercise twice a week. The nurses at the participants’ home pointed out the risky obstacles in the space, educating the participants about safe movement in old age. Physiotherapists and physiotherapy students designed and maintain custom exercise for elderly at 4 locations in the City of Rijeka.
The public health intervention “reducing loneliness” consisted of organized weekly and monthly education and workshops for the elderly, which were also conducted over a period of 1 year. Weekly trainings on “healthy aging” were conducted in cooperation elderly NGOs. Monthly workshops were provided as part of the program activities Healthy City Rijeka.
Elderly persons resident in the Western part of the City of Rijeka were included in the intervention groups, and the control group consisted of the elderly resident in the Eastern part of the City of Rijeka. Participants were interviewed at the beginning of the research and participants from the Western part of the city were free to choose and participate in 1 of the 2 interventions according to their preference.
2.4. Statistical analysis
Descriptive statistics are summarized as frequencies (percentages) for categorical variables. The normality of the distribution of continuous variables was tested with the Kolmogorov–Smirnov test. In all cases, median and interquartile ranges were used as central tendency and scattering measures, while nonparametric statistical tests were used to test differences within and between the studied groups of participants. The McNemar test was used for the differences with regard to the categorical variables between the 2 metering points and the Wilcoxon test of equivalent pairs was used to compare the other aging parameters between two time points expressed as continuous variables. In the case of statistically significant differences, these differences were additionally examined by the post-hoc Mann–Whitney U test series with Bonferroni correction of the level of statistical significance. Univariate relationship between frailty and independent living was investigated using the Spearman correlation coefficient. Linear multiple regression was used to predict the factors significant for frailty after the interventions. We have scoped a number of large intervention studies in frailty and found that the effect sizes of the interventions (intragroup differences) on total frailty (measured using Tilburg Frailty Indicator [TFI] which we also used in this study) range from Cohen d of 0.5 to 0.6, which is consistent with our hypothesis of small to medium effect size. We have thus taken a conservative estimate of Cohen d of 0.45 (corresponding to small effect size), 2-tailed hypothesis α = 0.05 and β = 0.80 which resulted in a sample size of 79 subjects per group. We have planned to enrol 158 patients in the control group and 79 patients in each intervention group for a total of 316 subjects in the study. The level of statistical significance was determined at P < .05 (2-tailed). All data were analyzed with the IBM SPSS v23 (Armonk, NY: IBM Corp., USA).
3. Results
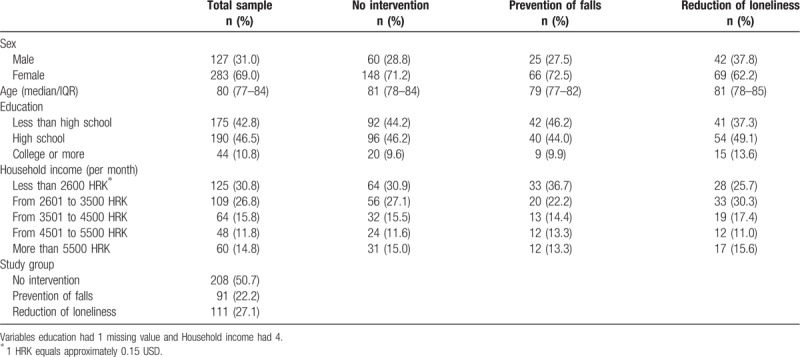
A total of 410 elderly subjects were included in the study. Among the active elderly persons, 91 (22.2%) were involved in the public health intervention programme to prevent falls, while 111 (27.1%) of elderly persons were involved in the intervention programme to prevent loneliness. The control group with inactive elderly persons numbered 208 (50.7%) subjects. Observing the respondents’ marital status, the first point of measurement showed that most of them were widowers (210/410, 51.2%), followed by married persons (176/41,042, 9%), persons living in living extramarital relationships (1/410, 0.2%), singles (11/410, 2.7%), and divorced (12/410, 2.9%) (Table 1).
Table 1.
Baseline demographic characteristics of subjects.
