Abstract
Background:
The electronic medical record (EMR) is considered to be a vital tool of information and communication technology (ICT) to improve the quality of medical care, but the limited adoption of EMR by physicians results in a considerable warning to its successful implementation. The purpose of the present review is to explore and identify the potential barriers perceived by physicians in the adoption of EMR.
Methods:
The systematic review was carried out based on literature published in 5 databases: PubMed, Web of Science, Scopus, The Cochrane Library, and ProQuest from 2014 to 2018, concerning barriers perceived by physicians to the adoption of EMR.
Results:
The present study incorporates 26 articles based on their appropriateness out of 1354 for the final analysis. Authors explore 25 barriers that appeared 112 times in the literature for the present review; the top 5 frequently mentioned barriers are privacy and security concerns, high start-up cost, workflow changes, system complexity, lack of reliability, and interoperability.
Conclusion:
The systematic review explores that physicians deal with different barriers as they intend to adopt EMR. The barriers explored in the present review are the potential to play as references for the implementer of the EMR system. Thus an attentive analysis of the definitive condition is needed before relevant intervention is determined as the implementation of EMR must be considered as a behavioral change in medical practice.
Keywords: adoption, barriers, electronic medical record, physicians, review
1. Introduction
It has considerably consented that the usage of information technology (IT) in healthcare offers inclusive potentiality for improving the excellence, efficacy, and competence of the provided services, as well as personnel, meanwhile reduces the organizational overheads.[1,2] Electronic medical record (EMR) is considered as the incorporation of several information tools (e.g., test ordering, electronic prescription, decision support system, digital imagery, and telemedicine) would improve clinical decision-making. However, using such evidence in everyday clinical practice might advocate a secure and effective healthcare system.[3] Previous studies confirmed several benefits of EMR,[4] and one of the main benefits stated, is to improve quality of care ensuring the access of patients’ vital health information from different providers, that considerably improves the coordination of care,[5] and the efficiency of healthcare practice.[6]
Regardless of the several advantages mentioned above, the previous studies also reported that the overall adoption rate of EMR is comparatively low.[6,7] Sines and Griffin[8] explored that several prior clinical system implementations had failed due to a lack of the physicians’ adoption. As physicians are the significant user-group of patients’ care, their intention to adopt EMR determines the overall success of its implementation. Nonetheless the previous study revealed that physicians would not be interested in using a system that interferes with their workflow and modifies the way they care for patients.[7] Therefore, identifying barriers affecting physicians’ intention to adopt EMR is believed to be one of the critical elements in confirming its optimal integration and ultimately measure the benefits within the healthcare system. Thus, the aim of the present study is to explore and evaluate the potential barriers perceived by physicians regarding the adoption of EMR. We are positive that the critical factors, which have been recognized by the current review, can potentially help the implementers to develop relevant policies and regulations regarding EMR adoption by physicians more clearly in the future.
2. Methods
2.1. Search strategy and key terms
Five databases, including PubMed, Web of Science, Scopus, The Cochrane Library, and ProQuest, were used to obtain the articles for the present review. Keywords such as “physician,” “doctor,” “electronic health record” (EHR), “electronic medical record,” “acceptance,” “adoption,” “barrier,” and “factor” were employed in different combinations in Boolean AND/OR to search paper.
2.2. Eligibility criteria
Studies explored based on the above strategies had to further come across the following eligibility criteria to be incorporated in the present review: must be written in English and published between 2014 and 2018; be focused only on EMR/EHR usage, not included studies regarding other health information system (HIS); imitate original research work published in the peer-reviewed journal, thus studies exhibited in the dissertation, conference, and proceeding were not eligible; accessible from scientific databases enabling both open access and subscription services.
2.3. Included studies
By using the differing database search strategies, 1354 potential papers were identified. After the initial screening, 95 papers were eliminated because of their resemblance. Out of the remaining 1259 papers, 1191 were excluded as they did not meet the selection criteria (the title, abstract, and keywords). Of the remaining 68 papers, 42 were eliminated after reviewing study context, design, and literature review, hence a lack of significant contribution. Thus, 26 papers that met the inclusion criteria were selected for the final analysis. Figure 1 reports the extensive selection process, and Table 1 reports all the potential papers, as well as the potential barriers explored by authors.
