Abstract
The effects of exercise interventions on blood pressure control in hypertensive patients have received extensive attention and recognition. However, the influence of exercise-related behaviors on the effects of blood pressure control and the management factors that affect exercise behaviors remain inconclusive. Therefore, this study aimed to explore the relationships between exercise and exercise-related behaviors and blood pressure control, expecting to provide a scientific basis for further improvement of exercise intervention programs for patients with hypertension.
Long-term residents in a community in Fuzhou, Fujian Province, China who were diagnosed with hypertension at a medical facility were recruited for this study. Hypertensive patients with uncontrolled blood pressure were placed in the case group, and those with controlled blood pressure were placed in the control group. The count data were analyzed with the χ2 test based on α = 0.05. A univariate logistic regression analysis was performed to screen significant variables; independent variables were selected based on professional knowledge and were tested for co-linearity. These variables were incorporated into a non-conditional multivariate logistic regression analysis to analyze relevant factors for blood pressure control, while calculating odds ratio (ORs), 95% confidence intervals (CIs), and P values. Differences with a P < .05 were considered statistically significant.
A total of 598 patients were included in the present study. Univariate and multivariate analyses showed that exercise (OR = 0.194; 95%CI: 0.133–0.283), frequency of self-monitoring of blood pressure (OR = 2.412; 95%CI: 1.137–5.117), and regular housework (OR = 0.397, 95%CI: 0.248–0.633) were statistically significant factors for blood pressure control. In addition, there was a relationship between exercise-related behaviors and blood pressure control: walking (OR = 0.189, 95% CI: 0.065–0.551), 60 to 120 min/day of exercise time (OR = 0.317, 95% CI: 0.118–0.856). Sex (OR = 2.248, 95% CI: 1.279–3.954), health belief (OR = 0.016, 95% CI: 0.004–0.059), and company of a family member during exercise (OR = 0.048, 95% CI: 0.025–0.094) were significant factors predictive of regular exercise in hypertensive patients.
Improving exercise-related behaviors and their management can help improve the effects of exercise interventions on blood pressure control in middle-aged and elderly hypertensive patients.
Keywords: blood pressure control, exercise, exercise-related behaviors, hypertension
1. Introduction
Hypertension is an important risk factor for cardiovascular and cerebrovascular diseases and mortality.[1] Currently, there are ∼1.5 billion hypertensive patients globally. According to the data released in 2015, the prevalence of hypertension in Chinese adults was 25.2% in 2012.[2] However, one study found that the rate of blood pressure control in hypertensive patients was only 8.2% (BP well controlled at goal) in 115 Chinese communities.[3] Blood pressure control in patients with high blood pressure faces significant challenges.
Unhealthy lifestyle is one of the most important risk factors for hypertension, especially for essential hypertension. So maintaining a healthy lifestyle and other non-drug therapies play an important role in disease prevention and control. A healthy lifestyle and behavior mainly include psychological balance, reasonable diet, moderate exercise, weight control, and smoking cessation limit. Among these factors, the relationship between exercise and hypertension control has been an area of wide concern. Many studies have shown that strengthening exercises and physical activity can help reduce blood pressure in patients with hypertension.[4,5] However, the influence of exercise-related behaviors on the effects of blood pressure control and the management factors that affect exercise behaviors remain inconclusive.
The research questions of the study were: What is the effect of exercise and exercise-related behaviors on blood pressure control? And what factors affect the exercise behaviors of hypertensive patients? This study is expected to provide a scientific basis for further improvement of exercise intervention programs for patients with hypertension.
2. Methods
2.1. Patients and public involvement
Long-term residents in a community in Fuzhou, Fujian Province (continuously or cumulatively residing in the community for 6 months or more in the past year) who were diagnosed with hypertension at a medical facility were recruited for the present study. Patients with incorrect or incomplete medical records, those missing contact information, or those with incorrect phone numbers were excluded. Ultimately, 1942 patients were eligible in accordance with the community standard management practice. This research was approved by the Ethics Review Group of the Fujian Provincial Key Laboratory of Environment and health.