At the beginning of the study there were 38 (9.3%) smokers, while 145 (35.4%) of respondents consumed alcohol. At the beginning of the study 177 (43.2%) of participants had a partner. There was statistically no significant difference between beginning and end of study concerning the number of persons living in the household (P = .19). The proportion of smokers between the 2 time points also decreased (P = .001), as well as the proportion of elderly persons who at least occasionally consume alcohol (P < .001) (Table 2).
Table 2.
Marital status, household, and alcohol use.

After 1 year, physical frailty measured in the control group showed a statistically significant increase (z = −2.25; P = .024; r = −0.11), while in the intervention groups physical frailty did not increase (both P > .05). Psychological frailty measured after 1 year in the control group was significantly higher (z = −3.87; P < .001; r = −0.19), as well as in the group where the public health interventions to reduce loneliness were carried out (z = −2.07; P = .039; r = −0.19). Psychological frailty did not increase in the group in which public health interventions to prevent falls were carried out, and social frailty did not increase at all in the study period. The total level of frailty in the control group after 1 year was significantly increased (z = −3.84, P < .001, r = −.19), while no increase was seen in the overall frailty in the intervention groups (Table 3).
Table 3.
Measurement of total, physical, psychological, and social frailty in study groups at the beginning and end of study.

When assessing between group differences we compared differences in change of frailty over time and found that the 3 groups differed in the rate of change, that is, physical frailty increased more in the control group than in prevention of falls group (P = .045), while there were no differences among the control group and prevention of loneliness group or between the 2 intervention groups (P = .24 and P > .99, respectively). Additionally, there were no statistically significant between group differences in the rate of change of total, psychological, or social frailty (all P > .05), but total frailty showed a non-significantly higher rate in the control group compared with the 2 intervention groups (P = .08).
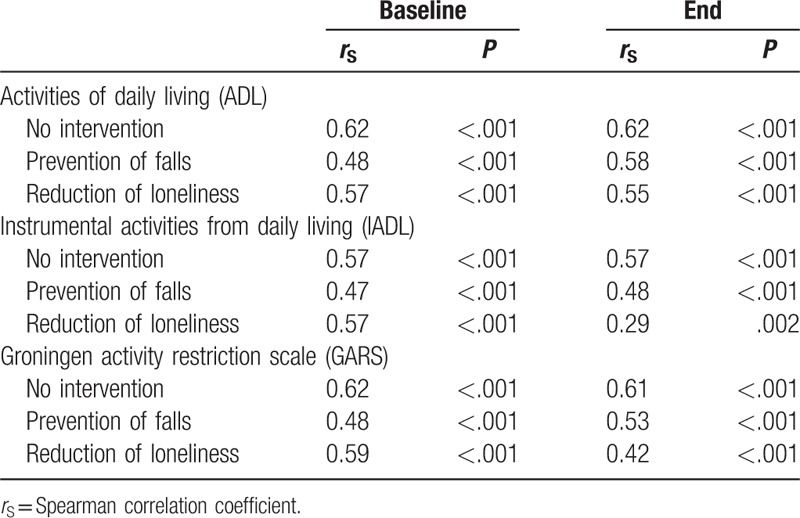
The analysis of independent living showed that after 1 year in the control group there was a statistically significant increase in ADL values, along with restrictions in daily activities (z = −6.35, P < .001, r = −0.32). The same was observed in the group in which public health interventions to reduce loneliness were carried out (z = −2.51; P = .012; r = −0.17). In the group in which the intervention programme to reduce physical frailty (prevention of falls) was carried out, there was no increase in ADL restriction values after 1 year in the respondents’ daily activities. The IADL measurements relating to the capability of carrying out more complex tasks related to life quality has shown an increase in the IADL restriction values in all 3 of the study groups: the control group (z = −7.52, P < .001, r = −0.37), the group with interventions to reduce loneliness (z = −5.57; P < .001; r = −0.38), and the group with interventions to prevent falls (z = −3.20; P = .001; r = −0.24). In conclusion, the results of the total GARS restrictions showed the highest increase in the control group (z = −7.58; P < .001; r = −0.38), a slightly smaller increase in the group with interventions to reduce loneliness (z = −4.98; P < .001; r = −0.35), and the lowest increase was found in the group with interventions to prevent falls (z = −2.45; P = .014; r = −0.35). In determining the relationship between frailty and independent living in all groups of participants, a statistically significant connection of frailty with both forms of restriction was obtained, ADL and IADL—as well as in the overall result of GARS restrictions. All of these correlations were positive, which means that a higher level of frailty is associated with a higher degree of ADL restrictions in daily activities and IADL complex tasks related with the quality of life (Tables 4 and 5).
