Abstract
Background:
Unrecovered Bell palsy is difficult to treat, because until now in literature there is not a gold standard. This study aimed to evaluate the effectiveness of neuromuscular electrical stimulation (NMES) and shortwave diathermy (SWD) therapy for chronic Bell palsy.
Methods:
After 5 months of conventional therapy, this 2-arm randomized controlled trial enrolled and randomly allocated 20 patients to a treatment group with NMES+SWD and supervised exercises (n = 10) or a sham group with supervised exercise alone (n = 10). The administration of NMES or sham NMES, as intervention, was performed 30 min/session, 5 sessions/wk, for 4 weeks. The primary outcome was assessed by Sunnybrook scale. The secondary outcomes were evaluated by the Kinovea©, a movement analysis software. All primary and secondary outcomes were measured at baseline (T0), at the end of 4-week treatment (T1).
Results:
At the end of 4-week treatment, the patients in the treatment group did not achieve better outcomes in resting symmetry, but we observed an increase of the perceived a significant improvement (P < .05) for symmetry of voluntary movements by the Sunnybrook subscale, with a score of 55.4 ± 9 compared to 46.4 ± 3.7 to control group and an increase in zygomatic muscle movement symmetry ratio (P < .05) by Kinovea©. No adverse events occurred in either group.
Conclusion:
The improvements in the symmetry of voluntary movements demonstrated that combining diathermy with neuromuscular electrostimulation is valid and reliable in the treatment of chronic Bell palsy.
Keywords: Bell palsy, facial paralysis, shortwave diathermy, neuromuscular electrical stimulation, neuromuscular electrical stimulation
1. Introduction
Facial paralysis, also known as Bell palsy (BP), is an acute facial nerve disease in which the 1st symptoms can be pain in the mastoid region and cause facial hemiparesis or paralysis. The annual incidence of BP is between 11.5 and 40.2 cases for 100,000 people. BP has a good prognosis.[1] Regression of BP was reported within 3 weeks in 85% of 2570 patients and in the remaining 15% after 3 to 5 months; normal mimic function was observed in 71% and mild to severe sequelae in the remaining 29% of patients, the contracture and associated movements were present in 17% and 16% of patients, respectively.[2] A survey showed that no treatment, including prednisone, could provide a better prognosis. The American Academy of Otolaryngology recommends 10 days of oral corticosteroids. No evidence supports only oral antiviral therapy for the management of BP.[3] In the past auto-massage and infrared (10 minutes) of the face muscles were applied, over interrupted galvanic stimulation for 3 times for a total of 90 contractions (pulse 100 milliseconds).[4] More than half of the patients need physical therapy,[5] in particular the importance of combining rehabilitation with conventional medical treatment for a better BP result in all age groups has been reported.[5] Pereira et al reported that mime therapy is effective for facial palsy for the outcome functionality.[6] It was demonstrated that early electric stimulation (ES) after a denervation injury could maintain normal motor unit characteristics and could improve functional recovery.[5] Alakram and Puckree reported that ES in BP acute phase improves the rate of recovery.[7] Tuncay et al, in a randomized controlled trial (RCT) with 60 patients, showed that the addition of 3 weeks of daily ES shortly after the start of facial paralysis (4 weeks) improved functional facial movements and electrophysiological outcome measures at 3 months of follow-up in patients with Bell palsy.[8] Neuromuscular electrical stimulation (NMES) is a treatment that uses a small electrical current to activate nerves innervating muscles affected by paralysis neurologic disorders.[9] Choi demonstrated that NMES is effective in muscle strengthening, in preventing muscular atrophy, in neuromuscular rehabilitation and improves facial muscle strength in stroke patients with facial paralysis.[10] Kim reported that for facial muscles, it is hard to generate enough tensions by applying loads since they insert into skin while limb muscles insert to bones. It is hypothesized that facial NMES would be more effective if a certain amount of load or tension could be applied while the facial muscles are contracting voluntarily or by electrical stimulation.[11] Pan added shortwave diathermy (SWD) to acupuncture in 38 individuals and compared them with another 37 participants that received only acupuncture. There was no statistically significant difference between groups in the number of participants that had not improved after 30 days.[12,13] A review demonstrated that SWD determines pain relief and increases metabolic functions and deep tissue temperature.[14,15] However, some may not recommend its use in BP because there is acute viral inflammation of the facial nerve in its early stage. On the contrary, it was suggested that pulsed SWD could be of benefit in BP.[5] Baude et al showed that a free 2-dimensional motion analysis software can perform a 2-dimensional analysis of the movements related to 6 facial muscles, evaluating distances, angles and space-time parameters, frame by frame, from a video recording.[16,17] The purpose of this pilot study is to demonstrate that the application of ES and SWD is able to combine the benefits of the 2 physical therapies, reducing the risk of complications and ensuring adequate functional recovery.
