Abstract
To investigate whether the control of morning blood pressure (MBP) reflects the control of blood pressure (BP) in other periods (daytime, nighttime and 24-hour) and to assess whether morning BP displays a closer association with subclinical target organ damage (TOD) than the BP measured in other periods.
One thousand one hundred forty patients with primary hypertension who completed subclinical TOD detection and 24-hour ambulatory BP monitoring were included in the analysis. Pearson correlation analysis, Kappa consistency test, multiple linear regression analysis, and area under the receiver operating curve were used to analyze the data.
Morning BP and daytime BP displayed good agreement, but not 24-hour BP , particularly the nighttime BP (all P < .001). Approximately 39.4% of the hypertensive patients receiving drug treatment who had achieved control of the morning BP presented masked nocturnal hypertension, which was associated with worse subclinical TOD. The BP measured in all periods correlated with subclinical TOD, and the correlation was more obvious in the treatment subgroup. However, morning BP did not independently affect subclinical TOD. Morning BP appeared to exhibit less discriminatory power than nighttime BP, particularly with respect to the urinary albumin to creatinine ratio.
The use of morning BP for monitoring during hypertension management may not be enough. Masked uncontrolled nocturnal hypertension should be screened when morning BP is controlled.
Keywords: 24-hour ambulatory blood pressure monitoring, masked nocturnal hypertension, morning blood pressure, target organ damage
1. Introduction
Ischemic stroke and coronary events often occur in the early morning.[1–4] Blood pressure (BP) also usually increases in early morning during awakening hours.[5–6] This parallel phenomenon suggests that high BP in the morning may be particularly important for the occurrence of cardiovascular events. Recent studies have established this association.[7–8]
Morning BP is assessed using ambulatory BP monitoring (ABPM) and home BP monitoring. Morning hypertension is defined as morning BP ≥135/85 mm Hg for both ABPM and home BP monitoring, according to the expert recommendations on the management of morning hypertension published by the Council on Hypertension of the Chinese Society of Cardiology.[9] Morning hypertension is associated with a risk of cardiovascular events.[10] Morning BP may be a critical factor for the incidence of cardiovascular events and the management of hypertension. Recently, a consensus statement from an Asian expert panel on the management of morning hypertension was published.[11] Morning BP monitoring potentially represents a clinically relevant concept in the therapeutic management of hypertension and in the prevention of cardiovascular complications by defining and treating morning hypertension.
However, before establishing morning BP monitoring as a breakthrough in hypertension management, some questions remain to be answered. First, researchers must determine whether the control of morning BP reflects the control of BP in other periods (daytime, nighttime and 24-hour). Second, the findings describing the ability of BP measured in each period to predict subclinical target organ damage (TOD) are not consistent.[12–17] Compared with other periods, researchers have not yet clearly determined whether morning BP is more closely related to subclinical TOD. Therefore, the aim of our study is to answer these 2 questions.
2. Patients and methods
2.1. Study population
A cross-sectional study of hypertensive patients from the Outpatient and Inpatient Departments in West China Hospital of Sichuan University was conducted. All patients were recruited between January 2015 and December 2015. Patients who completed the subclinical TOD detection (including the urinary albumin/creatinine ratio (UACR), carotid intima-media thickness (IMT), and echocardiography) and ABPM were included. Participants were excluded from the analysis if any 1 of the following conditions existed:
-
(1)
Hypertensive urgency or emergency,
-
(2)
Confirmed secondary hypertension,
-
(3)
Hepatic or renal insufficiency (serum creatinine > 260 μmol/L or serum aspartate aminotransferase/alanine aminotransferase level > 2 times the upper limits of normal),
-
(4)
Malignant tumor,
-
(5)
A history of cerebrovascular or mental disease, and
-
(6)
Acute myocardial infarction or heart failure within 6 months. Finally, the data from 1140 patients were included in the analysis. The Medical Ethics Committee of West China Hospital affiliated with Sichuan University approved all of the procedures.
2.2. Data collection
As described in our previous surveys, the eligible subjects were asked to complete a questionnaire, including data on age, gender, alcohol consumption, cigarette smoking, and classes of antihypertensive medications prescribed.[18,19] The body mass index was calculated as the weight in kg/height in meters squared (kg/m2). Fasting blood glucose, total cholesterol (TC), low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglyceride (TG), uric acid, and creatinine levels and the UACR was tested in the Department of Laboratory Medicine in West China Hospital of Sichuan University.[20,21] A UACR≥30 mg/g was defined as microalbuminuria.