Table 4.
Restrictions in activities of daily living by intervention and time point.

Table 5.
Correlation between frailty and activities of daily living.
The variables included in the predictive multivariate model of frailty in the elderly were as follows: demographic characteristics, initial level of frailty, public health interventions, quality of life, independent living, and the use of health care. The tested variables explained 56.5% of the variance in the second time point of measurement (R2 = 0.565, F = 24.91, df1 = 19, df2 = 365, P < .001). Multivariate analysis also shown that both interventions where independently associated with lower end frailty (both P < .05). Additionally, higher baseline frailty and visit to a physician in the last year were positively associated with higher end-study frailty level, while higher number of subjects in the household and higher total psychological quality of life (SF-12) were independently associated with lower end-study frailty (all P < .05) (Table 6). Total frailty was included in the final regression model due to potential multicollinearity problem if physical, psychological, and social frailty are included separately in one regression model. However, testing this potential model with all 3 dimensions of frailty included showed that it did not improve on the final model with total frailty included ( , 0.541 vs 0.542, respectively).
, 0.541 vs 0.542, respectively).
Table 6.
Multivariate linear regression analysis showing predictors of final/end study frailty (N = 385).

4. Discussion
The study analyzed the physical, psychological, and social nature of frailty in order to get a comprehensive view on the frailty of the elderly, and in order to do so an integrated conceptual model of frailty was implemented.
While few well-designed trials were designed specifically to target incidence and characteristics of pre-frailty and frailty in the elderly, some trials have shown success. Frailty Intervention Trial (FIT) which recruited 216 persons and showed that a multifactorial, interdisciplinary approach tailored for each individual subject and targeted specifically to reduce the frailty component present on baseline exam consisting of dietetic evaluation and nutritional intervention, measures to reduce social isolation and physiotherapy and exercise regime significantly reduced frailty in a 12-months period.[35,36] Recent randomized, open label, controlled trial by Serra-Prat et al[37] showed that nutritional assessment and potential intervention and physical intervention consisting of aerobic, strengthening, balance, and coordination exercises are effective in preventing frailty in community-dwelling pre-frail individuals. Tarazona-Santabalbina et al[38] performed a randomized controlled trial which showed that a multicomponent exercise intervention reverses frailty and improves cognition, emotional, and social networking in rural community-dwelling elderly population.
Physical frailty, defined as a syndrome characterized by reduced strength, reduced endurance, and reduced physiological functions that increase the vulnerability of an individual, as well as his/her dependence on others, is associated with multiple negative health outcomes.[10] Previous studies established that physical frailty is associated with consequences such as falls, dependency, hospitalization, institutionalization, and death.[10,11,39] According to this study, in inactive elderly person's physical frailty increased significantly throughout the study period, which is most probably a consequence of the reduction of strength and endurance. This is in accordance with other research findings and studies with a similar timeframe and duration which showed that physical inactivity is associated with frailty in the elderly.[40] Our study also analyzed the effect of combined interventions to reduce frailty in the elderly and established that both public health interventions had an effect on the level of physical frailty. The public health intervention programme to prevent falls has had an effect on the physical frailty level, which confirms the other finding of the study, that is, that elderly frail persons should practice physical activity.[41,42] The effect of the intervention to reduce loneliness on physical frailty is interpreted by the interest of elderly persons in the preservation of their health, which motivated them to move more in order to attend organized activities such as lectures, workshops, and focus groups. A study by Bortz[14] was one of the first to define the phenotype of frailty and to show that frail subjects are at a higher risk of falls. Frequent falls are associated with lower quality of life and interventions including physical exercise alone or combined with various interventions has shown to lower the risk of injurious falls compared with usual care.[43] Results of the ongoing “Sarcopenia and Physical frailty IN older people: multi-component Treatment strategies” (SPRINTT) phase III multicenter randomized controlled trial might offer more insight on the long-term effect of multicomponent interventions which impact frailty and reduce mobility disability.[44]
Psychological frailty includes cognitive, motivational, and mood components. In the study an increase in psychological frailty was found in 3/4 of the participants. Our results confirmed that with the progression of age psychological frailty of inactive and active elderly persons also increases. Taking into account the results of numerous epidemiological studies which reported that frailty increases the risk of cognitive decline, this study confirmed the above findings on the psychological-functional decline in the elderly.[45]
