Abstract
The transition to adulthood is a developmental period marked by increased stress, especially among African Americans. In addition to stress related to emerging adulthood, neighborhood fear may contribute to depressive symptoms for African Americans. We examined gender differences in longitudinal associations between changes in perceived neighborhood fear, parental support, and depressive symptoms among African American youth who were in transition to adulthood. Five hundred and thirteen African American youths (235 males and 278 females) were included in the study. An increase in perceived neighborhood fear was associated with an increase in depressive symptoms and change in perceived maternal support was predictive of depressive symptoms among males, but not females. The findings suggest that policies and programs should help parents provide support to young adult children who live in violent neighborhoods as a strategy to prevent depressive symptoms during emerging adulthood.
Keywords: violence, depression, parenting, African Americans, gender, emerging adulthood
1. Introduction
1.1. Depression and African Americans
Major depressive disorder (MDD) and depressive symptoms are substantial sources of public health burden in United States [1]. Depression is the leading cause of disability and a significant contributor to the global burden of disease [2] and 20% of U.S. residents may have high levels of depressive symptoms [3]. Although at least that 10% of adults in the United States meet DSM-IV criteria for major depression, this prevalence differs by race, gender, and age [4]. Although several studies have shown that MDD may have a lower prevalence among African Americans than Whites in the U.S. [5,6,7], other reports suggest that African Americans may experience higher severity of depressive symptoms than Whites [8]. Depression tends to be more chronic, severe, and disabling for African Americans [7,9].
1.2. Developmental Risks for Depressive Symptoms among African Americans
Emerging adulthood may be a key developmental stage when African American youth may be at risk for experiencing depression and depressive symptoms. Researchers examining depressive symptoms among nationally representative samples of emerging adults indicate that African Americans report higher rates of depressive symptoms during the transition to adulthood than their White peers. A seminal work on depression among a nationally representative sample of African Americans conducted by Williams and colleagues indicated that adults between the ages of 18–29 reported higher lifetime rates of depression compared to those 30 or older [7]. Earlier work examining prevalence of depression in an epidemiologically defined sample of 1197 African American young adults ages 18–22 living in Baltimore City found a 9.4 percent lifetime MDD prevalence among their study population [10]. These findings are largely explained by socioeconomic disadvantage and living in stressful conditions [11].
The transition to adulthood is a developmental period marked by increased perceived stress combined with multiple transitions as young people strive to achieve financial, residential, and emotional independence [12,13]. In addition to these normative developmental challenges, African Americans transitioning to adulthood in economically disadvantaged urban contexts experience many contextually specific stressors that place them at risk for experiencing depressive symptoms [14]. In 2012, Estrada-Martinez et al. examined the effect of perceived stress in multiple life domains (daily life, finances, racial discrimination, and neighborhood) on risk for depressive symptoms among African American males and females during emerging adulthood. Their results indicated that depressive symptoms increase as the number of stressors increase during emerging adulthood [14].
1.3. Fear of Neighborhood Violence
For African Americans transitioning to adulthood in the inner city, neighborhood fear may be a significant risk factor for depression. Exposure to violence is known to result in higher depressive symptoms among African Americans [15,16,17,18,19,20,21,22]. African American youth, especially those living in low-income neighborhoods are more likely to witness shootings, stabbings, and killings in their neighborhoods than their White and middle to upper income peers, with African American males more likely to be victims of neighborhood violence than African American females [23,24].
Even in the absence of direct exposure to violence, living in unsafe neighborhoods engenders fear of neighborhood violence [25,26,27]. Studies examining the relationship between fear of violence and mental health among adolescents [25] and adults [27] living in economically disadvantaged neighborhoods suggest that perceived neighborhood fear is predictive of higher depressive symptoms [28]. African Americans are more likely to live in low-income communities where structural inequities increase the propensity for disorder and violence placing them at increased vulnerability for the onset of depressive symptomology [27,29].
Fear of violence has unique implications for the mental health and well-being of African American youth during the transition to adulthood [30,31]. Developmentally, young people are expected to craft occupational, educational, and relational aspirations for their lives and futures. In addition to the reality of constrained geographies of opportunity [31,32], fear of neighborhood violence may add to perceived stress and reduce future orientation among African Americans [33]. In unsafe neighborhoods, maintenance of survival may become a priority for the residents [34].
1.4. Parental Support and Depression
Parental support may prevent depression during transition to adulthood. Although young adults are working to individuate from parents during this developmental period, research has suggested that young adults may be in particular need of parental support [13]. Research has shown a negative relationship between parental support and depressive symptoms during the transition to adulthood [11,35]. Yet, variation in the relationship between parental support and depressive symptoms may emerge based on race, gender, and socioeconomic status [35].
Using a life course perspective [36,37] and informed by socio-ecological model of development [38], the present study investigates the association between fear of neighborhood violence, parental support, and depressive symptoms during emerging adulthood in a longitudinal sample of African American youth who live in an urban area. Specifically, the current study explored gender differences in the associations between changes in perceived fear of neighborhood violence from ages 21 to 22, changes in perceived support from mothers and fathers from ages 21 to 24, and changes in depressive symptoms from ages 23 to 24.
2. Methods
This study used data of the Flint Adolescent Study (FAS), an 18-year longitudinal study of youth from adolescence to their transition to early adulthood from 1994 to 2012 [39,40]. Participants provided consent or assent before each interview. The study protocol was approved by the local Institutional Review Board.
Participants were sampled from four local public high schools. The study sampled ninth graders who had a grade point average (GPA) of 3.0 or lower (in eighth-grade) if they did not have a diagnosis of a developmental disability or emotional impairment.
For the current analysis we used socio-economic data collected at age 15 (Wave 1, year 1994), fear of neighborhood violence at ages 21 and 22 (Waves 5 and 6, years 1999 and 2000), parental support at ages 21 and 24 (Waves 5 and 8, years 1999 and 2002), and depressive symptoms at ages 23 and 24 (Waves 7 and 8, years 2001 and 2002).
513 African American youths (235 males and 278 females) were entered to the current study. Retention rate was 90% from Waves 1 to 4, 75% from Waves 4 to 8. African Americans in this study were not different from those who did not participate for age, education level, and family structure (p > 0.05 for all comparisons).
2.1. Procedure
Data were collected using structured face-to-face interviews conducted either at school or at alternative community locations (Appendix. 1). On average, each interview lasted about 60 min. This study followed participants regardless of students’ dropping out of school.
2.2. Measures
2.2.1. Covariates
Age and two measures of family socio-economic status (parental employment and family structure) were measured at baseline. Parental employment status was self-reported and was operationalized as a dichotomous variable (both parents employed versus any other conditions). Family structure was also measured as intact (youth living with both biological parents versus any other condition) or others.