2.2. Number of participants and sampling method
This was a non-matched case–control study in which equivalent numbers of participants were enrolled in the case group and the control group. The sample size was calculated at α = 0.05 (two-sided) and β = 0.10, with exercise as a representative protective factor (OR = 0.87, the exercise rate was 68.49%[6] among the patients with controlled blood pressure). The results showed that the required sample size was 261 for each group, given a 20% non-response rate, 314 participants should be included in each group. We extracted the corresponding samples by using the Systematic sampling method (also called Isometric sampling method or Mechanical sampling method) that we used the patients’ health file numbers as the serial numbers. 1 person was selected every interval in the case group as the study object and 1 person in the control group at intervals. With the informed consent of the patients, 288 patients were included in the case group and 310 were included in the control group
2.3. Standard of diagnosis and control of hypertension
The criteria for hypertension were SBP ≥140 mm Hg and (or) DBP ≥90 mm Hg. The control criteria for hypertension were as follows: controlled blood pressure was defined as two consecutive blood pressure values, including the latest blood pressure and blood pressure test within 6 months, both SBP < 140 mm Hg and DBP < 90 mm Hg; in people over 65 years included SBP < 150 mm Hg and DBP < 90 mm Hg; uncontrolled blood pressure was defined as two consecutive blood pressure values (same as before) above 140 and (or) 90 mm Hg; in people over 65 years included values above 150 and (or) 90 mm Hg.[7]
2.4. Inclusion and exclusion criteria
Inclusion criteria: patients who were diagnosed with essential hypertension at a medical facility at least 1 year ago.
Exclusion criteria: cognitive impairment, inability to cooperate during the survey, or incomplete tests or data.
2.5. Data collection and quality assurance
According to Sports Proposal in “China Hypertension Prevention Guide (2010 Edition),”[7] a self-designed questionnaire was used to survey the patients. The questions were asked by unified investigators who were chronic disease researchers and had received knowledge about hypertension. The survey assessed social demographic characteristics, blood pressure control and exercise-related behaviors. The blood pressure and BMI values in this study were based on the historical data of the patients in the community health records and data from a recent physical examination; these values were confirmed by asking the patients. After completion of the questionnaire design, a small sample survey was conducted, and the content was further perfected to create a formal questionnaire. To ensure the quality of the investigation and data, we filled in gaps in telephone interviews and visits with other forms.
2.6. Variable definitions
Exercise: this referred to various forms of regular exercise (at least once per week, more than 20 min each time, for at least 2 months) for the purpose of exercising and improving the body's physical condition.
Exercise-related behaviors: behaviors directly related to exercise, defined as the frequency, time, and duration of regular exercise.
Overweight/obesity: underweight was defined as BMI < 18.5 kg/m2; normal weight as 18.5 kg/m2 ≤ BMI < 24 kg/m2; overweight as 24 kg/m2 ≤ BMI < 28 kg/m2; and obesity as BMI ≥ 28 kg/m2.[8]
Hypertension-related complications: in this paper, these included cerebrovascular diseases (such as ischemic stroke and cerebral hemorrhage), heart diseases (such as myocardial infarction and angina), and kidney diseases (such as hypertensive nephropathy and renal failure).
Guidance for personalized exercise: the patient received personalized exercise guidance from a healthcare professional in the past year.
Company during exercise: the patient engaged in regular exercise accompanied by his/her parents, spouse, or children living with the patient.
Doing housework on a regular basis: the patient did housework at least three times per week (laundry, cleaning, gardening, housekeeping) for >20 min each time.
Participation in health education workshops: the patient regularly participated in community health education activities, where health education involved information about health and exercise.
Health belief: The public belief that awareness (e.g., fear) of the predisposition and severity of a disease was associated with behaviors to prevent the disease; this belief affected public perception of the threat and subsequently the possibility to take preventative actions. In this paper, health belief referred to patient awareness that a lack of exercise had an adverse effect on blood pressure control, with serious consequences, which supported and promoted regular exercise.
Smoking: it referred to smoking ≥1 cigarette/day for 6 months or more.
Drinking: it referred to drinking one or more alcoholic beverages per week (average) for 6 months or more.