Figure 1.
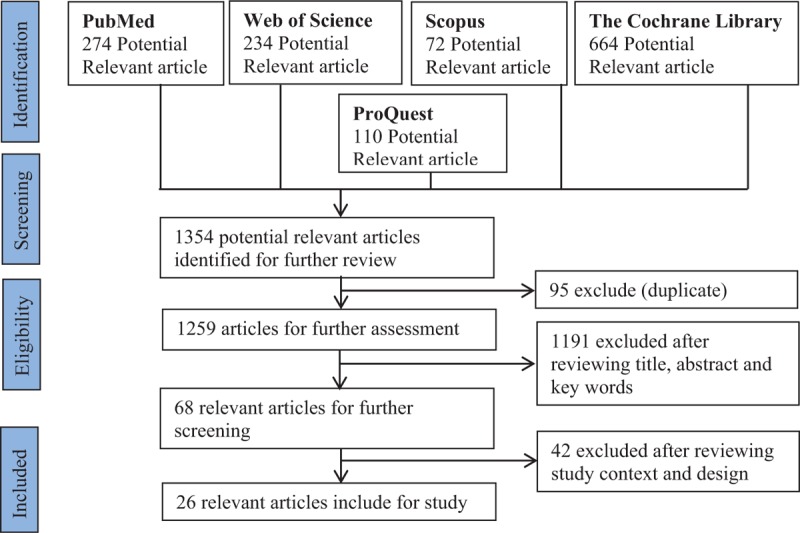
The selection process of the studies included in the present systematic review. → represents the next step. Identification: In this step, authors started to search the 5 databases to identify the relevant articles for the present study. Screening: In this step, the authors screened the initially obtained studies by title, abstract, and keywords, focusing on reasons to exclude the studies. Eligibility: In this step, the authors considered the criteria that were employed to select articles for the present study based on the research objectives. Included: In this step, authors finally selected the articles, used for the present study, based on the research objectives.
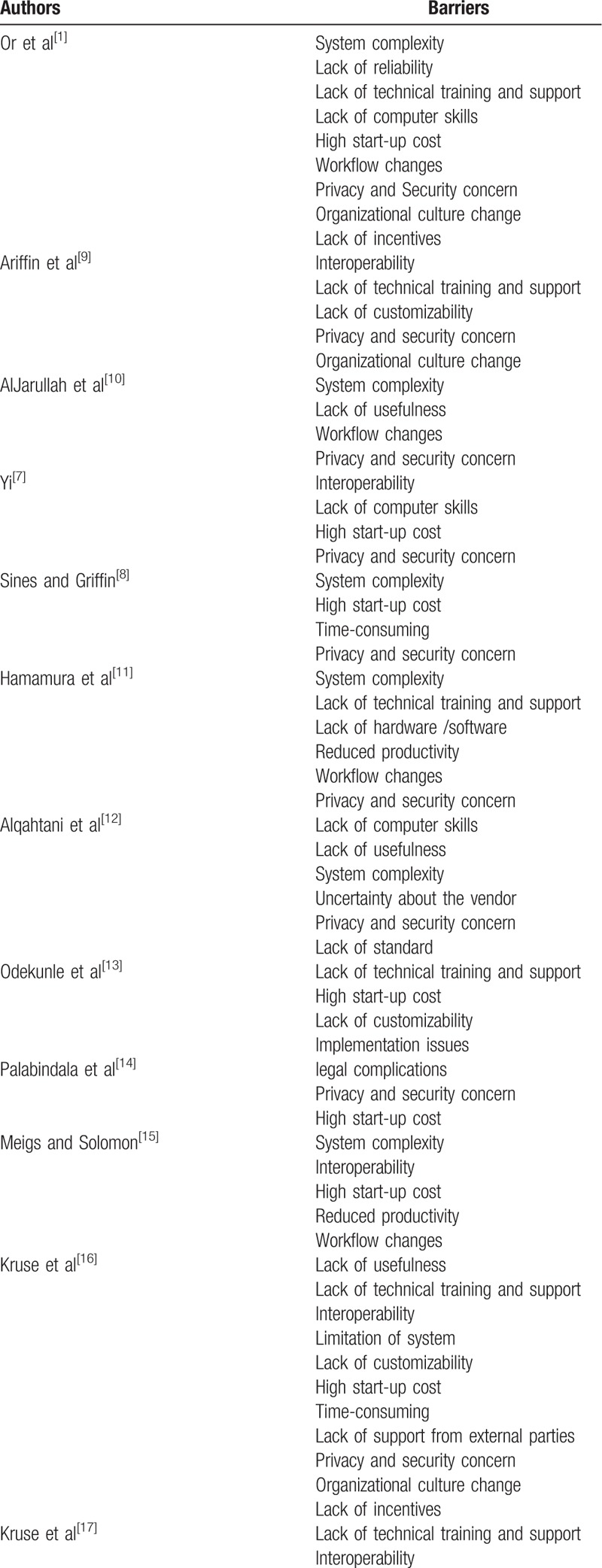
Table 1.