2. Methods
2.1. Study design
A randomized, single-blind, controlled study was conducted in 20 patients affected by unrecovered Bell palsy. This study was performed according to the guidelines of the Declaration of Helsinki. Before the enrollment of the 1st patient, the study protocol, the informed consent, and any other document were submitted to the analysis of the local ethical committee, whose approval was obtained before the start of the study.
Twenty-two patients were assessed for eligibility, 1st diagnosed with Bell palsy by a neurologist were referred for physiotherapy. Subjects had no history of any type of facial paralysis. Thirteen patients had a right-side facial droop and 9 a left side. A neurologist after diagnosis of exclusion prescribed corticosteroid and antiviral therapy in all cases within 3 days of onset. Only patients who did not show healing after 5 months (10.4 ± 6.4 months from diagnosis) of conventional therapy prescribed by the neurologist were selected.[2] All patients signed informed consent. The exclusion criteria were neoplasia, dermatologic and autoimmune diseases in progress, and motor neuron diseases. Twenty-two patients were assessed for eligibility (n = 2, declined to participate). Twenty patients (M = 14, F = 6; 42.2 ± 7.6 years), using the minimization, a stratified sampling method,[18] patients were randomly allocated into 2 groups: group A (n = 10) for the therapeutic NMES with SWD and supervised re-education exercise, and group B (n = 10) for sham NMES-diathermy therapy and supervised re-education exercise.
2.2. Outcome
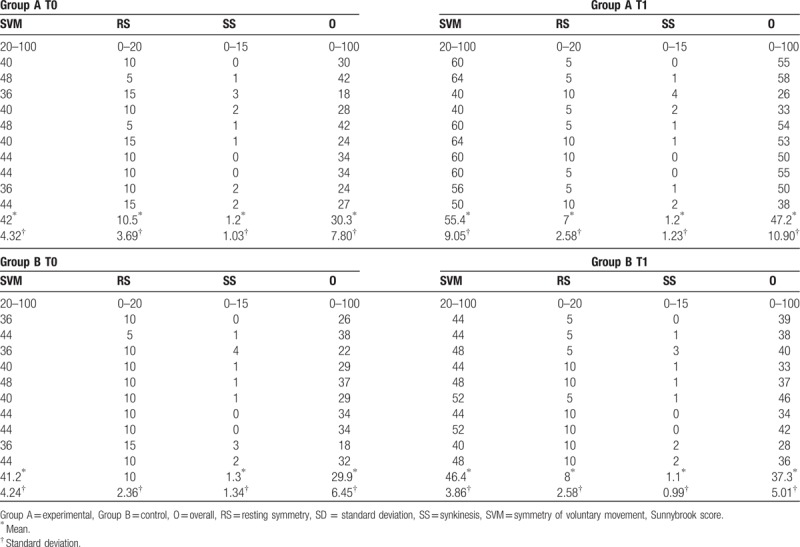
An independent expert assessor evaluated the severity of BP by Sunnybrook facial assessment scale.[19] It is a weighted scale based on evaluation of 3 different subscale including resting symmetry, symmetry of voluntary movement, and severity of synkinesis to form one single composite score from 0 to 100. Firstly, the physician assesses the symmetry of the eye (0–1), cheek (0–2), and mouth (0–1) at rest. (0 = normal, weighted factor of 5). Secondly, the physician rates facial movements during 5 standard facial expressions: brow lift, gentile eye closure, open mouth smile, snarl and lip pucker, on a scale of 1 to 5 (1 = no movement, to 5 = normal movement). The values are added together and multiplied by 4. In the 3rd step, the severity of synkinesis on a 3-point scale (0 = none, to 3 = severe) during the 5 expressions as in the 2nd step. The overall score is given by the symmetry value of the voluntary movements minus the resting symmetry and the synkinesis. Before the treatment the subject showed an overall score in Sunnybrook scale of 30.3 ± 7.8 in group A and 29.9 ± 6.45 in group B (Table 1). The patients, in addition to Sunnybrook scale, were evaluated with a video postproduction software before (T0) and at the end of the treatment (T1).