2.3. Carotid ultrasonography
The IMT was measured by an experienced sonographer using a Philips CX50 color Doppler ultrasound system, an L12 to 3 probe, and the QLab software (Phillips Medical Systems). An IMT > 0.9 mm was defined as carotid wall thickening.[22]
2.4. Transthoracic echocardiography
Transthoracic echocardiography was conducted by experienced operators who performed at least 1000 such procedures annually and who were blinded to the participants’ ABPM results. The measurement was conducted using the GE Vivid E9 color Doppler ultrasound detector with an M5S probe (GE Healthcare). The linear method with M-mode tracing was used to measure the end-diastolic interventricular septal wall thickness (IVS), left ventricular end-diastolic diameter (LVID), and end-diastolic posterior wall thickness (PWT). LAD was defined as the anteroposterior dimension of the left atrium, measured in the parasternal long-axis view. The left ventricular mass (LVM; in grams) was then calculated using the following formula: LVM = 0.8 × 1.04 × [(IVS + LVID+PWT)3 – LVID3] + 0.6. LVM index (LVMI) was calculated as LVM/body surface area. LVH was defined as an LVMI ≥125g/m2 for men and ≥110g/m2 for women.[23]
2.5. Twenty-four hour ABPM
Noninvasive ambulatory BP monitoring was performed with a SpaceLabs 90217 monitor (SpaceLabs Medical, Redmond, WA). The BP was measured every 20 minute during the daytime (06:00–22:00 hour) and every 30 minute during the night (22:00–06:00 hour). The measurement was only considered valid when > 75% of BP data were recorded. Daytime and nighttime BP were defined as the mean BP from 06:00 to 22:00 hour and 22:00 to 06:00 hour, respectively. Morning BP was defined as the mean BP measured 2 hour after waking. Morning hypertension was defined as a morning BP ≥ 135/85 mm Hg.[9,21] Hypertension was defined as the presence of at least 1 of the following conditions:
-
(1)
24-hour BP ≥130/80 mm Hg,
-
(2)
daytime BP ≥135/85 mm Hg,
-
(3)
nighttime BP ≥120/70 mm Hg, and
-
(4)
taking antihypertensive drugs.
The nocturnal BP dipping rate was calculated based on the systolic BP (SBP) as follows: (daytime SBP − nighttime SBP)/(daytime SBP) × 100%. Furthermore, the nocturnal dipping status was classified into 4 categories according to the dipping rate:
-
(1)
dipper (≥10% but < 20%),
-
(2)
nondipper (≥0% but < 10%),
-
(3)
extreme dipper (≥20%), and
-
(4)
reverse dipper (<0%).[24]
2.6. Statistical analysis
Categorical variables are presented as numbers and percentages (n, %). Continuous variables are presented as means ± standard deviations. Differences in baseline characteristics between 2 groups were analyzed using independent t tests for normally distributed variables, the nonparametric Mann-Whitney or Wilcoxon test for skewed variables, and the Chi-square test for categorical variables. Pearson correlation analysis was used to determine the correlation between the BP measured in each period and subclinical TOD. The cut off values for uncontrolled morning BP (MBP), diastolic BP, nighttime BP (NBP), and 24-hour BP were established according to the guideline. Kappa consistency was performed to assess the consistency of control rates between MBP and BP measured in other periods. A multivariate stepwise linear regression analysis was used to analyze the association between the BP measured in each period and subclinical TOD. Because subclinical TOD is mainly related to the SBP, the analysis used SBP as a dependent variable. Additionally, the discriminatory power of BP measured in each period for subclinical TOD was assessed from the area under the receiver operating curve (AROC). Integrated discrimination improvement (IDI) was used to quantify the added predictive ability of NSBP compared with MSBP. Statistical analyses were performed using SPSS 19.0 software (IBM, Armonk, NY). Statistical significance was defined as P < .05.