2.7. Data analysis
Epidata3.1 was used to establish a database, and the data were double entered. SPSS v17.0 was used for the statistical analysis. The count data were analyzed with the χ2 test based on α = 0.05. A univariate logistic regression analysis was performed to screen significant variables; independent variables were selected based on professional knowledge and were tested for co-linearity. These variables were incorporated into a non-conditional multivariate logistic regression analysis to analyze relevant factors for blood pressure control, while calculating ORs, 95%CIs, and P values. Differences with a P < .05 were considered statistically significant.
3. Results
3.1. Analysis of relevant factors for blood pressure control outcomes in hypertensive patients
In the present study, 628 questionnaires were sent out, with 30 recipients exiting the study early (did not complete the survey) or not answering all the questions on the survey. In total, the response rate of this study was 95.2%, of which 288 patients with uncontrolled blood pressure were assigned to the case group and 310 with controlled blood pressure were included in the control group. Moreover, social demographic characteristics analysis of the two groups showed that no significant between-group differences were observed in age, sex, residence type, marital status, education level, or occupation (P > .05).
3.1.1. Univariate analysis of relevant factors for blood pressure control outcomes in hypertensive patients
Blood pressure control outcome was used as the dependent variable, and 11 variables (Including BMI, course of disease, family history, hypertension-related complications, hypertension combined with diabetes, the frequency of self-monitoring of blood pressure, medication compliance, smoking, drinking, exercise, doing housework on a regular basis) were used as independent variables for the χ2 test and the subsequent individual univariate logistic regression analysis. The results showed that after controlling for age and sex, variables of the frequency of self-monitoring of blood pressure, exercise, and regular housework were statistically significant factors for blood pressure control (P < .05); the remaining variables were unrelated to blood pressure control (P > .05).
3.1.2. Multivariate analysis of relevant factors for blood pressure control outcomes in hypertensive patients
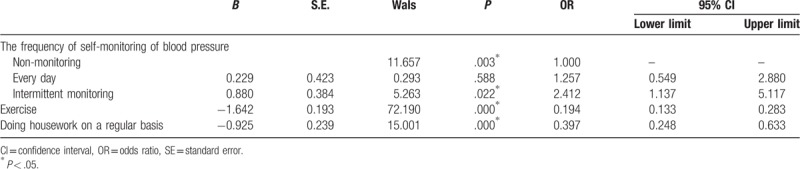
Significant factors identified in the univariate analysis and well-known factors were incorporated into a multivariate logistic regression analysis. A co-linearity analysis showed a VIF <5 and no co-linearity among the independent variables (Table 1). The multivariate logistic analysis showed that the frequency of self-monitoring of blood pressure, exercise, and regular housework were independent factors for blood pressure control in hypertensive patients. The risk of adverse blood pressure control was 0.194-fold lower in patients who exercised regularly than in those who did not (95% CI: 0.133–0.283) and was 0.397-fold lower in patients who did housework regularly than in those who did not (95% CI: 0.248–0.633). Intermittent monitoring of blood pressure was a risk factor for adverse blood pressure control (OR = 2.412, 95% CI: 1.137–5.117) (P < .05) (Table 2).
Table 1.
Co-linearity analysis of factors that influence blood pressure control in patients with hypertension.
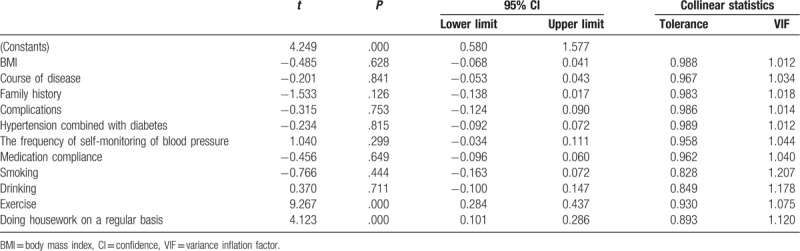
Table 2.
Multifactor logistic analysis of the effect of blood pressure control in patients with hypertension.
3.2. Analysis of the relationship between exercise-related behaviors and blood pressure control outcomes in hypertensive patients
The above analysis showed that exercise was a protective factor for blood pressure control in hypertensive patients. We further analyzed the effects of exercise-related behaviors on blood pressure control. Among the 598 hypertensive patients in the present study, 343 (57.4%) exercised regularly. We then analyzed the effects of the frequency, and time of exercise on blood pressure control in these 343 patients. In the case group, 107 patients (37.2%) exercised regularly, whereas in the control group, 236 (76.1%) exercised regularly. No significant between-group differences were observed in socio-demographic features (including sex, age, household type, marital status, degree of education, occupation type) in these 343 patients (P > .05).