Studies have defined social frailty as a continuity of risk of losing resources important for meeting one or more basic social needs. The results in this study did not show an increase in social frailty in any of the study groups, however there was no significant effect of either intervention on the reduction of social frailty.[46] Design of studies aimed to specifically reduce social frailty is of utmost importance, since several studies have showed that social frailty is associated with adverse outcomes and disability in community-dwelling elderly.[47,48] This is emphasized even more when evaluating the results of a recent study by Zhang et al[49] which showed that social frailty was independently associated with both physical and mental health-related quality of life, even after controlling for physical and psychological frailty and the findings of a cross-sectional study by Makizako et al[50] which reported that social frailty was associated with more than twice the odds for muscle weakness. Furthermore, a prospective study by Yamada[51] which followed up a cohort of Japanese community-dwelling elderly showed that both socially prefrail and frail had significantly higher risks for incident disability and mortality.
The results of independent living of the elderly show that in 2/3 of the participants with the progression of age we also find the progression of restrictions in daily activities—ADLs. Participants in the intervention group to prevent falls did not show any increase in restrictions of their daily activities, so it was concluded that the adjusted public health care intervention for the elderly was effective. The results suggest that multi-component exercise programmes have a positive effect on ADL for frail elderly persons.[42,52,53] Research has shown that independent living largely depends on the ability to perform more complex tasks related to the quality of life—IADL.[54,55] The results of this study show an increase in IADL restriction in all participants and confirm the findings of previous research that with the progression of age psychological frailty increases too, that is, the cognitive health of the elderly decreases. There was no effect after applying the combined interventions for IADL of the elderly, which is interpreted by the need for an individual approach to improve the performance of complex independent living tasks. This fact is pointed out in a review study of IADL interventions concerning the capability of elderly persons, which concludes that interventions must be client-focused, along with specific activities of multidisciplinary teams aiming to assist elderly persons who live alone in the community.[56]
The study has some limitations. While subjects were broadly enrolled according to place of residence and allocated to intervention or control, there was no randomization between the 2 intervention groups and participants were free to choose the intervention they wanted. The possibility that subjects which are more health-conscious, prone to physical activity and generally healthier chose to be enrolled in the intervention arms might be a source of selection bias (i.e., “healthy-user bias”). Additionally, there could potentially, but very unlikely, be a difference in the characteristics of elderly subjects between the Western and Eastern part of the city, but both parts very probably had similar demographic structures. We believe that the freedom of choice in selecting the intervention contributed to a more “real-world” aspect of the study. To further prove this case, we decided to test if there were any differences in no intervention group (including only subjects from Eastern part of the city) and interventions group (both interventions taken together, i.e., including only subjects from Western part of the city) and found no differences in baseline characteristics which further supported our hypothesis and reduced potential for bias (data not shown). Blinding was not possible as the interventions differed visibly and significantly among each other and compared to control. Additionally, persons which accepted to be enrolled might differ from the general elderly population and therefore the results cannot be extrapolated to different populations (e.g., rural). Men comprised only around 31% of subjects enrolled in our study which is comparable with the proportion of men of 33.3% in the general population of Croatia aged ≥75 years (source: Croatian Bureau for Statistics, www.dzs.hr). Moreover, the male-to-female ratio in our study is similar to that in other studies and is a consequence of at least 2 important intersex differences: difference in life expectancy and consequent higher proportion of women in the elderly population (mean life expectancy men vs women, 75 vs 81 years, source: EU 2018 Ageing Report) and it is well-known and described in several studies not only that sex plays a role in health-risk and health-promoting behavior,[57,58] including higher prevalence of physical inactivity in men,[59] but also that men are less likely to seek medical help or participate in health-promotion programs.[60] And that men comprise only around 20% of samples in health behavior research studies.[61] A total of 385 (93.9%) subjects had complete data and were included in the regression analysis. Moreover, none of the variables had ≥1.2% missing values. While this posed only a 6.1% reduction in sample size, we performed a missing-value analysis and compared baseline data of included versus excluded patients and found that excluded patients did not differ in any of the baseline characteristics (age, sex, education, study group, and household income; data not shown).