3. Result
3.1. Basic characteristics of the subjects
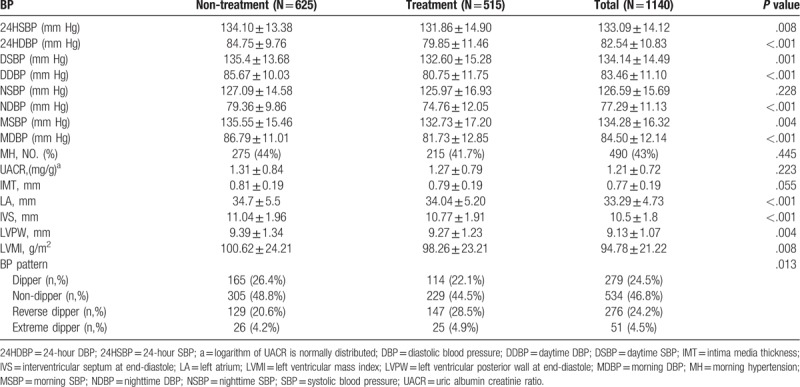
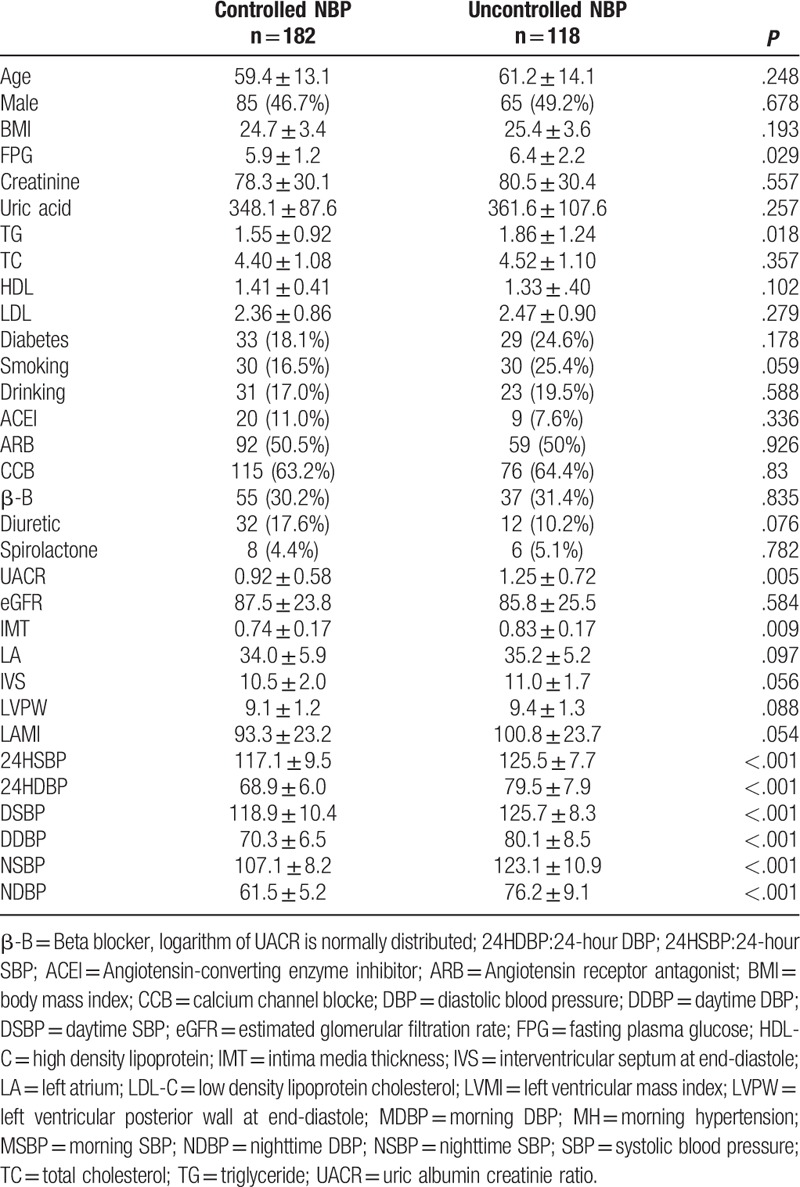
The general characteristics of the subjects are shown in Table 1. Overall, our sample had a mean age of 56.21 ± 14.25 years (1140 patients), 45.1% of patients were receiving antihypertensive medications (515 patients), 50.9% were male (580 patients), and 19.7% had diabetes mellitus (225 patients). Subjects treated with antihypertensive medications displayed a higher age, FPG level and creatinine level, but a lower estimated glomerular filtration rate TC level and TG level (all P < .05, Table 1). The non-treatment group shared higher MBP, daytime BP and 24-hour BP (all P < .05, Table 2), but not nighttime SBP and LVMI. The rates of morning hypertension in 2 groups were not significantly different (P = .445, Table 2).