2.2.2. Symptoms of Depression
Depressive symptoms were measured by six items from the Brief Symptom Inventory [41,42]. These items assess frequency of feeling uncomfortable during the past seven days due to symptoms of depression such as feeling hopeless about the future, and having no interest in things. Response options on the Likert scale ranged from 1 (not at all uncomfortable) to 5 (extremely uncomfortable). These six items were averaged to form the final scale. Literature has shown that this scale has high internal consistency and test–retest reliability and is valid to use with adolescents [41,42,43]. Cronbach’s alpha was 0.77 for the current sample at Wave 5.
2.2.3. Parental Support
Maternal and paternal support measures in the current study were the modified versions of measure by Procidano and Heller developed in 1983 for measuring parental support [44]. This measure had five items on the degree to which the parent gave emotional and instrumental support and the closeness of the parent-youth relationship. All items used a 5-point scale, ranging from 1 (not true) to 5 (very true). A composite score was created by taking the average of the items [45]. Cronbach’s alpha = 0.88 and 0.86 for maternal and paternal support at Wave 5, respectively.
2.2.4. Fear of Neighborhood Violence
The following two items were used to measure individual perception of fear from violence in the neighborhood: (1) I am afraid of the violence in my neighborhood; and (2) I worry that someone in my neighborhood will physically hurt me. Both items used a 4-point Likert scale, ranging from 1 (strongly disagree) to 4 (strongly agree). The two items were positively correlated (r = 0.435, p < 0.05).
2.3. Data Analysis Strategy
The current study only included African Americans, as only 17% of the original sample was composed of Whites. Univariate and bivariate analysis were done in SPSS 20.0. Bivariate associations were tested using Pearson’s correlation and paired samples t-test. We used AMOS 18.0 for multivariable analysis [46,47].
Structural equation modeling (SEM) was used for multivariable data analysis [48]. In the first step, we fitted model with no constraining of paths across the groups. In the next step, we released constraints and compared the fit with that of previous mode. We also tested models where the error variances for corresponding pretest and posttest measures were correlated. As the fit did not improve in the second model, we reported the model with released constraints. In our models, we performed multi-group analysis where the group was defined based on gender. We compared the path coefficients between the groups for statistically significant difference.
Fit statistics included were Chi square, the comparative fit index (CFI) [>0.90], the root mean squared error of approximation (RMSEA) [<0.06], and X2 to degrees of freedom ratio [49,50,51]. Unstandardized and standardized regression coefficients were reported. We implemented full information maximum likelihood (FIML) to account for missing data. We considered p less than 0.05 as significant.
3. Results
3.1. Univariate Analysis
Table 1 provides descriptive statistics for fear of neighborhood violence, paternal support, maternal support, and depressive symptoms. Paired samples t-test suggested that depressive symptoms increased among male but decreased among females. In both genders, maternal support decreased from ages 21 to 24, while support from father increased.
Table 1.
Descriptive statistics among male and female African American youth.
| Men | Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Min | Max | Mean | SD | n | Min | Mas | Menu | SD | |
| Fear of violence ill neighborhood at age 21 | 205 | 1.0 | 4.0 | 1.39 | 0.64 | 265 | 1.0 | 4.0 | 1.50 | 0.67 |
| Fear of violence in neighborhood at age 22 | 235 | 1.0 | 4.0 | 1.43 | 0.66 | 278 | 1.0 | 4.0 | 1.47 | 0.69 |
| Maternal Support at age 21 | 200 | 1.0 | 5.0 | 4.11 | 0.94 | 247 | 1.0 | 5.0 | 3.96 | 1.07 |
| Maternal Support at age 24 | 201 | 1.0 | 5.0 | 4.01 | 0.99 | 235 | 1.0 | 5.0 | 3.97 | 1.09 |
| Paternal Support at age 21 | 142 | 1.0 | 5.0 | 3.36 | 1.15 | 210 | 1.0 | 5.0 | 2.98 | 1.24 |
| Paternal Support at age 24 | 149 | 1.0 | 5.0 | 3.42 | 1.16 | 202 | 1.0 | 5.0 | 3.22 | 1.27 |
| Depressive Symptoms at age 23 | 197 | 1.0 | 5.0 | 1.59 | 0.61 | 262 | 1.0 | 4.3 | 1.84 | 0.75 |
| Depressive Syniptonis at age 24 | 209 | 1,0 | 4.8 | 1.65 | 0.70 | 262 | 1.0 | 4.7 | 1.78 | 0.73 |
3.2. Bivariate Analysis
As Table 2 suggests, fear of violence in the neighborhood at ages 21 and 22 were positively correlated with depressive symptoms at age 23 and 24 both among men and women. Among both genders, support from mother was negatively associated with depressive symptoms. Support from father was not correlated with depressive symptoms for either males or females.
Table 2.
Correlation matrix among male and female African American youth.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 1 | −0.1 | −0.099 | 0.022 | 0.062 | −0.123 | −0.152 * | −0.055 | −0.136 | 0.054 | −0.08 |
| Parent employment | −0.098 | 1 | 0.146 ** | 0.04 | 0.071 | 0.045 | 0.145 * | −0.004 | 0.07 | −0.233 ** | −0.124 |
| Intact family | 0.123 * | 0.128 * | 1 | −0.012 | −0.03 | 0.192** | 0.181 * | 0.169* | 0.273 ** | −0.146 * | −0.121 |
| Fear of violence in neighborhood | 0055 | −0.105 | −0.003 | 1 | 0.384** | −0.128 | −0.054 | −0.155 | 0129 | 0.006 | 0.196* |
| Fear of violence in neighborhood | 0.04 | −0.05 | −0.092 | 0.369 ** | 1 | 0.035 | −0.005 | 0.011 | 0043 | 0.019 | 0.221 ** |
| Support of mother in daily life | 0.015 | 0.016 | 0.044 | −0.111 | −0.015 | 1 | 0.657 ** | 0.361 ** | 0.298 ** | −0.056 | −0.116 |
| Support of mother in daily life | −0.014 | 0.077 | 0.11 | −0.083 | 0.006 | 0.660 ** | 1 | 0.217* | 0.329 ** | −0.195* | −0.290** |
| Support of father in daily life | −0.038 | 0.091 | 0.163* | −0.103 | −0.136 | 0.265 ** | 0.255 ** | 1 | 0.697 ** | −0.132 | −0.078 |
| Support of father in daily life | −0.027 | 0.036 | 0.147* | 0.032 | 0.051 | 004 | 0.221 ** | 0.452** | 1 | −0.199* | −0.13 |
| Depressive Symptoms | 0.089 | −0.086 | −0.104 | 0.126 | 0.078 | −0.302 ** | −0.343 ** | −0.204** | −0.153 * | 1 | 0.575** |
| Depressive Symptoms | −0.053 | −0.005 | 0.003 | 0.146 * | 0.111 | −0.243 ** | −0.157* | −0.069 | −0.042 | 0.539 ** | 1 |
P < 0.05,
P < 0.01; males upper diagonal, females lower diagonal.
