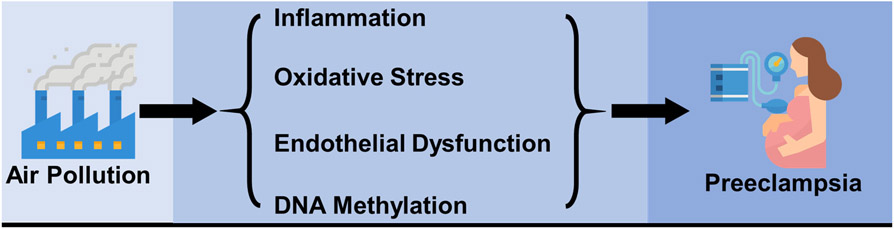
Preeclampsia is a common pregnancy complication and a top contributor to maternal and fetal morbidity and mortality,1 affecting 2% to 8% of all pregnancies globally. Ambient particulate matter air pollution has been recognized as an independent risk factor for cardiovascular morbidity and mortality in the general population,2 and recent meta-analyses suggested that ambient particulate matter and gaseous air pollution are associated with increased odds of preeclampsia.3 While the biological mechanisms underlying the association between air pollution and preeclampsia are largely unknown, several potential pathways have been suggested,3 including inflammation, oxidative stress, endothelial dysfunction, and more recently DNA methylation (Figure 1).4
Figure 1.
Potential mechanisms underlying the associations between air pollution and preeclampsia.
However, significant knowledge gaps exist in the current literature. First, although it is widely recognized that preeclampsia with different onset and severity has distinct pathogenic mechanisms as well as maternal and fetal complications,5 few studies have examined the association between air pollution and the onset and severity of preeclampsia.3 Second, limited research has been conducted to assess the impact of source-specific air pollutants or to identify critical windows of exposure for preeclampsia. Such information may enhance our understanding of the underlying biological mechanisms and help inform the design of more targeted preventive strategies.
In this issue of Hypertension, Assibey-Mensah et al.6 used electronic medical records with linked birth certificate data on 16,116 pregnant women from two hospitals in Monroe County, New York during 2009–2013 to examine the association between wintertime fine particulate matter (PM2.5) and preeclampsia. The authors determined early- and late-onset preeclampsia using the date of clinical diagnosis and/or gestational age at time of diagnosis. The data were then linked with source-specific ambient PM2.5 estimated by land-use regression models to generate women’s month-specific exposures. The authors found that exposure to PM2.5, wood smoke, and traffic pollution in early pregnancy during winter was associated with increased odds of early-onset preeclampsia.
This study represents one of the first efforts to bridge several critical gaps by considering the onset of preeclampsia, assessing source-specific PM2.5, and identifying critical windows of exposure. It also shows several challenges in the field to move this line of research forward. First, when stratifying preeclampsia by its onset and/or severity, the low incidence rate in each category dramatically decreases statistical power, making it hard to be studied in traditional pregnancy and birth cohorts. Similar to Assibey-Mensah et al., many studies in the field utilized electronic medical records data and administrative data such as birth certificates. While these real-world data are increasingly available, challenges remain in algorithmically determining and extracting phenotypes from these complex data sets with not only structured (e.g. diagnosis codes) but also richer unstructured (e.g. physician notes) information. Diagnosis codes-based case definitions are known to have varying misclassification errors across many disease areas including hypertension.7 Leveraging the rich information other than just the diagnosis codes, especially the unstructured clinical notes, can drastically increase the accuracy of these computable phenotypes.8 More efforts on developing standardized, automated, and computerized phenotype algorithms are needed to minimize potential misclassifications. Second, while some modelled estimates of the six criteria air pollutants at high spatiotemporal resolutions are publicly available,9 limited resources exist for source-specific particulate matter air pollution, which usually relies on data collected from stationary monitors. Future efforts are needed to explore innovative methods such as integrations of multisource data (e.g. stationary monitored data and remote sensing data) to assess source-specific particulate matter with large spatiotemporal coverages and high resolutions. Third, despite the existence of statistical methods to account for autocorrelated time-varying exposures such as distributed lag models and survival models with time-varying covariates and coefficients, they have not been widely used in studying ambient air pollution and preeclampsia. Future studies need to implement these methods to identify susceptible windows of exposure.