Table 1.
Basic characteristics of subjects.
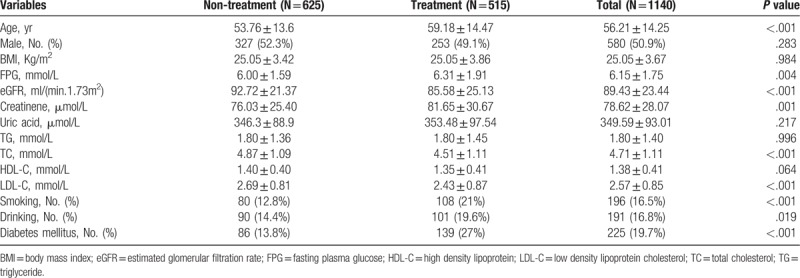
Table 2.
Ambulatory blood pressure monitoring and subclinical target organ damage in subjects.
3.2. Relationship between MBP and BP measured in other periods
Table 3 reveals the positive correlations between MBP with daytime, nighttime and 24-hour BP (all P < .01), and the correlation with nighttime BP was the weakest. The Kappa consistency analysis revealed that the rate of MBP control displayed good consistency with daytime BP, but poor consistency with NBP and 24-hour BP (Fig. 1). Particularly in the treatment group, among the patients with controlled MBP (<135/85 mm Hg, N = 300), approximately 23.7% of subjects did not achieve control of 24-hour BP, 9.7% did not achieve control of daytime BP and 39.4% did not achieve control of nighttime BP. These patients presented a higher IMT and UACR, as shown in Table 4.
Table 3.
Relationship between MBP and other periods’ BPs in subjects.
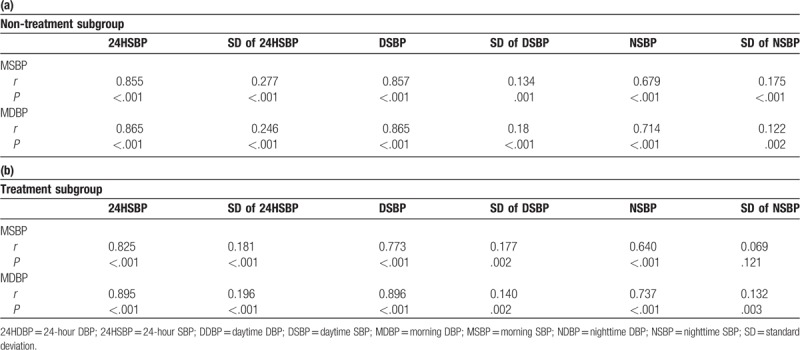
Figure 1.
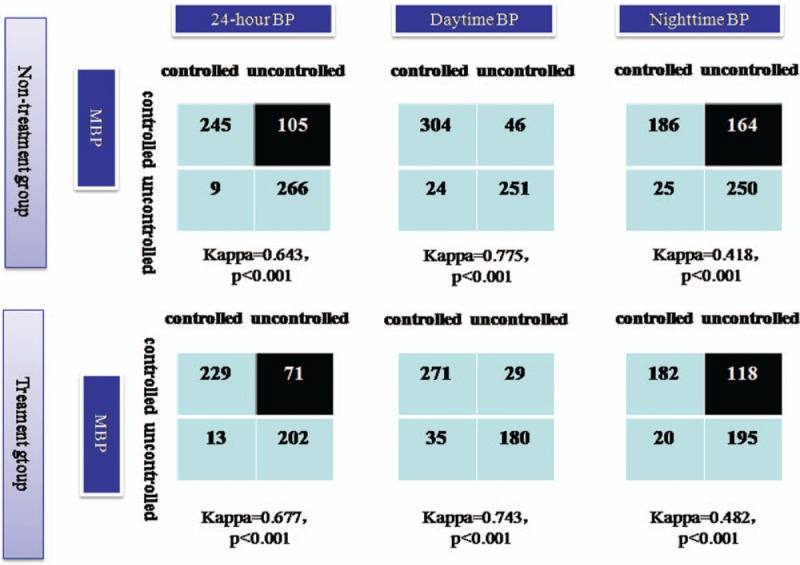
Consistency check of controlling rates between MBP and other periods’ BP. BP = blood pressure, MBP = morning blood pressure.