3.3. Multivariable Model
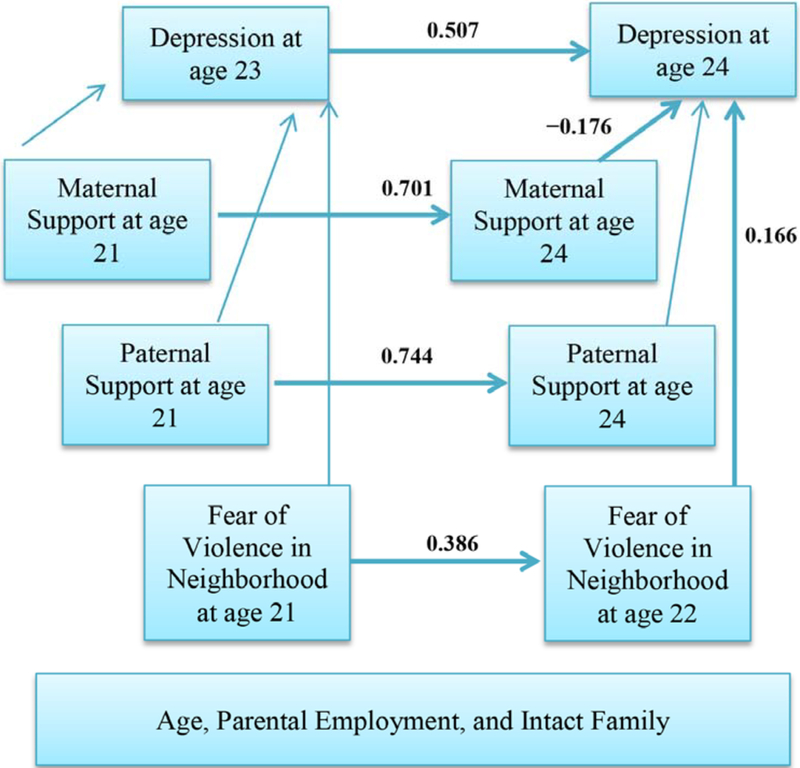
The fit of the structural equation model (Figure 1) was good [χ2 =82.126, df = 52, p = 0.005, χ2/df = 1.579, CFI = 0.950, RMSEA = 0.029, (90% CI = 0.016, 0.041)].
Figure 1.
Summary of path analysis among male African American youth. [χ2 = 82.126, df = 52, p = 0.005, χ2/df = 1.579, root mean squared error of approximation (RMSEA) = 0.029, (90% CI = 0.016, 0.041)]. Paths from covariates and also covariance between exogenous variables are not shown in this model. Numbers are standardized regression coefficients. Significant regression coefficients have been shown in bold.
As depicted in Table 3 and Figure 1, among males, we found a significant and positive path from fear of neighborhood violence at age 21 to fear of neighborhood violence at age 22 (β = 0.386, p < 0.001). We also found a significant and positive path from depressive symptoms at age 23 to depressive symptoms at age 24 (β = 0.507, p < 0.001). The paths from maternal support at age 21 to maternal support at age 24 (β = 0.701, p < 0.001) and also from paternal support at age 21 to paternal support at age 24 (β = 0.744, p < 0.001) were also positive and significant. We also found a significant and positive path from fear of neighborhood violence at age 22 to depressive symptoms at age 24 (β = 0.166, p = 0.013), suggesting that an increase in fear of neighborhood violence over one year from age 21 to age 22 was associated with the increase in depressive symptoms from age 23 to age 24. In addition, there was a negative and significant path from changes in maternal support at age 24 (compared to maternal support at age 21) to increase in depressive symptoms from age 23 to age 24 (β = −0.176, p = 0.003). This path suggests that above and beyond the effect of changes to fear of neighborhood violence over one year from age 21 to age 22, age, family structure, and parental employment, more maternal support at age 24 was associated with lower depressive symptoms from age 23 to age 24. There was not such an association between paternal support at age 24 and changes in depressive symptoms from age 23 to age 24 (p > 0.05).
Table 3.
Summary of path coefficients among male and female African American youth.
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Standardized B | SE | P | Standardized B | SE | P | |||
| Fear of violence in neighborhood at age 21 | → | Pear of violence in neighborhood at age 22 | 0.386 | 0.068 | <0.001 | 0.361 | 0.062 | <0.001 |
| Fear of violence in neighborhood at age 21 | → | Depressive Symptoms at age 23 | 0.016 | 0.072 | 0.836 | 0.062 | 0.07 | 0.321 |
| Maternal Support at age 21 | → | Maternal Support at age 24 | 0.701 | 0.052 | <0.001 | 0.672 | 0.05 | <0.001 |
| Maternal Support at age 21 | → | Depressive Symptoms at age 21 | −0.09 | 0.051 | 0.286 | −0.28 | 0.044 | <0.001 |
| Paternal Support at age 21 | → | Paternal Support at age 24 | 0.744 | 0.061 | <0.001 | 0.472 | 0.069 | <0.001 |
| Paternal Support at age 21 | → | Depressive Symptoms at age 21 | −0036 | 0.048 | 0.699 | −0.098 | 0.043 | 0167 |
| Age | → | Depressive Symptoms at age 21 | 0.007 | 0.062 | 0.921 | 0.044 | 0.07 | 0.447 |
| Parent employment | → | Depressive Symptoms at age 21 | −0184 | 0.083 | 0.008 | −0.048 | 0.09 | 0.424 |
| Intact family | → | Depressive Symptoms at age 21 | −0.06 | 0.093 | 0393 | −0.057 | 0.109 | 0.337 |
| Depressive Symptoms at age 23 | → | Depressive Symptoms at age 24 | 0.507 | 0.068 | <0.001 | 0.528 | 0.055 | <0.001 |
| Fear of violence in neighborhood at age 21 | → | Depressive Symptoms at age 22 | 0.166 | 0.069 | 0013 | 0.054 | 0.063 | 0365 |
| Fear of violence in neighborhood at age 22 | → | Depressive Symptoms at age 21 | 0.098 | 0.075 | 0.163 | 0.067 | 0.068 | 0.281 |
| Maternal Support at age 24 | → | Depressive Symptoms at age 24 | −0.176 | 0.042 | 0.003 | 0.018 | 0.038 | 0.758 |
| Paternal Support at age 24 | → | Depressive Symptoms at age 24 | −0.007 | 0.039 | 0.918 | 0.038 | 0.034 | 0.523 |
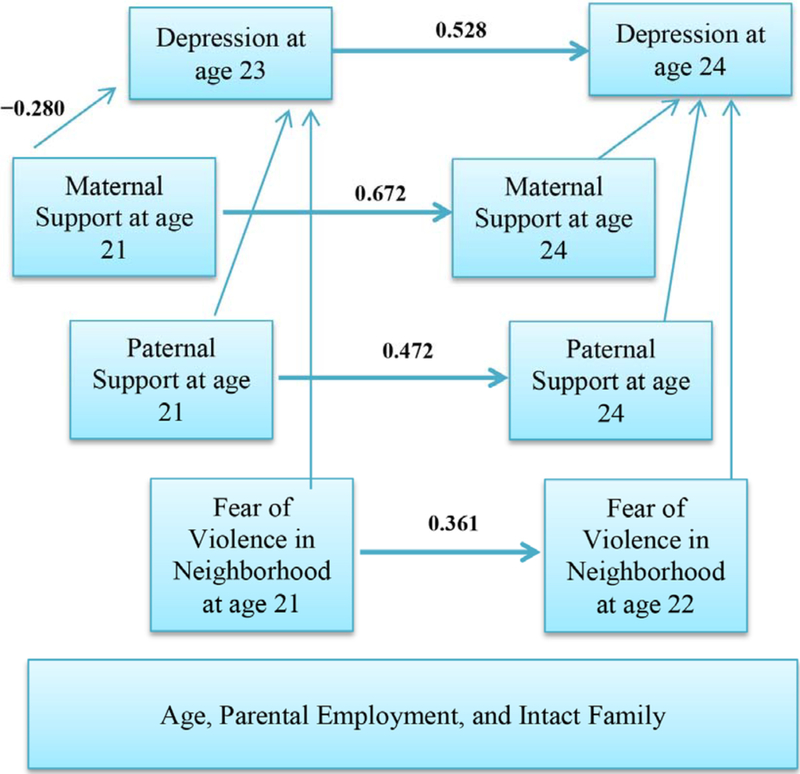
As shown in Table 3 and Figure 2, among females, significant and positive paths from fear of neighborhood violence at age 21 to fear of neighborhood violence at age 22 (β = 0.361, p < 0.001), from depressive symptoms at age 23 to depressive symptoms at age 24 (β = 0.528, p < 0.001), from maternal support at age 21 to maternal support at age 24 (β = 0.672, p < 0.001), and from paternal support at age 21 to paternal support at age 24 (β = 0.472, p < 0.001) were found. We also found a significant and negative path from maternal support at age 21 to depressive symptoms at age 23 (β = −0.280, p < 0.001), but no significant paths from fear of neighborhood violence at age 21 or 22 to depressive symptoms at age 23 or 24 (p > 0.05). This result suggests that baseline or changes in fear of neighborhood violence between ages 21 and 22 are not associated with baseline or changes in depressive symptoms between ages 23 and 24. The path from changes in maternal support at age 24 (compared to maternal support at age 21) changes in depressive symptoms from ages 23 to 24, above and beyond the effect of changes to fear of neighborhood violence over one year from ages 21 to 22, age, family structure, and parental employment, and more paternal support at age 24 (p > 0.05) was not significant.