3.2.1. Univariate analysis of the effects of exercise-related behaviors on blood pressure control
For the hypertensive patients who exercised regularly, blood pressure control outcome was used as the dependent variable, and 3 variables related to exercise-related behaviors (frequency of exercise, time spent on exercising, duration of regular exercise) were used as the independent variables for the χ2 test and the subsequent individual univariate logistic regression analysis. The results showed that the time, frequency, and duration of exercise were significant factors for blood pressure control (P < .05). Moreover, our study found that because most people (88.05%) chose walking as their form of exercise, the sample size of other exercise forms (resistance campaigns, Chinese traditional sports, ball games, swimming, aerobics/square dance, running) was too small to be analyzed.
3.2.2. Multivariate analysis of the effects of exercise-related behaviors on blood pressure control
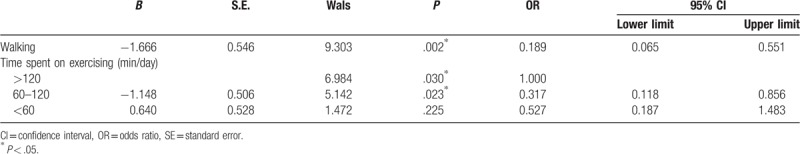
Significant factors identified via the univariate analysis and well-known factors were incorporated into the multivariate logistic regression analysis. A co-linearity analysis showed a VIF <5 and no co-linearity among the independent variables (Table 3). The multivariate logistic analysis showed that walking and 60 to 120 min/day of exercise time had significant effects on blood pressure control (P < .05). Regular walking was correlated with better blood pressure control (OR = 0.189, 95% CI: 0.065–0.551); 60 to 120 min/day of exercise time was more effective for blood pressure control than >120 min/day (OR = 0.317, 95% CI: 0.118–0.856) (Table 4).
Table 3.
Co-linearity analysis of blood pressure control by exercise-related behaviors.
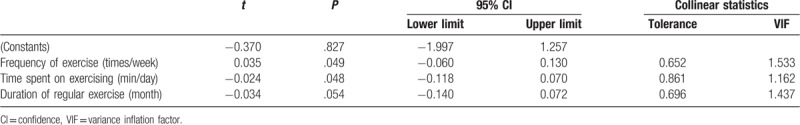
Table 4.
Multivariate logistic analysis of exercise-related behaviors for blood pressure control.
3.3. Analysis of relevant factors for regular exercise in hypertensive patients
3.3.1. Univariate analysis of relevant factors for regular exercise in hypertensive patients
Among the 598 hypertensive patients, 343 exercised regularly and 255 did not. We investigated relevant factors for regular exercise in hypertensive patients. The univariate analysis of 10 potential variables (including sex, age, course of disease, BMI, hypertension combined with diabetes, complications, participation in health education workshops, health belief, company during exercise, guidance for personalized exercise) revealed that sex, participation in health education workshops, health beliefs, company of a family member during exercise, and personalized exercise guidance were significant factors for regular exercise in hypertensive patients (P < .05)
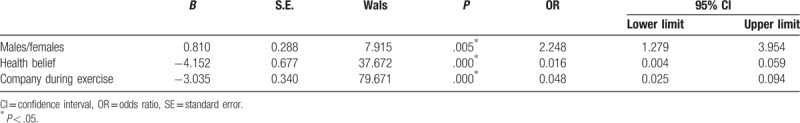
3.3.2. Multivariate analysis of relevant factors for regular exercise in hypertensive patients
Significant factors identified via the univariate analysis and known factors were incorporated into the multivariate logistic regression analysis. The co-linearity analysis showed a VIF <5 and no co-linearity among the independent variables (Table 5). The multivariate logistic analysis showed that sex, health belief, and company of a family member during exercise had significant effects on blood pressure control (P < .05). Women were 2.248 times more likely than men to not engage in regular exercise; company of a family member during exercise was correlated with regular exercise (OR = 0.048, 95% CI: 0.025–0.094); and patients with health beliefs were more likely to engage in regular exercise (OR = 0.016, 95% CI: 0.004–0.059) (Table 6).