The study established a connection between frailty and independent living, as well as restrictions in ADL, IADL, and GARS. A higher degree of frailty was associated with a higher degree of restrictions of ADL and IADL, which corroborates the results of a systematic review and a meta-analysis which showed frailty is associated with functional capacity and is a significant predictor of the occurrence and worsening of ADL and IADL restrictions.[62] The results of investigating the predictability of frailty show a lower degree of frailty among the elderly in households with a larger number of members because there is more help available to them in their day-to-day activities and in performing more complex tasks which are related to their quality of life. A higher level of psychosocial adjustment, that is, a higher psychological quality of life (when the elderly person is satisfied with the way, the conditions, and possibilities of life) is a predictor of a lower degree of frailty in the elderly. If the elderly are more frail it is expected that they will visit the family medicine outpatient facility more often. The findings of the study confirm that frailty in the elderly is related to increasing age, the status of single living, reduced functional capacity, quality of life, risk of falls and bone fractures.[63–65]
5. Conclusions
Our study showed that with increasing age, physical frailty also increases in inactive urban elderly persons due to the lack of maintaining stamina and reduction of force. Combined interventions of exercise and health care have a positive effect on the physical frailty of the elderly. Psychological frailty increases in active and inactive elderly persons due to the decline of cognitive abilities upon which the public health interventions have no significant effect. On the other hand, they have a positive effect on social frailty because they contribute to the fulfilment of the social needs of the elderly. A key factor in the independent living among the elderly is the functional capacity in which with the age the restrictions related to the daily activities of the elderly (ADL) increase. In this respect, public health interventions consisting of organized and client-focused physical exercises for the elderly have proven to be effective. With age, also the ability to perform more complex tasks related to quality of life (IADL) declines, due to the decrease in cognitive health caused by the psychological frailty of the elderly.
A higher degree of frailty of the elderly is associated with a higher degree of restrictions of ADL, IADL, and GARS. A lower degree of frailty of elderly persons envisions more family members and a higher capability of the elderly to adjust. Regular visits to the family medicine outpatient clinics are predictor of greater frailty of the elderly.
Acknowledgment
The authors thank all the participants and researchers for their cooperation in this research and for the support of the research thanks to the Faculty of Medicine, University of Rijeka, Primorje-Gorski Kotar County Health Centre, City of Rijeka.
Author contributions
None.
Footnotes
Abbreviations: ADL = activities of daily living, GARS = Groningen Activity Restriction Scale, IADL = instrumental activities from daily living.
How to cite this article: Ožić S, Vasiljev V, Ivković V, Bilajac L, Rukavina T. Interventions aimed at loneliness and fall prevention reduce frailty in elderly urban population. Medicine. 2020;99:8(e19145).
The authors have no conflicts of interest to disclose.