Figure 2.
Summary of path analysis among female African American youth. [χ2 = 82.126, df = 52, p = 0.005, χ2 / df = 1.579, RMSEA = 0.029, (90% CI = 0.016, 0.041)]. Paths from covariates and also covariance between exogenous variables are not shown in this model. Numbers are standardized regression coefficients. Significant regression coefficients have been shown in bold.
In summary, our study suggested two major gender differences: (1) an increase in perceived fear of neighborhood violence was associated with an increase in depressive symptoms among males but not females; and (2) change in perceived maternal support was predictive of depressive symptoms among males but not females.
4. Discussion
Our results indicate that an increase in fear of neighborhood violence may be associated with an increase in depressive symptoms for African American male, but not for female young adults who live in urban areas. Based on our findings, even a one-year incremental increase in fear of neighborhood violence among African American males between ages 21 and 22 may increase depressive symptoms at ages 23 to 24. These findings offer new insights for policy makers, public health researchers, mental health practitioners, and programmers who wish to design and implement interventions for prevention of depression among African Americans who are in transition to adulthood.
4.1. Fear of Violence and Depressive Symptoms among African American Males
Neighborhood violence is an imminent threat to the mental health of African American males for a protracted period of time during the transition to young adulthood. Our finding on the association between the increase in fear of violence and depressive symptoms is consistent with findings from earlier studies examining the relationship between perceived threat of neighborhood violence and depression [25,27,28]. Our gender differences may be explained by masculinity and gender identity among African American males, which has major implications for their depression [52].
Men are socialized to display toughness, fearlessness, and the denial of vulnerability in the presence of trauma and its risk [53]. We can argue that responses to neighborhood violence among men are not exempt from masculine expectations, and young men may mask their fear in such a way that they adhere to masculine norms. Yet, this incongruence between the internal experience of increasing fear and the external presentation of coolness [54] may contribute to increasing depressive symptoms among African American males during the transition to adulthood. Future studies that examine the relationship between fear of neighborhood violence and depressive symptoms among young African American men during the transition to adulthood may need to consider the role of masculinity in this association.
4.2. Parental Support and Depressive Symptoms during Emerging Adulthood
Our findings also add to existing knowledge about the contribution of changes in parental support to the trajectories of depressive symptoms during transition to adulthood. In 2007, Tracy and colleagues showed that perceived parental support explained most of the relationship between low family income and childhood depressive symptoms [55]. In a study among African American youth, parental support predicted less anxiety and depression longitudinally [56]. Their findings suggested that parental support may help insulate African-American youths from anxiety and depression. Although perceived paternal support increased among both African American males and females, such changes were not associated with depressive symptoms among male and female young adults. Additional research is needed to understand gender differences in the protective role of paternal support on depressive symptoms for African Americans during emerging adulthood in the violent neighborhoods. Future research should compare the protective effect of the same construct (paternal support) in different developmental periods of youth’s lives. We also cannot rule out possible ceiling effect in our results.
In line with previous findings [57,58], our study suggested a major protective role for parental support among African American males. Previous research indicated that more socio-emotional support from the mother was associated with less depressive mood and disruptive behavior among youth [59]. Another study suggested that the influence of maternal support on depression among youth was mediated by perceived stress [23]. This study suggested that maternal support perceived by African American youth is critical to their psychological well-being [23].