Table 5.
Co-linearity analysis of factors that influence regular exercise in hypertensive patients.
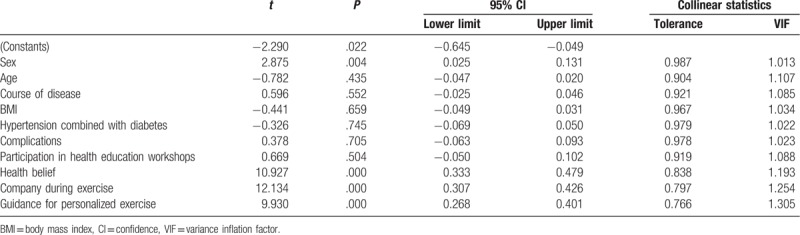
Table 6.
Multifactor logistic analysis of variables affecting regular exercise in hypertensive patients.
4. Discussion
This study investigated the effects of exercise and exercise-related behaviors on blood pressure control in hypertensive patients. The univariate logistic analysis showed that the frequency of blood pressure self-monitoring, exercise, regular housework, and certain exercise-related behaviors (time, frequency, duration of exercise) were correlated with blood pressure control. The multivariate logistic analysis showed that the frequency of blood pressure self-monitoring, and regular housework were correlated with blood pressure control. Moreover, the multivariate logistic analysis showed that exercise and exercise-related behaviors (walking, 60–120 min/day of exercise time) were primary factors for blood pressure control in hypertensive patients.
Regular exercise had a positive effect on blood pressure control. However, this effect was influenced by many factors. We investigated the potential factors for regular exercise in hypertensive patients. The univariate analysis showed that sex, health education workshops, health beliefs, company of a family member during exercise, and personalized exercise guidance were factors affecting regular exercise in these patients. The multivariate logistic analysis showed that female sex, company of a family member during exercise, and health beliefs were the primary factors for regular exercise in these patients.
Some studies have shown that daily activities such as commuting and housework can help prevent cardiovascular and cerebrovascular diseases and improve blood pressure control.[9,10] Uhlig et al[11] conducted a meta-analysis and showed that self-monitoring of blood pressure was associated with better blood pressure control in hypertensive patients. The present study first analyzed the relationships between common relevant factors and blood pressure control in hypertensive patients. The multivariate analysis showed that the frequency of self-monitoring of blood pressure, and regular housework were closely associated with blood pressure control. Intermittent monitoring of blood pressure had an adverse effect on blood pressure control. Some studies showed that family history and BMI were associated with the morbidity of hypertension. Lee et al[12] found that each 1 kg/m2 increase in BMI was associated with a 19% increase in hypertension risk. However, the present study found no correlations between family history, BMI, comorbidities, complications, smoking, or drinking and blood pressure in people who had been diagnosed with hypertension. Moreover, studies on the intervention effects of exercise on blood pressure control in hypertensive patients have been conducted in many countries. Sadja et al[13] showed that a 12-week exercise programme had a positive effect on blood pressure control, and Zhang et al[14] performed a meta-analysis and showed that exercise intervention had a certain effect on the reduction of the SBP and DBP in hypertensive patients, which is consistent with the findings of this study.
Studies on exercise-related behaviors have focused on the relationship between the form of exercise and blood pressure control in hypertensive patients. For example, Cornelissen and Smart[15] conducted a meta-analysis and showed that endurance, dynamic resistance and isometric resistance training lower SBP and DBP. Cornelissen et al[16] and Rossi et al[17] supported the blood pressure-lowering potential of resistance training. Few studies have reported the relationships between exercise-related behaviors (time, frequency, and duration of exercise) and blood pressure control. Ishikawa-Takata et al[18] showed no correlation between more frequent exercise and blood pressure control. Currently, researchers are still debating whether more frequent exercise enables better blood pressure control. The present study systematically analyzed exercise-related behaviors in hypertensive patients and showed that walking and exercise time were the primary factors for blood pressure control in hypertensive patients. Moreover, this study showed a correlation between exercise time (preferably 60–120 min/day) and blood pressure control. The present study showed that the frequency of exercise and the duration of exercise were not independent factors for blood pressure control, indicating that relations between the frequency of exercise, or the duration of exercise and blood pressure control could not be determined, though the time, frequency, duration of exercise were correlated with blood pressure control according to the univariate logistic analysis.