References
- [1].Clegg A, Young J, Iliffe S, et al. Frailty in elderly people. Lancet 2013;381:752–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Xue QL. The frailty syndrome: definition and natural history. Clin Geriatr Med 2011;27:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Ruiz M, Cefalu C, Reske T. Frailty syndrome in geriatric medicine. Am J Med Sci 2012;344:395–8. [DOI] [PubMed] [Google Scholar]
- [4].Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: a call to action. J Am Med Dir Assoc 2013;14:392–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Collard RM, Boter H, Schoever RA, et al. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 2012;60:1487–92. [DOI] [PubMed] [Google Scholar]
- [6].Santos-Eggimann B, Cuénoud P, Spagnoli J, et al. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. J Gerontol A Biol Sci Med Sci 2009;64:675–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].O’Caoimh R, Galluzzo L, Rodríguez-Laso Á, et al. Prevalence of frailty at population level in European ADVANTAGE Joint Action Member States: a systematic review and meta-analysis. Ann Ist Super Sanita 2018;54:226–38. [DOI] [PubMed] [Google Scholar]
- [8].Siriwardhana DD, Hardoon S, Rait G, et al. Prevalence of frailty and prefrailty among community-dwelling older adults in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open 2018;8:e018195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Rechel B, Grundy E, Robine JM, et al. Ageing in the European union. Lancet 2013;381:1312–22. [DOI] [PubMed] [Google Scholar]
- [10].Cesari M, Prince M, Thiyagarajan JA, et al. Frailty: an emerging public health priority. J Am Med Dir Assoc 2016;17:188–92. [DOI] [PubMed] [Google Scholar]
- [11].Fried LP, Hadley EC, Walston JD, et al. From bedside to bench: research agenda for frailty. Sci Aging Knowledge Environ 2005;2005:pe24. [DOI] [PubMed] [Google Scholar]
- [12].Lipsitz LA. Dynamics of stability: the physiologic basis of functional health and frailty. J Gerontol A Biol Sci Med Sci 2002;57:B115–25. [DOI] [PubMed] [Google Scholar]
- [13].Fried LP, Tangen C, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146–56. [DOI] [PubMed] [Google Scholar]
- [14].Bortz WM. The physics of frailty. J Am Geriatr Soc 1993;41:1004–8. [PubMed] [Google Scholar]
- [15].Lang IA, Hubbard RE, Andrew MK, et al. Neighborhood deprivation, individual socioeconomic status, and frailty in older adults. J Am Geriatr Soc 2009;57:1776–80. [DOI] [PubMed] [Google Scholar]
- [16].Topinková E. Aging disability and frailty. Ann Nutr Metab 2008;52:6–11. [DOI] [PubMed] [Google Scholar]
- [17].Walston J, Hadley EC, Ferrucci L, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc 2006;54:991–1001. [DOI] [PubMed] [Google Scholar]
- [18].Eeles EM, White SV, O’Mahony SM, et al. The impact of frailty and delirium on mortality in older inpatients. Age Ageing 2012;41:412–6. [DOI] [PubMed] [Google Scholar]
- [19].Bergman H, Béland F, Karunananthan S, et al. English translation of article published in ‘Gérontologie et société’. Dévelopment d’un cadre de travail pour comprendre et étudier la fragilité. Gérontol Société 2004;109:15–29. [Google Scholar]
- [20].Harrefors C, Sävenstedt S, Axelsson K. Elderly people's perceptions of how they want to be cared for: an interview study with healthy elderly couples in Northern Sweden. Scand J Caring Sci 2009;23:353–60. [DOI] [PubMed] [Google Scholar]
- [21].Stula S. Living in Old Age in Europe. Current Developments and Challenges. Working Paper No. 7 of the Observatory for Socio-political Developments in Europe; 2012. [Google Scholar]
- [22].Seah B, Kowitlawakul Y, Jiang Y, et al. A review on healthy ageing interventions addressing physical, mental and social health of independent community-dwelling older adults. Geriatr Nurs 2019;40:37–50. [DOI] [PubMed] [Google Scholar]
- [23].Wahrendorf M, Siegrist J. Are changes in productive activities of older people associated with changes in their well-being? Results of a longitudinal European study. Eur J Ageing 2010;2:59–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Bravell ME, Berg S, Malmberg B. Health, functional capacity, formal care and survival in the oldest old: a longitudinal study. Arch Gerontol Geriatr 2007;46:1–4. [DOI] [PubMed] [Google Scholar]
- [25].Beswick AD, Gooberman-Hill R, Smith A, et al. Maintaining independence in older people. Rev Clin Gerontol 2010;20:128–53. [Google Scholar]