Table 4.
The influence of daytime and nighttime BP on TOD among treatment patients with controlled MBP.
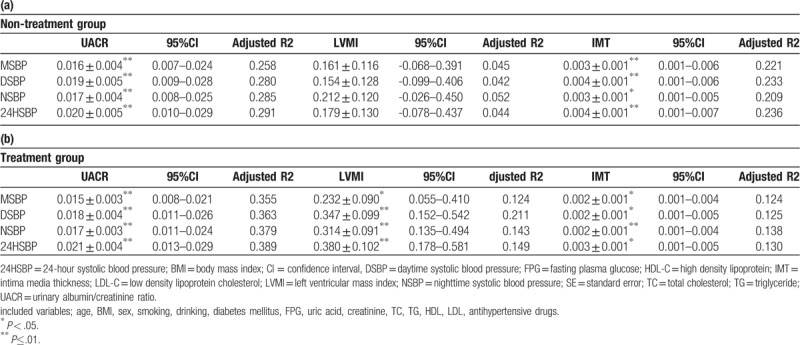
3.3. Relationship between MBP and subclinical TOD
Table 5 shows positive correlations between the BP measured in each period with UACR, IVS, LVPW and IMT, and BP measured in each period affected the UACR, LVMI and IMT in the linear regression after adjusting for covariates, except for LVMI in the nontreatment group (Table 6). After simultaneously inputting MBP and NBP into the regression equation, NBP affected the UACR (β=0.013, P = .052 for the non-treatment group; β=0.012, P = 0.012 for the treatment group) and LVMI in the treatment group (β=0.268, P = .019) and IMT in the treatment group (β=0.002, P = .050) independent of the MBP.
Table 5.
Pearson correlation analysis between each period's SBP and subclinical TOD in patients.
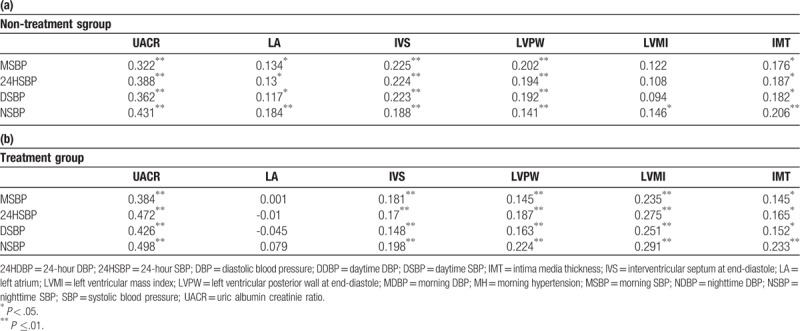
Table 6.
Multiple linear regression analysis between each period's BP and subclinical target organ damage in patients (β±SE).
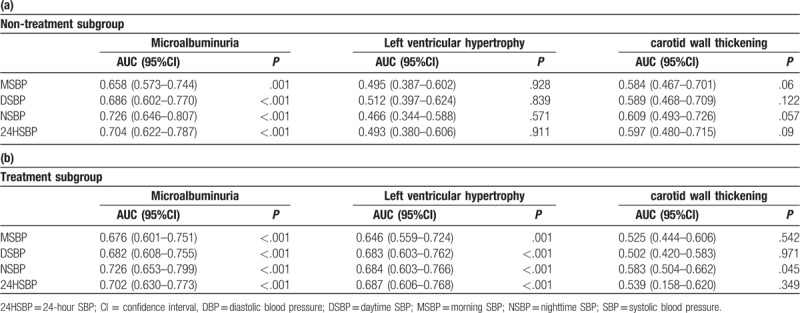
3.4. ROC curve analyses
In the treatment group, BP measured in all periods discriminated a UACR indicating damage and left ventricular hypertrophy. NBP and 24-hour BP had larger AROC values. However, they were unable to discriminate left ventricular hypertrophy or thickened IMT in the nontreatment subgroup. Only NBP discriminated a thickened IMT in the treatment subgroup (Table 7). The ability of NSBP to predict microalbuminuria in the nontreatment group was increased by 6% compared with MSBP (IDI = 0.06, P = .002). In the treatment group, the ability of NSBP to predict microalbuminuria and left ventricular hypertrophy increased by 4.7% (IDI = 0.047, P = .01) and 4.5% (IDI = 0.045, P = .003), respectively, compared with MSBP.