Relevant data on factors affecting regular exercise are still lacking. This study focused on potential factors for regular exercise in hypertensive patients and showed that sex, company of a family member during exercise, and health beliefs were primary factors for regular exercise in hypertensive patients. The present study showed that women were more likely not to engage in regular exercise. There may be a lot of reasons for this. One of the possibilities was in China most middle-aged and elderly women had to spend most of the time doing the housework and making them unable to engage in additional exercise. Moreover, women were less likely to continue to exercise, thus requiring additional attention during health education. This study showed that family support improved the exercise participation rate of hypertensive patients, indicating that a healthy family environment, including the family structure, relationships among family members, economic level, education level, and lifestyle, was vital to patients because family support could encourage and motivate the patient to engage in regular exercise. One study found that family-of-origin attitudes about food and exercise were related to current lifestyle choices in interracial and same-race couples. It showed that family of origin played a role in current lifestyle choices.[19] Therefore, health education and promotion among key family members can affect all family members. Moreover, the patients who attached great importance to blood pressure control were more likely to engage in regular exercise, likely because once patients perceived the threat of lack of exercise on blood pressure control and the serious consequences, they were more likely to take preventive measures.
Many studies have investigated the intervention effects of exercise on blood pressure control in hypertensive patients; however, data on the effects of exercise-related behaviors on blood pressure control and relevant factors for regular exercise in hypertensive patients are lacking, and few systematic studies have been conducted. This study fills this gap.
This study has some limitations. This is a case–control study with its inherent limitations, which may result in recollection bias among patients who participated in the survey. Moreover, given the limited amount of data, we analyzed factors for regular exercise but not factors for exercise-related behaviors; thus, future research is necessary for further analysis.
So in community hypertension management and patient health education, for middle-aged and elderly patients with hypertension, we should attach importance to patient self-management, such as self-monitoring of blood pressure, and pay attention to the role of exercise and exercise-related behaviors on blood pressure control. Actively promoting walking for exercise and encouraging patients exercise more than 60 min a day can help improve the effects of blood pressure control. Meanwhile, to promote hypertensive patients to participate in sports, we should pay attention to gender differences (including increasing attention to female patients), encourage the patients’ families to accompany the patient in sports, and attach importance to health beliefs as an effective way to improve exercise participation rates.
In conclusion, there was a close relationship between exercise/exercise-related behaviors (such as exercise forms, exercise duration, etc) and blood pressure control in hypertensive patients. Exercise management (such as health belief, company of a family member during exercise) had a significant effect on patients’ exercise behaviors. So improving exercise-related behaviors and their management can help improve the effects of exercise interventions on blood pressure control in middle-aged and elderly hypertensive patients.
Acknowledgments
The authors are grateful to the volunteers for their willingness to participate in the study. Thanks are also due to the professors in the Department of Health Care Management and Department of Epidemiology and Statistics of Fujian Medical University for their strong technical support.
Author contributions
Data curation: Chenyun Zhang, Yanping Zhang, Hao Lin, Siyang Liu, Jing Xie, Yao Tang.
Formal analysis: Yanping Zhang, Jing Xie.
Funding acquisition: Chenyun Zhang.
Investigation: Yanping Zhang, Hao Lin, Jing Xie, Yao Tang.
Methodology: Huiling Huang, Wenchang Zhang.
Resources: Hao Lin, Siyang Liu, Huiling Huang, Wenchang Zhang.
Supervision: Huiling Huang, Wenchang Zhang.
Writing – original draft: Chenyun Zhang, Yanping Zhang.
Writing – review & editing: Chenyun Zhang.
Footnotes
Abbreviations: 95%CI = 95% confidence interval, BMI = body mass index, DBP = diastolic blood pressure, OR = odds ratio, SBP = systolic blood pressure, VIF = variance inflation factor.
How to cite this article: Zhang C, Zhang Y, Lin H, Liu S, Xie J, Tang Y, Huang H, Zhang W. Blood pressure control in hypertensive patients and its relation with exercise and exercise-related behaviours: A case-control study. Medicine. 2020;99:8(e19269).