- [26].Apóstolo J, Cooke R, Bobrowicz-Campos E, et al. Efficacy of interventions to prevent pre-frality and frailty progression in older adults: a systematic review. JBI Database System Rev Implement Rep 2018;16:140–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Faber MJ, Bosscher RJ, Chin A, et al. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: a multicenter randomized controlled trial. Arch Phys Med Rehabil 2006;87:885–96. [DOI] [PubMed] [Google Scholar]
- [28].Gale CR, Westbury L, Cooper C. Social isolation and loneliness as risk factors for the progression of frailty: the English Longitudinal Study of Ageing. Age Ageing 2018;47:392–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Herrera-Badilla A, Navarrete-Reyes AP, Amieva H, et al. Loneliness is associated with frailty in community-dwelling elderly adults. J Am Geriatr Soc 2015;63:607–9. [DOI] [PubMed] [Google Scholar]
- [30].Ganesalingam G. Higher risk of physical frailty in older person is associated with increased levels of loneliness rather than social isolation. Evid Based Nurs 2019;22:116. [DOI] [PubMed] [Google Scholar]
- [31].Zhao M, Gao J, Li M, et al. Relationship between loneliness and frailty among older adults in nursing homes: the mediating role of activity engagement. J Am Med Dir Assoc 2019;20:759–64. [DOI] [PubMed] [Google Scholar]
- [32].Gobbens RJ, van Assen MA, Luijkx KG, et al. The Tilburg frailty indicator: psychometric properties. J Am Med Dir Assoc 2010;11:344–55. [DOI] [PubMed] [Google Scholar]
- [33].Gobbens RJ, Luijkx KG, Wijnen-Sponselee MT, et al. Towards an integral conceptual model of frailty. J Nutr Health Aging 2010;14:175–81. [DOI] [PubMed] [Google Scholar]
- [34].Suurmeijer TP, Doeglas DM, Moum T, et al. The Groningen activity restriction scale for measuring disability: its utility in international comparisons. Am J Public Health 1994;84:1270–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Fairhall N, Aggar C, Kurrle SE, et al. Frailty Intervention Trial (FIT). BMC Geriatr 2008;8:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Cameron Ian D, Fairhall N, Langron C, et al. A multifactorial interdisciplinary intervention reduces frailty in older people: randomized trial. BMC Geriatr 2013;11:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Serra-Prat M, Sist X, Domenich R, et al. Effectiveness of an intervention to prevent frailty in pre-frail community-dwelling older people consulting in primary care: a randomised controlled trial. Age Ageing 2017;46:401–7. [DOI] [PubMed] [Google Scholar]
- [38].Tarazona-Santabalbina FJ, Gómez-Cabrera MC, Pérez-Ros P, et al. A multicomponent exercise intervention that reverses frailty and improves cognition, emotion, and social networking in the community-dwelling frail elderly: a randomized clinical trial. J Am Med Dir Assoc 2016;17:426–33. [DOI] [PubMed] [Google Scholar]
- [39].Chen X, Mao G, Leng SX. Frailty syndrome: an overview. Clin Interv Aging 2014;9:433–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Vermeulen J, Neyens J, van Rossum E, et al. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: a systematic review. BMC Geriatr 2011;11:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Cesari M, Vellas B, Hsu FC, et al. A physical activity intervention to treat the frailty syndrome in older persons-results from the LIFE-P study. J Gerontol A Biol Sci Med Sci 2015;70:216–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].De Labra C, Guimaraes-Pinheiro C, Maseda A, et al. Effects of physical exercise interventions in frail older adults: a systematic review of randomized controlled trials. BMC Geriatr 2015;15:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Tricco AC, Thomas SM, Veroniki AA, et al. Comparisons of Interventions for preventing falls in older adults: a systematic review and meta-analysis. JAMA 2017;318:1687–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Agosta L, Bo M, Bianchi L, et al. Polypharmacy and sarcopenia in hospitalized older patients: results of the GLISTEN study. Aging Clin Exp Res 2019;31:557–9. [DOI] [PubMed] [Google Scholar]
- [45].Robertson DA, Savva GM, Kenny RA, et al. Frailty and cognitive impairment—A review of the evidence and causal mechanisms. Ageing Res Rev 2013;12:840–51. [DOI] [PubMed] [Google Scholar]