Analysis of studies included in this review.
2.4. Ethical consent
Ethical consent was not called for the present review as no human participants are involved in the present study. The present study reviews and explores the barriers in previously published papers regarding physicians’ intention to adopt the EMR system based on the predetermined objectives of the present study.
3. Results
3.1. Principle findings
By applying different search strategies, a total of 25 barriers were identified, and these 25 barriers appeared 112 times in total. The comprehensive list of the total number of barriers, their sources, and the frequencies of these barriers appeared in the review are reported in Table 2.
Table 1 (Continued).
Analysis of studies included in this review.
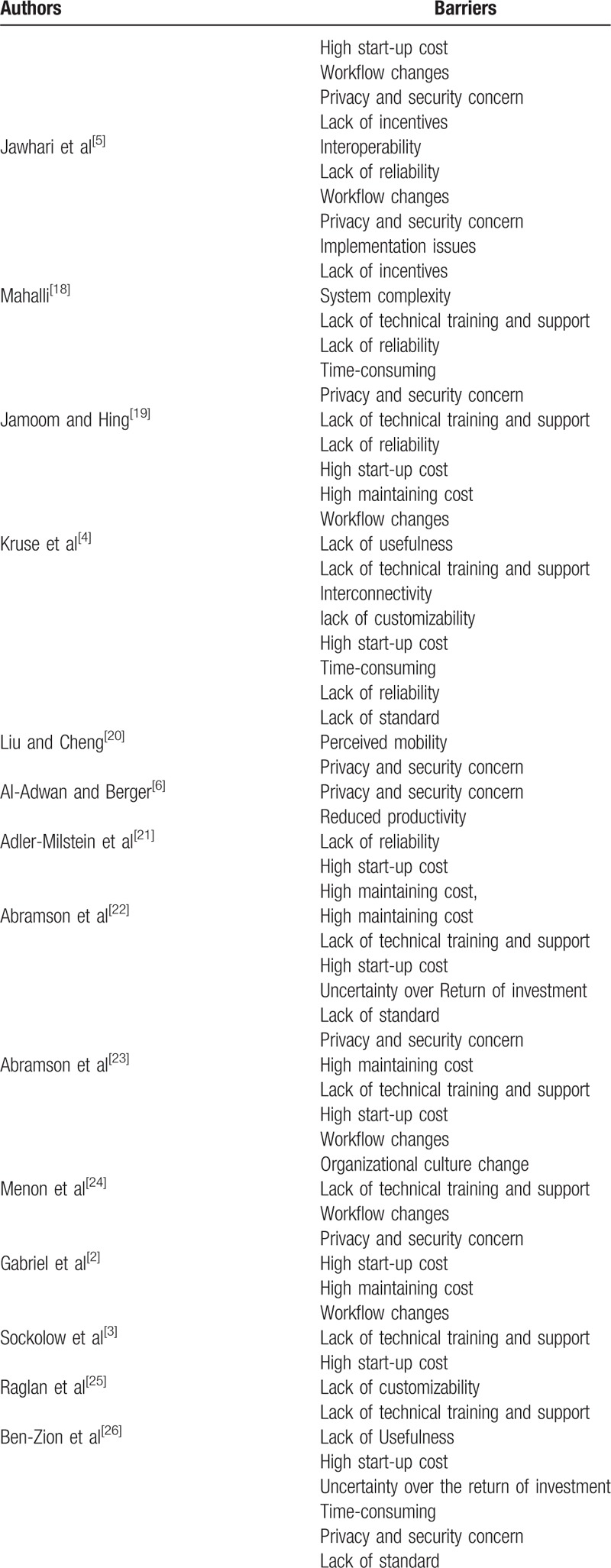
Table 2.