This work was supported by New Technology Research and Application Project of “Fujian Provincial Key Laboratory of Environment and Health” in 2015 (201506) and supported by Fujian Provincial Department of Education Young and Middle-aged Teacher Education Science Project in 2015 (JAS150259).
The authors have no conflicts of interest to disclose.
References
- [1].Bromfield S, Muntner P. High blood pressure: the leading global burden of disease risk factor and the need for worldwide prevention programs. Curr Hypertens Rep 2013;15:134–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].National Health and Family Planning Commission of the People's Republic of China. Report on Chinese Residents’ Chronic Diseases and Nutrition. 2015;Beijing, China: People's Medical Publishing House, 48. [Google Scholar]
- [3].Li W, Gu H, Teo KK, et al. Hypertension prevalence, awareness, treatment, and control in 115 rural and urban communities involving 47000 people from China. J Hypertens 2016;34:39–46. [DOI] [PubMed] [Google Scholar]
- [4].Diaz KM, Booth JN, Seals SR, et al. Physical activity and incident hypertension in African Americans: the Jackson heart study. Hypertension 2017;69:421–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kawasaki T, Sullivan CV, Ozoe N, et al. A long-term, comprehensive exercise program that incorporates a variety of physical activities improved the blood pressure, lipid and glucose metabolism, arterial stiffness, and balance of middle-aged and elderly Japanese. Hypertens Res 2011;34:1059–66. [DOI] [PubMed] [Google Scholar]
- [6].Lu HT, Fang HY, Ding C, et al. A case-control study on influencing factors of community-based hypertension control. Zhejiang Prev Med 2015;27:665–8. [Google Scholar]
- [7].Writing Group of 2010 Chinese Guidelines for the Management of Hypertension. 2010 Chinese guidelines for the management of hypertension. Chin J Cardiol 2011;39:579–616. [PubMed] [Google Scholar]
- [8].Coorperative Meta-analysis Group of China Obesity Task Force. Predictive values of body mass index anoud waist circumference to risk factors of related diseases in Chinese adult population. Chin J Epidemiol 2002;23:5–10. [PubMed] [Google Scholar]
- [9].Börjesson M, Onerup A, Lundqvist S, et al. Physical activity and exercise lower blood pressure in individuals with hypertension: narrative review of 27 RCTs. Br J Sports Med 2016;50:356–61. [DOI] [PubMed] [Google Scholar]
- [10].Bennett DA, Du H, Clarke R, et al. Association of physical activity with risk of major cardiovascular diseases in Chinese men and women. JAMA Cardiol 2017;2:1349–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Uhlig K, Patel K, lp S, et al. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med 2013;159:185–94. [DOI] [PubMed] [Google Scholar]
- [12].Lee MR, Lim YH, Hong YC. Causal association of body mass index with hypertension using a Mendelian randomization design. Medicine 2018;97:e11252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sadja J, Tomfohr L, Jiménez JA, et al. Higher physical fatigue predicts adherence to a 12-week exercise intervention in women with elevated blood pressure. Health Psychol 2012;31:156–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Zhang YP, Zhang CY, Tang Y, et al. A meta-analysis on the effectiveness of exercise interventions on blood pressure control among hypertensives in China. Chin J Hypertens 2018;26:745–53. [Google Scholar]
- [15].Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc 2013;2:e004473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Cornelissen VA, Fagard RH, Coeckelberghs E, et al. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension 2011;58:950–8. [DOI] [PubMed] [Google Scholar]
- [17].Rossi A, Moullec G, Lavoie KL, et al. Resistance training, blood pressure, and meta-analysis. Hypertension 2012;59:e22–3. [DOI] [PubMed] [Google Scholar]
- [18].Ishikawa-Takata K, Ohta T, Tanaka H. How much exercise is required to reduce blood pressure in essential hypertensives: a dose-response study. Am J Hypertens 2003;16:629–33. [DOI] [PubMed] [Google Scholar]
- [19].Fonseca AL, Koyama J, Butler EA. The role of family of origin in current lifestyle choices: a qualitative secondary data analysis of interracial and same-race couples. Fam Community Health 2018;41:146–58. [DOI] [PMC free article] [PubMed] [Google Scholar]