Table 7.
The area under ROC curve of each period's BP in discriminating TOD among patients.
4. Discussion
In the present study, patients with a controlled MBP did not display control of NBP and 24-hour BP. In the treatment group, approximately 39.4% hypertensive patients had masked uncontrolled nocturnal hypertension when MBP was controlled. The morning BP did not affect subclinical TOD independent of night time BP in the treatment group. MBP was less sensitive to predict early kidney damage and left ventricular hypertrophy than night time BP.
Similarly, Little P et al also reported a good correlation between HBPM and daytime BP measured using ABPM.[25] Although the study used HBPM, the recommended time period for measurement often coincides with the defined morning BP, and other researchers also found that MBP measured using HBPM or ABPM displayed good agreement.[26,27] On the other hand, MBP displayed poor agreement with NBP in the present study. Morning BP is related to the morning surge and NBP.[28] Approximately 12.4% of patients had isolated nocturnal hypertension in our survey. These data explain our findings. More importantly, a higher percentage than Japan morning surge home blood pressure (J-HOP) study,[29] nearly 40% patients had masked uncontrolled nocturnal hypertension while whose MBP were controlled in our study, and these patients had a higher IMT and UACR. This result reflected a terrible fact that masked nocturnal hypertension remains unrecognized by conventional HBPM. The use of morning BP monitoring as a breakthrough in hypertension management in addition to stressing the control of early morning BP has great clinical significance to identify masked nocturnal hypertension.
BP measured in all periods correlated with subclinical TOD, and more obvious correlations were observed in the treatment subgroup in the present study. However, MBP did not independently affect subclinical TOD indicators. MSBP appeared to display less power in discriminating subclinical TOD than NSBP, particularly the UACR. Although the UACR is an indicator of early renal damage, the kidney is an organ with a high level of perfusion, and damage to the renal afferent arteriole and efferent arteriole exerts an important effect on the UACR,[30] suggesting that nighttime BP may directly reflect blood vessel-related TOD. The findings were inconsistent with the results reported in some studies.[15,16,31,32] We believe that a crucial explanation for the difference is the BP measurement method. These previous studies used HBPM. Nighttime BP was measured 2 hours before subjects fell asleep. Obviously, this measurement would not objectively reflect virtual BP during sleep.[33,34] The J-HOP study reported a sleeping BP (measured 3 times during sleep at 2 am , 3 am , 4 am) measured using a new home BP monitoring device that was approximately 10 mm Hg lower than BP measured 2 hours before the subject fell asleep and acquired a similar result that the associations of home sleep SBP with UACR remained significant after controlling for clinical SBP and home monitored morning SBP.[28] Furthermore, Andreadis EA et al verified that the sleeping BP measured using this new HBPM equipment displayed good consistency with nighttime BP measured using ABPM.[35] These results confirm the reliability of our findings and highlight the importance of monitoring nighttime BP.
Some limitations of this study should be acknowledged. The first was the cross-sectional design that did not allow us to determine whether morning BP predicts cardiovascular events independently of BP measured in other periods. The second was that we do not have data on HBPM, and thus the true difference between bedtime blood pressure and nighttime BP in our sample was unknown.
In summary, the use of MBP as a monitoring target during hypertension management may not be enough. The recognition of masked, uncontrolled NBP has important clinical significance.
Author contributions
Data curation: Kai Liu, Ying Xu, Shenzhen Gong, Jiangbo Li.
Funding acquisition: Xiaoping Chen.
Investigation: Kai Liu, Ying Xu, Shenzhen Gong, Xinran Li, Runyu Ye, Hang Liao.
Project administration: Xiaoping Chen.
Resources: Xiaoping Chen.
Software: Kai Liu, Ying Xu, Jiangbo Li.
Supervision: Xiaoping Chen.
Validation: Xiaoping Chen.
Writing – original draft: Kai Liu, Ying Xu.
Writing – review and editing: Kai Liu, Ying Xu.
Footnotes
Abbreviations: ABPM = ambulatory blood pressure monitoring, AROC = area under the receiver operating curve, BP = blood pressure, IMT = intima-media thickness, IVS = interventricular septal, LVM = left ventricular mass, LVMI = left ventricular mass index, MBP = morning blood pressure, NBP = nighttime blood pressure, PWT = posterior wall thickness, TC = total cholesterol, TG = triglyceride, TOD = target organ damage, UACR = urinary albumin/creatinine ratio.