- [46].Bunt S, Steverink N, Olthof J, et al. Social frailty in older adults: a scoping review. Eur J Ageing 2017;14:323–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Kojima G. Prevalence of frailty in nursing homes: a systematic review and meta-analysis. J Am Med Dir Assoc 2015;16:940–5. [DOI] [PubMed] [Google Scholar]
- [48].Teo N, Gao Q, Nyunt MSZ, et al. Social frailty and functional disability: findings from the Singapore longitudinal ageing studies. J Am Med Dir Assoc 2017;18: 637.e13-637.e19. [DOI] [PubMed] [Google Scholar]
- [49].Zhang X, Tan SS, Franse CB, et al. Association between physical, psychological and social frailty and health-related quality of life among older people. Eur J Public Health 2019;29:936–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Makizako H, Kubozono T, Kiyama R, et al. Associations of social frailty with loss of muscle mass and muscle weakness among community-dwelling older adults. Geriatr Gerontol Int 2019;19:76–80. [DOI] [PubMed] [Google Scholar]
- [51].Yamada M. Arai H social frailty predicts incident disability and mortality among community-dwelling Japanese older adults. J Am Med Dir Assoc 2018;19:1099–103. [DOI] [PubMed] [Google Scholar]
- [52].Daniels R, van Rossum E, de Witte L, et al. Interventions to prevent disability in frail community-dwelling elderly: a systematic review. BMC Health Serv Res 2008;8:278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Cadore EL, Rodríguez-Mañas L, Sinclair A, et al. Effects of different exercise interventions on risk of falls, gait ability, and balance in physically frail older adults: a systematic review. Rejuvenation Res 2013;16:105–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Baker MW. Creation of a model of independence for community dwelling elders in the United States. Nurs Res 2005;54:288–95. [DOI] [PubMed] [Google Scholar]
- [55].Suchy Y, Williams P, Kraybill M, et al. Instrumental activities of daily living among community dwelling elderly: Personality associations with self-report, performance, and awareness of functional difficulties. J Gerontol B Psychol Sci Soc Sci 2010;65:542–50. [DOI] [PubMed] [Google Scholar]
- [56].Orellano E, Colón WI, Arbesman M. Effect of occupation- and activity-based interventions on instrumental activities of daily living performance among community-dwelling older adults: a systematic review. Am J Occup Ther 2012;66:292–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Mahalik, Burns SM, Syzdek M. Masculinity and perceived normative health behaviors as predictors of men's health behaviors. Soc Sci Med 2007;64:2201–9. [DOI] [PubMed] [Google Scholar]
- [58].Ryan J, Lopian L, Le B, et al. It's not raining men: a mixed-methods study investigating methods of improving male recruitment to health behaviour research. BMC Public Health 2019;19:814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Noble N, Paul C, Turon H, et al. Which modifiable health risk behaviours are related? A systematic review of the clustering of Smoking, Nutrition, Alcohol and Physical activity (‘SNAP’) health risk factors. Prev Med 2015;81:16–41. [DOI] [PubMed] [Google Scholar]
- [60].Yousaf O, Grunfeld EA, Hunter MS. A systematic review of the factors associated with delays in medical and psychological help-seeking among men. Health Psychol Rev 2015;9:264–76. [DOI] [PubMed] [Google Scholar]
- [61].Maher CA, Lewis LK, Ferrar K, et al. Are health behavior change interventions that use online social networks effective? A systematic review. J Med Internet Res 2014;16:e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Kojima G. Frailty as a predictor of disabilities among community-dwelling older people: a systematic review and meta-analysis. Disabil Rehabil 2017;39:1897–908. [DOI] [PubMed] [Google Scholar]
- [63].Fhon JRS, Rodrigues RAP, Santos JLF, et al. Factors associated with frailty in older adults: a longitudinal study. Rev Saude Publica 2018;52:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Gobbens RJ, Van Assen M. The prediction of quality of life by physical, psychological and social components of frailty in community-dwelling older people. Qual Life Res 2014;23:2289–300. [DOI] [PubMed] [Google Scholar]
- [65].Vermeiren S, Vella-Azzopardi R, Beckwée D, et al. Frailty and the prediction of negative health outcomes: a meta-analysis. J Am Med Dir Assoc 2016;17:1163.e1–7. [DOI] [PubMed] [Google Scholar]