Frequency of barriers.
From Figure 2, we can find that “Privacy and security concerns” is reported as the key barrier to the implementation of EMR appeared 15.2% of all incidents (17/112).[1,5–12,14,16–18,20,22,24,26] High start-up cost emerged 14.3% of all incidents (16/112)[1–4,7,8,13–17,19,21–23,26] and workflow changes emerged 8.04% of all occurrences (9/112)[1,2,5,10,11,17,19,23,24] stood 2nd and 3rd, respectively. System complexity emerged in 6.3% of all occurrences (7/112)[1,8,10–12,15,18] and lack of reliability[1,4,5,18,19,21] and interoperability[5,7,9,15–17] each appeared 5.4% of all occurrences (6/112) stood 4th and 5th, respectively. Lack of customizability,[4,9,13,16,25] lack of usefulness,[4,10,12,16,26] time consuming,[4,8,16,18,26] and high maintaining cost[2,19,21–23] each appeared 4.5% of all incidents (5/112). Lack of incentives,[1,5,16,17] organizational culture change,[1,9,16,23] and lack of standard,[4,12,22,26] emerged 3.6% of all occurrences (4/112).
Figure 2.
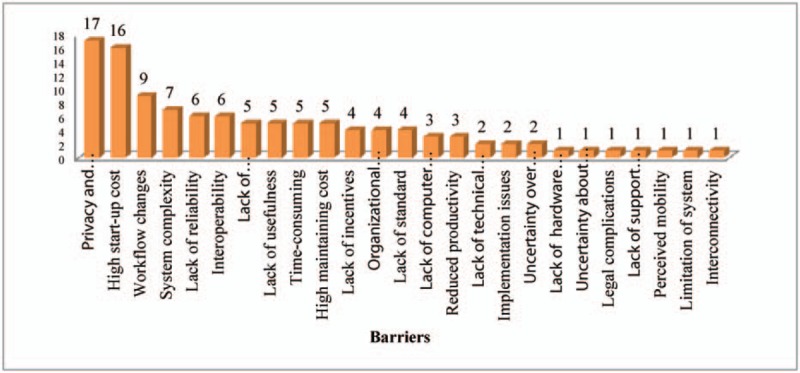
The total number of potential barriers and the total number of times these barriers appear in the present review. How many times each barrier appears are represented vertically. The horizontal line states the total number of barriers.
3.2. The main barriers and research utilization
Based on the findings of the present study, the top 5 barriers are as follows: “privacy and security concerns,” “high start-up cost,” “workflow changes,” “system complexity,” “lack of reliability,” and “interoperability” (Table 2). It is interesting to keep in mind that even if the studies were conducted in 5 years and different geographic settings, not many differences in the type of mentioned barriers are evident. “Privacy and security concerns” is stated around 65% of all included studies (17/26), which make it the key and top of the list of all barriers. Although every study mostly focused on the principle barriers, in some studies, barriers such as “lack of computer skills,” “reduced productivity,” “lack of technical training and support,” “implementation issues,” “uncertainty over the return of investment,” “lack of hardware/software,” “uncertainty about the vendor,” “legal complications,” “lack of support from external parties,” “perceived mobility,” “limitation of system,” and “interconnectivity” appeared 3 or fewer times, categorized as a secondary barrier.