How to cite this article: Liu K, Xu Y, Gong S, Li J, Li X, Ye R, Liao H, Chen X. The disadvantage of morning blood pressure management in hypertensive patients. Medicine. 2020;99:8(e19278).
KL and YX contributed equally to this work and should be considered co-first authors.
This study was supported by Science and Technology Pillar Program in Sichuan Province, China (grant no:17ZDYF3050) and Resident Research Fund in West China Hospital (grant no:YB0000005).
The datasets generated and analyzed during the current study are not publicly available because the data are also part of an ongoing study, but are available from the corresponding author upon reasonable request.
Funding Sources: This study was supported by grants from the Science & Technology Pillar Program in Sichuan Province, China (grant no: 17ZDYF3050) and Resident Research Fund in West China Hospital (grant no: YB0000005).
The authors have no conflicts of interest to disclose.
References
- [1].Muller JE, Stone PH, Turi ZG, et al. Circadian variation in the frequency of onset of acute myocardial infarction. N Engl J Med 1985;313:1315–22. [DOI] [PubMed] [Google Scholar]
- [2].Muller JE, Ludmer PL, Willich SN, et al. Circadian variation in the frequency of sudden cardiac death. Circulation 1987;75:131–8. [DOI] [PubMed] [Google Scholar]
- [3].Argentino C, Toni D, Rasure M, et al. Circadian variation in the frequency of ischemic stroke. Stroke 1990;21:387–9. [DOI] [PubMed] [Google Scholar]
- [4].Willich SN, Levy D, Rocco MB, et al. Circadian variation in the Framingham heart study population. Am J Cardio 1987;60:801–6. [DOI] [PubMed] [Google Scholar]
- [5].Mancia G, Verdecchia P. Clinical value of ambulatory blood pressure: evidence and limits. Circ Res 2015;116:1034–45. [DOI] [PubMed] [Google Scholar]
- [6].Weber MA, Drayer JI, Nakamura DK, et al. The Circadian blood pressure pattern in ambulatory normal subjects. Am J Cardiol 1984;54:115–9. [DOI] [PubMed] [Google Scholar]
- [7].Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation 2003;107:1401–6. [DOI] [PubMed] [Google Scholar]
- [8].Li Y, Thijs L, Hansen TW, et al. International database on ambulatory blood pressure monitoring in relation to cardiovascular outcomes investigators. Prognostic value of the morning blood pressuresurge in 5645 subjects from 8 populations. Hypertension 2010;55:1040–8. [DOI] [PubMed] [Google Scholar]
- [9].Council on Hypertension of the Chinese Society of Cardiology. Chinese expert consensus on early morning blood pressure. Chin J Cardiol 2014;42:721–5. [PubMed] [Google Scholar]
- [10].Kario K, Saito I, Kushiro T, et al. Morning home blood pressure is astrong predictor of coronary artery disease: the HONEST study. J AmColl Cardiol 2016;67:1519–27. [DOI] [PubMed] [Google Scholar]
- [11].Wang JG, Kario K, Chen CH, et al. Management of morning hypertension: a consensus statement of an Asian expert panel. J Clin Hypertens (Greenwich) 2018;20:39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Mulè G, Caimi G, Cottone S, et al. Value of home blood pressures as predictor of target organ damage in mild arterial hypertension. J Cardiovasc Risk 2002;9:123–9. [DOI] [PubMed] [Google Scholar]
- [13].Cuspidi C, Michev I, Meani S, et al. Left ventricular hypertrophy in treated hypertensive patients with good blood pressure control outside the clinic, but poor clinic blood pressure control. J Hypertens 2003;21:1575–81. [DOI] [PubMed] [Google Scholar]
- [14].Martínez MA, Sancho T, García P, et al. Home blood pressure in poorly controlled hypertension: relationship with ambulatory blood pressure and organ damage. Blood Press Monit 2006;11:207–13. [DOI] [PubMed] [Google Scholar]
- [15].Bliziotis IA, Destounis A, Stergiou GS, et al. ambulatory and office blood pressure in predicting target organ damage in hypertension: a systematic review and meta-analysis. J Hypertens 2012;30:1289–99. [DOI] [PubMed] [Google Scholar]
- [16].Stergiou GS, Argyraki KK, Moyssakis I, et al. Home blood pressure is as reliable as ambulatory blood pressure in predicting target-organ damage in hypertension. Am J Hypertens 2007;20:616–21. [DOI] [PubMed] [Google Scholar]