Table 1.
Sunnybrook scale scores.
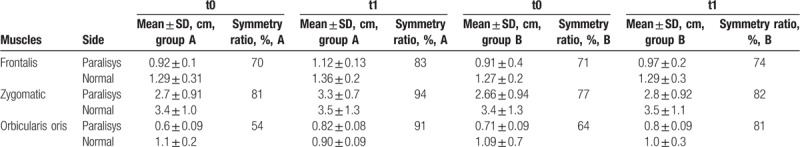
As a secondary outcome, we used Kinovea©, a free and open-source tool for movement analysis (Kinovea©, 0.8.15 2006 to 2011; Joan Charmant & Contrib, Bordeaux, France). From plain video-recordings of movements, the software allows measuring distances and times, manually or using semiautomated tracking to follow points and check live values or trajectories. Facial distances were measured after maximal contractions movements of 3 selected facial muscles: frontalis, orbicularis oris, zygomatic. A symmetry ratio calculated comparing sides of each movement pattern. Subjects had to look straight ahead towards a specified target fixed on the facing wall and it was asked them not to move during video acquisitions. It was asked to keep the head lean the wall, keeping firm it during the 3 tested movements.[16]
2.3. Treatments
All patients in experimental group were treated by a bipolar hand piece (Imperium 400; Brera Technologies, Ogliastro Cilento SA, Italy) able to generate simultaneous short waves and low frequency electrical stimulation, using a bipolar handpiece (Fig. 1).
Figure 1.

Bipolar handpiece.
The 2 electrodes were positioned on of the 3 muscles: orbicularis oris, zygomaticus, and frontalis, in addition to generating a current, acting like 2 plates of a condenser and develop a SWD. Therefore, in the area under the line of each electric waveform a radiofrequency has been produced such as to generate a SWD (8–12 W power; 2.2 MHz frequency[15]). In each session, we delivered 2 different waveforms. A monophasic waveform, triangular in the beginning and then rectangular was used, respectively, to stimulate partially denervated motor units and those totally denervated. The electrical stimulation unit provided 1 channel of bipolar electrical stimulation at a fixed 80-Hz pulse rate and a fixed biphasic pulse duration of 700 microseconds. The intensity was gradually increased from 0.5 mA until the physiotherapist confirmed the visible muscle contraction and the subject felt a grabbing sensation in facial muscles. Subjects received the treatment for 30 min/session, 5 sessions/wk, for 4 weeks.[10] All patients received a supervised rehabilitation exercise (mime therapy): therapeutic massage, breathing and relaxation exercise, exercise for opening and closing eye and lip, exercise of facial expression (mime), and pronunciation of letter and word.[6]
3. Results
Data were analyzed using R v3.5.1 (USA-2018). Data tested for normality using the Shapiro–Wilk normality test. Median and interquartile range were used to describe the nonparametric data and Wilcoxon signed rank test were used for significance testing. Parametric data were reported as mean ± SD and tested with Student t test and analysis of variance. At the end of the treatment a significant improvement was evident for symmetry of voluntary movements (P < .05) by the Sunnybrook subscale, with a score of 55.4 ± 9 in group A compared to 46.4 ± 3.7 in group B. No significant improvement showed in Sunnybrook subscales for resting symmetry from −7 ± 2.6 in group A compared to group B 8 ± 2.8. In Sunnybrook subscale for synkinesis showed no evidence in both groups. Using Kinovea©, we reported a significant improvement (P < .05) in the symmetry ratio voluntary movement of the zygomatic muscle in group A 94 ± 3.7% compared to 82 ± 1.4% in group B (Fig. 2, Table 2).
Figure 2.

Before (A, B) and after treatment (C, D) using Kinovea© software.
Table 2.
Kinovea symmetry ratio.