3.3. Demographic data
On the per-country basis, most of the studies, 11 papers, conducted in the United States, represent more than half. The rest of the studies mainly were conducted in Asia (Taiwan, Malaysia, Hong Kong, Korea, Jordan, and Saudi Arabia) and Africa (Kenya, Sub-Saharan Africa). In terms of age of respondents, 5 out of 26 papers[6,13,15,18,25] indicate that 30 to 45 years old is the prime age group of physicians intended to adopt EMR. Regarding the gender effect, 6 out of 26 papers[1,6,15,18,20,25] explore this issue. Gender differences denote both psychologic and physical differences between male and female physicians regarding their intention to adopt EMR. The finding of the present study indicates that male physicians are more interested in adopting EMR than their female counterparts, and male physicians consider that EMR could improve their performance by cutting down medical errors and the time required for treatment. On the specialty issue, 5 out of 26 papers[15,18,20,23,25] report that physician's intention to adopt EMR differs among different medical specialties. Literature indicated that the different specialties have different requirements in terms of patients’ care, information collection, and clinical documentation methodologies together with, differences in standard clinical work, invoicing, compliance necessities, and specialty-specific terminology. The findings of the present study indicate that some specialties, such as internal medicine, and surgery are in favor of adopting EMR than other specialties. The 4 out of 26[1,6,15,18] papers indicate that physicians’ maturity regarding professional efficiency (10–12 years) influences physicians’ intention to adopt EMR.
4. Discussion
The present review found that the privacy and security concerns barrier seems to employ a considerable adverse impact on physicians’ intention to adopt EMR.[1,5,6–12,14,16–18] Physicians are indeterminate whether EMR is trustworthy to store patient's information as the unauthorized access of the stored information could be possible, which leads them to legal problems besides losing patient's trust. Even most of the physicians using EMR believe that storing patient's information in EMR is riskier than paper records in terms of security and confidentiality. There is a clear indication of the extent to which physicians perceived definitive policies associated with the design and implementation of the EMR system. Jawhari et al[5] emphasized that insufficient policy and legislation could play a vital role regarding the physicians’ perceived intention to adopt EMR and indirectly influences the overall success of EMR implementation. Thus, physicians consider that government should come out with a comprehensive security and privacy standard regarding the storage of medical information and strictly instructs parties involved in the implementation of EMR such as vendors, and healthcare providers, to follow the regulations while implementing the EMR system, that could ease the physicians’ concerns and also improve their trust in the EMR system.
Lack of interoperability, restricting physicians’ capability to exchange electronic information between other general practices or with HIS they use, is also considered one of the other primary barriers.[7,9,15–17] Meigs and Solomon[15] explored that providers have stated their dissatisfaction with the lack of interoperability instituted by government agencies, which allows the dormant nature of EMR development at the vendor, and significantly restricts the specialty regarding systems development. However, interoperability is essential as it reduces the cost of EMR, improves diffusion and evaluation of advanced medical knowledge among physicians, and makes the EMR system achievable for an individual or small group of physicians.
Financial barriers were the critical system-level measurement determining physician's adoption of EMR, from the high start-up to the maintaining cost: a concern emphasized in previous studies.[1–4,7,8,9,13–17,21–23] According to the study findings of Adler-Milstein et al[21] physicians who are working in the hospital are more likely to use and adopt EMR than those who practice privately. Physicians practice in private is most preferably to mention high start-up and ongoing cost as the vital barriers to EMR adoption. Sixteen out of 26 papers reported that high start-up costs are one of the primary and critical barriers to physicians adopting EMR, but only 5 articles associated “high maintenance cost” to the adoption of EMR.[19,21–23] Thus additional qualitative researches would be needed to determine the influence of high maintenance cost with other potential barriers regarding physician's intention to adopt EMR.
Implementation of EMR changes the unique way of patient care, which is developed by physicians over the years, and is itself a critical concern. As the change in patient care not only goes along with a switch from the paper records to the EMR system, also leads to change in organizational aspects. Or et al[1] explored difficulties that arise during the workflow change process, for example, lack of incentives, change of organizational culture, issues regarding implementation, creating a barrier to improve the quality of care. Thus, an EMR friendly culture could support organization-wide use of EMR and improve the potential of successful implementation of EMR.
Currently, most of the EMR systems tended to be “one-size-fits-all” with features and tabs that may be practicable for some specialties but not others. Currently used EMR system adapted overall recommendations advocated by different specialties to fulfill the requirements of all specialties. Thus, EMR system developers must carefully look into the problem regarding the lack of specialty related functions as different specialties have different requirements. However, EMR developers have recently developed specialty-specific EMR systems. Though, it is still not clear what kind of effects this specialty-specific program will have on the implementation of the EMR system soon.