In this study, emotional support from African American mothers was protective against worsening depressive symptoms among their young adult sons. From the age 21 to 24, perceived maternal support showed a slight increase among African American females, but a considerable decrease among African American males. For females, changes in perceived maternal support were not predictive of changes in depressive symptoms measured at ages 23–24. The decrease in perceived maternal support was associated with an increase in depressive symptoms among African American males, above and beyond increasing fear of violence, family structure, and parental employment. This partly supports previous findings suggesting that parental support during the transition to adulthood is protective against development of depressive symptoms [60]. Our study, however, suggests that this relationship differs by gender. Gender, race, ethnicity, and other contextual factors are known to be associated with specific paths that shape well-being, health, and illness [40,61,62,63,64,65,66,67,68,69,70,71].
African American males experience many challenges throughout the transition to adulthood as they work to achieve and maintain employment, advance educationally, and transition relationally (e.g., partnering and parenting) [14,72]. For many young adult African American males, these developmental tasks magnify the structural iniquities affecting young African-American men [37,73]. The collective effect of these challenges can be stressful for African American males and can contribute to worsening depressive symptoms for this group [14,74].
In the face of structural and environmental challenges, African American males may turn to their primary and long-standing source for emotional support, their mothers. African American young adult males in economically disadvantaged communities often share residence with their mothers for a longer period of time than their white counterparts. This proximity and accessibility of African American mothers may position them as primary emotional supports for their sons. If there is a shift in perceived emotional support from mothers, particularly for sons co-residing with their mothers, this may be challenging for sons to experience. Yet, this shift may not be indicative of conflict in the mother-son relationship, rather it may be reflective of mothers’ attempts to employ developmentally appropriate parenting. Aware of the need for sons to achieve independence during the transition to adulthood [12], African American mothers may work to slowly pull back emotionally so that their sons can individuate.
Our findings suggest that maintenance of higher levels of emotional support as African American males approach their mid-twenties supports their mental health and protects against worsening depression. Many African American mothers may not recognize depressive symptoms in their sons [75] and unless articulated, may not detect sons’ continued need for higher level of emotional support during the transition to adulthood [37]. Psycho-educational resources for African-American mothers to raise awareness about depressive symptoms among their sons during the transition to adulthood may be necessary to help mothers parent during this developmental period.
4.3. Implications, Recommendations, and Future Directions
The implications of our findings are important because African Americans have lower rates for utilizing formal mental health services broadly [76], and may have lower tendency to seek professional health care for psychiatric disorders such as depression [77]. In the National Survey of American Life, most (55%) of the African Americans who endorsed a clinical diagnosis of major depression had received no treatment for depression during their lifetime [7]. African Americans also less frequently accept medications, and report lower levels of adherence to medication regimens [78]. African Americans also have a tendency to prefer non-pharmacological treatments of depression that are known to be less effective for treatment of depression [79]. African Americans have greater preference for counseling [80] and more interest in counseling from clergy [81].
Our findings suggest that interventions, programs, and policies that boost the maternal support available for African American males who live in violent neighborhoods may be a useful strategy to prevent depressive symptoms during emerging adulthood. Mental health practitioners and public health professionals working to reduce or prevent depressive symptoms among African American young men may benefit by using a family-based approach that leverages maternal support as an available resource during this developmental context.
Although our findings offer additional insights about social factors that may contribute to the trajectories of depressive symptoms among African Americans during transition to adulthood and offers potential preventive strategies, this study is not without limitations. As sampling was not random, the results are not generalizable to all African Americans. Measuring depressive symptoms instead of clinical diagnosis of MDD is another limitation. Future research should address measurement of a clinical diagnosis of depression. Duration of follow up in this analysis was short; future studies should benefit from longer term follow ups. The study was also limited as we only used individual level data. Researchers should investigate how violence at the neighborhood level influences perception of safety and crime at the individual level [82]. The longitudinal design and prolonged enrollment of a minority population should be considered strengths of the study.
To conclude, links between perceived fear of neighborhood violence, parental support and depression among African Americans differ by gender. An increase in perceived fear of violence and a decrease in perceived maternal support are both associated with increase in depressive symptoms for African American males during their transition to adulthood. Clinical practice and public health interventions designed to treat or prevent depression during the transition to adulthood for African American males should consider the critical contributions of unsafe neighborhood contexts and parental support.
Acknowledgments
This study was funded by the National Institute on Drug Abuse (NIDA) (grant DA07484) to Marc Zimmerman. Publication of this manuscript was possible with the Cornely Fellowships awarded by the Department of Psychiatry and also Center for Research on Ethnicity, Culture and Health, University of Michigan to the first and second authors, Shervin Assari, and Jocelyn R. Smith. The content of this article does not necessarily reflect the views or policies of the National Institute on Drug Abuse.
Appendix 1.
Items Used for Measurement of Study Constructs.