- [17].Oliveras A, Armario P, Martell-Clarós N, et al. Spanish society of hypertension-resistant hypertension registry. Urinary albumin excretion is associated with nocturnal systolic blood pressure in resistant hypertensives. Hypertension 2011;57:556–60. [DOI] [PubMed] [Google Scholar]
- [18].He S, Zheng Y, Wang H, et al. Assessing the relationship between a body shape index and mortality in a group of middle-aged men. Clin Nutr 2017;36:1355–9. [DOI] [PubMed] [Google Scholar]
- [19].Liu K, Wang Y, He J, et al. Is pulse pressure a predictor of diabetes in Chinese Han nationality population? 15-year prospective study in Chengdu community. Int J Cardiol 2014;176:529–32. [DOI] [PubMed] [Google Scholar]
- [20].Liu K, Wang S, Wan S, et al. Arterial stiffness, central pulsatile hemodynamic load, and orthostatic hypotension. J Clin Hypertens (Greenwich) 2016;18:655–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Li X, Li J, Liu K, et al. Association between sleep disorders and morning blood pressure in hypertensive patients. Clin Exp Hypertens 2018;40:337–43. [DOI] [PubMed] [Google Scholar]
- [22].Gong S, Liu K, Ye R, et al. Nocturnal dipping status and the association of morning blood pressure surge with subclinical target organ damage in untreated hypertensives. J Clin Hypertens (Greenwich) 2019;21:1286–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Wu QS, He Q, He JQ, et al. The role of mitofilin in left ventricular hypertrophy in hemodialysis patients. Ren Fail 2018;40:252–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Williams B, Mancia G, Spiering W, et al. 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC task force for the management of arterial hypertension. J Hypertens 2018;36:2284–309. [DOI] [PubMed] [Google Scholar]
- [25].Little P, Barnett J, Barnsley L, et al. Comparison of agreement between different measures of blood pressure in primary care and daytime ambulatory blood pressure. BMJ 2002;325:254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Parati G, Stergiou GS, Asmar R, et al. European society of hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens 2010;24:779–85. [DOI] [PubMed] [Google Scholar]
- [27].Stergiou GS, Nasothimiou EG, Roussias LG. Morning hypertension assessed by home or ambulatory monitoring: different aspects of the same phenomenon? J Hypertens 2010;28:1846–53. [DOI] [PubMed] [Google Scholar]
- [28].Kario K, White WB. Early morning hypertension: what does it contribute to overall cardiovascular risk assessment? J Am Soc Hypertens 2008;2:397–402. [DOI] [PubMed] [Google Scholar]
- [29].Kario K, Hoshide S, Haimoto H, et al. Sleep blood pressure self-measured at home as a novel determinant of organ damage: Japan morning surge home blood pressure (J-HOP) study. J Clin Hypertens (Greenwich) 2015;17:340–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hashimoto J, Ito S. Central pulse pressure and aortic stiffness determine renal hemodynamics: pathophysiological implication for microalbuminuria in hypertension. Hypertension 2011;58:839–46. [DOI] [PubMed] [Google Scholar]
- [31].Hoshide S, Kario K, Yano Y, et al. Association of morning and evening blood pressure at home with asymptomatic organ damage in the J-HOP Study. Am J Hypertens 2014;27:939–47. [DOI] [PubMed] [Google Scholar]
- [32].Eguchi K, Matsui Y, Shibasaki S, et al. Controlling evening BP as well as morning BP is important in hypertensive patients with prediabetes/diabetes: the JMS-1 study. Am J Hypertens 2010;23:522–7. [DOI] [PubMed] [Google Scholar]
- [33].Bloomfield D, Park A. Night time blood pressure dip. World J Cardiol 2015;7:373–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Pickering TG, Harshfield GA, Kleinert HD, et al. Blood pressure during normal daily activities, sleep, and exercise. Comparison of values in normal and hypertensive subjects. JAMA 1982;247:992–6. [PubMed] [Google Scholar]
- [35].Andreadis EA, Agaliotis G, Kollias A, et al. Night-time home versus ambulatory blood pressure in determining target organ damage. J Hypertens 2016;34:438–44. [DOI] [PubMed] [Google Scholar]