Customizability states the capability to be adapted to the system that breaks down to comply with the definitive requirement of the user applications.[9] Several studies explored that physicians are unwilling to adopt EMR as they find the system cannot meet their specific needs.[4,9,13,16,25] Thus it appears that more effort is needed from the implementers and healthcare providers of EMR to improve EMR customizability, which in other ways, can improve physicians’ intention to adopt EMR.
Literature has provided evidence that the implementation of EMR can improve the quality of medical care, but a lack of financial incentives is regarded as a critical barrier to physicians adopting EMR. Though, despite physicians find some personal benefit from practicing EMR, they could not be interested in adopting it and will stick to their traditional patient care process. Hwang et al[27] and Vishwanath and Scamurra[28] explored that though physicians perceive some personal incentives during the implementation of EMR, the implementation of EMR will not reach the predicted level. Remarkably, the incentives measured in the literature were mainly financial ones. Nonetheless, this finding is not consistent[10] as several studies explored the inconclusive effect of financial incentives on EMR adoption.[1,7,9] Thus, further investigation is required regarding the effect of financial incentives on physicians’ intention to adopt EMR.
Several studies explored that physician's lack of technical knowledge and skills to cope with EMR as one of the vital barriers for adopting EMR.[1,7,12] Alqahtani et al[12] stated that EMR use introduces a new kind of medical errors: typos. Additionally, it is not only a problem for physicians but also for other medical staff, who have insufficient computer skills. This general lack of skills obstructs the comprehensive adoption of EMR. Thus, implementers should create the proper environment to support the physicians to come out with this problem, which could be efficient in both ways: it could improve physicians’ technical ability and intention to adopt EMR.
The time required to enter the patient's record is another critical complexity for physicians as they are more comfortable with the summaries, handwritten notes, histories, and so on.[18] Mahalli[18] indicated that data entry was both burdensome and time-consuming for physicians as decent typing skills are required to enter patient medical information, notes, and prescriptions into the EMR system, and several physicians are not comfortable with doing it. Thus, physicians generally need a long time to enter the patient's record, which restricts them to stop the consultation in the middle and interrupts the flow of the patient's care. For this reason, time consumed to enter the patient's record becomes a commonly experienced problem among physicians. This barrier may also be associated with the complexity of the EMR system, lack of technical training and support, as well as the time required to learn a new system. As the time of physicians is limited and they are unable to spend time to be familiar with the EMR system, thus the organization must organize the proper training for physicians and inspire them to spend time with the EMR system to be intimate, which in other ways, develops physicians’ intention to adopt the EMR system.
Previous studies concluded that the implementation of EMR changes and slows down physicians’ workflow, as physicians needed additional time to learn the system, which in other ways, degrade their productivity and increase their workload.[6,11,15] This condition may bring financial losses, such as a loss of revenue. Thus, implementers must come up with policies such as financial exemption in case of adopting EMR, etc, to fulfill their initial losses and encourage physicians to adopt EMR for long-term betterment in their medical practice as well as for their improvement in terms of finance and revenue.
Previous studies indicated that a lack of technical support from vendors is being considered as a vital barrier to the adoption of EMR by physicians. So, the eminence of vendors is vital for the adoption of EMR as it is still relatively new in the market.[11] Physicians are concerned that vendors may not be capable of providing proper technical assistants, or may run out of business and disappear from the market, causing a great loss of technical support and finance too.[1,11] That is one of the many reasons physicians are reluctant to spend high costs for implementing the EMR system without the confidence in trustworthy and highly regarded vendors.
4.1. Contributions and limitations
The present review also contributes to theory and practice in multiple ways. Firstly, implementers should consider the findings of the present review as a synopsis of concerning barriers perceived by physicians to the adoption of EMR while implementing policies and incentive programs for physicians. Secondly, both start-up and maintaining costs are crucial barriers that may particularly influence physicians practicing in small and rural settings or in private. Thus, the government should come up with definitive policies, which could improve their intention to adopt EMR. Thirdly, in addition to practical implications, the present study also contributed to previous literature and provide additional evidence that the most common barriers revolve around security and privacy concerns, cost issues, technical concerns, and ways to change medical practice. Fourthly, policymakers should consider ways how to lessen the disparities among physicians, especially in terms of financial rewards and the context of the working environment, which alternatively can improve physicians’ intention to adopt the EMR system.