| Maternal Support | |||||
| How often do you speak with or see your Mother? | |||||
| 1. Daily 2. Every 2–3 days 3. Every 4–6 days 4. Once a week 5. Two times/month | |||||
| 6. Once a month 7. More than 1 month ago 8. No contact 9 Never met 10. Deceased | |||||
| Please answer the following questions. | |||||
| Not True | Little True | Somewhat True | Pretty True | Very True | |
| My Mother enjoys hearing about what I think. | 1 | 2 | 3 | 4 | 5 |
| I rely on my Mother for emotional support. | 1 | 2 | 3 | 4 | 5 |
| My Mother is good at helping me solve problems. | 1 | 2 | 3 | 4 | 5 |
| I have a deep sharing relationship with my Mother. | 1 | 2 | 3 | 4 | 5 |
| I rely on my Mother for moral support. | 1 | 2 | 3 | 4 | 5 |
| Although I trust my Mother, sometimes I have my doubts. | 1 | 2 | 3 | 4 | 5 |
| My Mother understands me. | 1 | 2 | 3 | 4 | 5 |
| I wish I had a different Mother. | 1 | 2 | 3 | 4 | 5 |
| Paternal Support | |||||
| How often do you speak with or see your Father? | |||||
| 1. Daily 2. Every 2–3 days 3. Every 4–6 days 4. Once a week 5. Two times/month | |||||
| 6. Once a month 7. More than 1 month ago 8. No contact 9 Never met 10. Deceased | |||||
| Please answer the following questions. | |||||
| Not True | Little True | Somewhat True | Pretty True | Very True | |
| My Father enjoys hearing about what I think. | 1 | 2 | 3 | 4 | 5 |
| I rely on my Father for emotional support. | 1 | 2 | 3 | 4 | 5 |
| My Father is good at helping me solve problems. | 1 | 2 | 3 | 4 | 5 |
| I have a deep sharing relationship with my Father. | 1 | 2 | 3 | 4 | 5 |
| I rely on my Father for moral support. | 1 | 2 | 3 | 4 | 5 |
| Although I trust my Father, sometimes I have my doubts. | 1 | 2 | 3 | 4 | 5 |
| My Father understands me. | 1 | 2 | 3 | 4 | 5 |
| I wish I had a different Father. | 1 | 2 | 3 | 4 | 5 |
| Fear of Violence in the Neighborhood | |||||
| Using this 4-point scale, please tell me how much you agree with the following statements. | |||||
| Strongly Disagree | Strongly Agree | ||||
| I am afraid of the violence in my neighborhood. | 1 | 2 | 3 | 4 | |
| I worry that someone in my neighborhood will physically hurt me. | 1 | 2 | 3 | 4 | |
| Depressive Symptoms | |||||
| I am now going to read a list of problems and complaints that people sometimes have. During the past week, including today, please tell me how often you felt or thought that way. | |||||
| Never | Almost Never | Sometimes | Fairly Often | Very Often | |
| Thoughts of ending your life | 1 | 2 | 3 | 4 | 5 |
| Feeling lonely | 1 | 2 | 3 | 4 | 5 |
| Feeling blue (or sad) | 1 | 2 | 3 | 4 | 5 |
| Feeling no interest in things | 1 | 2 | 3 | 4 | 5 |
| Feeling hopeless about the future | 1 | 2 | 3 | 4 | 5 |
| Feelings of worthlessness | 1 | 2 | 3 | 4 | 5 |
Footnotes
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Lepine JP Epidemiology, burden, and disability in depression and anxiety. J. Clin. Psychiatry 2001, 62 (Suppl. 13), 4–10. [PubMed] [Google Scholar]
- 2.Lepine JP; Briley M The increasing burden of depression. Neuropsychiatr. Dis. Treat 2011, 7, 3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shim RS; Baltrus P; Ye J; Rust G Prevalence, treatment, and control of depressive symptoms in the United States: Results from the National Health and Nutrition Examination Survey (NHANES), 2005–2008. J. Am. Board Fam. Med 2011, 24, 33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riolo SA; Nguyen TA; Greden JF; King CA Prevalence of depression by race/ethnicity: Findings from the National Health and Nutrition Examination Survey III. Am. J. Public Health 2005, 95, 998–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blazer DG; Kessler RC; McGonagle KA; Swartz MS The prevalence and distribution of major depression in a national community sample: The National Comorbidity Survey. Am. J. Psychiatry 1994, 151, 979–986. [DOI] [PubMed] [Google Scholar]
- 6.Kessler RC; McGonagle KA; Zhao S; Nelson CB; Hughes M; Eshleman S; Wittchen HU; Kendler KS Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch. Gen. Psychiatry 1994, 51, 8–19. [DOI] [PubMed] [Google Scholar]
- 7.Williams DR; Gonzalez HM; Neighbors H; Nesse R; Abelson JM; Sweetman J; Jackson JS Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life. Arch. Gen. Psychiatry 2007, 64, 305–315. [DOI] [PubMed] [Google Scholar]
- 8.Blazer DG; Landerman LR; Hays JC; Simonsick EM; Saunders WB Symptoms of depression among community-dwelling elderly African-American and white older adults. Psychol. Med 1998, 28, 1311–1320. [DOI] [PubMed] [Google Scholar]
- 9.Jones-Webb RJ; Snowden LR Symptoms of depression among blacks and whites. Am. J. Public Health 1993, 83, 240–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ialongo N; McCreary BK; Pearson JL; Koenig AL; Schmidt NB; Poduska J; Kellam SG Major depressive disorder in a population of urban, African-American young adults: prevalence, correlates, comorbidity and unmet mental health service need. J. Affect. Disord 2004, 79, 127–136. [DOI] [PubMed] [Google Scholar]
- 11.Gore S; Aseltine RH Jr. Race and ethnic differences in depressed mood following the transition from high school. J. Health Soc. Behav 2003, 44, 370–389. [PubMed] [Google Scholar]
- 12.Arnett J Emerging Adulthood: The Winding Road through the Late Teens and Twenties; Oxford University Press: New York, NY, USA, 2004. [Google Scholar]
- 13.Settersten RA; Ray B What’s going on with young people today? The long and twisting path to adulthood. Future Child. 2010, 20, 20–41. [DOI] [PubMed] [Google Scholar]
- 14.Estrada-Martinez LM; Caldwell CH; Bauermeister JA; Zimmerman MA Stressors in multiple life-domains and the risk for externalizing and internalizing behaviors among African Americans during emerging adulthood. J. Youth Adolesc 2012, 41, 1600–1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bell CC; Jenkins EJ Community violence and children on Chicago’s southside. Psychiatry 1993, 56, 46–54. [DOI] [PubMed] [Google Scholar]
- 16.Buka SL; Stichick TL; Birdthistle I; Earls FJ Youth exposure to violence: Prevalence, risks, and consequences. Am. J. Orthopsychiatry 2001, 71, 298–310. [DOI] [PubMed] [Google Scholar]
- 17.Cooley-Strickland M; Quille TJ; Griffin RS; Stuart EA; Bradshaw CP; Furr-Holden D Community violence and youth: Affect, behavior, substance use, and academics. Clin. Child. Fam. Psychol. Rev 2009, 12, 127–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gorman-Smith D; Tolan P The role of exposure to violence and developmental problems among inner-city youth. Dev. Psychopathol 1998, 10, 101–116. [DOI] [PubMed] [Google Scholar]