In summary, the study by Assibey-Mensah et al.6 is a critical first step in understanding how source-specific PM2.5 may impact the onset of preeclampsia. Moving forward, several gaps need to be addressed. First, it would be critical to conduct mechanistic studies to examine the molecular mechanisms such as epigenetic factors in mediating the association between ambient air pollution and preeclampsia, and to elucidate the biological mechanisms underlying the potential differential effects of air pollution exposure on preeclampsia with different onset. Second, more advanced approaches need to be implemented to examine the joint effects of air pollution mixtures on preeclampsia.10 Third, more studies are warranted to examine the impact of pregnancy air pollution exposure on women’s cardiovascular health (CVH) during and after pregnancy. While many studies have examined the association between air pollution and pregnancy complications such as hypertensive disorders of pregnancy (HDP) and gestational diabetes mellitus (GDM), no study has assessed the potential impact of air pollution on CVH among pregnant women. A recent study reported that a better CVH in pregnancy was associated with a better CVH and a lower cardiovascular disease (CVD) risk 10 years postpartum,11 suggesting that pregnancy may be a prime time to promote CVH among women. Given the increased odds of HDP and GDM associated with air pollution, it is plausible that air pollution may impact pregnancy CVH, even among those without any pregnancy complication. In addition, previous studies showed that women with a history of preeclampsia have around 2 times higher risk of CVD later in life compared with those without preeclampsia.12 However, no epidemiological study has examined the potential long-term cardiovascular impact of air pollution exposure during pregnancy. Further investigation is warranted to address these gaps in existing literature.
Supplementary Material
Acknowledgments
Sources of funding: Dr. Hu’s work was supported by the Scientist Development Grant (17SDG33630165) from the American Heart Association. Dr. Bian’s work was supported by the University of Florida Clinical and Translational Science Institute, which is supported in part by the National Institute of Health National Center for Advancing Translational Sciences under award number UL1TR001427. Dr. Zhao’s work was supported by the National Institute of Health under award number R01DK107532, RF1AG052476 and R01MH097018.
Footnotes
Disclosures: None.
References
- 1.Duley L. The global impact of pre-eclampsia and eclampsia. Seminars in perinatology. 2009;33:130–137 [DOI] [PubMed] [Google Scholar]
- 2.Brook RD, Rajagopalan S, Pope III CA, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the american heart association. Circulation. 2010;121:2331–2378 [DOI] [PubMed] [Google Scholar]
- 3.Hu H, Ha S, Roth J, Kearney G, Talbott EO, Xu X. Ambient air pollution and hypertensive disorders of pregnancy: A systematic review and meta-analysis. Atmospheric Environment. 2014;97:336–345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abraham E, Rousseaux S, Agier L, Giorgis-Allemand L, Tost J, Galineau J, Hulin A, Siroux V, Vaiman D, Charles M- A. Pregnancy exposure to atmospheric pollution and meteorological conditions and placental DNA methylation. Environment international. 2018;118:334–347 [DOI] [PubMed] [Google Scholar]
- 5.Valensise H, Vasapollo B, Gagliardi G, Novelli GP. Early and late preeclampsia: Two different maternal hemodynamic states in the latent phase of the disease. Hypertension. 2008;52:873–880 [DOI] [PubMed] [Google Scholar]
- 6.Assibey-Mensah V, Glantz JC, Hopke PK, Jusko TA, Thevenet-Morrison K, Chalupa D, Rich DQ. Wintertime wood smoke, traffic particle pollution, and preeclampsia. Hypertension. 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quan H, Khan N, Hemmelgarn BR, Tu K, Chen G, Campbell N, Hill MD, Ghali WA, McAlister FA. Validation of a case definition to define hypertension using administrative data. Hypertension. 2009;54:1423–1428 [DOI] [PubMed] [Google Scholar]
- 8.Mo H, Thompson WK, Rasmussen LV, Pacheco JA, Jiang G, Kiefer R, Zhu Q, Xu J, Montague E, Carrell DS. Desiderata for computable representations of electronic health records-driven phenotype algorithms. Journal of the American Medical Informatics Association. 2015;22:1220–1230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim S, Bechle M, Hankey S, Sheppard L, Szpiro A, Marshall J. Concentrations of criteria pollutants in the contiguous us, 1979–2015: Role of model parsimony in integrated empirical geographic regression: University of washington biostatistics working paper series; 2018. [cited 2019 april 12]. 2018 [Google Scholar]
- 10.Coull B, Bobb J, Wellenius G, Kioumourtzoglou M, Mittleman M, Koutrakis P, Godleski J. Part 1. Statistical learning methods for the effects of multiple air pollution constituents. Research report (Health Effects Institute). 2015:5–50 [PubMed] [Google Scholar]
- 11.Benschop L, Schalekamp-Timmermans S, Schelling SJ, Steegers EA, Roeters van Lennep JE. Early pregnancy cardiovascular health and subclinical atherosclerosis. Journal of the American Heart Association. 2019;8:e011394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu P, Haththotuwa R, Kwok CS, Babu A, Kotronias RA, Rushton C, Zaman A, Fryer AA, Kadam U, Chew-Graham CA. Preeclampsia and future cardiovascular health: A systematic review and meta-analysis. Circulation: Cardiovascular Quality and Outcomes. 2017;10:e003497. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.