Apart from the noteworthy results, the present review and analysis have some limitations. Firstly, even though we were extremely cautious in developing our search strategy, given that employing EMR adoption of the physician in the healthcare sector is a comprehensive area, we could not assure that we do not skip any significant outcomes. Secondly, the present study is exclusively based on a literature review. All the incorporated studies have had different objectives and employed different approaches and interpretations coming to their inferences that do not inevitably concord with the present study.
5. Conclusion
Despite the significant outcomes of using EMR in patients’ care, the adoption rate of EMR is still low. In the present study, based on a systematic literature review of 26 articles, the potential barriers behind the comparatively low adoption rate of EMR by physicians are being identified. Among these barriers, the top 5 barriers perceived by physicians to the adoption of EMR are privacy and security concerns, high start-up cost, workflow changes, system complexity, lack of reliability, and interoperability.
The results of the present review could be considered as a synopsis of barriers that physicians might potentially perceive in the EMR implementation process and, per se, could be significant for policymakers and healthcare providers. The review recommends that policymakers should be more responsive to the fact that eliminating technical barriers, such as system complexity, and financial barriers such as high start-up cost, and lack of incentive, is not enough to ensure the success of the potential implementation of EMR. The resistance to change is one of the basic characteristics of human behavior. Thus, the changes in the unique way of patient care developed by the physicians, due to the implementation of the EMR system also need to be addressed.
Furthermore, the implementation of the EMR system is a critical revolution that is perceived all through medical practice; it appeals to corresponding modifications and improvement in other aspects, for example, to the structure and approach of the patient. Thus, implementers should also consider a variety of other measures, such as lack of standard, uncertainty over vendors, implementation issues, etc, might also influence physicians’ intention to adopt the EMR system, and they should take corrective measures to eliminate these barriers too.
Author contributions
Bireswar Dutta: Prepare study design, Literature review, final draft, and conduct the Statistics. Hsin-Ginn Hwang: Check Literature review, and final draft.
Footnotes
Abbreviations: EHR = electronic health record, EMR = electronic medical record, HIS = health information system, ICT = information and communication technology, IT = information technology.
How to cite this article: Dutta B, Hwang HG. The adoption of electronic medical record by physicians: a PRISMA-compliant systematic review. Medicine. 2020;99:8(e19290).
The authors have no funding and conflicts of interest to disclose.
References
- [1].Or C, Tong E, Tan J, et al. Exploring factors affecting voluntary adoption of electronic medical records among physicians and clinical assistants of small or solo private general practice clinics. J Med Syst 2018;42:121. [DOI] [PubMed] [Google Scholar]
- [2].Gabriel MH, Jones EB, Samy L, et al. Progress and challenges: implementation and use of health information technology among critical-access hospitals. Health Affairs 2014;33:1262–70. [DOI] [PubMed] [Google Scholar]
- [3].Sockolow PS, Bowles KH, Adelsberger MC, et al. Challenges and facilitators to adoption of a point-of-care electronic health record in home care. Home Health Care Serv Q 2014;33:14–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kruse CS, Mileski M, Alaytsev V, et al. Adoption factors associated with electronic health record among long-term care facilities: a systematic review. BMJ Open 2015;5:e006615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Jawhari B, Keenan L, Zakus D, et al. Barriers and facilitators to electronic medical record (EMR) use in an urban slum. Int J Med Inform 2016;94:246–54. [DOI] [PubMed] [Google Scholar]
- [6].Al-Adwan AS. Exploring physicians’ behavioural intention toward the adoption of electronic health records: an empirical study from Jordan. Int J Healthcare Technol Manag 2015;15: [Google Scholar]
- [7].Yi M. Major issues in adoption of electronic health records. J Digital Inform Manag 2018;16: [Google Scholar]