4. Discussion
This study was conducted to investigate the synergistic effect on chronic Bell palsy of 2 physical therapies (NMES and SWD) simultaneously by the same device. The comparison with supervised exercise showed significant results in recovery from palsy in symmetry during voluntary movement and zygomatic muscle task. The exact etiology of BP remains uncertain, so initially most therapies focused on treatment of the inflammation of the facial nerve. A corticosteroid-antiviral combination therapy is recommended, but it should be better to use physical therapy that not only enhances the success of the conventional treatments but also minimizes the risk of serious side effects related to the medications.[20] Others confirmed the relevance of association of the physical therapy to the conventional medical treatment for a better outcome from BP in all age groups.[21] Diels did not recommend ES[22] for fear of worsening contracture, interfering with re-innervation or increasing treatment costs, but the literature supports that NMES is safe and can enhance muscle strength, delay muscle atrophy, and reduce spasticity.[9] Additionally, even if motor recovery is not evident, long-term electrical stimulation may improve residual clinical impairments in patients with chronic facial paralysis.[23] Nevertheless, to avoid any sequelae, contractures, or synkinesis, we used NMES and SWD simultaneously. In fact, no subject treated with NMES+SWD showed sequelae compared to control group. SWD could be beneficial in BP,[5,24] due to the capacity of SW to decrease pain, increase metabolic functions, improve microcirculation, and avoid muscles contractures.[14] Facial paralysis, synkinesis, and resting asymmetry presented before treatment in either group remained or slightly improved, but improvements in voluntary facial muscle movements, especially for the zygomatic muscle, have been significant. After 6 months from the diagnosis of a mild BP, full recovery is difficult, but improving the voluntary movements of the facial muscles becomes essential for everyday activities. The success achieved in the normalization of movements and functions following treatment supports the effectiveness of this type of intervention.
4.1. Limitation
The use of electrotherapy in literature is controversial, but NMES showed indications in neurorehabilitation of paralysis.[9] The sample is small, but it was necessary to have a homogeneous number of patients, with a mild unrecovered chronic BP.[2] There is no consensus assessment for the evaluation of facial paralysis, but the Sunnybrook score compared to other scales is able to divide what is the symmetry at rest and the movements of the face, as well as to consider the synkinesis. Kinovea© is an easy software, free, and available online. It allowed us to objectify the improvements, although this software was not created for this purpose.[16]
5. Conclusion
In present pilot study, the synergic use of NMES and short-wave diathermy demonstrates, avoiding contractures and synkinesis, a significant improvement in symmetry of voluntary movement in spontaneously unrecovered chronic Bell palsy.
Author contributions
Conceptualization: Nicola Marotta, Maria Teresa Inzitari.
Data curation: Andrea Demeco, Maria Giovanna Caruso.
Formal Analysis: Nicola Marotta.
Investigation: Nicola Marotta, Andrea Demeco.
Methodology: Andrea Demeco, Maria Teresa Inzitari.
Project administration: Antonio Ammendolia.
Software: Nicola Marotta, Andrea Demeco.
Supervision: Antonio Ammendolia.
Writing – original draft: Nicola Marotta.
Writing – review & editing: Antonio Ammendolia, Andrea Demeco, Maria Giovanna Caruso.
Nicola Marotta orcid: 0000-0002-5568-7909.
Footnotes
Abbreviations: BP = Bell palsy, ES = electrical stimulation, NMES = neuromuscular electrical stimulation, RCT = randomized controlled trial, SWD = short-wave diathermy.
How to cite this article: Marotta N, Demeco A, Inzitari MT, Caruso MG, Ammendolia A. Neuromuscular electrical stimulation and shortwave diathermy in unrecovered Bell palsy: a randomized controlled study. Medicine. 2020;99:8(e19152).