- 19.Fitzpatrick KM Exposure to violence and presence of depression among low-income, African-American youth. J. Consult. Clin. Psychol 1993, 61, 528–531. [DOI] [PubMed] [Google Scholar]
- 20.Fitzpatrick KM; Piko BF; Wright DR; LaGory M Depressive symptomatology, exposure to violence, and the role of social capital among african american adolescents. Am. J. Orthopsychiatry 2005, 75, 262–274. [DOI] [PubMed] [Google Scholar]
- 21.Jenkins EJ; Wang E; Turner L Traumatic events involving friends and family members in a sample of african american early adolescents. Am. J. Orthopsychiatry 2009, 79, 398–406. [DOI] [PubMed] [Google Scholar]
- 22.Rasmussen A; Aber MS; Bhana A Adolescent coping and neighborhood violence: Perceptions, exposure, and urban youths’ efforts to deal with danger. Am. J. Community Psychol 2004, 33, 61–75. [DOI] [PubMed] [Google Scholar]
- 23.Caldwell CH; Zimmerman MA; Bernat DH; Sellers RM; Notaro PC Racial identity, maternal support, and psychological distress among african american adolescents. Child Dev. 2002, 73, 1322–1336. [DOI] [PubMed] [Google Scholar]
- 24.Lambert SF; Nylund-Gibson K; Copeland-Linder N; Ialongo NS Patterns of community violence exposure during adolescence. Am. J. Community Psychol 2010, 46, 289–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aneshensel CS; Sucoff CA The neighborhood context of adolescent mental health. J. Health Soc. Behav 1996, 37, 293–310. [PubMed] [Google Scholar]
- 26.Garbarino J; Kostelny K; Dubrow N What children can tell us about living in danger. Am. Psychol 1991, 46, 376–383. [DOI] [PubMed] [Google Scholar]
- 27.Ross CE; Mirowsky J Neighborhood disorder, subjective alienation, and distress. J. Health Soc. Behav 2009, 50, 49–64. [DOI] [PubMed] [Google Scholar]
- 28.Latkin CA; Curry AD Stressful neighborhoods and depression: A prospective study of the impact of neighborhood disorder. J. Health Soc. Behav 2003, 44, 34–44. [PubMed] [Google Scholar]
- 29.LaVeist TA Disentangling race and socioeconomic status: A key to understanding health inequalities. J. Urban Health 2005, 82, iii26–iii34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bellair PE; McNulty TL Beyond the bell curve: Community disadvantage and the explanation of black-white differences in adolescent violence. Criminology 2005, 43, 1135–1168. [Google Scholar]
- 31.Copeland-Linder N; Lambert SF; Chen YF; Ialongo NS Contextual stress and health risk behaviors among african american adolescents. J. Youth Adolesc 2011, 40, 158–173. [DOI] [PubMed] [Google Scholar]
- 32.Squires GD; Kubrin CE Privileged places: Race, uneven development and the geography of opportunity in urban America. Urban Stud. 2005, 42, 47–68. [Google Scholar]
- 33.Dupéré V; Leventhal T; Vitaro F Neighborhood processes, self-efficacy, and adolescent mental health. J. Health Soc. Behav 2012, 53, 183–198. [DOI] [PubMed] [Google Scholar]
- 34.Theall KP; Sterk CE; Elifson KW Perceived neighborhood fear and drug use among young adults. Am. J. Health Behav 2009, 33, 353–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miller B; Taylor J Racial and socioeconomic status differences in depressive symptoms among black and white youth: An examination of the mediating effects of family structure, stress and support. J. Youth Adolesc 2012, 41, 426–437. [DOI] [PubMed] [Google Scholar]
- 36.Elder GH; Giele JZ (Eds.) The Craft of Life Course Research; The Guildford Press: New York: NY, USA, 2009. [Google Scholar]
- 37.Watkins DC Depression over the adult life course for African American men: Toward a framework for research and practice. Am. J. Men’s Health 2012, 6, 194–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bronfenbrenner U; Ceci SJ Nature-nurture reconceptualized in developmental perspective: A bioecological model. Psychol Rev 1994, 101, 568–586. [DOI] [PubMed] [Google Scholar]
- 39.Aiyer SM; Heinze JE; Miller AL; Stoddard SA; Zimmerman MA Exposure to violence predicting cortisol response during adolescence and early adulthood: understanding moderating factors. J. Youth Adolesc 2014, 43, 1066–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Assari S; Caldwell CH; Zimmerman MA Sex differences in the association between testosterone and violent behaviors. Trauma Mon. 2014, 19, e18040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Derogatis LR; Spencer PM The Brief Symptom Inventory (BSI): Administration, Scoring and Procedures Manual–I; Johns Hopkins University School of Medicine, Clinical Psychometric Research Unit: Baltimore, MD, USA, 1982. [Google Scholar]
- 42.Derogatis LR SCL-90: Administration, Scoring, and Procedures Manual for the (R)evised Version and other Instruments of the Psychopathology Rating Scale Series; Johns Hopkins University Hospital: Baltimore, MD, USA, 1977. [Google Scholar]
- 43.Connolly MB; Crits-Christoph P; Shelton RC; Hollon S; Kurtz J; Barber JP; Butler SF; Baker S; Thase ME The reliability and validity of a measure of self-understanding of interpersonal patterns. J. Couns. Psychol 1999, 46, 472–482. [Google Scholar]
- 44.Procidano ME; Heller K Measures of perceived social support from friends and from family: Three validation studies. Am. J. Community Psychol 1983, 11, 1–24. [DOI] [PubMed] [Google Scholar]
- 45.Brenner AB; Bauermeister JA; Zimmerman MA Neighborhood variation in adolescent alcohol use: Examination of socioecological and social disorganization theories. J. Stud. Alcohol Drugs 2011, 72, 651–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alessi P Professional iOS Database Applications, and Programming, 2nd ed.; Taylor and Francis Group: New York, NY, USA, 2002. [Google Scholar]
- 47.Arbuckle JL Amos™ 18 User’s Guide; Amos Development Corporation: Crawfordville, FL, USA, 2009. [Google Scholar]
- 48.Kline RB Principles and Practice of Structural Equation Modeling; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- 49.Hu L; Bentler PM Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model 1999, 6, 1–55. [Google Scholar]
- 50.Lei M; Lomax RG The effect of varying degrees of nonnormality in structural equation modeling. Struct. Equ. Model 2005, 12, 1–27. [Google Scholar]
- 51.Tabachnick BG; Fidell LS Using Multivariate Statistics, 3rd ed.; Harper Collins: New York, NY, USA, 1996. [Google Scholar]
- 52.Hammond WP Taking it like a man: Masculine role norms as moderators of the racial discrimination-depressive symptoms association among African American men. Am. J. Public Health 2012, 102 (Suppl 2), S232–S241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.O’Loughlin RE; Duberstein PR; Veazie PJ; Bell RA; Rochlen AB; Fernandez y Garcia E; Kravitz RL Role of the gender-linked norm of toughness in the decision to engage in treatment for depression. Psychiatr. Serv 2011, 62, 740–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Majors R; Billson JM Cool Pose: The Dilemmas of Black Manhood in America; Lexington Books: New York, NY, USA, 1992. [Google Scholar]