- [8].Sines C, Griffin GR. Potential effects of the electronic health record on the small physician practice: a Delphi study. Perspect Health Inf Manag 2017;14:1f. [PMC free article] [PubMed] [Google Scholar]
- [9].Ariffin NAN, Ismail AK, Kadir IKA, et al. Implementation of electronic medical records in developing countries: challenges & barriers. Int J Acad Res Prog Educ Dev 2018;7:187–99. [Google Scholar]
- [10].AlJarullah A, Crowder R, Wald M, et al. Factors affecting the adoption of EHRs by primary healthcare physicians in the kingdom of Saudi Arabia: an integrated theoretical framework. Int J e-Healthcare Inform Syst 2018;5: [Google Scholar]
- [11].Hamamura FD, Withy K, Hughes K. Identifying barriers in the use of electronic health records in Hawai‘i. Hawai‘i J Med Public Health 2017;76: [PMC free article] [PubMed] [Google Scholar]
- [12].Alqahtani A, Crowder R, Wills G. Barriers to the adoption of EHR systems in the kingdom of Saudi Arabia: an exploratory study using a systematic literature review. J Health Infor Dev Count 2017;11: [Google Scholar]
- [13].Odekunle FF, Odekunle RO, Shankar S. Factors affecting electronic health record adoption in sub-Saharan Africa. Int J Health Sci 2017;11: [PMC free article] [PubMed] [Google Scholar]
- [14].Palabindala V, Pamarthy A, Jonnalagadda NR. Adoption of electronic health records and barriers. Journal of Community Hospital Internal Medicine Perspectives 2016;6:32643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Meigs SL, Solomon M. Electronic health record use a bitter pill for many physicians. Perspect Health Inf Manag 2016;13:1d. [PMC free article] [PubMed] [Google Scholar]
- [16].Kruse CS, Kothman K, Anerobi K, et al. Adoption factors of the electronic health record: a systematic review. JMIR Med Infor 2016;4:e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Kruse CS, Kristof C, Jones B, et al. Barriers to electronic health record adoption: a systematic literature review. J Med Syst 2016;40:252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Mahalli AAE. Electronic health records: use and barriers among physicians in eastern province of Saudi Arabia. Saudi J Health Sci 2015;4:32–41. [Google Scholar]
- [19].Jamoom E, Hing E. Progress with electronic health record adoption among emergency and outpatient departments: United States, 2006-2011. NCHS Data Brief 2015;187:1–8. [PubMed] [Google Scholar]
- [20].Liu CF, Cheng TJ. Exploring critical factors influencing physicians’ acceptance of mobile electronic medical records based on the dual-factor model: a validation in Taiwan. BMC Med Infor Decision Making 2015;15:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Adler-Milstein J, DesRoches CM, Furukawa MF, et al. More than half of US hospitals have at least a basic EHR, but stage 2 criteria remain challenging for most. Health Aff 2014;33:1664–71. [DOI] [PubMed] [Google Scholar]
- [22].Abramson EL, McGinnis S, Moore J, et al. HITEC investigators. A statewide assessment of electronic health record adoption and health information exchange among nursing homes. Health Serv Res 2014;49(Pt 2):361–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Abramson EL, Edwards A, Silver M, et al. HITEC investigators. Trending health information technology adoption among New York nursing homes. Am J Manag Care 2014;20:eSP53-9. [PubMed] [Google Scholar]
- [24].Menon S, Singh H, Meyer AN, et al. Electronic health record-related safety concerns: a cross sectional survey. J Healthc Risk Manag 2014;34:14–26. [DOI] [PubMed] [Google Scholar]
- [25].Raglan GB, Margolis B, Paulus RA, et al. Electronic health record adoption among obstetrician/gynecologists in the United States: physician practice and satisfaction. J Healthc Qual 2017;39:144–52. [DOI] [PubMed] [Google Scholar]
- [26].Ben-Zion R, Pliskin N, Fink L. Critical success factors for adoption of electronic health record systems: literature review and prescriptive analysis. Inform Syst Manag 2014;31:296–312. [Google Scholar]
- [27].Hwang HG, Dutta B, Chang HC. The differing effect of gender and clinical specialty on physicians’ intention to use electronic medical record. Methods Infor Med 2019;58:e58–71. [DOI] [PubMed] [Google Scholar]
- [28].Vishwanath A, Scamurra SD. Barriers to the adoption of electronic health records: using concept mapping to develop a comprehensive empirical model. Health Inform J 2007;13:119–34. [DOI] [PubMed] [Google Scholar]