The material was not presented at an AAPM&R Annual Assembly and not any funding source.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Adour KK. Diagnosis and management of facial paralysis. N Engl J Med 1982;307:348–51. [DOI] [PubMed] [Google Scholar]
- [2].Peitersen E. Bell's palsy: the spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta Otolaryngol Suppl 2002;4–30. [PubMed] [Google Scholar]
- [3].Vargish L, Schumann SA. For Bell's palsy, start steroids early; no need for an antiviral. J Fam Pract 2008;57:22–5. [PMC free article] [PubMed] [Google Scholar]
- [4].Mosforth J, Taverner D. Physiotherapy for Bell's palsy. Br Med J 1958;2:675–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Shafshak TS. The treatment of facial palsy from the point of view of physical and rehabilitation medicine. Eur Med 2006;42:41–7. [PubMed] [Google Scholar]
- [6].Pereira LM, Obara K, Dias JM, et al. Facial exercise therapy for facial palsy: systematic review and meta-analysis. Clin Rehabil 2011;25:649–58. [DOI] [PubMed] [Google Scholar]
- [7].Alakram P, Puckree T. Effects of electrical stimulation in early Bells palsy on facial disability index scores. South Afr J Physiotherapy 2011;67:35–40. [Google Scholar]
- [8].Tuncay F, Borman P, Taser B, et al. Role of electrical stimulation added to conventional therapy in patients with idiopathic facial (Bell) palsy. Am J Phys Med Rehabil 2015;94:222–8. [DOI] [PubMed] [Google Scholar]
- [9].Sheffler LR, Chae J. Neuromuscular electrical stimulation in neurorehabilitation. Muscle Nerve 2007;35:562–90. [DOI] [PubMed] [Google Scholar]
- [10].Choi JB. Effect of neuromuscular electrical stimulation on facial muscle strength and oral function in stroke patients with facial palsy. J Phys Ther Sci 2016;28:2541–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kim CA, Chung SG, Kim KE. Force Generation Capacity of Zygomaticus Muscle by Facial NMES. 11th Annual Conference of the International FES Society, September 2006 – Zao, Japan. [Google Scholar]
- [12].Pan L. Acupuncture plus short wave for 38 peripheral facial paralysis. J Clin Acupunct Moxibust 2004;20:26–7. [Google Scholar]
- [13].Teixeira LJ, Valbuza JS, Prado GF. Physical therapy for Bell's palsy (idiopathic facial paralysis). Cochrane Database Syst Revs 2011;CD006283. [DOI] [PubMed] [Google Scholar]
- [14].Cacolice PA, Scibek JS, Martin RR. Diathermy: a literature review of current research and practices. Orthopaedic Phys Ther Prac 2013;25:155–61. [Google Scholar]
- [15].de Sousa, JN. O uso da diatermia por radiofrequência no tratamento das rugas e flacidez facial: Revisão bibliográfica, 2016. [Google Scholar]
- [16].Baude M, Hutin E, Gracies JM, et al. A bidimensional system of facial movement analysis conception and reliability in adults. BioMed Res Int 2015;2015: 812961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Puig-Diví A, Escalona-Marfil C, Padullés-Riu JM, et al. Validity and reliability of the Kinovea program in obtaining angles and distances using coordinates in 4 perspectives. PLoS One 2019;14:e0216448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial (1975) biometrics (International Biometric Society) 1975;31:103–15. [PubMed] [Google Scholar]
- [19].Kang TS, Vrabec JT, Giddings N, et al. Facial nerve grading systems (1985–2002): beyond the House-Brackmann scale. Otology & neurotology 2002;23:767–71. [DOI] [PubMed] [Google Scholar]
- [20].Phan NT, Panizza B, Wallwork B. A general practice approach to Bell's palsy. Australian family physician 2016;45:794–7. [PubMed] [Google Scholar]
- [21].Pourmomeny AA, Asadi S. Facial rehabilitation. Phys Treat Specific Phys Therapy J 2014;4:61–8. [Google Scholar]
- [22].Diels HJ. Facial paralysis: is there a role for a therapist? Facial Plast Surg 2000;16:361–4. [DOI] [PubMed] [Google Scholar]
- [23].Targan RS, Alon G, Kay SL. Effect of long-term electrical stimulation on motor recovery and improvement of clinical residuals in patients with unresolved facial nerve palsy. Otolaryngol Head Neck Surg 2000;122:246–52. [DOI] [PubMed] [Google Scholar]
- [24].Murray CC, Kitchen S. Effect of pulse repetition rate on the perception of thermal sensation with pulsed shortwave diae perception of thermal sensation with pulsed shortwave diathermy. Physiotherapy Res Int 2000;5:73–84. [DOI] [PubMed] [Google Scholar]