- 55.Tracy M; Zimmerman FJ; Galea S; McCauley E; Stoep AV What explains the relation between family poverty and childhood depressive symptoms? J. Psychiatr. Res 2008, 42, 1163–1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zimmerman A; Ramirez-Valles J; Zapert KM; Maton KI A longitudinal study of stress-buffering effects for urban African-American male adolescent problem behaviors and mental health. J. Community Psychol 2000, 28, 17–33. [Google Scholar]
- 57.Ellis KR; Caldwell CH; Assari S; de Loney EH Nonresident African-American fathers’ influence on sons’ exercise intentions in the fathers and sons program. Am. J. Health Promot.: AJHP 2014, 29, 89–98. [DOI] [PubMed] [Google Scholar]
- 58.Howard Caldwell C; Antonakos CL; Assari S; Kruger D; de Loney EH; Njai R Pathways to prevention: Improving nonresident african american fathers’ parenting skills and behaviors to reduce sons’ aggression. Child Dev. 2014, 85, 308–325. [DOI] [PubMed] [Google Scholar]
- 59.Klein K Socioemotional support in african american families coping with maternal HIV: An examination of mothers’ and children’s psychosocial adjustment. Behav. Ther 2000, 31, 1–26. [Google Scholar]
- 60.Costello DM; Swendsen J; Rose JS; Dierker LC Risk and protective factors associated with trajectories of depressed mood from adolescence to early adulthood. J. Consult. Clin. Psychol 2008, 76, 173–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Assari S Race and ethnicity, religion involvement, church-based social support and subjective health in united states: A case of moderated mediation. Int. J. Prev. Med 2013, 4, 208–217. [PMC free article] [PubMed] [Google Scholar]
- 62.Assari S Additive effects of anxiety and depression on body mass index among blacks: Role of ethnicity and gender. Int. Cardiovasc. Res. J 2014, 8, 44–51. [PMC free article] [PubMed] [Google Scholar]
- 63.Assari S; Ahmadi K; Kazemi Saleh D Gender differences in the association between lipid profile and sexual function among patients with coronary artery disease. Int. Cardiovasc. Res. J 2014, 8, 9–14. [PMC free article] [PubMed] [Google Scholar]
- 64.Assari S; Lankarani MM; Lankarani RM Ethnicity modifies the additive effects of anxiety and drug use disorders on suicidal ideation among black adults in the united states. Int. J. Prev. Med 2013, 4, 1251–1257. [PMC free article] [PubMed] [Google Scholar]
- 65.Assari S; Moghani Lankarani M; Kazemi Saleh D; Ahmadi K Gender modifies the effects of education and income on sleep quality of the patients with coronary artery disease. Int. Cardiovasc. Res. J 2013, 7, 141–146. [PMC free article] [PubMed] [Google Scholar]
- 66.Dejman M; Forouzan A; Assari S; Malekafzali H; Nohesara S; Khatibzadeh N; Falahat K; Ekblad S An Explanatory Model of Depression among Female Patients in Fars, Kurds, Turks Ethnic Groups of Iran. Iran. J. Public Health 2011, 40, 79–88. [PMC free article] [PubMed] [Google Scholar]
- 67.Dejman M; Forouzan AS; Assari S; Rasoulian M; Jazayery A; Malekafzali H; Baradaran Eftekhari M; Falahat K; Ekblad S How iranian lay people in three ethnic groups conceptualize a case of a depressed woman: An explanatory model. Ethn. Health 2010, 15, 475–493. [DOI] [PubMed] [Google Scholar]
- 68.Kazemi-Saleh D; Pishgou B; Farrokhi F; Assari S; Fotros A; Naseri H Gender impact on the correlation between sexuality and marital relation quality in patients with coronary artery disease. J. Sex. Med 2008, 5, 2100–2106. [DOI] [PubMed] [Google Scholar]
- 69.Khooshabi K; Ameneh-Forouzan S; Ghassabian A; Assari S Is there a gender difference in associates of adolescents’ lifetime illicit drug use in Tehran, Iran? Arch. Med. Sci.: AMS 2010, 6, 399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mohammadkhani P; Forouzan AS; Khooshabi KS; Assari S; Lankarani MM Are the predictors of sexual violence the same as those of nonsexual violence? A gender analysis. J. Sex. Med 2009, 6, 2215–2223. [DOI] [PubMed] [Google Scholar]
- 71.Tavallaii SA; Fathi-Ashtiani A; Nasiri M; Assari S; Maleki P; Einollahi B Correlation between sexual function and postrenal transplant quality of life: does gender matter? J. Sex Med 2007, 4, 1610–1618. [DOI] [PubMed] [Google Scholar]
- 72.Roy K; Messina L; Smith J; Waters D Growing up as “Man of the House”: Adultification and the Transition into Adulthood for Young Men in Economically Disadvantaged Families. New Dir. Child Adoles. Dev 2014, 143, 55–72. [DOI] [PubMed] [Google Scholar]
- 73.Berzin SC; de Marco AC Understanding the impact of poverty on critical events in emerging adulthood. Youth Soc. 2010, 42, 278–300. [Google Scholar]
- 74.Watkins DC; Green BL; Rivers BM; Rowell KL Depression and black men: Implications for future research. J. Men’s Health Gender Issues 2006, 3, 227–235. [Google Scholar]
- 75.Watkins DC; Abelson JM; Jefferson SO “Their depression is something different…It would have to be”: Findings from a qualitative study of black women’s perceptions of depression in black men. Am. J. Men’s Health 2013, 7, 45S–57S. [DOI] [PubMed] [Google Scholar]
- 76.Givens JL; Houston TK; van Voorhees BW; Ford DE; Cooper LA Ethnicity and preferences for depression treatment. Gen. Hosp. Psychiatry 2007, 29, 182–191. [DOI] [PubMed] [Google Scholar]
- 77.Das AK; Olfson M; McCurtis HL; Weissman MM Depression in African Americans: Breaking barriers to detection and treatment. J. Fam. Pract 2006, 55, 30–39. [PubMed] [Google Scholar]
- 78.Givens JL; Katz IR; Bellamy S; Holmes WC Stigma and the acceptability of depression treatments among african americans and whites. J. Gen. Intern. Med 2007, 22, 1292–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cooper LA; Gonzales JJ; Gallo JJ; Rost KM; Meredith LS; Rubenstein LV; Wang NY; Ford DE The acceptability of treatment for depression among African-American, Hispanic, and white primary care patients. Med. Care 2003, 41, 479–489. [DOI] [PubMed] [Google Scholar]
- 80.Dwight-Johnson M; Sherbourne CD; Liao D; Wells KB Treatment preferences among depressed primary care patients. J. Gen. Intern. Med 2000, 15, 527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Blank MB; Mahmood M; Fox JC; Guterbock T Alternative mental health services: The role of the black church in the South. Am. J. Public Health 2002, 92, 1668–1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Assari S Multilevel approach to intimate partner violence research and prevention. Int. J. Prev. Med 2013, 4, 616–617. [PMC free article] [PubMed] [Google Scholar]